1. Introduction
The assessment of anxiety symptoms in youth with autism spectrum disorders (ASD) is challenging for both clinicians and researchers (Kerns & Kendall, 2013). Although recent literature suggests that youth with ASD are at increased risk of developing anxiety symptoms (Simonoff et al., 2008), few studies have explored the clinical utility of existing anxiety measures in this population (Lecavalier et al., 2013). The validity of self-report of symptoms has been questioned, given the significant impairments in affective awareness and insight characteristic of youth with neurodevelopmental disorders (Mazzone, Ruta, & Reale, 2012; White, Oswald, Ollendick, & Scahill, 2009). The accuracy of parent report of youth symptoms is also problematic, given that anxiety is, by nature, an internal experience; external (i.e., observable) aspects of anxiety (such as increased motor agitation or social withdrawal) can be difficult for parents and clinicians to differentiate from core symptoms of autism (Mazzone et al., 2012). Similarly, it is often difficult to distinguish between anxiety and other co-occurring psychiatric disorders such as depression and ADHD (Brown & Barlow, 2009).
More work is needed examining the psychometric characteristics of commonly used anxiety assessment tools in youth with ASD (Lecavalier et al., 2006). Given that most youth with ASD will be seen in primary care settings and not in psychiatric clinics, there is a particular need for validation of time-efficient, brief rating scales to screen those who require further psychiatric evaluation and/or referral for anxiety treatment.
Silverman and Ollendick (2005) describe the evidence for different brief anxiety assessment tools in the general pediatric population. Common screening tools include the Multidimensional Anxiety Scale for Children (MASC; March, Sullivan, & Parker, 1999), the Revised Children’s Manifest Anxiety Scale (Reynolds & Richmond, 1985), the Spence Children’s Anxiety Scale (Spence, Barrett, & Turner, 2003), the State Trait Anxiety Inventory for Children (Southam-Gerow, Flannery-Schroeder, & Kendall, 2002; Spielberger, Gorsuch, & Lushene, 1970), and the Screen for Child Anxiety Related Disorders (SCARED) (Birmaher et al., 1999). They determined that the SCARED and the MASC have the most empirical support for discriminating between anxiety and other disorders in typically developing youth (Birmaher et al., 1999; Silverman & Ollendick, 2005).
Psychometric properties of the SCARED have been well established in typically developing children by Birmaher’s (1997, 1999) original validation studies, as well as through subsequent research (e.g., Hale, Crocetti, Raaijmakers, & Meeus, 2011). In the original SCARED study, Birmaher (1997) established a five-factor structure in a typically developing sample with clinical anxiety, demonstrating high internal consistency (α=.93, range: .74 – .89 for subscales) and strong discriminant validity (for disruptive behavior disorders and depressive disorders), based on the Child Behavior Checklist (CBCL; Achenbach & Edelbrock, 1980; Birmaher et al., 1997). These findings were replicated in a second study by the group (Birmaher et al., 1999). Hale and colleagues (2011) conducted a meta-analysis of 25 studies with typically developing children around the world examining the psychometric properties of the SCARED. This meta-analysis found a 3–5 factor structure with generally high internal consistency (α=.91). One relatively weak factor in this study was school anxiety/refusal. Additionally, females were found to report more anxiety than males, particularly in younger children. Linyan and colleagues (2008) found similarly robust psychometric properties in a community sample of Chinese children and adolescents; they also report that total anxiety scores increased with age. van Steensel, Deutschman, and Bögels (2012) examined psychometric properties in the extended 71-question Screen for Child Anxiety Related Disorders (Bodden, Bögels, & Muris, 2009) in a group of children aged 8–13 with ASD and compared them with a group of typically developing children with anxiety disorders. The group used the ADIS (parent and child versions) for comparison. They found a high internal consistency (α > 0.9 for both ASD and typically developing groups) and correlations between ADIS and SCARED in the ASD group ranging from .20 to .47. We are not aware of any studies examining the briefer 41-item SCARED for assessment of anxiety in youth through age 18 with ASD.
The goal of the present study was to examine the psychometric characteristics of the 41-item version of the SCARED in a sample of youth with ASD seeking treatment for anxiety symptoms. The SCARED was chosen due to its brevity (41 questions), the face validity of the items, the availability of both parent and youth versions, and its strong psychometric properties in typically developing children. The specific aims of the present study were to (1) examine the factor structure and internal consistency of sub scales; (2) describe mean values and distributions of subscales in this ASD sample, as compared to previously published normative samples; (3) investigate sources of variability including gender, age, and race/ethnicity; 4) assess convergent validity with an empirically strong structured interview. We hypothesized that (1) the SCARED will demonstrate strong internal consistency and would conform to a five-factor structure, similar to previous studies in the general pediatric population; (2) youth with ASD will evince somewhat different patterns of anxiety symptoms compared to norms established with typically developing populations; (3) endorsement of separation anxiety and school phobia symptoms will be higher among children than adolescents, girls will evince higher levels of social anxiety than boys, and anxiety symptoms will be similar across racial/ethnic groups; and (4) the SCARED will demonstrate good convergence with an established interview assessment of anxiety symptoms.
2. Method
2.1 Participants
Participants were recruited through Colorado Multiple Institution Review Board (COMIRB) approved study announcements for two studies of a CBT-based treatment for youth with autism spectrum disorder and anxiety (see Reaven, Blakeley-Smith, Culhane-Shelburne, & Hepburn, 2012a; Reaven, Blakeley-Smith, Leuthe, Moody, & Hepburn, 2012b). The first cohort comprised 83 children (86.7% male) ranging in age from 7 to 14 years old (M = 10.81, SD = 1.75) and their parents; the second cohort comprised 36 adolescents (69.4% male) ranging in age from 13 to 18 years old (M = 15.69, SD = 1.12) and their parents.
Inclusion criteria for the current study were: (1) chronological age from 7–18 years; (2) speaking in full, complex sentences, as determined through completion of Module III or Module IV on the Autism Diagnostic Observation Schedule (ADOS; Lord, Rutter, DiLavore, & Risi, 1999); (3) verbal IQ of at least 70 on a recent administration of the Wechsler Abbreviated Scales of Intelligence (WASI; Weschler, 2002) or an equivalent intelligence measure; and (4) confirmed diagnosis of an ASD, as determined by a clinical psychologist’s review of a recently administered ADOS and of scores on the Social Communication Questionnaire (SCQ; Berument, Rutter, Lord, Pickles, & Bailey, 1999). The total sample for the current investigation included 119 families (see Table 1 for participant characteristics).
Table 1.
Participant Characteristics
| Child Characteristic | M (SD) or Percent | Range |
|---|---|---|
| Age (years) | 12.3 (2.8) | 8 – 18 |
| IQ | 101.7 (17.7) | 62 – 139 |
| Verbal | 102.9 (19.4) | 40 – 155 |
| Nonverbal | 103.3 (17.8) | 64 – 144 |
| Gender | ||
| Male | 81.5% | |
| Race and Ethnicity | ||
| Caucasian | 84.6% | |
| African American | 2.6% | |
| Latino/Hispanic | 8.5% | |
| Asian | 3.4% | |
| Biracial & Other | 6.9% | |
| Diagnoses (structured interview) | ||
| Panic Disorder | 0.8% | |
| GAD | 44.5% | |
| Specific Phobia | 39.5% | |
| Social Anxiety | 40.3% | |
| Separation Anxiety | 16.8% | |
| OCD | 26.1% |
Note: structured interview=Anxiety Disorders Interview Schedule—Parent Version or Kiddie Schedule for Affective Disorders and Schizophrenia; GAD = Generalized Anxiety Disorder; OCD = Obsessive Compulsive Disorder.
The original sample used in Birmaher’s paper describing the psychometric properties of the SCARED used a clinical sample of children 9–18 years referred to a mood and anxiety disorder clinic. Of those, 82 percent were Caucasian and 18 percent African American; 59% were female (Birmaher et al., 1999). Our sample was also a clinical population with the additional criteria that all had a diagnosis of ASD, more were male (82.6%) and the age range was 7 to 18 years.
2.2 Procedure
The study was completed in compliance with COMIRB guidelines. Parents initiated contact with the research clinic and completed a brief telephone screen for eligibility. If the child was potentially eligible for the study, the family was invited to attend a clinic session, where informed consent was obtained prior to initiating any data gathering activities. The family then completed a qualification battery, which included the ADOS, the SCQ, standardized cognitive testing (when necessary), the SCARED (completed separately for children and parents), and additional measures not relevant to the current investigation. If the child met eligibility criteria on these assessments, the parent was invited to complete a structured clinical interview assessing child anxiety at a second session. Families were compensated for their participation. Details regarding the intervention methodology and outcome measures are described elsewhere (see Reaven et al. 2012a; 2012b). The current study investigates the psychometric properties of the SCARED as administered to parents and children/adolescents meeting eligibility criteria at pretreatment.
2.3 Measures
Autism Diagnostic Observation Schedule
The ADOS (Lord et al., 1999) is a semi-structured, standardized assessment of social and communicative behavior indicative of Autism Spectrum Disorder (ASD). It is considered the “gold standard” for the diagnosis of ASD (Lord, Rutter, & Couteur, 1994). The measure consists of four modules, each approximately 30 to 45 minutes in length, which assess behavior across a range of ages and developmental and verbal levels; for the current sample, Modules 3 and 4 were used. Items are scored on a 4-point scale from 0 (“no abnormality of type specified”) to 3 (“moderate to severe abnormality”). Lab personnel met research reliable administration criteria on the ADOS prior to the study and were trained to 85% reliability on the full range of scores. Assessments were videotaped and subject to expert clinical review, and reliability was maintained at 85% for more than 20% of the ADOS administrations across both the child and the adolescent cohorts.
Social Communication Questionnaire—Lifetime Version
The SCQ—Lifetime Version (Berument et al., 1999) is a 40-item parent-report checklist of current and historical symptoms of autism derived from the Autism Diagnostic Interview-Revised (ADI-R; Lord et al., 1994). The SCQ demonstrates strong specificity (.72) and sensitivity (.88) in middle childhood samples (Chandler et al., 2007). Chronbach’s alpha was .76 in the current sample. Clinicians reviewed parent responses on the SCQ in conjunction with results from the ADOS to determine whether children met criteria for an ASD.
Structured clinical interview
One of two structured interviews was used to determine baseline anxiety disorder status: the Anxiety Disorders Interview Schedule for DSM-IV: Parent Version (ADIS-P; Silverman & Albano, 1996) or the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS; Kaufman et al. 1997).
The ADIS is a best-practice, structured psychiatric interview that assesses symptoms of anxiety and related disorders in children and adolescents. The ADIS demonstrates excellent psychometric properties, including test-retest reliability for both symptom scales and diagnoses (Silverman et al., 2001) and convergent validity with other anxiety assessments (Lyneham & Rapee, 2005; Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). Independent clinical evaluators trained in the ADIS protocol conducted the interviews, provided diagnostic classifications across categories on the DSM-IV, and assigned Clinician Severity Ratings (CSRs) of severity and interference for individual diagnoses, as well as a Clinical Global Impressions—Severity (CGI-S) score for the interview overall. All evaluators were trained to 80% reliability for clinical diagnoses, CSRs, and CGI-S ratings on three videotaped and three live administrations of the ADIS-P. The ADIS-P was administered prior to treatment, and reliability was obtained on at least 20% of cases.
In a minority of cases,1 the K-SADS was administered to parents in place of the ADIS. The K-SADS is a widely used standardized psychiatric interview assessing children’s developmental, educational, family, and treatment history. Following a set of screening questions, the interviewer queries about specific symptoms and interference with functioning; responses are scored against DSM criteria to determine the presence or absence of each disorder. The K-SADS has been used in multiple studies of children with ASD (e.g., Gjevik et al., 2011; Leyfer et al., 2006).
Screen for Child Anxiety Related Disorders
The SCARED (Birmaher et al., 1999) is a 41-item inventory of child anxiety symptoms with parallel versions for parent-report and child self-report. Children (ages 8–18) and parents respond to a series of statements such as “People tell me I look nervous/that my child looks nervous” using a 3-point Likert scale, with 0 indicating “not true or hardly ever true” and 2 indicating “very true or often true”. Item scores are summed to yield a total anxiety score, as well as subscale scores for somatic symptoms/panic disorder, generalized anxiety disorder (GAD), separation anxiety, social phobia, and school phobia. Prior investigations indicate an optimal cutoff score of 25 for clinically significant anxiety (Birmaher et al., 1999). In studies of outpatient psychiatric samples, the SCARED demonstrated good convergent and divergent validity with other psychiatric assessment tools, as well as strong sensitivity (.71) and specificity (.67) (Birmaher et al., 1997, 1999; Monga, Birmaher, Chiappetta et al., 2000). Due to the timeframe of the study, instructions were modified such that participants reported on anxiety severity only in the past two weeks.
3. Results
3.1 Aim 1: Factor structure and internal consistency
First, the factorability of the parent and child versions of the SCARED was examined in terms of established criteria for factor analysis. All items of both versions correlated with at least one other item at the .30 level or greater. The Kaiser-Meyer-Olkin measure of sampling adequacy was .75 for the child version and .69 for the parent version, both well above the recommended .60 level. Barlett’s test of sphericity was significant for the child version (χ2 (820) = 1,964.99, p < .001) as well as the parent version (χ2 (820) = 2,088.92, p < .001). In addition, almost all communalities were above .30. Together, these indicators supported the use of factor analysis for the full 41-item scale.
Principal components analysis was performed separately on the parent and child versions of the SCARED. Eigenvalues exceeded 1.0 for 12 factors on the child version and 12 factors on the parent version. A number of possible solutions were examined using varimax rotations of the factor loading matrix. Varimax rotation was used to replicate the analyses reported by Birmaher and colleagues (1997, 1999).2 Examination of the scree plot, as well as extant research, supported a five factor solution, which explained 49% and 47% of the variance in the child and parent versions of the SCARED, respectively. All items had primary factor loadings of .30 or higher. Most conformed to the factor structure originally proposed by Birmaher and colleagues (1997, 1999); however, school phobia remained a weak factor. (See Table 2 for child and parent factor loadings.)
Table 2.
Factor Loadings for Principal Components Analysis of Child Self-Report and Parent-Report (in Parentheses) of the SCARED.
| Factor |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | Panic/Somatic | Generalized Anxiety | Separation Anxiety | Social Phobia | School Phobia | ||||||
| Panic/Somatic | |||||||||||
| 1. | When I feel frightened, it is hard to breathe. | .50 | (.67) | .07 | (−.05) | .32 | (−.17) | .13 | (.07) | .27 | (.17) |
| 6. | When I get frightened, I feel like passing out. | .41 | (.57) | .10 | (−.02) | .33 | (.30) | .18 | (.08) | .25 | (−.04) |
| 9. | People tell me that I look nervous. | .28 | (.06) | .01 | (−.07) | .19 | (−.07) | .27 | (.23) | .30 | (.51) |
| 12. | When I get frightened, I feel like I am going crazy. | .26 | (.31) | .49 | (−.15) | .19 | (.12) | −.03 | (.05) | −.04 | (.41) |
| 15. | When I get frightened, I feel like things are not real. | .32 | (.35) | −.01 | (−.14) | .29 | (.40) | .05 | (.09) | .54 | (.08) |
| 18. | When I get frightened, my heart beats fast. | .23 | (.46) | .31 | (−.10) | .14 | (.16) | .35 | (.26) | .16 | (.21) |
| 19. | I get shaky. | .48 | (.68) | .32 | (.10) | .06 | (−.03) | .24 | (.08) | −.02 | (.17) |
| 22. | When I get frightened, I sweat a lot. | .46 | (.29) | .10 | (−.01) | .07 | (−.11) | .09 | (.34) | .17 | (.14) |
| 24. | I get really frightened for no reason at all. | .01 | (.18) | .56 | (−.05) | .23 | (.22) | .13 | (−.01) | .29 | (.64) |
| 27. | When I get frightened, I feel like I am choking. | .63 | (.61) | .03 | (.11) | .10 | (−.06) | .07 | (−.10) | .17 | (.13) |
| 30. | I am afraid of having anxiety (or panic) attacks. | .42 | (.38) | .19 | (.09) | .19 | (−.03) | .32 | (.03) | .11 | (.59) |
| 34. | When I get frightened, I feel like throwing up. | .51 | (.64) | .00 | (.20) | .31 | (.09) | .01 | (.00) | .24 | (.06) |
| 38. | When I get frightened, I feel dizzy. | .72 | (.67) | −.04 | (.08) | −.02 | (.17) | .06 | (.05) | .22 | (.13) |
| Generalized Anxiety | |||||||||||
| 5. | I worry about other people liking me. | .14 | (.09) | .38 | (.66) | .15 | (.15) | .11 | (.04) | .48 | (.12) |
| 7. | I am nervous. | .10 | (.15) | .64 | (−.01) | .09 | (.26) | .23 | (.22) | .06 | (.54) |
| 14. | I worry about being as good as other kids. | .13 | (.14) | .30 | (.76) | −.07 | (.00) | .18 | (.12) | .67 | (−.08) |
| 21. | I worry about things working out for me. | .15 | (.07) | .48 | (.55) | −.36 | (−.11) | −.07 | (.18) | .44 | (.43) |
| 23. | I am a worrier. | .04 | (.15) | .61 | (.44) | −.04 | (.10) | .35 | (.16) | .09 | (.55) |
| 28. | People tell me that I worry too much. | .19 | (.00) | .58 | (.06) | −.03 | (.00) | .11 | (.19) | .06 | (.68) |
| 33. | I worry about what is going to happen in the future. | −.09 | (.02) | .51 | (.35) | .23 | (.00) | .10 | (.07) | .50 | (.57) |
| 35. | I worry about how well I do things. | .29 | (.00) | .20 | (.74) | −.12 | (−.19) | .27 | (.25) | .56 | (.08) |
| 37. | I worry about things that have already happened. | −.06 | (.34) | .68 | (.33) | .32 | (.20) | .09 | (.00) | .08 | (.41) |
| Separation Anxiety | |||||||||||
| 4. | I get scared if I sleep away from home. | .19 | (.10) | .10 | (.09) | .51 | (.58) | .35 | (.22) | .20 | (.03) |
| 8. | I follow my mother or father wherever they go. | .12 | (.05) | .10 | (−.32) | .55 | (.47) | .25 | (.16) | −.06 | (.20) |
| 13. | I worry about sleeping alone. | .02 | (.00) | .21 | (−.14) | .64 | (.48) | .01 | (−.12) | .26 | (.00) |
| 16. | I have nightmares about something bad happening to my parents. | .48 | (−.09) | .10 | (.09) | .60 | (.69) | −.07 | (−.20) | .24 | (.10) |
| 20. | I have nightmares about something bad happening to me. | .26 | (.08) | .08 | (−.02) | .73 | (.44) | −.10 | (−.03) | .20 | (.36) |
| 25. | I am afraid to be alone in the house. | .20 | (.06) | .14 | (−.10) | .52 | (.67) | .23 | (.05) | −.29 | (−.08) |
| 29. | I don’t like to be away from my family. | .07 | (.09) | .00 | (.14) | .71 | (.47) | .10 | (.33) | .17 | (.18) |
| 31. | I worry that something bad might happen to my parents. | .29 | (−.16) | .21 | (.16) | .71 | (.52) | −.16 | (.05) | .18 | (.40) |
| Social Phobia | |||||||||||
| 3. | I don’t like to be with people I don’t know well. | −.15 | (.03) | .04 | (.09) | .39 | (.23) | .60 | (.73) | .01 | (.06) |
| 10. | I feel nervous with people I don’t know well. | .08 | (.18) | .25 | (.06) | .18 | (.11) | .69 | (.77) | .00 | (.04) |
| 26. | It is hard for me to talk with people I don’t know well. | .03 | (−.02) | .10 | (.14) | .10 | (−.06) | .71 | (.81) | .27 | (.09) |
| 32. | I feel shy with people I don’t know well. | .17 | (.06) | .18 | (.06) | −.20 | (−.02) | .78 | (.84) | .21 | (−.04) |
| 39. | I feel nervous when I am with other children or adults and I have to do something while they watch me. | .14 | (−.06) | .09 | (.17) | .23 | (.13) | .29 | (.70) | .33 | (.17) |
| 40. | I feel nervous when I am going to parties, dances, or any place where there will be people that I don’t know well. | .09 | (.15) | .02 | (.13) | .03 | (−.02) | .70 | (.68) | .20 | (.34) |
| 41. | I am shy. | .19 | (−.06) | .22 | (−.02) | −.09 | (−.09) | .66 | (.74) | .09 | (.15) |
| School Phobia | |||||||||||
| 2. | I get headaches when I am at school. | .63 | (.32) | .13 | (.19) | .10 | (.37) | .03 | (.19) | −.08 | (.11) |
| 11. | I get stomachaches at school. | .53 | (.38) | .17 | (.11) | .43 | (.43) | .01 | (−.13) | −.22 | (.08) |
| 17. | I worry about going to school. | .12 | (.25) | .10 | (.15) | .27 | (.32) | .22 | (.10) | .61 | (.39) |
| 36. | I am scared to go to school. | .12 | (.31) | −.05 | (.15) | .23 | (.33) | .19 | (.00) | .50 | (.55) |
The SCARED demonstrated good internal consistency for both parent and child report in the current sample. Chronbach’s alpha on the full scale was .90 for parent report and .92 for child report, ranging from .62–.89 for individual subscales (see Table 3). Results were comparable to those published by Birmaher and colleagues in their validation studies (1997; 1999).
Table 3.
Internal Consistency (Cronbach’s Alpha) for Subscales of the SCARED
| Subscale | N items | α | Sensitivity | Specificity |
|---|---|---|---|---|
| Child Version | ||||
| Panic/Somatic | 13 | .82 | .67 | .62 |
| GAD | 9 | .80 | .30 | .40 |
| Separation Anxiety | 8 | .84 | .73 | .75 |
| Social Anxiety | 7 | .82 | .37 | .80 |
| School Avoidance | 4 | .62 | – | – |
| Total (all items) | 41 | .92 | .52 | .78 |
| Parent Version | ||||
| Panic/Somatic | 13 | .79 | 1.00 | .53 |
| GAD | 9 | .80 | .75 | .33 |
| Separation Anxiety | 8 | .74 | .86 | .74 |
| Social Anxiety | 7 | .89 | .70 | .83 |
| School Avoidance | 4 | .73 | – | – |
| Total (all items) | 41 | .90 | .71 | .67 |
Note: SCARED = Screen for Child Anxiety Related Disorders; GAD = Generalized Anxiety Disorder. Sensitivity and specificity were calculated via comparison to the ADIS-P.
3.2 Aim 2: Means and distribution of scores
Child- and parent-reported anxiety scores were normally distributed for most subscales, with mild floor effects (positive skew) for panic, separation anxiety, and school phobia. Children reported the most symptom severity on the Separation Anxiety subscale, with 50.4% scoring above the clinical cutoff. Parents reported greatest severity on the GAD subscale, with 69.9% of scoring above the cutoff. On the full scale of items, as well as on all subscales, parents reported greater severity of anxiety symptoms (M = 33.01, SD = 13.09) than did their children (M = 22.77, SD = 14.59) (see Table 4). Results were generally consistent with Birmaher et al. (1997), but parent-reported anxiety was somewhat higher in the current sample for GAD and social anxiety. Correlations between parent and child report of symptoms was low to moderate; results are reported elsewhere (see Blakeley-Smith et al., 2012).
Table 4.
Descriptive Statistics on Subscales of the SCARED
| Subscale | % Above Cutoff | M (SD) |
Birmaher
(1997) M (SD) |
|---|---|---|---|
| Child report | |||
| Panic/Somatic | 39.0% | 6.0 (4.8) | 6.9 (6.1) |
| GAD | 30.5% | 6.9 (4.2) | 9.1 (4.9) |
| Separation Anxiety | 50.9% | 5.3 (4.1) | 3.5 (3.4) |
| Social Anxiety | 37.6% | 6.7 (3.7) | 3.7 (2.5) |
| School Avoidance | 39.3% | 2.3 (1.9) | 2.6 (2.1) |
| Total (all items) | 46.9% | 27.4 (14.4) | 26.8 (14.7) |
| Parent report | |||
| Panic/Somatic | 42.0% | 6.5 (4.6) | – |
| GAD | 69.8% | 10.5 (4.0) | – |
| Separation Anxiety | 50.9% | 5.0 (3.5) | – |
| Social Anxiety | 54.7% | 7.9 (4.3) | – |
| School Avoidance | 47.5% | 2.8 (2.2) | – |
| Total (all items) | 68.9% | 32.8 (12.9) | – |
3.3 Aim 3: Discriminant and convergent validity
Discriminant validity was assessed by comparing the number of children meeting criteria for one or more anxiety diagnoses on the SCARED with the number meeting criteria for an anxiety disorder on a structured clinical interview. Sensitivity was .71 for the SCARED—Parent Version and .52 for the Child Version. Specificity was .67 for the SCARED—Parent Version and .78 for the Child Version.3 Sensitivity and specificity for subscales of the SCARED are presented in Table 3.
Convergent validity was examined via correlations between parent and youth total scores on the SCARED with the Clinicians Global Impressions—Severity (CGI-S), and via correlations between SCARED subscales and Clinician Severity Ratings (CSRs) of corresponding diagnostic categories based on the ADIS-P. Moderate correlations were observed between total SCARED Scores and the overall CGI-S on the ADIS-P (youth report: r = .49, p = .022; parent report: r = .44, p = .041). For specific diagnoses, GAD symptoms (CSRs) on the ADIS-P were associated with GAD scores on the SCARED—parent report (r = .35, p = .006) and youth report (r = .29, p = .029). Similarly, separation anxiety on the ADIS-P was associated with parent-reported separation anxiety on the SCARED (r = .46, p = .032), and social anxiety on the ADIS-P was associated with child-reported social anxiety on the SCARED (r = .28, p = .043). Because no children met clinical criteria for panic disorder on the ADIS-P and there is no rating assigned for school avoidance on the interview, CSRs were not available for these diagnoses and comparisons to the panic/somatic and school phobia subscales of the SCARED could not be made.
3.4 Aim 4: Sources of variability
Child age
Children reported greater separation anxiety symptoms (M = 6.14, SD = 4.27) than did adolescents (M = 3.50, SD = 3.16), F(1, 106) = 10.32, p = .002, consistent with Birmaher et al. (1997). Similarly, children reported higher levels of school phobia (M = 2.56, SD = 1.89) compared to adolescents (M = 1.74, SD = 1.66), F(1, 105) = 4.77, p = .031. Parents reported significantly higher scores on the GAD subscale of the SCARED for adolescents (M = 11.78, SD = 3.95) than for children (M = 9.93, SD = 3.91), F(1, 114) = 5.54, p = .020. Parents also reported higher total scores for adolescents (M = 36.42, SD = 14.87) than for children (M = 31.11, SD = 11.61), F(1, 104) = 3.98, p = .049. No other differences were observed between the two age cohorts. Figure 1 displays parent- and child-reported total scores for the two cohorts. (For detailed discussion of parent-youth agreement, see Blakeley-Smith et al., 2012.)
Figure 1.
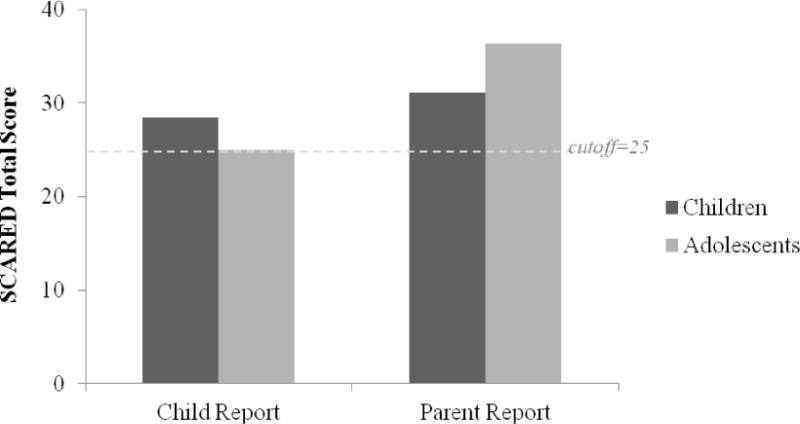
Total scores on the parent and child versions of the SCARED for the child and adolescent cohorts
Child gender
There were no significant gender differences in child-reported anxiety symptoms. Parent-reported social anxiety scores were higher for female children (M = 10.10, SD = 3.48) than for male children (M = 7.35, SD = 4.36), F(1, 115) = 7.27, p = .008. A similar pattern of gender differences was noted across all subscales in Birmaher et al. (1997).
Race and ethnicity
Comparisons by ethnicity (i.e., Hispanic vs. non-Hispanic) revealed that Hispanic children reported slightly greater GAD symptoms (M = 9.67, SD = 2.83) compared to non-Hispanic children (M = 6.66, SD = 4.21), F(1, 101) = 4.38, p = .039. Results of a one-way Analysis of Variance (ANOVA) indicated that anxiety scores did not differ between racial groups (i.e., African-American, Asian, Caucasian, biracial/other).
Discussion
Assessing anxiety in youth with developmental disabilities represents a significant challenge for researchers, mental health practitioners, and families seeking help for social and emotional difficulties (Kerns & Kendall, 2013). Additional research is needed to establish the validity of assessment tools in special populations where risk for comorbid psychopathology is high (Simonoff et al., 2008). Given that good, psychometrically robust anxiety screening tools have been established in the general pediatric population, examining these tools in youth with ASD is a crucial next step (Lecavalier et al., 2006, 2013). The current study is one of the first to examine the reliability and validity of a brief, easily implemented anxiety screening tool integrating parent- and youth self-report in an ASD sample. Our findings suggest that the 41-item SCARED is a valid and clinically useful tool for assessing anxiety in treatment-seeking children and adolescents with ASD. The results of each study aim, as well as areas for further study, are discussed below.
4.1 Examination of internal consistency and factor structure (Aim 1)
The SCARED demonstrated moderate-to-strong psychometric properties in the current sample of youth with high-functioning ASD seeking treatment for anxiety. Internal consistency of the scale items was high for both parent and youth report in our sample, similar to levels reported in previous studies of typically developing youth (e.g., Birmaher et al., 2007). Chronbach’s alpha on the full scale was .90 for parent report and .92 for child report. Both parent- and child-report generally conformed to the five-factor structure observed in typically developing youth from clinical populations (Birmaher et al., 1997, 1999; Weitkamp et al., 2010) as well as community populations (Essau et al., 2002; Muris et al, 2006; Su et al., 2008; Wren et al., 2004). School Phobia emerged as a weak factor, similar to Birmaher et al. (1997), and consistent with psychometric studies yielding four-factor solutions without School Phobia (Muris et al., 1998a, 1998b, 2002; Ogliari et al., 2006). Somatic school phobia symptoms (i.e., “I get headaches when I am at school” and “I get stomachaches at school”) tended to load onto the Separation Anxiety factor for parent-report and onto the Panic/Somatic factor for youth-report. This suggests that parents of children with ASD may view these behaviors as stemming from relationship-related fears about leaving the parent, while children may view them as part of their general somatic symptomology.
Factor loadings in our sample of youth with ASD differed from those reported for typically developing youth with regard to the Panic/Somatic subscale and GAD (Birmaher et al., 1997), with several items in each subscale loading onto the School Phobia factor. We speculate that these results may reflect differences in sensory processing and modulation often associated with ASD (e.g., Ben-Sasson et al., 2009). For GAD, youth report on peer-oriented items such as “I worry about other people liking me” and “I worry about being as good as the other kids” tended to load onto the School Phobia factor, suggesting that school-related fears may be tied to fears of negative evaluation by peers (a more common concern for youth with ASD). Overall, the consistently strong internal consistency and factor structure support the use of the SCARED for clinical and research use in youth with ASD.
4.2 Mean values and distributions (Aim 2)
Anxiety scores were normally distributed for all the subscales. Relative to Birmaher’s (1997) sample of typically developing youth with clinical anxiety, our sample of ASD youth reported higher mean scores for social anxiety and separation anxiety, similar levels of school anxiety, and lower levels of panic and generalized anxiety. This variability may reflect genuine differences in how anxiety manifests in ASD, as well as difficulties individuals with ASD experience in describing certain internal psychological states. Alternatively, elevated scores for social anxiety may reflect diagnostic overlap with core deficits of ASD, as social avoidance behaviors may stem from both fear of embarrassment and lack of social skills or motivation (Wood & Gadow, 2010). Overall, however, differences in reported anxiety severity were slight, mirroring previous research and suggesting that anxiety may be a distinct, co-occurring symptom of ASD and not a core feature (see Kerns & Kendall, 2012 for review).
4.3 Discriminant and convergent validity (Aim 3)
The SCARED demonstrated strong sensitivity and specificity for parent-reported anxiety symptoms, although discriminant validity for child-report in our sample fell below levels reported in Birmaher’s (1997) normative sample. Results of comparisons to gold-standard diagnostic interviews indicated that the SCARED may be a useful diagnostic tool for some anxiety disorders but not others. Children who met clinical criteria for separation anxiety on the ADIS-P or K-SADS also tended to meet clinical criteria on the SCARED-Parent and Child Versions. Children who met clinical criteria for social anxiety on the interview also tended to meet clinical criteria on the parent version of the SCARED, but not youth version of the SCARED. Results were not significant for GAD. Panic and school phobia were not evaluated, as no CSRs were not available for these diagnoses on the structured interview. As van Steensel and colleagues (2012) suggest in their investigation of the 71-item SCARED, adjustments to cutoff scores may be needed when applying the SCARED in clinical settings with youth with ASD. Future studies should investigate this issue.
Moderate associations were observed between severity scores on the ADIS-P and the GAD, separation, and social anxiety subscales of the SCARED. As in Birmaher’s (1999) sample, SCARED scores above 25 were associated with an anxiety disorder in youth with ASD. Overall, parent report on the SCARED was sensitive across all four diagnostic categories; however, parent report of GAD on the SCARED lacked specificity. For youth self-report, the SCARED appears to be a less sensitive measure, with symptoms of GAD and Social Anxiety potentially underreported. When determining diagnostic status in youth with ASD, it may be necessary to follow up on youth report via parent report of symptoms or via clinical interview, particularly when diagnosing GAD.
4.4 Sources of variability (Aim 4)
We observed similar between-group variability in anxiety symptoms as has been reported in non-ASD samples (Birmaher et al., 1999). Parent-reported social anxiety scores were higher for girls than for boys, consistent with the increased prevalence of social anxiety in typically developing girls (Wittchen, Stein, & Kessler, 1999). However, these observed gender differences should be interpreted with caution, given the small number of girls in our sample (N=8).
When anxiety symptoms were compared by age cohort, school-aged children in our sample reported higher levels of separation anxiety and social phobia than adolescents, while parents of adolescents reported more GAD symptoms than did parents of school-aged children. In general, these patterns are consistent with the developmental course of these diagnoses in the typically developing population (Grant et al., 2005; Kessler et al., 2005; Wittchen et al., 1999).
4.5 Limitations and future directions
Our study is the first to examine the psychometric properties of the 41-item version of the SCARED in a population with ASD seeking treatment for anxiety. However, the size and racial/ethnic homogeneity of the sample may limit the generalizability of findings. Further, the cross-sectional design precludes examination of predictive validity and test-retest reliability in the current investigation. Future studies would benefit from longitudinal examination of a larger, more diverse population to further measure reliability and validity of the SCARED in ASD. Longitudinal investigations may also provide important information regarding the developmental psychopathology of anxiety in ASD. In addition, including more girls in future samples may illuminate other potential gender differences in anxiety symptomology.
Another limitation was the use of the ADIS as the gold standard for anxiety diagnosis, although its reliability has not been established in ASD populations. It has, however, been applied in this population successfully by several investigators conducting treatment studies (Reaven et al., 2012a; Storch et al., 2012; Wood et al., 2009). Relatedly, only the parent version of the ADIS was administered in the current investigation; future studies may benefit from comparisons between children’s self-reported symptoms on the SCARED and their report via clinical interview. Finally, the modification to the SCARED instructions to report on symptoms within the last two weeks may have altered results slightly.
4.6 Conclusions and clinical significance
Establishing the validity of the SCARED as a diagnostic tool for youth with ASD represents an important step toward meeting the mental health needs of this population (Lecavalier et al., 2013). Anxiety disorders are particularly common in children with ASD, and contribute to significant morbidity through childhood, adolescence, and adulthood if unrecognized and untreated (Fergusson & Woodward, 2002; Messer & Beidel, 1994; Pine, Cohen, Gurley, Brook, & Ma, 1998; Simonoff et al., 2008). Accurate and timely assessment of anxiety symptoms is essential in receiving appropriate treatment and, ultimately, in mitigating the negative impact of comorbidity on children’s functioning and development. Gold-standard anxiety scales require significant clinician time and are unhelpful for screening in primary care settings or even in traditional outpatient mental health clinics. Increased use of the brief 41-item SCARED would be helpful in screening children with ASD and anxiety and referring them for treatment. Our study demonstrates the effectiveness of the SCARED in screening for various anxiety disorder types in youth with ASD, particularly social phobia and separation anxiety, with strong convergent validity with a gold standard clinical interview. More broadly, given the high rates of co-occurrence among anxiety disorders in this population (van Steensel et al., 2011) and the discrepancies between parent- and child-report on specific diagnoses (Blakeley-Smith et al., 2012), the SCARED—total score may provide a useful method of screening for clinical anxiety. The above factors, as well as the ease of use of the SCARED, support its use in youth with ASD in both clinical and research contexts.
Highlights.
We evaluate the psychometrics of an anxiety measure (SCARED) in youth with ASD.
Parent and child versions of the SCARED demonstrated a five-factor structure.
Internal reliability and score distributions were similar to typically developing samples.
The SCARED showed moderate convergent validity with a structured clinical interview.
Results support use of the SCARED as a valid assessment tool for youth with ASD.
Acknowledgments
The authors gratefully acknowledge the parents and children who participated in our studies, as well as Katy Ridge and Mary Hetrick. This research was supported by grants awarded to JFK Partners, the University Center for Excellence in Developmental Disabilities at the University Colorado School of Medicine from the U.S. Department of Health and Human Services, through the Administration on Developmental Disabilities Grant no. 90DD0561. Additional support came from the Organization for Autism Research, Cure Autism Now, and Autism Speaks. Funding support also came from HRSA R40MC15593-01-00 (09/01/09-02/28/12).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Initially, we chose the K-SADS as our gold standard measure of psychopathology in youth; subsequent experience using the tool with this population led us to switch to the ADIS.
Given that the SCARED subscales likely overlap, non-orthogonal rotation would also be appropriate; however, orthogonal rotation was used in the present analyses for ease of comparison to previous studies.
Discriminant validity of the SCARED for a subset of this sample (N=31 adolescents) is also reported in a companion paper focused on self-report of anxiety in teens with ASD (Blakeley-Smith, Reaven, Stern, & Hepburn, under review).
References
- Achenbach T, Edelbrock C. Child Behavior Checklist: CBCL: T. Achenbach, University of Vermont; 1980. [Google Scholar]
- Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E. A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39(1):1–11. doi: 10.1007/s10803-008-0593-3. [DOI] [PubMed] [Google Scholar]
- Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Autism screening questionnaire: diagnostic validity. The British Journal of Psychiatry. 1999;175(5):444–451. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Blakeley-Smith A, Reaven J, Ridge K, Hepburn S. Parent–child agreement of anxiety symptoms in youth with autism spectrum disorders. Research in Autism Spectrum Disorders. 2012;6(2):707–716. [Google Scholar]
- Blakeley-Smith A, Reaven J, Stern J, Hepburn S. The use of parent and teen report: Assessing symptoms of anxiety in high functioning adolescents on the autism spectrum (under review) [Google Scholar]
- Bodden DH, Bögels SM, Muris P. The diagnostic utility of the screen for child anxiety related emotional disorders-71 (SCARED-71) Behaviour Research and Therapy. 2009;47(5):418–425. doi: 10.1016/j.brat.2009.01.015. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment. 2009;21:256–271. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler S, Charman T, Baird G, Simonoff E, Loucas T, Meldrum D, Pickles A. Validation of the social communication questionnaire in a population cohort of children with autism spectrum disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(10):1324–1332. doi: 10.1097/chi.0b013e31812f7d8d. [DOI] [PubMed] [Google Scholar]
- Essau CA, Muris P, Ederer EM. Reliability and validity of the Spence Children’s Anxiety Scale and the Screen for Child Anxiety Related Emotional Disorders in German children. Journal of Behavior Therapy and Experimental Psychiatry. 2002;33(1):1–18. doi: 10.1016/s0005-7916(02)00005-8. [DOI] [PubMed] [Google Scholar]
- Evans DW, Canavera K, Kleinpeter FL, Maccubbin E, Taga K. The fears, phobias and anxieties of children with autism spectrum disorders and Down syndrome: Comparisons with developmentally and chronologically age matched children. Child Psychiatry and Human Development. 2005;36:3–26. doi: 10.1007/s10578-004-3619-x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of general psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, June Ruan W, Goldstein RB, Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2005;35:1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Hale WW, Crocetti E, Raaijmakers QA, Meeus WH. A meta-analysis of the cross-cultural psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED) Journal of Child Psychology and Psychiatry. 2011;52(1):80–90. doi: 10.1111/j.1469-7610.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P, Ryan N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kerns CM, Kendall PC. The presentation and classification of anxiety in autism spectrum disorder. Clinical Psychology: Science and Practice. 2012;19:323–347. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Aman MG, Scahill L, McDougle CJ, McCracken JT, Vitiello B, Kau AS. Validity of the Autism Diagnostic Interview-Revised. American Journal on Mental Retardation. 2006;111(3):199–215. doi: 10.1352/0895-8017(2006)111[199:VOTADI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Wood JJ, Halladay AK, Jones NE, Aman MG, Cook EH, Scahill L. Measuring Anxiety as a Treatment Endpoint in Youth with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders. 2013:1–16. doi: 10.1007/s10803-013-1974-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, Lainhart JE. Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36(7):849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule-WPS edition. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- Lyneham HJ, Rapee RM. Agreement between telephone and in-person delivery of a structured interview for anxiety disorders in children. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(3):274–282. doi: 10.1097/00004583-200503000-00012. [DOI] [PubMed] [Google Scholar]
- March JS, Sullivan K, Parker J. Test-retest reliability of the Multidimensional Anxiety Scale for Children. Journal of Anxiety Disorders. 1999;13(4):349–358. doi: 10.1016/s0887-6185(99)00009-2. [DOI] [PubMed] [Google Scholar]
- Mazzone L, Ruta L, Reale L. Psychiatric comorbidities in Asperger syndrome and high functioning autism: diagnostic challenges. Annals of General Psychiatry. 2012;11(1):16. doi: 10.1186/1744-859X-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer SC, Beidel DC. Psychosocial correlates of childhood anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33(7):975–983. doi: 10.1097/00004583-199409000-00007. [DOI] [PubMed] [Google Scholar]
- Monga S, Birmaher B, Chiappetta L, Brent D, Kaufman J, Bridge J, Cully M. Screen for child anxiety-related emotional disorders (SCARED): Convergent and divergent validity. Depression and Anxiety. 2000;12(2):85–91. doi: 10.1002/1520-6394(2000)12:2<85::AID-DA4>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Muris P, Loxton H, Neumann A, du Plessis M, King N, Ollendick T. DSM-defined anxiety disorders symptoms in South African youths: Their assessment and relationship with perceived parental rearing behaviors. Behaviour Research and Therapy. 2006;44:883–896. doi: 10.1016/j.brat.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Mayer B, van Brakel A, Thissen S, Moulaert V, Gadet B. The Screen for Child Anxiety Related Emotional Disorders (SCARED) and traditional childhood anxiety measures. Journal of Behavior Therapy and Experimental Psychiatry. 1998a;29:327–339. doi: 10.1016/s0005-7916(98)00023-8. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Schmidt H, Mayer B. The revised version of the Screen for Child Anxiety Related Emotional Disorders (SCARED-R): Factor structure in normal children. Personality and Individual Differences. 1999a;26:99–112. [Google Scholar]
- Muris P, Schmidt H, Engelbrecht P, Perold M. DSM-IV-defined anxiety disorder symptoms in South African children. Journal of the American Academy of Child and Adolescent Psychiatry. 2002b;41:1360–1368. doi: 10.1097/00004583-200211000-00018. [DOI] [PubMed] [Google Scholar]
- Ogliari A, Citterio A, Zanoni A, Fagnani C, Patriarca V, Cirrincione R, Stazi MA, Battaglia M. Genetic and environmental influences on anxiety dimensions in Italian twins evaluated with the SCARED questionnaire. Journal of Anxiety Disorders. 2006;20:760–777. doi: 10.1016/j.janxdis.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55(1):56. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K, Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. Journal of Child Psychology and Psychiatry. 2012;53(4):410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. Revised Children’s Manifest Anxiety Scale. Los Angeles, CA: Western Psychological Services; 1985. [Google Scholar]
- Russell E, Sofronoff K. Anxiety and social worries in children with Asperger syndrome. Australian and New Zealand Journal of Psychiatry. 2005;39(7):633–638. doi: 10.1080/j.1440-1614.2005.01637.x. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Parent Version. San Antonio, TX: Graywing; 1996. [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Flannery-Schroeder EC, Kendall PC. A psychometric evaluation of the parent report form of the State–Trait Anxiety Inventory for Children–Trait Version. Journal of Anxiety Disorders. 2002;17:427–446. doi: 10.1016/s0887-6185(02)00223-2. [DOI] [PubMed] [Google Scholar]
- Spence SH, Barrett PM, Turner CM. Psychometric properties of the Spence Children’s Anxiety Scale with young adolescents. Journal of Anxiety Disorders. 2003;17(6):605–625. doi: 10.1016/s0887-6185(02)00236-0. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. The State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press Inc; 1970. [Google Scholar]
- Storch EA, Ehrenreich May J, Wood JJ, Jones AM, De Nadai AS, Lewin AB, Murphy TK. Multiple informant agreement on the anxiety disorders interview schedule in youth with autism spectrum disorders. Journal of Child and Adolescent Psychopharmacology. 2012;22:292–299. doi: 10.1089/cap.2011.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su L, Wang K, Fan F, Su Y, Gao X. Reliability and validity of the screen for child anxiety related emotional disorders (SCARED) in Chinese children. Journal of Anxiety Disorders. 2008;22(4):612–621. doi: 10.1016/j.janxdis.2007.05.011. [DOI] [PubMed] [Google Scholar]
- van Steensel FJ, Deutschman AA, Bögels SM. Examining the Screen for Child Anxiety-Related Emotional Disorder-71 as an assessment tool for anxiety in children with high-functioning autism spectrum disorders. Autism. 2012 doi: 10.1177/1362361312455875. 2012. [DOI] [PubMed] [Google Scholar]
- Weschler D. Weschler preschool and primary scale of intelligence. San Antonio, TX: Psychological Corporation; 2002. [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU, Stein MB, Kessler RC. Social fears and social phobia in a community sample of adolescents and young adults: Prevalence, risk factors and co-morbidity. Psychological Medicine. 1999;29(2):309–323. doi: 10.1017/s0033291798008174. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Gadow KD. Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology: Science and Practice. 2010;17:281–292. [Google Scholar]
- Wren FJ, Berg EA, Heiden LA, Kinnamon CJ, Ohlson LA, Bridge JA, Bernal MP. Childhood anxiety in a diverse primary care population: parent-child reports, ethnicity and SCARED factor structure. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(3):332–340. doi: 10.1097/chi.0b013e31802f1267. [DOI] [PubMed] [Google Scholar]
- Wren FJ, Bridge JA, Birmaher B. Screening for childhood anxiety symptoms in primary care: integrating child and parent reports. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(11):1364–1371. doi: 10.1097/01.chi.0000138350.60487.d3. [DOI] [PubMed] [Google Scholar]


