Abstract
Background
Mindfulness-Based Stress Reduction (MBSR) has the potential to reduce worry and improve cognitive functioning.
Objectives
In this treatment development project, we examined MBSR in older adults with worry symptoms and co-occurring cognitive dysfunction. We examined (1) acceptability of MBSR, (2) whether MBSR needs to be lengthened providing more repetition, (3) MBSR's benefits for worry reduction and cognitive improvements, and (4) continued use of MBSR techniques during follow-up.
Method
Two sites (St. Louis and San Diego) enrolled individuals aged 65+ with significant anxiety-related distress plus subjective cognitive dysfunction, into traditional 8-session MBSR groups and 12-session groups that had the same content but more repetition of topics and techniques. We examined measures of mindfulness, worry, and a neuropsychological battery focused on memory and executive function before and after the MBSR program, and we followed up participants for 6 months after the completion of MBSR regarding their continued use of its techniques.
Results
Participants (N=34) showed improvements in worry severity, increases in mindfulness, and improvements in memory as measured by paragraph learning and recall after a delay, all with a large effect size. Most participants continued to use MBSR techniques for six months post-instruction and found them helpful in stressful situations. There was no evidence that the extended 12-week MBSR produced superior cognitive or clinical outcomes, greater satisfaction, or greater continuation of MBSR techniques than 8-week MBSR.
Conclusions
These preliminary findings are promising for the further testing and use of MBSR in older adults suffering from clinical worry symptoms and co-occurring cognitive dysfunction. These are common problems in a broad range of older adults, many of whom have anxiety and mood disorders; therefore, stress reduction intervention for them may have great public health value.
Keywords: anxiety, elderly, mindfulness, yoga, meditation, stress, memory
Introduction
Excessive worry is common in older adults and, with the aging of the world population, will be an increasing source of human and economic burden. Excessive worry often co-occurs with cognitive impairment, which confers greater disability, and poor quality of life (Mackin et al., 2011, Beaudreau and O'Hara, 2008, Alexopoulos et al., 2005, Butters et al., 2000, Potter et al., 2012) and is a treatment-resistance factor for late-life depression and anxiety disorders (Caudle et al., 2007, Alexopoulos et al., 2005, Sneed et al., 2010). Cognitive dysfunction, referring to self-reported cognitive complaints and/or measurable impairments that fall below the level of dementia, is increasingly understood to be clinically significant (Sinoff and Werner, 2003, Begum et al., 2012). While some cognitive dysfunction in this setting is due to neurodegenerative disease such as cerebrovascular disease or Alzheimer's disease, data suggest that excess worry itself may cause cognitive dysfunction in older adults, with an effect size in observational studies equal to or greater than other negative affects such as depression (Wilson et al., 2011, Pietrzak et al., 2012, Rosenberg et al., 2012, Andreescu et al., In Press, Palmer et al., 2007). Although the causality and pathways of this relationship remain uncertain (Beaudreau et al., 2013), the finding raises the question of whether cognitive dysfunction may be reversible with effective intervention for worry symptoms (Lenze and Wetherell, 2011).
Mind-body techniques have appeal as treatment for late-life anxiety disorders and depression because of their potential to reduce worry and ameliorate cognitive dysfunction in older adults (Lavretsky et al., 2013). Mindfulness meditation emphasizes focused, nonjudgmental awareness of present moment experiences as an alternative to dwelling on the future (e.g., worrying) (Bishop, 2002). Mindfulness-Based Stress Reduction (MBSR) is a protocolized group-based instruction that introduces the concept of mindfulness and develops it through the practice of techniques such as informal mindfulness, yoga, mindful breathing, and various types of meditation. There are reasons to think that MBSR may improve cognitive dysfunction in older adults: MBSR not only teaches directed attention, it also reduces anxiety (Kabat-Zinn et al., 1992, Miller et al., 1995, Goldin and Gross) and depression (Deyo et al., 2009, Matousek and Dobkin, 2010, Lengacher et al., 2010). Several studies have demonstrated a rumination and worry-reducing effect of MBSR (Shapiro et al., 2008, Jain et al., 2007, Deyo et al., 2009). On a pragmatic level, MBSR is appealing because it is low-cost and delivers lasting benefits (Bedard et al., 2005, Carlson et al., 2007, Grossman et al., 2007). MBSR is practiced in most major cities and in over 250 clinics, hospitals, and HMOs in the U.S. and abroad (Gross et al., 2009). Mindfulness meditation programs have proliferated (Barnes et al., 2008, Nahin et al., 2009, Nahin et al., 2007, Kabat-Zinn et al., 1992) and have seen an explosion of interest and acceptability in older adults (Nguyen et al., Ryder et al., 2008, Loera et al., 2007, Meeks et al., 2007, Zhang et al., 2007). Thus, there appears to be considerable promise to use MBSR for anxious and depressed older adults who also suffer from cognitive dysfunction.
We carried out a treatment development project to answer the following questions: is MBSR acceptable and feasible for study in older individuals with anxiety and mood disorders and cognitive dysfunction? In this population, does MBSR needed to be lengthened with more repetition provided, as has been done with other interventions for late-life anxiety (Mohlman et al., 2003, Stanley et al., 2009, Wetherell et al., 2009), in order to provide clinical and cognitive benefits? And, do older adults continue to use MBSR techniques after the completion of the instruction?
Methods
This was a treatment development study funded by the National Center for Complementary and Alternative Medicine (NCCAM). The focus of the project was to assess the feasibility of MBSR for older adults with anxiety disorders and/or depression plus cognitive dysfunction. The project was carried out at Washington University in St. Louis and University of California, San Diego from September 2011–August 2012. Both sites' institutional review boards approved the project, and all participants provided informed consent prior to any research participation.
Sample
Participants were aged 65 or older and had clinically significant anxiety-related distress as defined by a screening score of ≥22 on the Penn State Worry Questionnaire-Abbreviated (Stanley et al., 2003), an 8-item measure of worry severity that has been validated in older adults (range 8–40; average score in a healthy community elderly person is 15) (Crittendon and Hopko, 2006, Hopko et al., 2003). All participants also had cognitive dysfunction defined by reporting having problems in response to a question from the screening instrument, “Have you noticed that you have any trouble with your memory or concentration?”, similar to prior research on anxiety and subjective cognitive complaints (Sinoff and Werner, 2003). We excluded individuals with dementia based on known diagnosis or meeting criteria during the screening evaluation; individuals were not evaluated to determine whether they met criteria for mild cognitive impairment. Exclusion criteria were: unable to provide informed consent, diagnosis of dementia, lifetime psychotic disorder, active substance abuse, unstable medical condition, or any condition or impairment likely to interfere with the ability to participate in MBSR. Participants were recruited from the community using advertisements, from outpatient psychiatry clinics, and from lists of participants of previous studies of older adults with anxiety disorders.
Intervention
Our MBSR program was based on the program developed by Jon Kabat-Zinn, Ph.D.'s group at the Center for Mindfulness in Medicine, Health Care, and Society at the University of Massachusetts. Content includes instruction in mindfulness meditation practices, gentle yoga and exercises to enhance mindfulness in everyday life. Participants are given daily home assignments along with CDs of MBSR activities for the participant to practice with at home, using a Mindfulness-Based Stress Reduction Workbook (Stahl and Goldstein, 2010) as course material. MBSR was taught by three instructors, two in St. Louis and one in San Diego, who had formal training in the MBSR model and regularly practiced and taught meditation techniques. Fidelity to the MBSR model was attained by all instructors viewing session tapes generated by the UCSD MBSR leader/supervisor (Dr. Hickman) and participation in weekly supervision calls. Fidelity was confirmed by the supervisor's review of each instructor's videotaped sessions against the operational criteria as laid out in the MBSR manual.
Thirty-four participants received MBSR in four groups across the two sites. Although MBSR is usually conducted as 8 weekly 2.5-hour classes plus one day-long retreat, we modified the protocol by extending the duration to 12 classes, reducing the day-long retreat to 2.5 hours, and repeating all material in at least three sessions. We tested both the modified protocol and standard MBSR. The MBSR groups were carried out as follows: first, an 8-session (traditional MBSR) group was conducted in St. Louis and a 12-session (modified MBSR) group was conducted in San Diego; then, the sites were reversed and a 12-session group was conducted in St. Louis while an 8-session group was conducted in San Diego.
Measures
Cognitive
We administered a cognitive battery before and after the MBSR course. Our focus was on the domains of memory and executive function since impairments in these areas most impaired in older adults with Generalized Anxiety Disorder and are thought to be related to stress-induced dysfunction (Butters et al., 2011). Since the purpose of this project was also to examine the feasibility of various measures of cognitive function for this context, some of the measures were changed between the first two groups and the last two groups. In the first two groups we measured verbal memory with the immediate and delayed list and paragraph recall tests of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). For the last two groups we switched to the California Verbal Learning Test (CVLT) for list recall and two paragraphs from a set of paragraph recall tests previously validated (Newcomer et al., 1994). We made this change because these measures are thought to be less susceptible to ceiling effects. Our variables of interest from these scales were the total number of words (in either the list or the paragraph) accurately recalled. To measure executive function, we used the Delis-Kaplan Executive Function Scale (DKEFS) verbal fluency test (“FAS” task), in which the key variable was number of correct words. We also examined some neuropsychological variables in only the first two groups: the RBANS digit span test (which was discontinued due to concerns about ceiling effects) and DKEFS color-word interference test (which was discontinued in favor of a computerized version; this however showed poor feasibility with the participants and no data are available).
Clinical
To measure improvements in anxiety-related distress, participants provided self-report assessments of worry using the PSWQ-A at baseline, midway through MBSR course, post-MBSR, and 3 and 6 months later. To measure changes in mindfulness from pre to post-MBSR, in the first two groups we used the Mindful Attention Awareness Scale (MAAS) (Brown and Ryan, 2003), whereas in the last two groups we used the Cognitive Affective Mindfulness Scale-Revised (CAMS-R) (Feldman et al., 2007). We made this change because the CAMS-R has shown sensitivity to change over the course of mindfulness-based therapy (Hayes and Feldman, 2004), and because it was specifically created to be understandable to participants with little knowledge or insight about mindfulness whereas the MAAS appeared to require some insight into one's level of mindfulness to accurately answer. To improve the CAMS-R understandability in this population, we modified its administration by creating flash cards for each question, and clarifying the response anchors. This modification is available from the first author on request. Additionally, although we did not require a psychiatric diagnosis for inclusion, all participants were characterized for current and lifetime disorders with the Structured Clinical Interview for DSM-IV Axis I disorders (First et al., 1997); diagnoses are listed in the results.
MBSR satisfaction and technique use during and post MBSR
An important focus for interventions research is to learn the perspectives of people who have received an intervention (Dakin and Arean, 2013); accordingly, an additional aim of this project was to examine acceptability of MBSR, including satisfaction with the instruction during the course of MBSR, and continued use of the techniques after the course was completed. Therefore, we carried out surveys at mid-point and then three and six months after the completion of MBSR in all groups. At the mid-point survey we queried participants about their satisfaction with the services received (Table 2), and at the three and six-month follow-ups we queried them about their frequency of use of techniques and whether they found them helpful in times of stress (Table 4).
Table 2.
Satisfaction with MBSR
| 8-session MBSR (n=15) | 12-session MBSR (n=18) | |
|---|---|---|
|
| ||
| How would you rate the service you received overall? | ||
| Very poor/Poor | 1 (7%) | 0 (0%) |
| Fair | 0 (0%) | 2 (11%) |
| Good | 3 (20%) | 3 (17%) |
| Very good | 11 (73%) | 13 (72%) |
|
| ||
| How satisfied were you with the style of instructions? | ||
| Very or Somewhat unsatisfied | 0 (0%) | 0 (0%) |
| Neutral | 0 (0%) | 2 (11%) |
| Somewhat satisfied | 2 (13%) | 2 (2%) |
| Very satisfied | 13 (87%) | 14 (78%) |
|
| ||
| Do you think this class has helped reduce your concerns? | ||
| No | 1 (7%) | 2 (11%) |
| Yes | 13 (93%) | 16 (89%) |
|
| ||
| Has this class helped improve your worry? | ||
| No | 1 (7%) | 4 (22%) |
| Yes | 13 (93%) | 14 (78%) |
Note: there were no significant differences between 8- and 12-week MBSR participants in any of the above responses.
Table 4.
Use of MBSR techniques post-MBSR class completion
| Over the past 3 months, how often did you engage in… | 3 month follow-up (n=25) | 6 month follow-up (n=29) |
|---|---|---|
|
| ||
| Formal meditation? | ||
| Never | 24% | 41% |
| A few times per month | 40% | 38% |
| A few times per week | 36% | 14% |
| Every day | 0% | 7% |
|
| ||
| Mindful eating? | ||
| Never | 32% | 41% |
| A few times per month | 44% | 38% |
| A few times per week | 16% | 14% |
| Every day | 8% | 7% |
|
| ||
| Yoga? | ||
| Never | 44% | 52% |
| A few times per month | 28% | 28% |
| A few times per week | 28% | 21% |
| Every day | 0% | 0% |
|
| ||
| Walking meditation? | ||
| Never | 44% | 66% |
| A few times per month | 44% | 21% |
| A few times per week | 12% | 14% |
| Every day | 0% | 0% |
|
| ||
| Body scan? | ||
| Never | 40% | 52% |
| A few times per month | 36% | 38% |
| A few times per week | 20% | 3% |
| Every day | 4% | 7% |
|
| ||
| Loving kindness meditation? | ||
| Never | 44% | 55% |
| A few times per month | 40% | 34% |
| A few times per week | 12% | 7% |
| Every day | 4% | 3% |
|
| ||
| Mindful breathing? | ||
| Never | 8% | 17% |
| A few times per month | 36% | 41% |
| A few times per week | 44% | 31% |
| Every day | 12% | 10% |
|
| ||
| Informal mindfulness? | ||
| Never | 8% | 17% |
| A few times per month | 36% | 34% |
| A few times per week | 40% | 31% |
| Every day | 16% | 17% |
|
| ||
| What practice did you prefer? | ||
| Meditation | 40% | 28% |
| Mindful breathing | 24% | 38% |
| Body scan | 24% | 24% |
| Yoga | 32% | 7% |
| Everyday mindfulness | 0% | 10% |
| Mindful eating | 8% | 0% |
|
| ||
| What practice did you dislike? | ||
| Body scan | 12% | 14% |
| Yoga | 8% | 14% |
| Mindful eating | 4% | 10% |
| Loving kindness | 4% | 3% |
| Walking meditation | 4% | 3% |
| Sitting meditation | 4% | 0% |
|
| ||
| What technique did you use when experiencing stress?* | ||
| Mindful breathing | 48% | 34% |
| Informal mindfulness | 8% | 14% |
| Meditation (including sitting, walking) | 28% | 14% |
| Yoga | 8% | 3% |
| Loving kindness | 12% | 0% |
| Body scan | 4% | 0% |
Note: the survey also asked whether the technique was helpful for stress reduction; all (100%) participants responded yes to this question.
Statistical analysis
All statistical analyses were conducted using SAS PROC MIXED, which employs a likelihood-based estimation method. PROC MIXED allows for covariate adjustment in a time course analysis (Wolfinger and Chang). Our analyses assessed whether the change over time for an outcome variable was statistically significant. Because the cognitive assessments for the list and paragraph variables were changed during the course of the study (i.e., from the RBANS list and story recall to the CVLT for list recall and Paragraph Recall Test for story recall), data from measures of the same construct (e.g., immediate list recall) were appended in order to achieve more statistical power by examining the entire sample of participants who completed pre and post MBSR cognitive testing. To create this appended data set, Z-scores ((raw data point - mean)/standard deviation) were computed for measures (e.g., RBANS and CVLT immediate list recall) for each individual. All effect sizes reported are pre-post MBSR changes.
Results
From September 2011–April 2012, we screened 89 individuals (56 in St. Louis, 33 in San Diego); 34 met eligibility criteria and entered the study (17 in St. Louis, 17 in San Diego). The main reason for non-participation was inability to comply with the timing (i.e., scheduling demands) of the group-based intervention. Of 34 participants, 32 (94%) completed MBSR instruction and provided post-treatment data. Two participants dropped out prior to finishing MBSR, another 3 refused follow-up neuropsychological testing and 3- and 6-month follow-ups, and one additional participant refused just the 3- and 6-month follow-ups. There were no site differences in dropout rate (one from each site). Table 1 shows demographic and baseline data on all 34 participants, broken down into 8-session MBSR participants (n=16) and 12-session MBSR participants (n=18). Current psychiatric diagnoses of the participants were GAD, n=12, anxiety disorder not otherwise specified, n=8, major depressive episode, n=7, panic disorder, n=3, dysthymic disorder, n=3,depressive disorder not otherwise specified (including minor depression), n=3, specific phobia, n=2, social phobia, n=2, obsessive-compulsive disorder, n=1. Five participants had no lifetime disorder, while the remainder had a lifetime history of a depressive or anxiety disorder. This heterogeneity likely reflects the common occurrence of high worry symptoms across mood and affective disorders in older adults (Golden et al., 2011).
Table 1.
Baseline characteristics of participants
| Variable | 8-week MBSR participants (n=16) Mean ± SD | 12-week MBSR participants (n=18) Mean ± SD | p |
|---|---|---|---|
| Age | 70.9 (4.5) | 70.7 (4.9) | 0.926 |
| Gender | 11 (69%) Female 5 (31%) Male |
14 (78%) Female 4 (22%) Male |
0.703 |
| Race | 13 (81%) White 3 (19%) Black |
16 (88%) White 1 (6%) Black 1 (6%) Hispanic |
0.323 |
| Years of Education | 14.88 (2.9) | 14.94 (2.5) | 0.940 |
| Total medical burden (Cumulative Illness Rating Scale for Geriatrics) | 10.1 (3.6) | 9.6 (3.6) | 0.716 |
Feasibility outcomes
Class attendance (inclusive of the retreat) was adequate in both 8- and 12-session MBSR: 79% of 8-session classes were attended, vs. 87% of 12-session MBSR. Satisfaction ratings were generally high in both 8- and 12-session MBSR, as seen in Table 2. The only concern, reported to us by several participants, was that some of the yoga was overly strenuous as was the all-day retreat. Therefore, the only modifications we made were (1) reducing the intensity of yoga based on participants' reports of minor muscle strains from some of the more difficult postures; (2) reducing the length of the retreat from all day to one-half day.
Cognitive outcomes
Table 3 shows the cognitive changes from pre to post MBSR. All cognitive measures showed at least a trend towards improvement; four out of the seven measures showed a highly significant improvement. The measure with the largest improvement was the Paragraph Recall task, in which both immediate and delayed recall improved with large effect sizes. The 8- and 12-session MBSR results were similar for these measures: for example, for delayed story recall, Cohen's d was 0.61 for the 8-week and 0.86 for the 12-week class.
Table 3.
Changes in neuropsychological test scores from baseline to post-treatment with MBSR.
| Measure | Baseline mean or z-score (SE) | Post-MBSR mean or z-score (SE) | Cohen's d (95% CI) | Analysis | |
|---|---|---|---|---|---|
| F (df) | p | ||||
| List learning, number of words recalled | −0.03 (.2) | 0.16 (0.17) | 0.19 (−0.33 to 0.70) | 2.9 (1,28) | 0.10 |
| List delayed recall, number of words recalled | −0.09 (.2) | 0.17 (0.18) | 0.26 (−0.26 to 0.77) | 6.17 (1,28) | 0.019 |
| Paragraph immediate recall, number of words recalled | −0.26 (0.17) | 0.47 (0.15) | 0.83 (.28 to 1.35) | 27.2 (1, 28) | <0.001 |
| Paragraph delayed recall, number of words recalled | −0.06 (0.2) | 0.65 (0.16) | 0.75 (0.21 to 1.27) | 25.0 (1,28) | <0.001 |
| Verbal fluency, number of correct words named | 35.1 (2.1) | 37.3 (2.0) | 0.20 (−0.32 to 0.71) | 3.9 (1,28) | 0.04 |
| Color-word interference, time (seconds) | 84.3 (9.9) | 71.7 (6.2) | 0.39 (−0.31 to 1.08) | 9.1 (1,15) | 0.009 |
| Digit span test, score (higher score = more digits forward correctly repeated) | 9.1 (2.7) | 10.3 (2.2) | 0.46 (−0.24 to 1.16) | 4.4 (1,15) | 0.053 |
Clinical outcomes
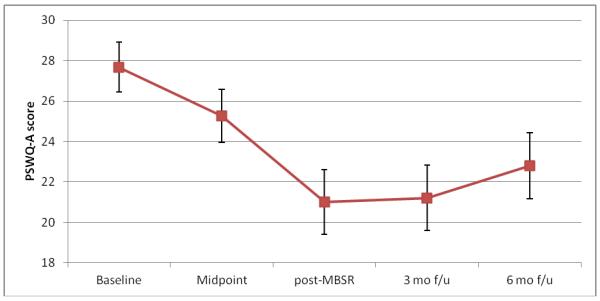
Figure 1 shows the improvements in worry severity as measured by the Penn State Worry Questionnaire, from pre to post MBSR and at 3 and 6 month follow-up. As the figure shows, worry severity was reduced, with a large effect size. The mean post-MBSR score of 21 is below the threshold of 22 for current Generalized Anxiety Disorder in older adults (Stanley et al., 2003) but above the mean score in healthy older adults (15) (Crittendon and Hopko, 2006). This suggests that the average result was clinically significant reduction in worry severity similar to findings in older adults with Generalized Anxiety Disorder treated with antidepressant medication and cognitive-behavioral therapy (Lenze et al., 2009, Stanley et al., 2009). There was no advantage for 12-week MBSR: Cohen's d for worry reduction was 1.47 for 8-week and 0.48 for 12-week. The improvement was sustained during the first three months of follow-up period, as shown in Figure 1, with the possible recurrence of worry symptoms in some participants by 6 months.
Figure 1. Changes in worry severity with MBSR, measured by the Penn State Worry Questionnaire-Abbreviated (PSWQ-A).
From baseline to post-treatment, mean PSWQ scores dropped from 27.8 to 21.0 (n=31), with Cohen's d =0.86 (95% confidence interval =0.33– 1.37), Proc Mixed Type 3 Test of Fixed Effects F(df 1, 30) = 20.6, p<0.001. Sample sizes by time point are 34, 33, 31, 25, and 29.
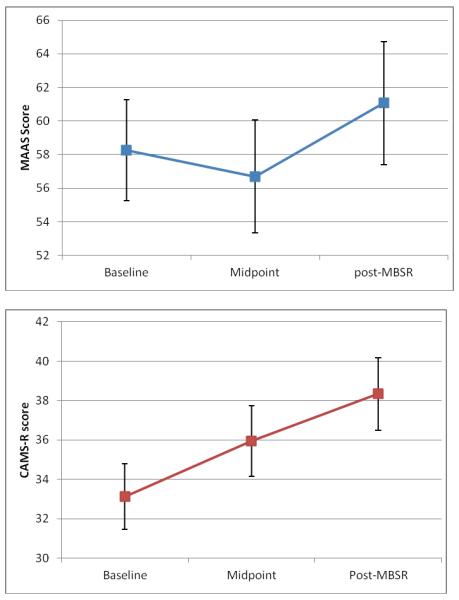
Figure 2 shows change in mindfulness. For the first two groups, we used the MAAS and, because of low effect size of change for the MAAS (d=0.22) switched to the CAMS-R in the second two groups. As the figure shows, there was a large effect size of increase in mindfulness with the CAMS-R (d=0.76). Increase in self-reported mindfulness over time was statistically significant for CAMS-R with PROC MIXED over the 3 time points (p= 0.02).
Figure 2. Changes in mindfulness during MBSR.
The Mindfulness Attention and Awareness Scale (MAAS), used in the first two groups receiving MBSR showed showed a small increase with MBSR (Cohen's d for baseline to post = 0.22 [95% CI −0.48 – +0.91, p=0.18, n=16]), whereas the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R), used in the second two groups, showed a large increase (d=0.76 [95% CI= 0 – 1.48, p=<0.001, n=15]. P-values are from PROC MIXED over the three time points.
Use of MBSR practices
At 3 and 6-month follow-up, the vast majority of participants in both 8- and 12-week MBSR groups reported continuing at least some practices, as shown in Table 4. The two techniques that participants most commonly reported continuing to use were mindful breathing and informal mindfulness. These techniques were used by both 8-week and 12-week MBSR participants; the only difference (at p<0.05 significance) was that more 8-week participants reporting using informal mindfulness (Wilcoxon test, p=0.03) at 3 months, and there were no differences at 6 months; for this reason, 8- and 12-week data were merged. Table 4 also shows participants' preferences for (and against) specific techniques and that substantial numbers of participants reported the successful use of MBSR techniques, particularly mindful breathing, during episodes of increased stress.
Discussion
We report here the first results of testing MBSR for older adults with high levels of worry symptoms and cooccurring cognitive dysfunction. Given the enormous human and societal burden of these late-life illnesses, it is imperative to have acceptable, cost-effective, and efficacious treatments that improve both symptoms and cognitive function. Chiefly, we found that MBSR was acceptable in this population. Individuals in this study showed improvements in worry severity, memory, and executive function, and most continued use of the techniques after the completion of the study. Therefore, our main finding is that MBSR is promising for further study as an intervention in this older adult population. Given its relative low cost, paucity of risk, and already wide availability, if MBSR can be shown in further research to improve worry symptoms and co-occurring cognitive dysfunction, it could be rapidly disseminated as a treatment option potentially across a range of mood and affective disorders (Golden et al., 2011). Further, our iterative treatment development project points the way for which methods – population characteristics, cognitive tests, clinical measures, and measures of mindfulness – could be used in such research.
Regarding feasibility and efficacy of MBSR, we examined the effects of extending MBSR and adding more repetition. This was not an RCT per se, but approximated one in its head-to-head comparison design. There was no evidence that 12-session MBSR, with its greater repetition of information and techniques was more acceptable, produced better outcomes (in terms of worry reduction or cognitive improvement), or yielded greater long-term use of MBSR techniques. We conclude that MBSR is optimal for older adults in its 8-session form already available throughout the U.S. and abroad (Gross et al., 2009), with no additional benefit from extending it. The only modifications we made were reducing the intensity of yoga and reducing the length of the retreat from all day to one-half day.
Clinical and neuropsychological improvements suggest that both worry severity and memory improve, with a large effect size, consistent with others' conclusions about the relationships between anxiety, subjective complaints, and cognitive impairment (Wilkes et al., 2013). These findings should be considered preliminary, as this was a treatment development study with a relatively small sample size which was predominantly white, female, and educated, and there was no control group (i.e., clinical improvements could represent expectancy or regression to the mean, while cognitive improvements could reflect practice effects). Future research should demonstrate efficacy of MBSR in a larger, randomized trial with patients diagnosed with anxiety disorders or depression (although it should be noted that 85.3% of the present sample had a current or past anxiety disorder or depressive episode) and with an active control group (MacCoon et al., 2012). Research should also examine the mechanisms by which MBSR may result in cognitive improvement and ideally whether these are similar to mechanisms by which other treatments (SSRIs, cognitive behavioral therapy) have provided cognitive benefits in some older adults with anxiety disorders (Mohlman and Gorman, 2005, Butters et al., 2011). There are several potential mechanisms, including the direct effects of attention training (i.e., MBSR as a type of cognitive training) and indirect effects through reducing worry and other emotional distress and its downstream biological manifestations (Brown et al., 2012, Creswell et al., 2012, Gallegos et al., 2013). Of note, a recent report in older adults showed improvements in neuropsychological function (measured with the Trail Making Test) with MBSR (Moynihan et al., 2013), agreeing with our preliminary conclusion that MBSR could have pro-cognitive effects.
Using the CAMS-R, we were able to demonstrate significant increases in mindfulness, with a large effect size. This is important because increased mindfulness is postulated to be the key active ingredient of MBSR. Further research would need to determine the extent to which clinical and cognitive improvements are mediated, or accounted for, by increases in mindfulness. In contrast, we could not demonstrate changes in mindfulness with the MAAS. These data suggest that the CAMS-R is better equipped to measure changes in mindfulness in an older adult population, perhaps because it was specifically designed for ease of understanding (Feldman et al., 2007) and perhaps because of our additional modifications to improve understanding of its items (see appendix). This conclusion is limited by the fact that we did not do a formal psychometric evaluation of mindfulness measures in this population; conceivably (though unlikely), the lack of change in the MAAS could mean that participants in the first two groups did not have an increase in mindfulness, and the MAAS accurately showed this lack of change. Other measures, such as the Five-Factor Mindfulness Questionnaire (Baer et al., 2006) should be considered as well, so that the various parts of the construct of mindfulness (e.g., observing, describing, acting with awareness, non-judging of inner experience, and nonreactivity to inner experience) can be examined with respect to changes with mindfulness instruction. In this regard, our conclusion is that, for studies of mindfulness interventions (particularly in new populations), it should not be assumed that existing validated measures of mindfulness will have adequate psychometric characteristics (particularly for sensitivity to change), and these measures should be pilot tested prior to their use in a large clinical trial.
We also found that the majority of participants continued to use some MBSR techniques after the completion of the instruction, and found their use helpful in stress reduction. This is noteworthy because there was no explicit maintenance component of the study (such as booster sessions or prompts to continue use of techniques). The fact that almost all participants reported that they continued to use, and benefit from, some of the MBSR techniques six months post-instruction speaks to the potential durability of MBSR as an intervention in this population. On the other hand, few if any participants established a regular (i.e., daily or almost every day) meditative practice. Future research should examine long-term use of mindfulness and meditative techniques in older adults after the cessation of MBSR instruction, as well as ways to stimulate their continued use, especially given what may have been a trend toward increasing worry among some participants 6 months post-intervention. Many participants who reported using mindful breathing and that doing so successfully combated stress; this is consistent with psychotherapy research which has shown that diaphragmatic breathing and other relaxation techniques, appear to be the most efficacious component of behavioral therapies in anxious older adults (Thorp et al., 2009). Theoretically, the difference is that in relaxation training, the emphasis is on breathing being from the diaphragm and slowing it down (i.e., focus on changing breathing). In contrast, in MBSR the emphasis is on paying attention to the breath and bringing attention back to the breath when the mind wanders (i.e., focus on noticing breathing but not changing it). Whether the two approaches are actually the same, different, or even complementary is unknown at this time.
In summary, our data show the feasibility, acceptability, and preliminarily the efficacy of MBSR in distressed older adults who report subjective co-occurring cognitive dysfunction.
Key points
In this pilot study, we found that Mindfulness-Based Stress Reduction (MBSR) was feasible for study in older adults with worry-related distress and co-occurring cognitive dysfunction, as ascertained by successful recruitment and retention, a high level of acceptability of the intervention, and adequate sensitivity to change of measures of mindfulness, worry pathology, and cognitive function.
After the MBSR course was completed, the vast majority of participants continued to use mindfulness techniques in their everyday life.
There was no apparent benefit to extending MBSR to allow greater repetition of material, in terms of worry reduction, cognitive improvement, or ongoing use of MBSR techniques during six months of follow-up.
These data are promising for further testing and eventual implementation of MBSR as an intervention for older adults with excessive worry and co-occurring cognitive dysfunction.
Acknowledgements
this study was supported by NIH R34 AT007064 from the National Center for Complementary and Alternative Medicine (St. Louis), NIH R34 AT007070 (San Diego), and the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS). The authors thank Lynn Rossy, Ph.D., and Bridget Rolens, O.T., for their efforts as MBSR instructors, and Helen Lavretsky, M.D., and Dmitris Kiosses, Ph.D., for their participation as external independent monitors.
Footnotes
Disclosures: Dr. Lenze receives funding from Lundbeck and Roche. The other authors report no potential conflicts.
References
- ALEXOPOULOS GS, KIOSSES DN, HEO M, MURPHY CF, SHANMUGHAM B, GUNNINGDIXON F. Executive dysfunction and the course of geriatric depression. Biological psychiatry. 2005;58:204–10. doi: 10.1016/j.biopsych.2005.04.024. [DOI] [PubMed] [Google Scholar]
- ANDREESCU C, TEVEROVSKY L, GANGULI M. Old Worries and New Anxieties - Behavioral Symptoms and Mild Cognitive Impairment in a Population Study. Am J Geriatr Psychiatry. doi: 10.1016/j.jagp.2012.09.010. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BAER RA, SMITH GT, HOPKINS J, KRIETEMEYER J, TONEY L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- BARNES PM, BLOOM B, NAHIN RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008:1–23. [PubMed] [Google Scholar]
- BEAUDREAU SA, MACKAY-BRANDT A, REYNOLDS J. Application of a cognitive neuroscience perspective of cognitive control to late-life anxiety. Journal of anxiety disorders. 2013;27:559–66. doi: 10.1016/j.janxdis.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BEAUDREAU SA, O'HARA R. Late-life anxiety and cognitive impairment: a review. Am J Geriatr Psychiatry. 2008;16:790–803. doi: 10.1097/JGP.0b013e31817945c3. [DOI] [PubMed] [Google Scholar]
- BEDARD M, FELTEAU M, GIBBONS C, KLEIN R, MAZMANIAN D, FEDYK K, MACK G. A mindfulness-based intervention to improve quality of life among individuals who sustained traumatic brain injuries: One year follow-up. Journal of Cognitive Rehabilitation. 2005;23:8–13. doi: 10.1080/0963828031000090489. [DOI] [PubMed] [Google Scholar]
- BEGUM A, MORGAN C, CHIU CC, TYLEE A, STEWART R. Subjective memory impairment in older adults: aetiology, salience and help seeking. International Journal of Geriatric Psychiatry. 2012;27:612–20. doi: 10.1002/gps.2760. [DOI] [PubMed] [Google Scholar]
- BISHOP SR. What do we really know about mindfulness-based stress reduction? Psychosom Med. 2002;64:71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- BROWN KW, RYAN RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- BROWN KW, WEINSTEIN N, CRESWELL JD. Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology. 2012;37:2037–2041. doi: 10.1016/j.psyneuen.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BUTTERS MA, BECKER JT, NEBES RD, ZMUDA MD, MULSANT BH, POLLOCK BG, REYNOLDS CF., 3RD Changes in cognitive functioning following treatment of late-life depression. Am J Psychiatry. 2000;157:1949–54. doi: 10.1176/appi.ajp.157.12.1949. [DOI] [PubMed] [Google Scholar]
- BUTTERS MA, BHALLA RK, ANDREESCU C, WETHERELL JL, MANTELLA R, BEGLEY AE, LENZE EJ. Changes in neuropsychological functioning following treatment for late-life generalised anxiety disorder. The British journal of psychiatry : the journal of mental science. 2011;199:211–8. doi: 10.1192/bjp.bp.110.090217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARLSON LE, SPECA M, FARIS P, PATEL KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21:1038–49. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- CAUDLE DD, SENIOR AC, WETHERELL JL, RHOADES HM, BECK JG, KUNIK ME, SNOW AL, WILSON NL, STANLEY MA. Cognitive errors, symptom severity, and response to cognitive behavior therapy in older adults with generalized anxiety disorder. Am J Geriatr Psychiatry. 2007;15:680–9. doi: 10.1097/JGP.0b013e31803c550d. [DOI] [PubMed] [Google Scholar]
- CRESWELL JD, IRWIN MR, BURKLUND LJ, LIEBERMAN MD, AREVALO JMG, MA J, BREEN EC, COLE SW. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain Behavior and Immunity. 2012;26:1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CRITTENDON J, HOPKO DR. Assessing worry in older and younger adults: Psychometric properties of an abbreviated Penn State Worry Questionnaire (PSWQ-A) Journal of anxiety disorders. 2006;20:1036–54. doi: 10.1016/j.janxdis.2005.11.006. [DOI] [PubMed] [Google Scholar]
- DAKIN EK, AREAN P. Patient perspectives on the benefits of psychotherapy for late-life depression. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2013;21:155–63. doi: 10.1016/j.jagp.2012.10.016. [DOI] [PubMed] [Google Scholar]
- DEYO M, WILSON KA, ONG J, KOOPMAN C. Mindfulness and rumination: does mindfulness training lead to reductions in the ruminative thinking associated with depression? Explore (NY) 2009;5:265–71. doi: 10.1016/j.explore.2009.06.005. [DOI] [PubMed] [Google Scholar]
- FELDMAN G, HAYES A, KUMAR S, GREESON J, LAURENCEAU JP. Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CMS-R) J Psychopathology and Behavioral Assessment. 2007;29:177–190. [Google Scholar]
- FIRST M, SPITZER R, GIBBON M, WILLIAMS J. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) American Psychiatric Press; Washington, D.C.: 1997. [Google Scholar]
- GALLEGOS AM, HOERGER M, TALBOT NL, KRASNER MS, KNIGHT JM, MOYNIHAN JA, DUBERSTEIN PR. Toward Identifying the Effects of the Specific Components of Mindfulness-Based Stress Reduction on Biologic and Emotional Outcomes Among Older Adults. Journal of alternative and complementary medicine. 2013 doi: 10.1089/acm.2012.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLDEN J, CONROY RM, BRUCE I, DENIHAN A, GREENE E, KIRBY M, LAWLOR BA. The spectrum of worry in the community-dwelling elderly. Aging & Mental Health. 2011;15:985–94. doi: 10.1080/13607863.2011.583621. [DOI] [PubMed] [Google Scholar]
- GOLDIN PR, GROSS JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 10:83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GROSS CR, KREITZER MJ, REILLY-SPONG M, WINBUSH NY, SCHOMAKER EK, THOMAS W. Mindfulness meditation training to reduce symptom distress in transplant patients: rationale, design, and experience with a recycled waitlist. Clin Trials. 2009;6:76–89. doi: 10.1177/1740774508100982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GROSSMAN P, TIEFENTHALER-GILMER U, RAYSZ A, KESPER U. Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom. 2007;76:226–33. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- HAYES AM, FELDMAN G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology-Science and Practice. 2004;11:255–262. [Google Scholar]
- HOPKO DR, STANLEY MA, REAS DL, WETHERELL JL, BECK JG, NOVY DM, AVERILL PM. Assessing worry in older adults: confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychol Assess. 2003;15:173–83. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- JAIN S, SHAPIRO SL, SWANICK S, ROESCH SC, MILLS PJ, BELL I, SCHWARTZ GE. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- KABAT-ZINN J, MASSION AO, KRISTELLER J, PETERSON LG, FLETCHER KE, PBERT L, LENDERKING WR, SANTORELLI SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936–43. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- LAVRETSKY H, EPEL ES, SIDDARTH P, NAZARIAN N, CYR NS, KHALSA DS, LIN J, BLACKBURN E, IRWIN MR. A pilot study of yogic meditation for family dementia caregivers with depressive symptoms: effects on mental health, cognition, and telomerase activity. International Journal of Geriatric Psychiatry. 2013;28:57–65. doi: 10.1002/gps.3790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LENGACHER CA, JOHNSON-MALLARD V, BARTA M, FITZGERALD S, MOSCOSO MS, POST-WHITE J, JACOBSEN PB, SHELTON MM, LE N, BUDHRANI P, GOODMAN M, KIP KE. Feasibility of a Mindfulness-Based Stress Reduction Program for Early-Stage Breast Cancer Survivors. J Holist Nurs. 2010 doi: 10.1177/0898010110385938. [DOI] [PubMed] [Google Scholar]
- LENZE EJ, ROLLMAN BL, SHEAR MK, DEW MA, POLLOCK BG, CILIBERTI C, COSTANTINO M, SNYDER S, SHI P, SPITZNAGEL E, ANDREESCU C, BUTTERS MA, REYNOLDS CF. Escitalopram for older adults with Generalized Anxiety Disorder: a placebo-controlled trial. JAMA. 2009;301:296–303. doi: 10.1001/jama.2008.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LENZE EJ, WETHERELL JL. A lifespan view of anxiety disorders. Dialogues in clinical neuroscience. 2011;13:381–99. doi: 10.31887/DCNS.2011.13.4/elenze. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LOERA JA, REYES-ORTIZ C, KUO YF. Predictors of complementary and alternative medicine use among older Mexican Americans. Complement Ther Clin Pract. 2007;13:224–31. doi: 10.1016/j.ctcp.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MACCOON DG, IMEL ZE, ROSENKRANZ MA, SHEFTEL JG, WENG HY, SULLIVAN JC, BONUS KA, STONEY CM, SALOMONS TV, DAVIDSON RJ, LUTZ A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour Research and Therapy. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MACKIN RS, DELUCCHI KL, BENNETT RW, AREAN PA. The effect of cognitive impairment on mental healthcare costs for individuals with severe psychiatric illness. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2011;19:176–84. doi: 10.1097/JGP.0b013e3181e56cfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MATOUSEK RH, DOBKIN PL. Weathering storms: a cohort study of how participation in a mindfulness-based stress reduction program benefits women after breast cancer treatment. Curr Oncol. 2010;17:62–70. doi: 10.3747/co.v17i4.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MEEKS TW, WETHERELL JL, IRWIN MR, REDWINE LS, JESTE DV. Complementary and alternative treatments for late-life depression, anxiety, and sleep disturbance: a review of randomized controlled trials. J Clin Psychiatry. 2007;68:1461–71. doi: 10.4088/jcp.v68n1001. [DOI] [PubMed] [Google Scholar]
- MILLER JJ, FLETCHER K, KABAT-ZINN J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- MOHLMAN J, GORENSTEIN EE, KLEBER M, DE JESUS M, GORMAN JM, PAPP LA. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: two pilot investigations. Am J Geriatr Psychiatry. 2003;11:24–32. [PubMed] [Google Scholar]
- MOHLMAN J, GORMAN JM. The role of executive functioning in CBT: a pilot study with anxious older adults. Behav Res Ther. 2005;43:447–65. doi: 10.1016/j.brat.2004.03.007. [DOI] [PubMed] [Google Scholar]
- MOYNIHAN JA, CHAPMAN BP, KLORMAN R, KRASNER MS, DUBERSTEIN PR, BROWN KW, TALBOT NL. Mindfulness-based stress reduction for older adults: effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology. 2013;68:34–43. doi: 10.1159/000350949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NAHIN RL, BARNES PM, STUSSMAN BJ, BLOOM B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl Health Stat Report. 2009:1–14. [PubMed] [Google Scholar]
- NAHIN RL, DAHLHAMER JM, TAYLOR BL, BARNES PM, STUSSMAN BJ, SIMILE CM, BLACKMAN MR, CHESNEY MA, JACKSON M, MILLER H, MCFANN KK. Health behaviors and risk factors in those who use complementary and alternative medicine. BMC Public Health. 2007;7:217. doi: 10.1186/1471-2458-7-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NEWCOMER JW, CRAFT S, HERSHEY T, ASKINS K, BARDGETT ME. Glucocorticoid-induced impairment in declarative memory performance in adult humans. J Neurosci. 1994;14:2047–53. doi: 10.1523/JNEUROSCI.14-04-02047.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NGUYEN HT, GRZYWACZ JG, LANG W, WALKUP M, ARCURY TA. Effects of complementary therapy on health in a national U.S. sample of older adults. J Altern Complement Med. 16:701–6. doi: 10.1089/acm.2009.0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PALMER K, BERGER AK, MONASTERO R, WINBLAD B, BACKMAN L, FRATIGLIONI L. Predictors of progression from mild cognitive impairment to Alzheimer disease. Neurology. 2007;68:1596–602. doi: 10.1212/01.wnl.0000260968.92345.3f. [DOI] [PubMed] [Google Scholar]
- PIETRZAK RH, MARUFF P, WOODWARD M, FREDRICKSON J, FREDRICKSON A, KRYSTAL JH, SOUTHWICK SM, DARBY D. Mild worry symptoms predict decline in learning and memory in healthy older adults: a 2-year prospective cohort study. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2012;20:266–75. doi: 10.1097/JGP.0b013e3182107e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- POTTER GG, MCQUOID DR, PAYNE ME, TAYLOR WD, STEFFENS DC. Association of attentional shift and reversal learning to functional deficits in geriatric depression. International Journal of Geriatric Psychiatry. 2012;27:1172–9. doi: 10.1002/gps.3764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ROSENBERG PB, MIELKE MM, APPLEBY BS, OH ES, GEDA YE, LYKETSOS CG. The Association of Neuropsychiatric Symptoms in MCI With Incident Dementia and Alzheimer Disease. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2012 doi: 10.1016/j.jagp.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RYDER PT, WOLPERT B, ORWIG D, CARTER-POKRAS O, BLACK SA. Complementary and alternative medicine use among older urban African Americans: individual and neighborhood associations. J Natl Med Assoc. 2008;100:1186–92. doi: 10.1016/s0027-9684(15)31475-9. [DOI] [PubMed] [Google Scholar]
- SHAPIRO SL, OMAN D, THORESEN CE, PLANTE TG, FLINDERS T. Cultivating mindfulness: effects on well-being. J Clin Psychol. 2008;64:840–62. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- SINOFF G, WERNER P. Anxiety disorder and accompanying subjective memory loss in the elderly as a predictor of future cognitive decline. Int J Geriatr Psychiatry. 2003;18:951–9. doi: 10.1002/gps.1004. [DOI] [PubMed] [Google Scholar]
- SNEED JR, CULANG ME, KEILP JG, RUTHERFORD BR, DEVANAND DP, ROOSE SP. Antidepressant medication and executive dysfunction: a deleterious interaction in late-life depression. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2010;18:128–35. doi: 10.1097/JGP.0b013e3181c796d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STAHL B, GOLDSTEIN E. A Mindfulness-Based Stress Reduction Workbook. New Harbinger Pubns Inc; 2010. [Google Scholar]
- STANLEY MA, DIEFENBACH GJ, HOPKO DR, NOVY D, KUNIK ME, WILSON N, WAGENER P. The nature of generalized anxiety in older primary care patients: Preliminary findings. Journal of Psychopathology and Behavioral Assessment. 2003;25:273–280. [Google Scholar]
- STANLEY MA, WILSON NL, NOVY DM, RHOADES HM, WAGENER PD, GREISINGER AJ, CULLY JA, KUNIK ME. Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial. JAMA. 2009;301:1460–7. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- THORP SR, AYERS CR, NUEVO R, STODDARD JA, SORRELL JT, WETHERELL JL. Meta-analysis comparing different behavioral treatments for late-life anxiety. Am J Geriatr Psychiatry. 2009;17:105–15. doi: 10.1097/JGP.0b013e31818b3f7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WETHERELL JL, AYERS CR, SORRELL JT, THORP SR, NUEVO R, BELDING W, GRAY E, STANLEY MA, AREAN PA, DONOHUE M, UNUTZER J, RAMSDELL J, XU R, PATTERSON TL. Modular psychotherapy for anxiety in older primary care patients. Am J Geriatr Psychiatry. 2009;17:483–92. doi: 10.1097/JGP.0b013e3181a31fb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WILKES CM, WILSON HW, WOODARD JL, CALAMARI JE. Do negative affect characteristics and subjective memory concerns increase risk for late life anxiety? Journal of anxiety disorders. 2013;27:608–18. doi: 10.1016/j.janxdis.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WILSON RS, BEGENY CT, BOYLE PA, SCHNEIDER JA, BENNETT DA. Vulnerability to stress, anxiety, and development of dementia in old age. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2011;19:327–34. doi: 10.1097/JGP.0b013e31820119da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WOLFINGER R, CHANG M. Comparing the SAS GLM and MIXED Procedures for Repeated Measures. In: INC SI, editor. SAS Institute Inc. Cary, NC: [Google Scholar]
- ZHANG AL, XUE CC, LIN V, STORY DF. Complementary and alternative medicine use by older Australians. Ann N Y Acad Sci. 2007;1114:204–15. doi: 10.1196/annals.1396.032. [DOI] [PubMed] [Google Scholar]