Abstract
Introduction:
Choosing adjuvant radiotherapy (RT) or salvage RT after radical prostatectomy (RP) for locally advanced prostate cancer is controversial. Performing RT early after RP may increase the risk of urinary complications compared to RT performed later. We evaluated the urinary complication rates of men treated with surgery followed by early or late RT.
Methods:
Using a retrospective chart review, we compared rates of urinary incontinence (UI), bladder neck contracture (BNC), or urethral stricture in men with prostate cancer treated with early RT (<6 months after RP) or late RT (≥6 months after RP), 3 years after RT.
Results:
In total, 652 patients (between 2000 and 2007) underwent early RT (162, 24.8%) or late RT (490, 75.2%) after RP. The mean time to early RT was 3.6 months (range: 1–5 months) and to late RT was 30.1 months (range: 6–171 months). At 3 years post-RT, UI rates were similar in the early RT and the late RT groups (24.5% vs. 23.3%, respectively, p = 0.79). Prior to RT, 27/652 (4%) patients had a BNC and 11/652 (1.7%) had a urethral stricture, of which only 1 BNC persisted at 3 years post-RT. After RT, 17/652 (2.6%) BNC and 4/652 (0.6%) urethral stricture developed; of these, 6 BNC and 2 urethral strictures persisted at 3 years.
Conclusion:
Rates of UI, BNC, and urethral stricture were similar with early and late RT at 3 years post-RT. These findings suggest that the timing of RT after RP does not alter the incidences of these urinary complications and can aid in the decision-making process regarding adjuvant RT versus salvage RT.
Introduction
Radiotherapy (RT) after radical prostatectomy (RP) is an effective treatment option for locally advanced prostate cancer (T3 or positive surgical margins).1–6 Phase III studies have shown the benefit of adjuvant RT over a wait-and-see strategy.2,4,5 Salvage RT, performed later and triggered by biochemical recurrence, has been shown to be beneficial in several retrospective analyses.6–9 Although the results of retrospective trials comparing adjuvant and salvage RT favour adjuvant RT,10–13 no prospective randomized trials have been completed. The timing of postoperative RT remains controversial and treatment toxicity should be one of the factors considered.14,15
Adjuvant RT is typically delayed for a couple of months after RP to allow for healing, as these patients are at increased risk of urinary incontinence (UI), bladder neck contracture (BNC) and urethral stricture.16 Adjuvant RT has shown worse genitourinary (GU) toxicity as compared to wait-and-see treatment strategy with rates of UI and urethral stricture between 6% to 20% and 6% to 18%, respectively.3,17 Toxicity and long-term complication rates for salvage RT are similar to those of adjuvant RT; however, the effect of timing of postoperative RT on long-term complication rates is unknown and comparison of complication rates associated with early or late RT have not been previously reported. In this study, we evaluated the complication rates of men treated with RP followed by early or late RT.
Methods
We performed a retrospective analysis of patients at our institution (University Health Network, Toronto, Canada) who underwent RT after RP for prostate cancer, with permission from the hospital research ethics board. We included men who had RT at our institution after RP for prostate cancer, with at least a 3-year follow-up. These patients were divided into early RT (<6 months after surgery) or late RT (≥6 months after surgery) groups. Using a retrospective chart review, we recorded patient demographics, treatment characteristics and complications from RT. Data collected were based on routine clinical follow-up and divided into year 1, year 2 and year 3 after RT. Clinical follow-up varied based on the pathologic stage, patient factors, clinician routine and prostate-specific antigen (PSA). On every clinic visit after surgery, patients were asked by their clinician about voiding function, incontinence and erectile function. Their responses were recorded in the clinical notes. UI was defined as the presence of any reported leakage. If UI status could not be determined, patients were marked as unknown and excluded from the analysis. BNC and urethral stricture status were based on cystoscopic findings, with the need for cystoscopy based on lower urinary tract symptoms. For BNC and urethral stricture, patients were marked as unknown and excluded from the analysis if they previously had BNC or urethral stricture and their status could not be determined. We compared the complication rates in each group and time interval using Fisher’s Exact t-test.
Results
A retrospective chart review revealed 652 patients with 3 years of follow-up who underwent RT after RP between January 2000 and October 2007. Of these patients, 162 underwent early RT (24.8%) and 490 underwent late RT (75.2%). The mean time to RT was 3.6 months (range: 1–5 months) in the early RT group and 30.1 months (range: 6–171 months) in the late RT group (Table 1).
Table 1.
Patient and treatment characteristics
| Early RT | Late RT | |||
|---|---|---|---|---|
|
| ||||
| No. patients | 162 (24.8%) | 490 (75.2%) | ||
| Age at RP | ||||
| Mean | 60.47 | 60.44 | ||
| Range | 45–75 | 41–76 | ||
| Time to RT | ||||
| Mean | 3.6 months | 30.1 months | ||
| Range | 1–5 months | 6–171 months | ||
| Radiation dose | ||||
| Mean | 66 Gy | 66 Gy | ||
| Range | 50–70 Gy | 50–70 Gy | ||
| Types of RT | ||||
| 3D conformal | 141 (87.0%) | 415 (84.7%) | ||
| IMRT | 21 (13.0%) | 75 (15.3%) | ||
| Nerve-sparing status | ||||
| Unilateral | 18 (11.1%) | 51 (10.4%) | ||
| Bilateral | 32 (19.8%) | 90 (18.4%) | ||
| Non-sparing | 18 (11.1%) | 40 (8.2%) | ||
| Unknown | 94 (58.0%) | 309 (63.0%) | ||
| Pre-RT | Post-RT | Pre-RT | Post-RT | |
| ADT | 38 (23.5%) | 50 (30.9%) | 104 (21.2%) | 142 (29.0%) |
RT: radiotherapy; RP: radical prostatectomy; ADT: androgen deprivation therapy; IMRT: intensity-modulated radiotherapy.
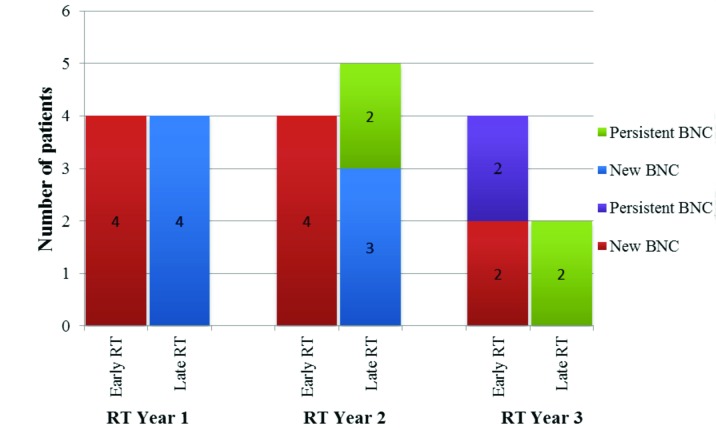
In the early and late RT groups, we tallied the number of patients per year with UI that developed postoperatively before RT (pre-existing) or after RT (new-onset) (Fig. 1). UI developed postoperatively but before RT in 88 patients (54.3%) in the early RT group and in 170 patients (34.7%) in the late RT group. Including both pre-existing and new-onset UI, at 3 years post-RT, 27 patients (24.5%) in the early RT group and 72 patients (23.3%) in the late RT group had UI (p = 0.79) (Table 2). Twelve patients (5 in the early RT group and 7 in the late RT group) received an artificial urinary sphincter (AUS) during the first 3 years after RT (p = 0.18).
Fig. 1.
Number of patients with UI, per-year, who developed before (preexisting) or after (new-onset) RT in the early and late RT groups. RT: radiotherapy; UI: urinary incontinence.
Table 2.
Urinary incontinence rates per year
| Early RT, no. (%) | Late RT, no. (%) | Fisher’s exact t-test | |
|---|---|---|---|
| No. patients | 162 | 490 | |
| Urinary continence | |||
| Leak | 88 (54.3) | 170 (34.7) | |
| No leak | 74 | 320 | |
| Unknown | 0 | 0 | |
| 1 Year post-RT | |||
| Leak | 42 (30.2) | 95 (22.4) | p = 0.068 |
| No leak | 97 | 329 | |
| Unknown | 23 | 66 | |
| 2 Years post-RT | |||
| Leak | 30 (24.6) | 82 (22.2) | p = 0.63 |
| No leak | 92 | 287 | |
| Unknown | 40 | 121 | |
| 3 Years post-RT | |||
| Leak | 27 (24.5) | 72 (23.3) | p = 0.79 |
| No leak | 83 | 237 | |
| Unknown | 52 | 181 |
RT: radiotherapy.
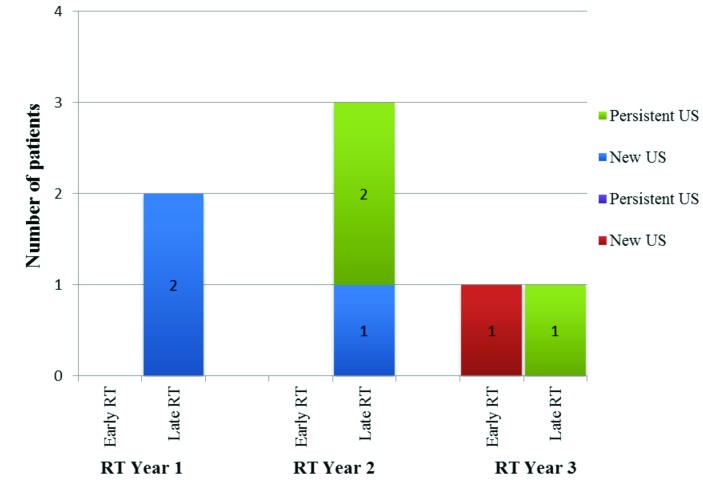
In both groups, 27 patients (4.1%) developed BNC postoperatively but before RT. Of these 27 pre-existing BNC, at 3 years after RT, 3 patients (1.9%) were in the early RT group (2 cases were resolved and 1 was unknown) and 24 patients (4.9%) were in the late RT group (I case persisted and 3 were unknown). After RT, 17 patients (2.6%) developed new-onset BNC; of these, 10 patients (6.1%) were in the early RT group (4 cases persisted at 3 years after RT and 1 unknown) and 7 patients (1.4%) in the late RT group (2 cases persisted at 3 years after RT (Fig. 2). Including both pre-existing and new-onset BNC, at 3 years post-RT, 4 persisted in the early RT group (2.5%) and 3 persisted in the late RT group (0.41%) (p = 0.068).
Fig. 2.
Number of patients with BNC that developed post-radiotherapy (new and persistent) in the early and late RT groups. RT: radiotherapy; BNC: bladder neck contracture.
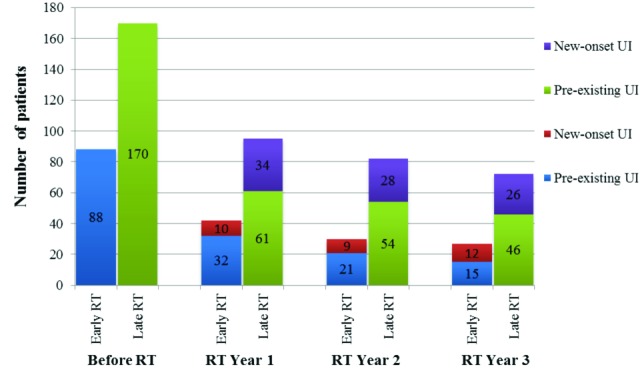
Urethral stricture developed postoperatively in 11 patients (1.7%) before RT, including 4 patients (2.4%) in the early RT group and 7 patients (1.4%) in the late RT group. At 3 years post-RT, none of these pre-existing urethral strictures persisted (4 were unknown). After RT, 4 patients (0.6%) developed new-onset urethral stricture; of these, 1 patient (0.62%) in the early RT group and 3 patients (0.61%) in the late RT group. At 3 years post-RT, 1 urethral stricture persisted in the early RT group (0.63%) and 1 urethral stricture persisted in the late RT group (0.20%) (p = 0.44) (Fig. 3).
Fig. 3.
Number of patients with US who developed post-RT (new and persistent) in the early and late RT groups. RT: radiotherapy; US: urethral stricture.
Discussion
Phase III studies that compared adjuvant RT with a wait-and-see strategy have shown that adjuvant RT improved local control,2 biochemical progression-free survival,2,5 metastases-free survival4 and overall survival.4 Salvage RT has been shown to be beneficial in several retrospective analyses.7–9 Although adjuvant RT and salvage RT have been compared in numerous retrospective studies with results favouring adjuvant RT, no prospective randomized trials have been completed.10–13 In one study, adjuvant RT was only found to be beneficial over salvage RT if the side effects were negligible, emphasizing the importance of side effects on treatment timing.18 In addition, long-term follow-up from the European Organization for Research and Treatment of Cancer (EORTC) trial 22911 has shown that clinical progression-free survival rates previously reported with adjuvant RT were no longer clinically significant; moreover, in patients over 70, adjuvant RT had a detrimental effect on progression-free and overall survival.2 The decision to treat with adjuvant or salvage RT is perhaps more controversial than ever and should include patient preference, demographics, pathologic features and risk of complications.
RT causes capillary destruction with reduced vascularity and tissue fibrosis, relative tissue hypoxia and reduced nutrient supply.16 After RP, as tissues are healing, early RT may further increase the risk of urinary complications, including urethral stricture, BNC and UI, compared to RT performed later. As such, adjuvant RT is frequently delayed after RP to allow for wound healing and return of urinary continence.19 In this study, the mean time to RT in the early group was 3.6 months with a range of 1–5 months indicating that some patients received RT earlier than recommended. Patients who received early RT in our series either opted for adjuvant RT or exhibited early biochemical relapse, whereas those who received late RT generally exhibited late relapse or a relapse with a slow doubling time. Six months was chosen as a separation point between patients who received RT while potentially still healing and those who had RT when fully healed postoperatively, although most patients who received late treatment were well beyond the 6-month interval. Salvage RT for biochemical failure is typically administered before PSA increases above 0.2 to 0.5 ng/mL and the average time to salvage RT is reported between 12 and 24 months.3,8,10,14,20,21 In this study, the time to RT in the late RT group was later at 30.1 months.
Chronic RT toxicity can present late after treatment, however most bladder complications manifest within 3 years of therapy.22 Data were collected in time intervals of 1, 2 and 3 years after RT to capture most long-term complications. We observed new-onset of UI in 3 years post-RT in both RT groups. Urinary continence can improve for up to 24 months after RP and early RT may interfere with or prolong this return to continence.19 In this study, UI was more common in the early RT group at the time of RT and UI rates improved in both groups at years 1, 2, and 3 post-RT. Although the severity of UI was not recorded, only 12 patients in the cohort had an AUS placed. These patients had UI which was severe and bothersome enough to require AUS and there was no difference in the number of AUS surgeries between the 2 RT groups.
Complication rates of RT post-RP vary and depend on the patient and radiation factors, such as timing, dose and technique.23 We found that the UI rates were not significantly different in patients receiving early (24.5%) or late RT (23.3%) at 3 years after RT. In the Southwest Oncology Group (SWOG) 8794 trial, adjuvant RT increased total UI (6.5% vs. 2.8%) compared with the wait-and-see group.3 In the 50 men who received salvage RT, Forman and colleagues reported a UI rate of 6%.24 Our UI rates were higher likely due to our subjective definition of UI, as well as the number of patients with unknown status who were not included in the analysis. If we included the unknown patients as continent, 3-year UI rates would have been closer to those reported in the literature (16.7% early RT and 14.7% late RT).
The urethral stricture rate is increased with ART compared with the wait-and-see strategy (17.8% vs. 9.5%, respectively).3 In the 959 men receiving adjuvant or salvage RT, the reported rates of urethral stricture and BNC were 1.2% and 0.8%, respectively.25 In our study, BNC developed prior to RT in more patients than expected (4.1%); however, almost all of these resolved despite RT therapy. The high resolution rates of BNC and urethral stricture demonstrate that treatment of these complications is highly successful. During the first 3 years post-RT, new-onset urethral strictures were rare (4 cases), occurring mostly at 1 and 2 years post-RT. There were no significant differences in the rates of BNC or urethral stricture between early and late RT groups at 3 years post-RT. Overall, persistent urethral stricture (0.31%) and BNC (1.1%) rates at 3 years post-RT correlated with those in the literature.
Intensity-modulated radiotherapy (IMRT) reduces acute toxicity and gastrointestinal side effects, but may not reduce urinary complications because of the difficulty of excluding the bladder neck from the treatment field.15,26 Adjuvant RT with high-dose IMRT (>70 Gy) has been shown to have a late UI rate of 18% and urethral stricture rate of 6%.17 In this study, only a small proportion of the patients received IMRT (96/652, 13% early RT group and 15% late RT group) and doses >66 Gy were rare. Therefore, the complication rate may be lower than reported with higher radiation doses.
The non-standardized reporting and retrospective nature of data collection of this study is a source of a collection bias. Questionnaires assessing voiding function and incontinence were not routinely used. The degree or bother of the UI (i.e., pad use and weight, questionnaires or urodynamics) was not routinely determined in all patients. The lack of specific assessment of the incontinence and its severity, other than by clinical history, is a limitation in the methodology of this study. However, patient reporting of the presence of UI and whether it was troublesome likely mirrors clinical practice for most urologists and radiation oncologists and gives some understanding to both clinicians and patients as to what can be expected after postoperative RT. UI, BNC and urethral stricture may have been under-reported, especially in patients with mild symptoms, with a bias towards clinically relevant complications being included in the analysis. In addition, if patients had previous UI but their continence status was unknown at 3 years, they were excluded from the analysis, which limits the accuracy of our results.
This study is limited by the definition for early and late RT as they do not strictly match those of adjuvant and salvage RT. However, the results of this study do not demonstrate any impact of timing of postoperative RT on the development of urinary complications and this allows for flexibility in the decision around the optimal timing of the treatment. This study does not take into account how differences in surgical techniques and complications could affect the selection, dosing and toxicity of RT.
Conclusion
We found that UI was frequently reported after RP and this improved over time regardless of RT timing. Early and late RT showed similar rates of urinary complications (UI, urethral stricture and BNC) at 3 years post-RT. This suggests that the timing of radiation does not alter the incidences of these complications after RP. Along with the patient’s age, comorbidity, disease and preference for treatment, this added information can be used to make a decision regarding adjuvant versus salvage RT. Further investigation into the timing of postoperative RT and complication rates is underway in 2 phase III trials (RAVES [TROG 08-03] and RADICALS [MRC PR10, NCIC PR13, NCT 00541047]) which may serve to answer these questions in a randomized prospective manner, validate these results, and aid in the decision-making of early versus late RT.
Footnotes
Competing interests: Dr. Sowerby, Dr. Gani, Dr. Yim, Dr. Radomski and Dr. Catton all declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Bolla M, van Poppel H, Collette L, et al. Postoperative radiotherapy after radical prostatectomy: A randomised controlled trial (EORTC trial 22911) Lancet. 2005;366:572–8. doi: 10.1016/S0140-6736(05)67101-2. [DOI] [PubMed] [Google Scholar]
- 2.Bolla M, van Poppel H, Tombal B, et al. Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: Long-term results of a randomised controlled trial (EORTC trial 22911) Lancet. 2012;380:2018–27. doi: 10.1016/S0140-6736(12)61253-7. [DOI] [PubMed] [Google Scholar]
- 3.Thompson IM, Tangen CM, Paradelo J, et al. Adjuvant radiotherapy for pathologically advanced prostate cancer: A randomized clinical trial. JAMA. 2006;296:2329–35. doi: 10.1001/jama.296.19.2329. [DOI] [PubMed] [Google Scholar]
- 4.Thompson IM, Tangen CM, Paradelo J, et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: Long-term followup of a randomized clinical trial. J Urol. 2009;181:956–62. doi: 10.1016/j.juro.2008.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiegel T, Bottke D, Steiner U, et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96-02/AUO AP 09/95. J Clin Oncol. 2009;27:2924–30. doi: 10.1200/JCO.2008.18.9563. [DOI] [PubMed] [Google Scholar]
- 6.Stephenson AJ, Scardino PT, Kattan MW, et al. Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol. 2007;25:2035–41. doi: 10.1200/JCO.2006.08.9607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boorjian SA, Karnes RJ, Crispen PL, et al. Radiation therapy after radical prostatectomy: Impact on metastasis and survival. J Urol. 2009;182:2708–15. doi: 10.1016/j.juro.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 8.Trock BJ, Han M, Freedland SJ, et al. Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA. 2008;299:2760–9. doi: 10.1001/jama.299.23.2760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song C, Kim YS, Hong JH, et al. Treatment failure and clinical progression after salvage therapy in men with biochemical recurrence after radical prostatectomy: Radiotherapy vs androgen deprivation. BJU Int. 2009;106:188–93. doi: 10.1111/j.1464-410X.2009.09136.x. [DOI] [PubMed] [Google Scholar]
- 10.Cozzarini C, Bolognesi A, Ceresoli GL, et al. Role of postoperative radiotherapy after pelvic lymphadenectomy and radical retropubic prostatectomy: A single institute experience of 415 patients. Int J Radiat Oncol Biol Phys. 2004;59:674–83. doi: 10.1016/j.ijrobp.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Hagan M, Zlotecki R, Medina C, et al. Comparison of adjuvant versus salvage radiotherapy policies for postprostatectomy radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59:329–40. doi: 10.1016/j.ijrobp.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 12.Trabulsi EJ, Valicenti RK, Hanlon AL, et al. A multi-institutional matched-control analysis of adjuvant and salvage postoperative radiation therapy for pT3-4N0 prostate cancer. Urology. 2008;72:1298–302. doi: 10.1016/j.urology.2008.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ost P, De Troyer B, Fonteyne VR, et al. A matched control analysis of adjuvant and salvage high-dose postoperative intensity-modulated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2011;80:1316–22. doi: 10.1016/j.ijrobp.2010.04.039. [DOI] [PubMed] [Google Scholar]
- 14.Izawa JI. Salvage radiotherapy after radical prostatectomy. Can Urol Assoc J. 2009;3:245. [PMC free article] [PubMed] [Google Scholar]
- 15.Cozzarini C, Di Muzio N. Contemporary role of radiation therapy in the adjuvant or salvage setting following radical prostatectomy. Curr Opin Urol. 2011;21:206–10. doi: 10.1097/MOU.0b013e3283449e06. [DOI] [PubMed] [Google Scholar]
- 16.Gabka CJ, Benhaim P, Mathes SJ, et al. An experimental model to determine the effect of irradiated tissue on neutrophil function. Plast Reconstr Surg. 1995;96:1676–88. doi: 10.1097/00006534-199512000-00023. [DOI] [PubMed] [Google Scholar]
- 17.Ost P, Fonteyne V, Villeirs G, et al. Adjuvant high-dose intensity-modulated radiotherapy after radical prostatectomy for prostate cancer: Clinical results in 104 patients. Eur Urol. 2009;56:669–75. doi: 10.1016/j.eururo.2009.05.041. [DOI] [PubMed] [Google Scholar]
- 18.Jani AB, Kao J. Postprostatectomy adjuvant versus salvage radiotherapy. Cancer. 2005;103:1833–42. doi: 10.1002/cncr.20949. [DOI] [PubMed] [Google Scholar]
- 19.Petroski RA, Warlick WB, Herring J, et al. External beam radiation therapy after radical prostatectomy: Efficacy and impact on urinary continence. Prostate Cancer Prostatic Dis. 2004;7:170–7. doi: 10.1038/sj.pcan.4500718. [DOI] [PubMed] [Google Scholar]
- 20.Cox JD, Gallagher MJ, Hammond EH, et al. Consensus statements on radiation therapy of prostate cancer: Guidelines for prostate re-biopsy after radiation and for radiation therapy with rising prostate-specific antigen levels after radical prostatectomy. J Clin Oncol. 1999;17:1155. doi: 10.1200/JCO.1999.17.4.1155. [DOI] [PubMed] [Google Scholar]
- 21.Heidenreich A, Aus G, Bolla M, et al. EAU guidelines on prostate cancer. Eur Urol. 2008;53:68–80. doi: 10.1016/j.eururo.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Marks LB, Carroll PR, Dugan TC, et al. The response of the urinary bladder, urethra, and ureter to radiation and chemotherapy. Int J Radiat Oncol Biol Phys. 1995;31:1257–80. doi: 10.1016/0360-3016(94)00431-J. [DOI] [PubMed] [Google Scholar]
- 23.Jereczek-Fossa BA, Zerini D, Fodor C, et al. Correlation between acute and late toxicity in 973 prostate cancer patients treated with three-dimensional conformal external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78:26–34. doi: 10.1016/j.ijrobp.2009.07.1742. [DOI] [PubMed] [Google Scholar]
- 24.Forman JD, Duclos M, Shamsa F, et al. Predicting the need for adjuvant systemic therapy in patients receiving postprostatectomy irradiation. Urology. 1996;47:382–6. doi: 10.1016/S0090-4295(99)80457-9. [DOI] [PubMed] [Google Scholar]
- 25.Feng M, Hanlon AL, Pisansky TM, et al. Predictive factors for late genitourinary and gastrointestinal toxicity in patients with prostate cancer treated with adjuvant or salvage radiotherapy. Int J Radiat Oncol Biol Phys. 2007;68:1417–23. doi: 10.1016/j.ijrobp.2007.01.049. [DOI] [PubMed] [Google Scholar]
- 26.Alongi F, Fiorino C, Cozzarini C, et al. IMRT significantly reduces acute toxicity of whole-pelvis irradiation in patients treated with post-operative adjuvant or salvage radiotherapy after radical prostatectomy. Radiother and Oncol. 2009;93:207–12. doi: 10.1016/j.radonc.2009.08.042. [DOI] [PubMed] [Google Scholar]