Abstract
Intravesical Bacillus Calmette-Guérin (BCG) is an important treatment for the management of non-muscle invasive bladder cancer because of its proven efficacy and favourable safety profile. The most common complications associated with BCG treatment are relatively minor. They include urinary frequency, cystitis, fever, and hematuria. Although serious complications are rare, patients can develop severe, life-threatening sepsis with disseminated mycobacterial infection. We report a rare case of periurethral diverticulum formation after intravesical BCG and review the literature on the potential complications of this treatment modality.
Case Report
A 74-year-old man with high-grade non-muscle invasive bladder cancer was managed with transurethral resection followed by Bacillus Calmette-Guérin (BCG). During his third treatment, it was difficult to insert the catheter, but the patient received treatment nonetheless. One week later, he developed a perineal mass posterior to the scrotum that was fluctuant and tender. A computed tomography (CT) demonstrated a 6 × 3 × 8-cm cystic collection without direct involvement of the bladder, prostate, or rectum (Fig. 1). The patient was brought to the operating room for a retrograde urethrogram (RUG), cystourethroscopy, and aspiration of the fluid collection. The RUG showed communication between the urethra and the collection (Fig. 2). Cystourethroscopy showed a small ostium in the pendulous urethra that communicated with the diverticulum. Percutaneous aspiration of the collection yielded a thick, white fluid. Cytology and cultures of were negative but AFB staining was positive. The polymerase chain reaction (PCR) confirmed the presence of Mycobacterium bovis, BCG subtype.
Fig. 1.
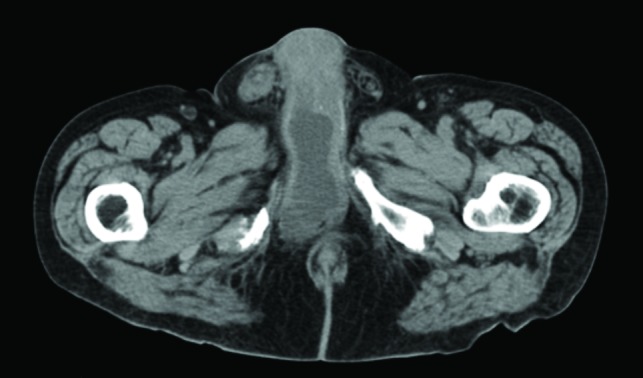
Computed tomography (CT) scan of a patient with a painful, fluctuant perineal mass after intravesical BCG instillation.
Fig. 2.
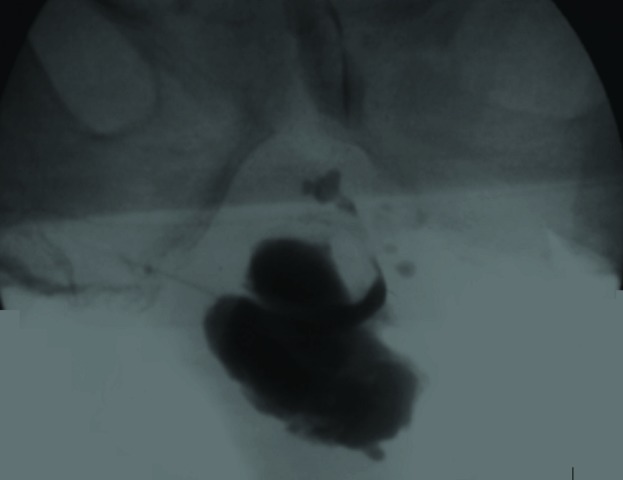
Retrograde urography demonstrating the presence of a pendulous periurethral diverticulum in the area of the perineal mass.
The patient’s symptoms resolved, and, at 6 months, the mass had regressed. A repeat RUG showed no further diverticulum (Fig. 3). This experience highlights the importance of deferring treatment in the setting of recent mucosal injury. In this paper, we review the complications of intravesical BCG.
Fig. 3.
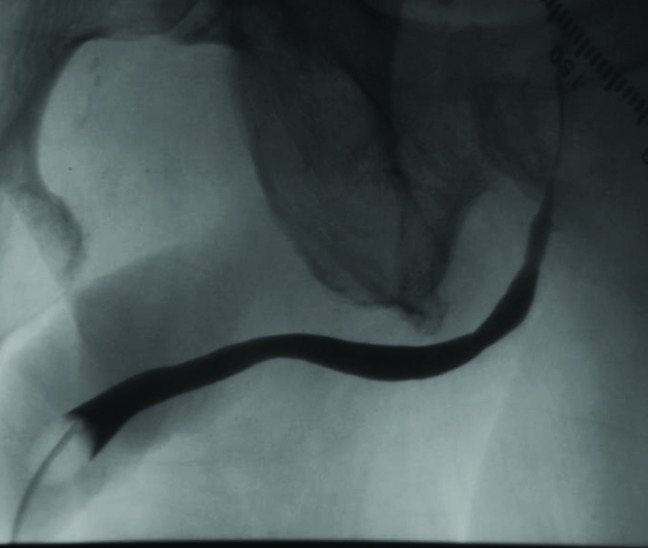
Retrograde urography demonstrating resolution of the periurethral diverticulum following aspiration.
Background
Intravesical therapy for non-muscle invasive bladder cancer has been a mainstay of treatment since the 1970s.1 BCG remains the most effective adjuvant treatment for non-muscle invasive bladder cancer, as demonstrated in multiple clinical trials.2 It is also the most effective treatment for carcinoma in situ, in terms of recurrence and progression.3 BCG is a live, attenuated strain of Mycobacterium bovis that was isolated by Calmette in 1921.4 Numerous strains are currently in use, although there were no differences in the efficacy or side effects of any standard preparations among 24 trials that included over 4800 patients.4 Continued efforts are being devoted to developing safer, more effective strains and the addition of agents to augment the immune response.5 The mechanism of tumour destruction due to BCG is not fully understood. One potential mechanism involves internalization of BCG by urothelial cells, which triggers an inflammatory cascade, inducing neutrophil and Th1 chemotaxis.6 Th1-induced production of IL-2, TNF, and IFN-γ is thought to mediate tumour destruction.
Side effects of intravesical BCG include local infection, multi-organ granulomata, reactive arthritis, hypersensitivity reactions, and severe BCG sepsis. Acid-fast bacilli can be difficult to identify despite the presence of granulomata, making diagnosis difficult. Because patients often initially present to non-urologists, educating them about these risks may prevent misdiagnosis and inappropriate treatment.
The largest series of complications from BCG included over 2600 patients.7,8 The most common were irritative lower urinary tract symptoms (LUTS) (27%-95%), fever greater than 39.5ºC (2.9%), hematuria (1.0%), granulomatous prostatitis (0.9%), granulomatous pneumonitis or hepatitis (0.7%), arthralgia (0.5%), epididymitis (0.4%), and severe disseminated BCG sepsis (0.4%), as well as very rare rashes, ureteral obstruction, bladder contraction, and renal abscesses (all <0.3%).7,8
Methods
We reviewed the literature on the complications of intravesical BCG for the treatment of non-muscle invasive bladder cancer. A PUBMED search was performed using the keywords “intravesical,” “BCG,” and “complications;” the search yielded 124 publications. The abstracts were judged by the authors independently and have been included based on consensus opinion.
Prostatitis
Granulomatous prostatitis has been documented as far back as 1985, when Stilmant reported it in a series of 6 patients receiving intravesical BCG.9 Subsequently, a larger series of 32 patients showed that 41% had histologically demonstrated granulomatous prostatitis after BCG, although not all patients were symptomatic.10 Others have reported cases identified by symptomatic presentation and incidentally during imaging.11,12 Acid-fast staining was typically positive, although it was not uniformly performed. Treatment with non-pyrazinamide antimycobacterials, ranging from single to triple therapy for 3–9 months, was successful.
Epididymo-orchitis
Numerous case reports have implicated M. bovis as the causal agent in epididymo-orchitis following intravesical BCG therapy.13 The mechanism is thought to include retrograde migration of the bacillus into the ejaculatory ducts. Granulomatous epididymo-orchitis has been diagnosed as soon as several months and as late as 4 years after BCG.14 Cases were treated with incision and drainage, orchiectomy, or single and multi-agent anti-tubercular therapy for several months.15–17 Because granulomata can mimic a testicular mass on ultrasound, the threshold for performing orchiectomy has been low to the detriment of the patient.18
Balanitis
The most widely reported penile complication of BCG is localized infection that manifests as granulomatous inflammation on biopsy. Several case reports describe yellowish papules or erythematous plaques on the glans, typically presenting after multiple cycles of BCG.19–21 Acid-fast bacilli may not be identified. All these lesions eventually resolved and no recurrence was seen at up to 18 months of follow-up.21
Ureteral obstruction
There is one case report of ureterovesical junction obstruction in a patient undergoing intravesical BCG for non-muscle invasive bladder cancer.22 The 76-year-old patient had a distant history of right nephroureterectomy. One week after receiving BCG, he became anuric. A left percutaneous nephrostomy tube was placed, at which time an antegrade nephrostogram showed complete left ureterovesical junction obstruction. The authors attributed the obstruction to severe inflammation of the bladder mucosa. The patient made a full recovery. It is unclear whether this occurs more frequently yet remains undetected in those who do not have a solitary kidney.
Bladder contraction
The rate of bladder contraction has been reported as 0.2% by Lamm and colleagues.7 Nieder and colleagues reviewed 2255 patients undergoing cystectomy for all causes. They found 1 male patient at each institution (0.09%) who underwent cystectomy for bladder contracture after BCG.23,24 Although this does not represent a true incidence, it does suggest that bladder contraction is extremely rare. More research is needed in order to characterize patients who mount atypically strong reactions that result in bladder contraction.
BCG persistence
Bowyer and colleagues retrospectively reviewed 125 patients who underwent BCG to assess the prevalence of persistent mycobacteriuria.25 Four patients had symptomatic persistent mycobacteriuria, while one patient was asymptomatic. These cases were diagnosed between 4.5 and 16.5 months after therapy. Two patients received double or triple agent anti-mycobaterial therapy to resolution, while the others had spontaneous resolution.
Orthopedic complications
Orthopedic complications of BCG therapy include myco-bacterial osteomyelitis and reactive arthritis. A recent series reported 8 cases of osteomyelitis after BCG therapy.26 Of these, 5 involved the vertebrae, 2 involved prostheses (1 knee and 1 hip), and 1 was monoarticular. BCG osteomyelitis is more difficult to diagnose because it presents late. Risk factors include recent fracture, recent placement of joint prosthesis, impaired wound healing (as a result of diabetes) and relative immune suppression (diagnosis of other malignancies). The sequelae of BCG osteomyeltis can be severe and lead to the destruction of weight-bearing bones.27
BCG-associated reactive arthritis is less morbid. It typically takes multiple instillations before onset of symptoms and usually manifests within 2 weeks of the most recent treatment.28–30 Cases are usually polyarticular and associated with uveitis and fever. Laboratory studies routinely showed ESR and CRP. Of those tested for HLA B27, 53% were positive. Reactive arthritis typically responded to NSAIDs, although in 7 refractory cases, isoniazid and rifampin were used, and, in 1 case, oral prednisone was used. Patients responded to pharmacotherapy with resolution in all cases.28
Rheumatologic complications
Immunological side effects from BCG therapy are not surprising, given that BCG incites robust immune activation. In a recent review, Tinazzi and colleagues summarized over 50 cases of arthritis and arthralgia resulting from BCG. The authors discuss reports of Reiter’s syndrome, polyarthritis, and rheumatoid-like arthritis, as well as mild arthralgias not otherwise specified. In most cases, patients responded to courses of high-dose non-steroidal anti-inflammatory drugs (NSAIDs). In some patients, however, particularly those with polyarthritis or Reiter’s syndrome, corticosteroids and prophylactic isoniazid and rifampin were added. The workup for these patients may be relatively exhaustive given a broad differential, including infectious, rheumatologic, and paraneoplastic causes.29
Remitting seronegative symmetrical synovitis pitting edema (RS3PE) is a polyarthritis characterized by pitting edema of the hands and feet, lack of bony erosions, and lack of rheumatoid factor (in contrast to rheumatoid arthritis).30 To date, there have been at least 2 cases of RS3PE reported in association with BCG.31 Typically, patients experience an acute onset of symmetric polyarthritis, fever, pitting edema in the hands and feet, and elevated CRP and ESR. Synovial, blood, and pharyngeal cultures are negative, including PCR and other acid-fast assays. HLA may be positive for B7. Patients respond to cessation of BCG and high-dose NSAIDs such as ketoprofen.
Pulmonary complications
Two kinds of pulmonary complications are reported: hypersensitivity and mycobacterial pneumonia. Hypersensitivity is characterized by an interstitial pattern on chest radiography, lymphocytosis on BAL, and absence of granulomas on lung biopsy, as well as sputum and tissue negativity for acid-fast bacilli.32 Mycobacterial pneumonia is typified by biopsies demonstrating granulomata and radiographic evidence of consolidation, although testing for AFB may be negative.33 Symptoms include fever, cough, chills, rigours and sweats.
The difficulty in isolating AFB in cases of suspected pneumonia has led some to question the diagnosis.32 However, in one patient with sepsis and radiographic evidence of miliary disease after BCG, AFB were not seen until a second pathologic review.34 Management for BCG-related pneumonitis and pneumonia includes double or triple anti-tubercular therapy (isoniazide, rifampin, or ethambutol). One patient was treated for 9 months with isoniazide and rifampin and was well at the 4-year follow-up.35 Another patient was treated on triple therapy for 5 months, with symptom resolution.33
Hepatic complications
Granulomatous hepatitis can be quite severe. We reviewed 6 cases cited in the literature between 1985 and 2007. Among these, there were 2 deaths [42–45].36–39 All 6 patients met the criteria for systemic inflammatory immune response during the course of their illness. Common features include fever, hepatosplenomegaly, transaminitis, and elevated inflammatory markers. Tissue biopsy demonstrated granulomatous hepatitis but generally failed to reveal AFB. Patients universally had incomplete responses to isoniazid, rifampin, and ethambutol until steroids or IVIG were added. Steroids were typically maintained until symptoms resolved, whereas anti-mycobacterial agents were continued for 6–12 months.37 The recovery time ranged from 7 days to 3 weeks.
Renal complications
Renal complications from BCG are relatively rare. At the tissue level, granulomatous nephritis, interstitial nephritis, and glomerulonephritis with immune deposits have been documented.38–46 Patients may fit nephritic or nephrotic clinical criteria. Granulomatous nephritis may cause severe renal compromise; one case led to nephroureterectomy.45 Another patient suffered a permanent decline in renal function.40 Interstitial nephritis from BCG can also be severe and is associated with acute azotemia and eosinophiluria, although urine AFB staining and cultures can be negative.42,43,46 Findings that suggest renal complications after BCG should prompt a renal biopsy. Treatment should be guided in consultation with a nephrologist and may include steroids and anti-mycobacterial therapy. Short-term hemodialysis may also be required.
Vascular complications
There are several reports of infectious vasculitis associated with BCG.47–50 Unlike other complications, the tissue specimens in these cases are universally positive for AFB when appropriate identification methods are used. BCG vasculitis has involved large arteries such as the aorta and popliteal artery leading to mycotic aneurysms and rupture. Diagnosis may be late due to the non-specific nature of symptoms.47 Patients who have undergone vascular surgery may be at increased risk.48 Treatment typically involves surgical repair of vessels, drainage of any abscesses, and anti-mycobacterial therapy for 9 to 12 months. In all reports reviewed, patients did well because of timely intervention.
Disseminated BCG
Disseminated BCG has been reported as a complication of both non-urologic51 as well as urologic34,52,53 indications. The incidence after intravesical treatment is 0.4%.7 Diagnosis may be made empirically or through identification of acid-fast bacilli in serum.52 Patients present with septicemia and hemodynamic compromise. Initial treatment should be aggressive and utilize as many as 5 antimicrobial agents, including isoniazid, rifampin, ethambutol, ciprofloxacin and pyrazinamide. Patients with severe hemodynamic compromise often require support with corticosteroids in addition to anti-mycobacterial agents.34,51
Conclusions
BCG remains the most effective treatment for prevention of recurrence and progression of non-muscle invasive bladder cancer. BCG-related complications can affect almost any organ, and appropriate consultation with specialists may be beneficial in managing these complications. BCG bacilli respond to isoniazid, rifampin, ethambutol, fluoroquinolones, clarithromycin, some aminoglycosides, and doxycycline, but generally not to pyrazinamide.54
Footnotes
Competing interests: Dr. Macleod, Dr. Ngo, and Dr. Gonzalgo all declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Morales A, Eidinger D, Bruce AW. Intracavitary bacillus Calmette-Guerin in the treatment of superficial bladder tumors. J Urol. 1976;116:180–3. doi: 10.1016/s0022-5347(17)58737-6. [DOI] [PubMed] [Google Scholar]
- 2.Lamm DL. Comparison of BCG with other intravesical agents. Urology. 1991;37:30–2. doi: 10.1016/0090-4295(91)80136-U. [DOI] [PubMed] [Google Scholar]
- 3.Jakse G. BCG for carcinoma in situ. Eur Urol. 1992;21(Suppl 2):30–4. doi: 10.1159/000474919. [DOI] [PubMed] [Google Scholar]
- 4.Sylvester RJ, Van der Meijden APM, Lamm DL. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: A meta-analysis of the published results of randomized clinical trials. J Urol. 2002;168:1964–70. doi: 10.1016/S0022-5347(05)64273-5. [DOI] [PubMed] [Google Scholar]
- 5.Kamat AM, Lamm DL. Immunotherapy for bladder cancer. Curr Urol Rep. 2001;2:62–9. doi: 10.1007/s11934-001-0027-7. [DOI] [PubMed] [Google Scholar]
- 6.Rosevear HM, Lightfoot AJ, O’Donnell MA, et al. The role of neutrophils and TNF-related apoptosis-inducing ligand (TRAIL) in bacillus Calmette-Guérin (BCG) immunotherapy for urothelial carcinoma of the bladder. Cancer Metastasis Rev. 2009;28:345–53. doi: 10.1007/s10555-009-9195-6. [DOI] [PubMed] [Google Scholar]
- 7.Lamm DL, van der Meijden PM, Morales A, et al. Incidence and treatment of complications of bacillus Calmette-Guerin intravesical therapy in superficial bladder cancer. J Urol. 1992;147:596–600. doi: 10.1016/s0022-5347(17)37316-0. [DOI] [PubMed] [Google Scholar]
- 8.Koya MP, Simon MA, Soloway MS. Complications of intravesical therapy for urothelial cancer of the bladder. J Urol. 2006;175:2004–10. doi: 10.1016/S0022-5347(06)00264-3. [DOI] [PubMed] [Google Scholar]
- 9.Stilmant M, Siroky MB, Johnson KB. Fine needle aspiration cytology of granulomatous prostatitis induced by BCG immunotherapy of bladder cancer. Acta Cytol. 1985;29:961–6. [PubMed] [Google Scholar]
- 10.Oates RD, Stilmant MM, Freedlund MC, et al. Granulomatous prostatitis following bacillus Calmette-Guerin immunotherapy of bladder cancer. J Urol. 1988;140:751–4. doi: 10.1016/s0022-5347(17)41803-9. [DOI] [PubMed] [Google Scholar]
- 11.Aust TR, Massey JA. Tubercular prostatic abscess as a complication of intravesical bacillus Calmette-Guérin immunotherapy. Int J Urol. 2005;12:920–1. doi: 10.1111/j.1442-2042.2005.01183.x. [DOI] [PubMed] [Google Scholar]
- 12.Ilgan S, Koca G, Gundogdu S. Incidental detection of granulomatous prostatitis by F-18 FDG PET/CT in a patient with bladder cancer: A rare complication of BCG instillation therapy. Clin Nucl Med. 2009;34:613–4. doi: 10.1097/RLU.0b013e3181b06c89. [DOI] [PubMed] [Google Scholar]
- 13.Harada H, Seki M, Shinojima H, et al. Epididymo-orchitis caused by intravesically instillated bacillus Calmette-Guérin: Genetically proven using a multiplex polymerase chain reaction method. Int J Urol. 2006;13:183–5. doi: 10.1111/j.1442-2042.2006.01257.x. [DOI] [PubMed] [Google Scholar]
- 14.Menke JJ, Heins JR. Epididymo-orchitis following intravesical bacillus Calmette-Guérin therapy. Ann Pharmacother. 2000;34:479–82. doi: 10.1345/aph.19212. [DOI] [PubMed] [Google Scholar]
- 15.Harving SS, Asmussen L, Roosen JU, et al. Granulomatous epididymo-orchitis, a rare complication of intravesical bacillus Calmette-Guérin therapy for urothelial cancer. Scand J Urol Nephrol. 2009;43:331–3. doi: 10.1080/00365590902930808. [DOI] [PubMed] [Google Scholar]
- 16.Hoag N, Pommerville PJ, Kibsey PC, et al. Tuberculous epididymitis following intravesical Bacillus Calmette-Guérin immunotherapy. Can J Urol. 2009;16:4589–91. [PubMed] [Google Scholar]
- 17.Bulbul MA, Hijaz A, Beaini M, et al. Tuberculous epididymo-orchitis following intravesical BCG for superficial bladder cancer. J Med Liban. 2002;50:67–9. [PubMed] [Google Scholar]
- 18.Truelson T, Wishnow KI, Johnson DE. Epididymo-orchitis developing as a late manifestation of intravesical bacillus Calmette-Guerin therapy and masquerading as a primary testicular malignancy: A report of 2 cases. J Urol. 1992;148:1534–5. doi: 10.1016/s0022-5347(17)36960-4. [DOI] [PubMed] [Google Scholar]
- 19.Michelet N, Spenattob N, Virabenb R, et al. BCG infection of the glans penis after intravesical BCG therapy. Ann Dermatol Venerol. 2008;135:479–83. doi: 10.1016/j.annder.2007.06.012. . [DOI] [PubMed] [Google Scholar]
- 20.Hillyer S, Gulmi FA. Cutaneous BCG of the penis after intravesical therapy for bladder cancer: A case report in a 66-year-old male. Can J Urol. 2009;16:4866–9. [PubMed] [Google Scholar]
- 21.Yusuke H, Yoshinori H, Kenichi M, et al. Granulomatous balanoposthitis after intravesical Bacillus-Calmette-Guerin instillation therapy. Int J Urol. 2006;13:1361–3. doi: 10.1111/j.1442-2042.2006.01553.x. [DOI] [PubMed] [Google Scholar]
- 22.Kaneko T, Fujita K, Homma Y. Transient anuria requiring nephrostomy after intravesical bacillus Calmette-Guérin instillations for superficial bladder cancer. Int J Urol. 2006;13:294–5. doi: 10.1111/j.1442-2042.2006.01283.x. [DOI] [PubMed] [Google Scholar]
- 23.Nieder AM, Sved PD, Stein JP, et al. Cystoprostatectomy and orthotopic ileal neobladder reconstruction for management of bacille Calmette Guérin-induced bladder contractures. Urology. 2005;65:909–12. doi: 10.1016/j.urology.2004.11.053. [DOI] [PubMed] [Google Scholar]
- 24.Hameed A, Sezian N, Thwaini A. Bladder contracture: Review for intravesical bacillus Calmette-Guerin complication. Can J Urol. 2007;14:3745–9. [PubMed] [Google Scholar]
- 25.Bowyer L, Hall RR, Reading J, et al. The persistence of bacille Calmette-Guérin in the bladder after intravesical treatment for bladder cancer. Br J Urol. 1995;75:188–92. doi: 10.1111/j.1464-410X.1995.tb07309.x. [DOI] [PubMed] [Google Scholar]
- 26.Clavel G, Grados F, Lefauveau P, et al. Osteoarticular side effects of BCG therapy. Joint Bone Spine. 2006;73:24–8. doi: 10.1016/j.jbspin.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Morgan MB, Iseman MD. Mycobacterium bovis vertebral osteomyelitis as a complication of intravesical administration of Bacille Calmette-Guérin. Am J Med. 1996;100:372–3. doi: 10.1016/S0002-9343(97)89500-9. [DOI] [PubMed] [Google Scholar]
- 28.Tinazzi E, Ficarra V, Simeoni S, et al. Reactive arthritis following BCG immunotherapy for urinary bladder carcinoma: A systematic review. Rheumatol Int. 2006;26:481–8. doi: 10.1007/s00296-005-0059-2. [DOI] [PubMed] [Google Scholar]
- 29.Onur O, Celiker R. Polyarthritis as a complication of intravesical bacillus Calmette-Guerin immunotherapy for bladder cancer. Clin Rheumatol. 1999;18:74–6. doi: 10.1007/s100670050059. [DOI] [PubMed] [Google Scholar]
- 30.Yao Q, Su X, Altman RD. Is remitting seronegative symmetrical synovitis with pitting edema (RS3PE) a subset of rheumatoid arthritis? Semin Arthritis Rheum. 2010;40:89–94. doi: 10.1016/j.semarthrit.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 31.El Mahou S, Popa L, Constantin A, et al. Remitting seronegative symmetrical synovitis pitting oedema after BCG instillation. Clin Rheumatol. 2006;25:566–7. doi: 10.1007/s10067-005-0157-2. [DOI] [PubMed] [Google Scholar]
- 32.Smith RL, Alexander RF, Aranda CP. Pulmonary granulomata. A complication of intravesical administration of bacillus Calmette-Guerin for superficial bladder carcinoma. Cancer. 1993;71:1846–7. doi: 10.1002/1097-0142(19930301)71:5<1846::AID-CNCR2820710521>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 33.Foster DR. Miliary tuberculosis: A complication of intravesical BCG treatment. Australas Radiol. 1998;42:167–8. doi: 10.1111/j.1440-1673.1998.tb00600.x. [DOI] [PubMed] [Google Scholar]
- 34.Nadasy KA, Patel RS, Emmett M, et al. Four cases of disseminated Mycobacterium bovis infection following intravesical BCG instillation for treatment of bladder carcinoma. South Med J. 2008;101:91–5. doi: 10.1097/SMJ.0b013e31815d4047. [DOI] [PubMed] [Google Scholar]
- 35.Gupta RC, Lavengood R, Jr, Smith JP. Miliary tuberculosis due to intravesical bacillus Calmette-Guerin therapy. Chest. 1988;94:1296–8. doi: 10.1378/chest.94.6.1296. [DOI] [PubMed] [Google Scholar]
- 36.Fradet V, Gaudreau C, Perrotte P, et al. Management of hepatic granulomatous tuberculosis complicating intravesical BCG for superficial bladder cancer. Can Urol Assoc J. 2007;1:269–72. doi: 10.5489/cuaj.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thevenot T, Di Martino V, Lagrange A, et al. Granulomatous hepatitis and hemophagocytic syndrome after bacillus Calmette-Guerin bladder instillation. Gastroenterol Clin Biol. 2006;30:480–2. doi: 10.1016/S0399-8320(06)73208-0. [DOI] [PubMed] [Google Scholar]
- 38.Ersoy O, Aran R, Aydinli M, et al. Granulomatous hepatitis after intravesical BCG treatment for bladder cancer. Indian J Gastroenterol. 2006;25:258–9. [PubMed] [Google Scholar]
- 39.Steg A, Sicard D, Leleu C, et al. Systemic complications of intravesical BCG therapy for bladder cancer. Lancet. 1985;2:899. doi: 10.1016/S0140-6736(85)90169-2. [DOI] [PubMed] [Google Scholar]
- 40.Modesto A, Marty L, Suc JM, et al. Renal complications of intravesical bacillus Calmette-Guérin therapy. Am J Nephrol. 1991;11:501–4. doi: 10.1159/000168368. [DOI] [PubMed] [Google Scholar]
- 41.Binaut R, Bridoux F, Provôt F, et al. Granulomatous interstitial nephritis with acute renal insufficiency, a potential complication of intravesicular bcg therapy [in French] Nephrologie. 1997;18:187–91. [PubMed] [Google Scholar]
- 42.Fry A, Saleemi A, Griffiths M, et al. Acute renal failure following intravesical bacille Calmette-Guérin chemotherapy for superficial carcinoma of the bladder. Nephrol Dial Transplant. 2005;20:849–50. doi: 10.1093/ndt/gfh688. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy SE, Shrikanth S, Charlesworth JA. Acute granulomatous tubulointerstitial nephritis caused by intravesical BCG. Nephrol Dial Transplant. 2006;21:1427–9. doi: 10.1093/ndt/gfk071. [DOI] [PubMed] [Google Scholar]
- 44.Singh NP, Prakash A, Kubba S, et al. Nephrotic syndrome as a complication of intravesical BCG treatment of transitional cell carcinoma of urinary bladder. Ren Fail. 2007;29:227–9. doi: 10.1080/08860220601098961. [DOI] [PubMed] [Google Scholar]
- 45.Soda T, Hori D, Onishi H, et al. Granulomatous nephritis as a complication of intrarenal bacille Calmette-Guérin therapy. Urology. 1999;53:1228. doi: 10.1016/S0090-4295(98)00499-3. [DOI] [PubMed] [Google Scholar]
- 46.Manzanera Escribano MJ, Morales Ruiz E, Odriozola Grijalba M, et al. Acute renal failure due to interstitial nephritis after intravesical instillation of BCG. Clin Exp Nephrol. 2007;11:238–40. doi: 10.1007/s10157-007-0483-6. [DOI] [PubMed] [Google Scholar]
- 47.Damm O, Briheim G, Hagström T, et al. Ruptured mycotic aneurysm of the abdominal aorta: A serious complication of intravesical instillation bacillus Calmette-Guerin therapy. J Urol. 1998;159:984. doi: 10.1016/S0022-5347(01)63796-0. [DOI] [PubMed] [Google Scholar]
- 48.Seelig MH, Oldenburg WA, Klingler PJ, et al. Mycotic vascular infections of large arteries with Mycobacterium bovis after intravesical bacillus Calmette-Guérin therapy: Case report. J Vasc Surg. 1999;29:377–81. doi: 10.1016/S0741-5214(99)70391-5. [DOI] [PubMed] [Google Scholar]
- 49.LaBerge JM, Kerlan RK, Jr, Reilly LM, et al. Diagnosis please. Case 9: Mycotic pseudoaneurysm of the abdominal aorta in association with mycobacterial psoas abscess — a complication of BCG therapy. Radiology. 1999;211:81–5. doi: 10.1148/radiology.211.1.r99ap4081. [DOI] [PubMed] [Google Scholar]
- 50.Witjes JA, Vriesema JLJ, Brinkman K, et al. Mycotic aneurysm of the popliteal artery as a complication of intravesical BCG therapy for superficial bladder cancer. Case report and literature review. Urol Int. 2003;71:430–2. doi: 10.1159/000074100. [DOI] [PubMed] [Google Scholar]
- 51.Rosenberg SA, Seipp C, Sears HF. Clinical and immunologic studies of disseminated BCG infection. Cancer. 1978;41:1771–80. doi: 10.1002/1097-0142(197805)41:5<1771::AID-CNCR2820410519>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 52.Del Prete R, Ditonno P, Mosca A, et al. BCG septicemia after radical cystectomy: A rare postoperative complication following BCG therapy. J Infect. 2002;45:112–4. doi: 10.1053/jinf.2002.1025. [DOI] [PubMed] [Google Scholar]
- 53.Sica S, Vargas N, Glielmi G, et al. A case of sepsis caused by BCG (Bacillus Calmette Guerin) after its bladder instillation in a 71-year-old patient affected by bladder carcinoma. Infez Med. 1999;7:257–9. [PubMed] [Google Scholar]
- 54.Durek C, Rüsch-Gerdes S, Jocham D, et al. Sensitivity of BCG to modern antibiotics. Eur Urol. 2000;37(Suppl 1):21–5. doi: 10.1159/000052378. [DOI] [PubMed] [Google Scholar]


