Abstract
Priapism is a rare event that may be induced by clinical conditions and medications. Ischemic priapism (IP) is a compartment syndrome of the penis, and it constitutes a medical emergency that may cause significant morbidity on the erectile function in particular. We report a case of a 30-year-old male in his fourth episode of priapism. The aspiration and washing of the corpora cavernosa with saline solution were performed, followed by washing with adrenaline solution without resolution of the condition. Treatment was followed by the performance of the Al-Ghorab shunt procedure with dorsal incision of the glans. During follow-up, an area of necrosis distal to the incision was detected, and after the catheter removal on postoperative day 14, the patient developed a glandular dorsal urethrocutaneous fistula and meatal stenosis. The meatal stenosis was corrected by Johanson urethroplasty with a neo-meatus at the coronal sulcus, along with resection and debridement of the fistula tract and a three-layer closure.
Introduction
Priapism is a rare event that may be induced by clinical conditions and medications. Ischemic priapism (IP) is a compartment syndrome of the penis, and it constitutes a medical emergency that may cause significant morbidity, particularly on the erectile function.
Aspiration and washing of the corpora cavernosa with or without sympathomimetic drug administration and the performance of cavernospongiosal shunts, in non-responsive cases, are treatment options in the event of IP. Although erectile dysfunction is a frequent consequence, in general the surgical procedure does not present significant complications.
Case report
A 30-year-old male patient was admitted with painful a penile erection lasting 20 hours. The erection was unrelated to sexual stimuli, perineal or genital trauma or the administration of intracavernous drug injections. The patient made use of valproic acid, clonazepam, haloperidol and levomepromazine to treat his schizophrenia, and he had already had 3 previous episodes of priapism, which resolved by puncture-aspiration of the corpora cavernosa.
On the physical examination, the penis was erect with full and painful tumescence of the corpora cavernosa and flaccid glans. The blood gasometry in the corpora cavernosa was consistent with an ischemic pattern (pH 7.2; pCO2 86 mmHg; pO2 38 mmHg).1 The aspiration and washing of the corpora cavernosa with saline solution were performed, followed by washing with adrenaline solution (1:1000) without resolution of the condition.
Treatment was followed by the performance of the Al-Ghorab shunt procedure,2 with dorsal incision of the glans and biopsy of the corpora cavernosa. There was an inadvertent injury of the urethral glans, which was sutured during the intraoperative period. The patient evolved to proper penile detumescence and was discharged with an indwelling urinary catheter on postoperative day 2.
The anatomopathological analysis of the biopsied material showed a focal area of necrosis and the presence of venous blood clots.
During the ambulatory follow-up, an area of necrosis distal to the incision was detected, and after the catheter removal on postoperative day 14, the patient developed a dorsal glandar urethrocutaneous fistula and meatal stenosis.
To access the urethral orifice of the fistulae, a ventral urethrotomy was performed. Since it was a distal defect, we opted for a definitive Johanson urethroplasty procedure, with a coronal neo-meatus, along with resection and debridement of the fistula tract and a three-layer closure (Fig. 1).
Fig. 1b.
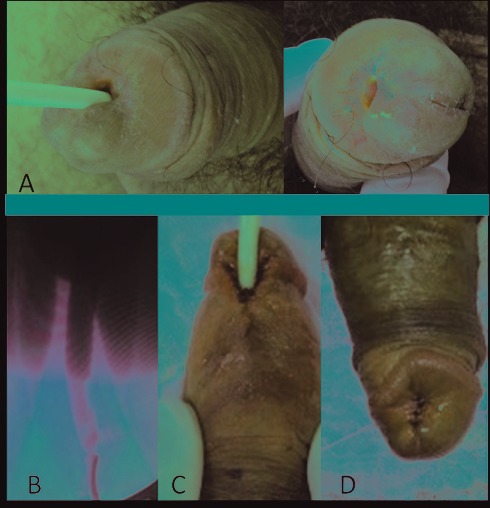
A: Dorsal aspect of the urethrocutaneous fistula associated with meatal stenosis; B: Intraoperative retrograde urethrography with no evidence of fistula in the corpus cavernosum; C: Final aspect of Johanson urethroplasty; D: Final aspect of dorsal closure of the fistula.
Discussion
About 95% of priapism cases are ischemic. These cases are a medical emergency which, if not properly and rapidly diagnosed and treated, may cause ischemia, acidosis and fibrosis of the corpora cavernosa with irreversible damage 4 to 6 hours after the event.1 In long-lasting cases, there may be necrosis in the corpora cavernosa.1
In only 40% of the cases the cause of IP can be identified. In this current report, the psychiatric drugs used by the patient may have triggered the process. The therapeutic option was based on the diagnosis of the type of priapism.3
Less than one third of IP cases respond to conservative treatment or the simple aspiration and washing of the corpora cavernosa with saline solution.4 However, the success rate of washing the corpora cavernosa with sympathomimetic agents may reach 80%.5 The distal cavernospongiosal shunt is the technique applied whenever the above-mentioned methods fail. All the surgical approaches employed in the early management of priapism aim to preserve the erectile function, evaluating the risk of early and late complications.6
Surgical complications are unusual, and fistula occurrences after a cavernospongiosal shunt procedure are even more uncommon. El-Bahnasawy and colleagues7 included 50 patients with a diagnosis of ischemic priapism in a study and only 1 patient evolved to urethro-cutaneous fistula. Other complications were infection (2 patients), bleeding (2 patients), localized skin necrosis (1 patient), partial glanular sloughing (1 patient) and tunica albuginea herniation (1 patient). Urethrocutaneous and urethro-caverno-cutaneous fistula cases have also been reported.9 It is believed that the fistula may occur due to an inadvertent urethral injury10 or to ischemia of the adjacent tissues.9 In this case, besides the intraoperative urethral injury, the biopsy of the corpora cavernosa showed an area of necrosis.
In the surgery, the incision had been made in third proximal glans, with easy access to the cavernous body, but it could increase the risk of urethra fistula in a tissue that had been exposed to a long period of ischemia.
In our patient, we opted for the Johanson surgery because he had a previous postectomy and the biopsy result of cavernous body had necrosis, which could represent a poor irrigation to an island flap. Besides that, the Johanson surgery with meatus in corona is very functional and after another procedure can repair this hypospadia state.
Conclusion
Urethrocutaneous fistula after cavernospongiosal shunt procedure as a result of ischemic priapism is a rare event that may occur due to ischemic etiology and/or a surgical trauma.
Footnotes
Competing interests: Dr. Paladino, Dr. Wroclawski, Dr. Den Julio, Dr. Teixeira, Dr. Glina and Dr. Pompeo all declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Tay YK, Spernart D, Rzetelski-West K, et al. Acute management of priapism in men. BJU Int. 2012;109:15–21. doi: 10.1111/j.1464-410X.2012.11039.x. [DOI] [PubMed] [Google Scholar]
- 2.Hanafy HM, Saad SM, El-Rifaie M, et al. Early Arabian medicine: Contribution to urology. Urology. 1976;8:63–7. doi: 10.1016/0090-4295(76)90059-5. [DOI] [PubMed] [Google Scholar]
- 3.Dangle PP, Patel MB, Pandya LK, et al. A modified surgical approach to the Al-Ghorab shunt – an anatomical basis. BJU Int. 2012;109:1872–4. doi: 10.1111/j.1464-410X.2012.11253.x. [DOI] [PubMed] [Google Scholar]
- 4.Montague DK, Jarow J, Broderick GA, et al. American Urological Association guideline on the management of priapism. J Urol. 2003;170:1318–24. doi: 10.1097/01.ju.0000087608.07371.ca. [DOI] [PubMed] [Google Scholar]
- 5.Kulmala RV, Tamella TL. Effects of priapism lasting 24 hours or longer caused by intracavernosal injection of vasoactive drugs. Int J Impot Res. 1995;7:131–6. [PubMed] [Google Scholar]
- 6.Burnett AL. Surgical management of ischemic priapism. J Sex Med. 2012;9:114–20. doi: 10.1111/j.1743-6109.2011.02446.x. [DOI] [PubMed] [Google Scholar]
- 7.El-Bahnasawy MS, Dawood A, Farouk A. Low-flow priapism: risk factors for erectile dysfunction. BJU Int. 2001;89:285–90. doi: 10.1046/j.1464-4096.2001.01510.x. [DOI] [PubMed] [Google Scholar]
- 8.Robbins DM, Crawford ED, Lackner HL. Late development of urethrocavernous fistula after cavernospongiosum shunt for priapism. J Urol. 1984;132:126–7. doi: 10.1016/s0022-5347(17)49496-1. [DOI] [PubMed] [Google Scholar]
- 9.De Stefani S, Savoca G, Ciampalini S, et al. Urethrocutaneous fistula as a severe complication of treatment for priapism. BJU Int. 2001;88:642–3. doi: 10.1046/j.1464-4096.2001.02400.x. [DOI] [PubMed] [Google Scholar]
- 10.Reddy MJ, Bhat VN, Rao KM, et al. Urethro-caverno-cutaneous fistula with distal urethral stricture and aberrant voiding into corpora cavernosa. Urology. 1980;15:593–5. doi: 10.1016/0090-4295(80)90375-1. [DOI] [PubMed] [Google Scholar]


