Abstract
AIM
To evaluate the accuracy of 20 MHz immersion B-scan ultrasonography in observing lens and to investigate the value of this noninvasive preoperative diagnosis method in alkali burn eyes.
METHODS
It was a comparative study. Fifty-six cases (56 eyes) of alkali burn eyes were examined by ultrasound biomicroscopy (UBM) and immersion 20 MHz B-scan ultrasonography from June 2011 to April 2013, the images were analyzed, and the ultrasonographic diagnosis compared with the operation results.
RESULTS
In 56 alkali burn eyes examined by UBM, the lens were not detected in 16 eyes; the IOL could be detected in 2 eyes; the anterior lens capsule surface or/and the front lens could be detected in 18 eyes, and lens opacification in 3 eyes of them; suspected abnormal lens were detected in the other 20 eyes. In all the same eyes examined by immersion 20 MHz B-scan ultrasonography, the lens were not detected in 16 eyes; the IOL could be detected in 2 eyes; 24 abnormal lens (opacity, lens expansion, shrinkage) and 14 normal lens were found. Compared with the intraoperative findings, the diagnostic accordance rate of the immersion 20 MHz B-scan appearance of lens was 100% (56/56), which was significantly higher than examined by UBM 57.14% (32/56) (χ2=30.55, P=0.0000).
CONCLUSION
Immersion 20 MHz B-scan ultrasonography can observe the lens accurately in alkali burn eyes. It has important clinical value to combine with UBM in eyes of alkali burn.
Keywords: immersion, B-scan, ultrasonography, alkali burn, ultrasound biomicroscopy
INTRODUCTION
Alkali burns is a serious and common disease cause of blindness in undeveloped and developing countries such as China and the vast majority of patients injured both of their eyes[1]. The alkali can cause devastating injuries to the anterior segment. The consequences of alkali injuries are notoriously severe due to the rapid penetration of these agents into the ocular tissues[2]–[6], and keratoplasty or artificial cornea transplant operation is the last hope for severe cases[7],[8]. The preoperative accurate exploration on lens is directly related to the design and operation condition of the assessment scheme. Though the ultrasound biomicroscopy (UBM) is the common method for observation of the anterior segment of the alkali burn eyes in clinic, the lens can only be partially or completely cannot be observed in most patients due to the limit of depth inspection of the UBM and the severe tissue damage of the anterior segment[9]–[12]. At present, the 20 MHz B-scan ultrasonography, because of its good resolution and better penetration, is gradually popularized in the clinical application, and it can probably observe the whole lens. In this study, 56 eyes from 56 patients scheduled to undergo keratoplasty or artificial cornea transplant operation are consecutively selected as the study object to evaluate the accuracy of 20 MHz immersion B-scan ultrasonography in observing the lens and to investigate the value of this noninvasive preoperative diagnosis method in the alkali burn eyes.
SUBJECTS AND METHODS
Subjects
In this prospective study, 56 consecutive patients scheduled to undergo artificial cornea transplant operation or keratoplasty in the Chinese People's Liberation Army General Hospital from June 2011 to May 2013 were recruited. The sample included 54 men and 2 women with an average age of 46.5±15.6 (range, 27-65y), and the course of alkali burn was from 1.2-6.5y. Of the 56 cases, 6 cases were lime burning, 9 cases were potassium hydroxide burning, 25 cases were sodium hydroxide burning, 10 cases were liquid aluminum burning and 6 cases were ammonia burning. Patients with fistula cornea or severe symblepharon were excluded from this study. All participants provided written informed consent in accordance with the Declaration of Helsinki via protocols approved by the appropriate Institutional Review Board.
The anterior segment organization of all the eyes were examined by two methods: immersion 20 MHz B-scan ultrasonography (SW-2100, A/B-mode ultrasound: A super-probe frequency, 20 MHz, SUOER, China), and the UBM (SW-3200, SUOER, China) with a 50 MHz transducer-probe allowing 15×9-mm2 tissue penetration and approximately 50 mm resolution.
Each eye was examined on the same day firstly by UBM, then by immersion 20 MHz B-scan ultrasonography. One examiner performed all the examination with the UBM and another examiner performed all the examination with the immersion 20 MHz B-scan ultrasonography. The images of the horizontal and vertical axial scanning of the two ultrasonography methods were collected and analyzed when the patients look forward.
Methods
Ultrasound biomicroscopy
UBM was performed with a gain of about 75 dB. After the cornea surface anesthesia, a Hansen immersion shell was placed on the ocular surface and slowly injected with saline, the UBM probe was inserted into the immersion shell about 5 mm from the cornea. Patients were asked to look forward and to adjust their eye positions according to the UBM images. When the ideal eye position was obtained, the image was frozen.
Immersion 20 MHz B-scan ultrasonography
It was performed with a gain of 70 dB to 95 dB and the vector A sampling line located in the center of the screen. After the cornea surface anesthesia, a Hansen immersion shell was placed on the ocular surface and slowly injected with saline, the B-mode ultrasound probe was inserted into the immersion shell 15-25 mm from the cornea. Patients were asked to watch the center of the probe and to adjust their eye positions according to B-mode ultrasound images. When the ideal eye position was obtained, the image was frozen.
Assessment method
The observation of the lens in the operation was settled as the gold standard and then contrast analysis was made on ultrasonographic diagnosis and operative results of the lens. The assessment contents included normal lens, aphakia, abnormal lens (malposition, deformity, internal echo anomaly and integrity of the lens have been destroyed etc. At least one of the above-mentioned aspects misdiagnosis and missed diagnosis was considered diagnosis inconsistency).
UBM appearance of normal lens: band-echo of anterior lens capsule and the posterior lens capsule or just the band-echo of anterior capsule could be detected and other area showed as free-echo after the anterior lens capsule (Figure 1A, Figure 2A); intraocular lens: parallel ribbon high echo in the posterior chamber (Figure 3A); aphakic eyes: band-echo of anterior lens capsule behind the pupil and iris cannot be detected (Figure 4A); lens opacification in normal place: the area behind the band-echo of anterior lens capsule showed as markedly inhomogeneous enhancement showed; suspected lens: inhomogeneous enhanced echo mass behind the cornea with or without band-echo of anterior lens capsule (Figure 5A, Figure 6A), or inhomogeneous enhenced echo mass behind the pupil and iris without band-echo of anterior lens capsule (Figure 7A).
Figure 1. Normal lens with no alkali burns.
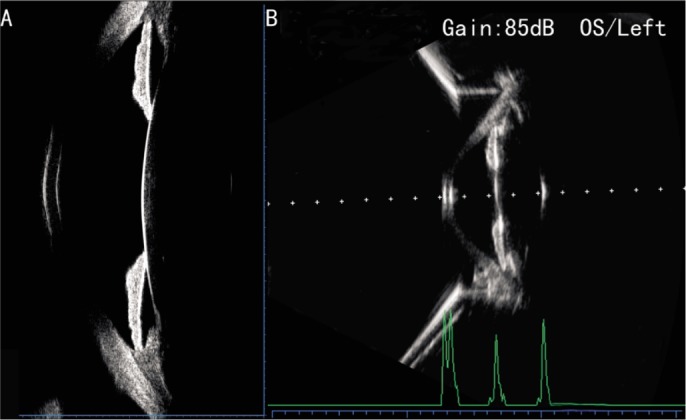
A: Normal lens image on the UBM in normal people; B: Normal lens image on the immersion 20 MHz B-scan ultrasonography in the same normal people.
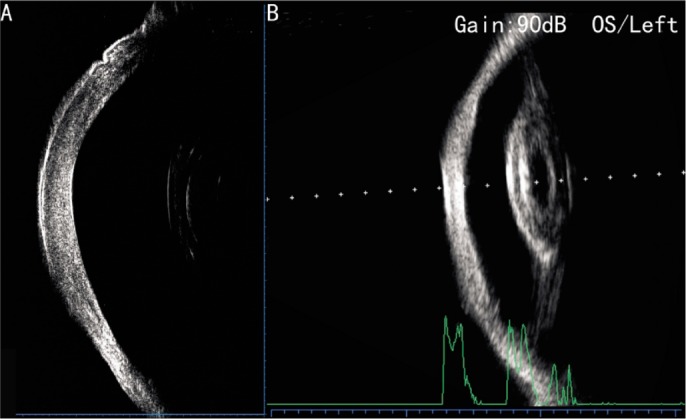
Figure 2. Normal lens in patients with alkali burns.
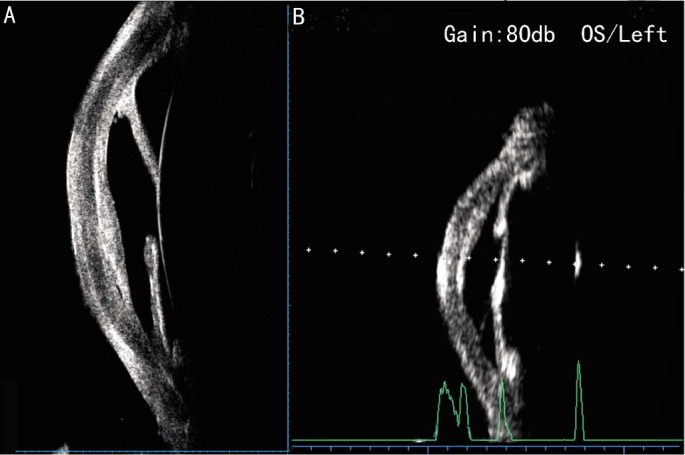
A: Normal lens image on the UBM in ocular alkali burns patients; B: Normal lens image on the immersion 20 MHz B-scan ultrasonography in the same ocular alkali burns patients.
Figure 3. Intraocular lens in patients with alkali burns.
A: Intraocular lens image on the UBM in ocular alkali burns patients; B: Intraocular lens image on the immersion 20 MHz B-scan ultrasonography in the same ocular alkali burns patients.
Figure 4. Aphakia in patients with alkali burns.
A: Aphakia image on the UBM in ocular alkali burns patients; B: Aphakia image on the immersion 20 MHz B-scan ultrasonography in the same ocular alkali burns patients.
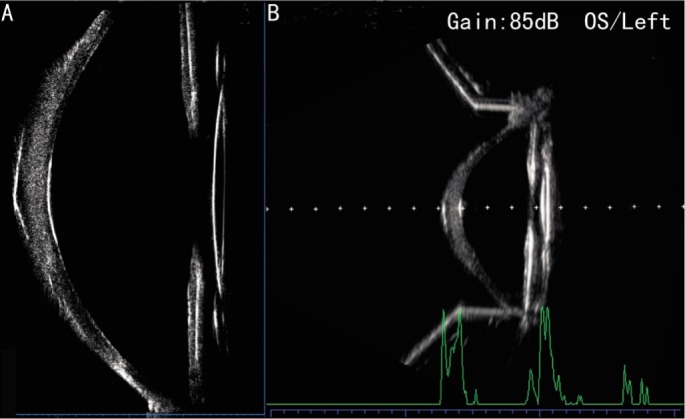
Figure 5. Lens opacification in patients with alkali burns.
A: Suspected lens opacification without the image of the iris on the UBM in ocular alkali burns patients; B: Lens opacification image on the immersion 20 MHz B-scan ultrasonography in the same ocular alkali burns patients.
Figure 6. Lens opacification and intumescent in patients with alkali burns.
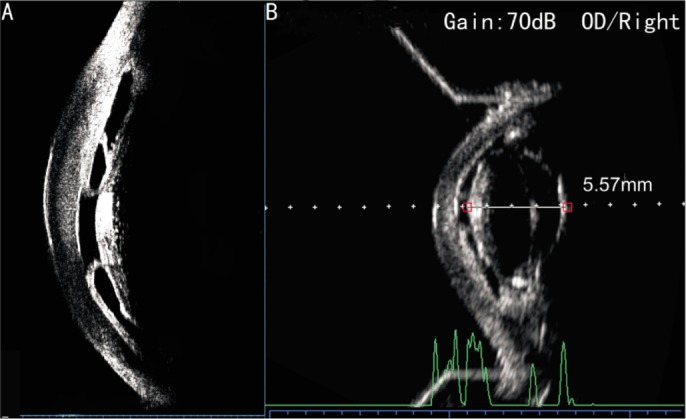
A: Suspected lens opacification with lens malposition image on the UBM in ocular alkali burns patients; B: Lens opacification and intumescent image on the immersion 20 MHz B-scan ultrasonography in the same ocular alkali burns patients, and the thickness of the lens was 5.57 mm.
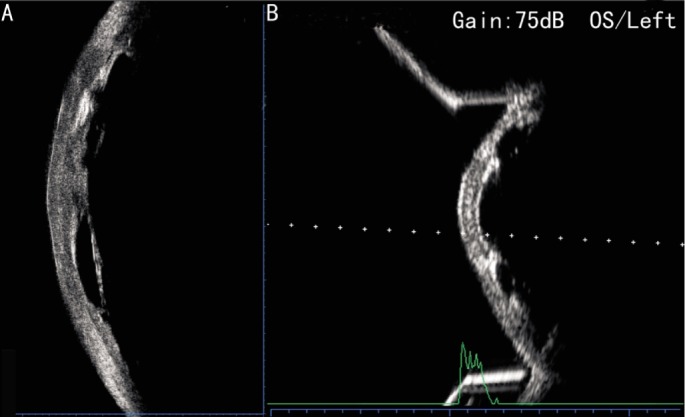
Figure 7. Lens pyknosis in patients with alkali burns.
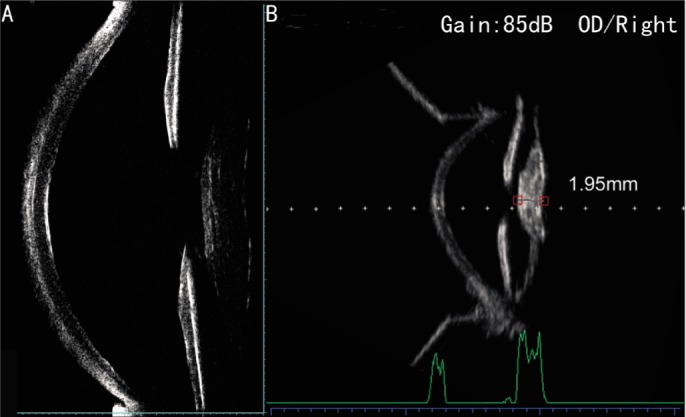
A: Suspected lens opacification without band-echo of anterior lens capsule image on the UBM in ocular alkali burns patients; B: Lens pyknosis image on the immersion 20 MHz B-scan ultrasonography in the same ocular alkali burns patients, and the thickness of the lens was 1.95 mm.
Immersion B-scan appearance of normal lens: band-echo of anterior lens capsule and the posterior lens capsule behind the pupil and iris, internal of the lens take the form of free-echo area (Figure 1B, Figure 2B); intraocular lens: parallel ribbon high echo in the posterior chamber (Figure 3B); aphakic eyes: band-echo of anterior lens capsule and the posterior lens capsule behind the pupil and iris cannot be detected (Figure 4B); lens opacification: the internal echo of the lens uneven enhanced (Figure 5B, Figure 6B); lens intumescent: the thickness of the lens great than 5 mm (Figure 6B); lens pyknosis: the thickness of the lens equal to or less than 3 mm (Figure 7B).
Statistical Analysis
The evaluation includes coincidental diagnosis rates and misdiagnosis/missed diagnosis rates between ultrasound diagnosis and surgical results. The diagnostic rate is the ratio of the ultrasound diagnosis consistent with the surgical results, and the misdiagnosis/missed diagnosis rates were the ratio of the ultrasound diagnosis inconsistent with the surgical results. Chi-square was used to compare the coincidental rate of the two ultrasound methods with the surgical results, then the accuracy of 20 MHz immersion B-scan ultrasonography in observing the lens was evaluated and the value of this noninvasive preoperative diagnosis method in the alkali burn eyes was investigated. All data were analyzed by SPSS 12.0 v12.0 statistical software (SPSS Inc., Chicago, IL, USA) and the statistical level of significance was preset at 0.05.
RESULTS
All operations were performed successfully and the patients' main details at the time of treatment and the best corrected postoperative visual acuity were summarized in Table 1.
Table 1. Characteristics of study population.
| Parameters | Characteristics |
| Age (a) | 27-65 (46.5±15.6) |
| Gender (F/M) | 2/54 |
| Course of disease (a) | 1.2-6.5 |
| Operation history (of the injured eyes) (Yes/No) | 33/23 |
| Binocular alkali burns (Yes/No) | 52/2 |
| Surgical method | Keratoplasty 2 eyes/artificial cornea transplant 54 eyes |
| Uncorrected visual acuity (UCVA) | Light perception (LP) -hand movement (HM) |
| Best corrected postoperative visual acuity | 0.05-0.8 |
In 56 alkali burn eyes examined by UBM, the lens were not detected in 16 eyes; the IOL were detected in 2 eyes; the anterior lens capsule surface or/and the front lens were detected in 18 eyes, and lens opacification in 3 eyes of them; suspected abnormal lens were detected in the other 20 eyes. In all the same eyes examined by immersion 20 MHz B-scan ultrasonography, the lens were not detected in only 16 eyes; the IOL were detected in 2 eyes; 24 abnormal lens (opacity, lens expansion, shrinkage) and 14 normal lens were found. The comparison of the diagnosis between the two ultrasound methods with surgical results was presented in Table 2. Compared with the intraoperative findings, the diagnostic accordance rate of the immersion 20 MHz B-scan appearance of lens was 100% (56/56), which was higher than examined by UBM 57.14% (32/56), and the difference had statistical significance (χ2=30.55, P=0.0000). The comparison of the diagnostic value between the two ultrasonic methods with the surgical results were presented in Table 3.
Table 2. Comparison of the diagnosis between the two ultrasound methods with surgical results.
| UBM diagnosis | Immersion ultrasonography diagnosis | Surgical results |
| Normal lens in 15 eyes | Normal lens in 12 eyes, lens intumescent in 3 eyes | Lens clear in 12 eyes, lens intumescent in 3 eyes |
| Aphakia in16 eyes | Aphakia in 16 eyes | Aphakia in 16 eyes |
| Intraocular lens in 2 eyes | Intraocular lens in 2 eyes | Intraocular lens in 2 eyes |
| Lens opacification in normal place in 3 eyes | Lens opacification in 3 eyes(lens intumescent in 1 eye) | Lens opacification in 3 eyes (lens intumescent 1 eye) |
| Suspected lens opacification with lens malposition in 4 eyes | Lens opacification, intumescent and in malposition in 4 eyes | Lens opacification and intumescent in 4 eyes |
| Suspected lens opacification in normal place in 16 eyes | Lens opacification in 14 eyes, lens pyknosis in 2 eyes | Lens opacification in 14 eyes, lens pyknosis in 2 eyes |
Table 3. Comparison of the diagnostic value between the two ultrasonic methods with the surgical results.
| Evaluation content | UBM diagnosis | Immersion ultrasonography diagnosis | χ2; P |
| Coincidental diagnosis rates | 32/56 (57.14%) | 56/56 (100%) | 30.55; 0.0000 |
| Misdiagnosis/missed diagnosis rates | 10/56 (17.86%) | 0/56 (0%) | 8.89; 0.0029 |
| Suspected diagnosis rates | 16/56 (28.57%) | 0/56 (0%) | 116.41; 0.0001 |
DISCUSSION
Ocular alkali burn is a common and serious diseases in China, and the chemical and thermal burns can cause devastating injuries to the anterior segment. The consequences of alkali injuries are notoriously severe due to the rapid penetration of these agents into the ocular tissues[1]–[6]. Penetration of alkali into the corneal stroma may result in loss of keratocytes, endothelial damage, and loss of proteoglycan from the stroma. Collagen shrinkage may cause an acute spike in intraocular pressure, whereas fragmentation products of the denatured stroma may be chemotactic to neutrophils, which in turn release mediators that recruit more inflammatory cells. Alkali in the anterior chamber can cause iris ischaemia with a fixed dilated pupil, raise intraocular pressure, or secondary hypotony from damage to the ciliary body. Extremely severe injuries may precipitate acute cataract[3]–[6]. Denaturation of tissue, inflammation, and scarring leads to loss of function. In this study, most of the patient were young, and 96.43% (54/56) patients injured both of their eyes, with visual acuity between light perception (LP) and hand movement (HM). In clinic, the treatment is extremely difficult, penetrating keratoplasty or implantation of artificial cornea is the last choice to regain one's sight for the serve case[7],[8],[13]–[20]. Then, the ocular anterior segment of the alkali burns eyes include a comprehensive exploration of the lens is the important basis of the assessment and selection of surgical planning.
Because of the corneal stroma scars, corneal neovascularization (CNV), or even the symblepharon due to the alkali burns, the observation with the slit-lamp microscope is very limited in clinic. In recent years, with the UBM being widely used in clinic, the anterior segment organization is clearly observed because of its ultrasonic frequency of up to about 50 MHz. In normal eyes, the UBM allows imaging of anatomic areas of interest in the anterior segment, the posterior capsule of the lens can be observed comprehensively[9]–[12],[21]. However, in the alkali burn eyes with corneal stroma scars or normal lens, the posterior capsule of the lens ofen cannot be observed by UBM due to its limited penetration. In this study, when the 56 alkali burns eyes were observed with the UBM, only the two eyes with intraocular lens could be observed completely; of the 15 normal lens in UBM diagnosis, surgical results showed that only 12 (12/15, 80%) eyes with normal lens; of the 4 cases suspected lens opacification with lens malposition in 4 eyes in UBM diagnosis, surgical results showed that all they were lens intumescent, the missed diagnosis rate was 100% (4/4), and all these results are due to the probing depth limit of the rganization with the UBM and the serious destruction of the anterior segment tissue.
The B-scan ultrasonography plays an important role in clinical diagnosis of ophthalmologic diseases, and it has many advantages, such as it is convenient, inexpensive, non-invasive and dynamic real-time observation, especially in diagnosing patients with cloudy refractive media, such as corneal edema, hyphema, lens opacity, vitreous opacity etc or patients with eyes opening difficult because of eyelid edema[22],[23]. It also plays a unique role in compensating for optical inspection methods such as slit-lamp, OCT and ophthalmoscopy insufficient[24]. The 20 MHz B-scan ultrasonography, because of its good penetration, higher resolutions than the 10 MHz B-scan ultrasonography, and improved diagnostic capacity, the contact method of it become more and more popular in the diagnosis of eye macular diseases, ocular trauma[25],[26]. And the immersion method, which avoids the near field interference, will allow the probe to be offset from the eye sufficiently to place the anterior segment in the focal plane to observe the anterior segment includes the whole lens clearly. In this study, the diagnosis of the lens in the alkali burns eyes by 20 MHz B-scan ultrasonography were all confirmed with surgical results, when used for observation of the lens, the immersion 20 MHz B-scan ultrasonography could clearly demonstrate the size, shape, characteristic of an echo and the surrounding structures as well.
However, this study still has a limitation that we would like to mention: we hadn't compared the observation of the details of the anterior segment structures (like, the cornea, anterior chamber, anterior chamber angle) between by the immersion 20 MHz B-scan ultrasonography or by the UBM.
In conclusion, in treating patients with ocular alkali burns, the immersion 20 MHz B-scan ultrasonography had important clinical practical value when combined with the UBM, which could observe theanterior segment structures include the whole lens, based on which to assess the severity and to select the method of operation to recover the eyesight.
Acknowledgments
The authors want to thank Zhang MN, MD for his careful reading of the manuscript and his useful comments and suggestions.
Foundations: Supported by National Key Basic Research Program of China (973 Program, No.2013CB967001); National Natural Science Foundation of China (No.81271052, No.31271059)
Conflicts of Interest: Yang QH, None; Chen B, None; Wang LQ, None; Li ZH, None; Huang YF, None.
REFERENCES
- 1.Singh P, Tyagi M, Kumar Y, Gupta KK, Sharma PD. Ocular chemical injuries and their management. Oman J Ophthalmol. 2013;6(2):83–86. doi: 10.4103/0974-620X.116624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuft SJ, Shortt AJ. Surgical rehabilitation following severe ocular burns. Eye (Lond) 2009;23(10):1966–1971. doi: 10.1038/eye.2008.414. [DOI] [PubMed] [Google Scholar]
- 3.Paterson CA, Pfister RR. Ocular hypertensive response to alkali burns in the monkey. Exp Eye Res. 1973;17(5):449–453. doi: 10.1016/0014-4835(73)90225-x. [DOI] [PubMed] [Google Scholar]
- 4.Paterson CA, Pfister RR. Intraocular pressure changes after alkali burns. Arch Ophthalmol. 1974;91(3):211–218. doi: 10.1001/archopht.1974.03900060219014. [DOI] [PubMed] [Google Scholar]
- 5.Pfister RR, Haddox JL, Sommers CI, Lam KW. Identification and synthesis of chemotactic tripeptides from alkali-degraded whole cornea. A study of N-acetyl-proline-glycine-proline and N-methyl-proline-glycine-proline. Invest Ophthalmol Vis Sci. 1995;36(7):1306–1316. [PubMed] [Google Scholar]
- 6.Sotozono C, He J, Matsumoto Y, Kita M, Imanishi J, Kinoshita S. Cytokine expression in the alkali-burned cornea. Curr Eye Res. 1997;16(7):670–676. doi: 10.1076/ceyr.16.7.670.5057. [DOI] [PubMed] [Google Scholar]
- 7.Liu C, Hille K, Tan D, Hicks C, Herold J. Keratoprosthesis surgery. Dev Ophthalmol. 2008;41:171–186. doi: 10.1159/000131088. [DOI] [PubMed] [Google Scholar]
- 8.Chen JQ, Zhai JJ, Gu JJ, Shao YF, Liu YM, Yuan J, Zhou SY. Preliminary study of Boston keratoprosthesis in treatment of severe late stage ocular chemical burns. Zhonghua Yan Ke Za Zhi. 2012;48(6):537–541. [PubMed] [Google Scholar]
- 9.Kunimatsu S, Araie M, Ohara K, Behrens-Baumann W. Ultrasound biomicroscopy of ciliary body cysts. Am J Ophthalmol. 1999;127(1):48–55. doi: 10.1016/s0002-9394(98)00308-0. [DOI] [PubMed] [Google Scholar]
- 10.Marigo FA, Esaki K, Finger PT, Ishikawa H, Greenfield DS, Liebmann JM, Ritch R. Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology. 1999;106(11):2131–2135. doi: 10.1016/S0161-6420(99)90495-5. [DOI] [PubMed] [Google Scholar]
- 11.McWhae JA, Rinke M, Crichton AC. Multiple bilateral iridociliary cysts: ultrasound biomicroscopy and clinical characteristics. Can J Ophthalmol. 2007;42(2):268–271. [PubMed] [Google Scholar]
- 12.Minavi AZ, Holdeman NR. Peripheral pigmentary iris cyst: evaluation and differential diagnosis. Clin Exp Optom. 2007;90(1):49–52. doi: 10.1111/j.1444-0938.2006.00087.x. [DOI] [PubMed] [Google Scholar]
- 13.Al Arfaj K, Hantera M. Short-term visual outcomes of Boston keratoprosthesis type I in saudi arabia. Middle East Afr J Ophthalmol. 2012;19(1):88–92. doi: 10.4103/0974-9233.92121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunlap K, Chak G, Aquavella JV, Myrowitz E, Utine CA, Akpek E. Short-term visual outcomes of Boston type 1 keratoprosthesis implantation. Ophthalmology. 2010;117(4):687–692. doi: 10.1016/j.ophtha.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Ilhan-Sarac O, Akpek EK. Current concepts and techniques in keratoprosthesis. Curr Opin Ophthalmol. 2005;16(4):246–250. doi: 10.1097/01.icu.0000172829.33770.d3. [DOI] [PubMed] [Google Scholar]
- 16.Khan B, Dudenhoefer EJ, Dohlman CH. Keratoprosthesis: an update. Curr Opin Ophthalmol. 2001;12(4):282–287. doi: 10.1097/00055735-200108000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Sayegh RR, Avena DL, Vargas-Martin F, Webb RH, Dohlman CH, Peli E. Optical functional properties of the Boston Keratoprosthesis. Invest Ophthalmol Vis Sci. 2010;51(2):857–863. doi: 10.1167/iovs.09-3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan BF, Harissi-Dagher M, Khan DM, Dohlman CH. Advances in Boston keratoprosthesis: Enhancing retention and prevention of infection and inflammation. Int Ophthalmol Clin. 2007;47(2):61–71. doi: 10.1097/IIO.0b013e318036bd8b. [DOI] [PubMed] [Google Scholar]
- 19.Zerbe BL, Belin MW, Ciolino JB. Results from the multicenter Boston Type 1 Keratoprosthesis Study. Ophthalmology. 2006;113(10):1779.e1–7. doi: 10.1016/j.ophtha.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 20.Chew HF, Ayres BD, Hammersmith KM, Rapuano CJ, Laibson PR, Myers JS, Jin YP, Cohen EJ. Boston keratoprosthesis outcomes and complications. Cornea. 2009;28(9):989–996. doi: 10.1097/ICO.0b013e3181a186dc. [DOI] [PubMed] [Google Scholar]
- 21.Ursea R, Silverman RH. Anterior-segment imaging for assessment of glaucoma. Expert Rev Ophthalmol. 2010;5(1):59–74. doi: 10.1586/eop.09.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dastevska-Djosevska Ultrasonography in ocular trauma. Prilozi. 2013;34(2):105–113. [PubMed] [Google Scholar]
- 23.Dehghani A, Giti M, Akhlaghi MR, Karami M, Salehi F. Ultrasonography in distinguishing optic neuritis from nonarteritic anterior ischemic optic neuropathy. Adv Biomed Res. 2012;1:3. doi: 10.4103/2277-9175.94425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia JP, Jr, Rosen RB. Anterior segment imaging: optical coherence tomography versus ultrasound biomicroscopy. Ophthalmic Surg Lasers Imaging. 2008;39(6):476–484. doi: 10.3928/15428877-20081101-02. [DOI] [PubMed] [Google Scholar]
- 25.Perry LJ. The evaluation of patients with traumatic cataracts by ultrasound technologies. Semin Ophthalmol. 2012;27(5–6):121–124. doi: 10.3109/08820538.2012.712733. [DOI] [PubMed] [Google Scholar]
- 26.Tabatabaei A, Kiarudi MY, Ghassemi F, Moghimi S, Mansouri M, Mirshahi A, Kheirkhah A. Evaluation of posterior lens capsule by 20-MHz ultrasound probe in traumatic cataract. Am J Ophthalmol. 2012;153(1):51–54. doi: 10.1016/j.ajo.2011.05.038. [DOI] [PubMed] [Google Scholar]


