Abstract
The National Strategy for Suicide Prevention (2012) has set a goal to reduce suicides by 20% within 5 years. Suicide rates are higher in older adults compared to most other age groups, and the majority of suicide completers have visited their primary care physician in the year before suicide. Primary care is an ideal setting to identify suicide risk and initiate mental health care. We review risk factors for late-life suicide; methods to assess for different levels of suicidality; and recent research developments regarding both effective assessment and management of suicide risk among older primary care patients. We highlight that broader scale screening of suicide risk may be considered in light of findings that suicidality can occur even in the absence of major risk factors like depression. We also highlight collaborative care models targeting suicide risk, and recent innovative interventions that aim to prevent the development of suicidal ideation and suicidal behavior.
Keywords: suicide, suicidal ideation, depression, primary care, geriatrics, screening, assessment, management
Introduction
Roughly 1% of Americans will die by suicide [1]. In both the U.S. and internationally, suicide rates are among the highest for older adults [2–4]. Older men account for considerably more suicide deaths than do older women [4] The World Health Organization has estimated suicide rates among those aged 75 and to be 50/100,000 for men and 16/100,000 for women [5].
The 2012 National Strategy for Suicide Prevention [6] has set as its goal to reduce suicides by 20% within 5 years, and by 40% within 10 years. The National Strategy identified four immediate priorities: integrate suicide prevention into health care policies; encourage transformation of health care systems to prevent suicide; change the way the public talks about suicide and suicide prevention; and improve quality of data on suicidal behaviors to develop increasingly effective prevention efforts.
A central premise of this article is that suicidality exists on a continuum, with different types or degrees of suicidal ideation representing different levels of risk for suicide. “Suicidal ideation” can range from passive death wishes, to active thoughts of committing suicide, to having a specific detailed suicidal plan with intention to carry out the plan. “Suicidal behavior” has been defined as self-injurious acts with the intent of ending one’s life [7], whether these are unsuccessful attempts or completed acts. Although suicidal ideation is a risk factor for completed suicide, thoughts of death can be common among older adults and can function as normative reflections on mortality [8]. Statements from an older adult that he or she has been thinking about death require further assessment to determine whether these thoughts are non-pathological and can be seen as normative from a developmental perspective, or whether they are pathological thoughts reflecting passive death wishes, active suicidal ideation, or an imminent intention to commit suicide. As we will discuss, each level of risk requires a different corresponding immediate response and may require a different ongoing management plan.
While suicide is a relatively rare event, primary care is an ideal setting to identify suicide risk and initiate some type of care for many reasons. Primary care physicians are the most likely provider to see older adults with mental health problems, including those experiencing suicidal ideation. Older adults with mental health problems rarely see mental health specialists but often do present to their physician, with whom they prefer to discuss mood and other aspects of their mental health [9]. Rates of suicidal ideation are also somewhat higher among older adults in primary care settings than in general community samples, with estimates ranging from 1% to 10% depending on the assessment method used [10]. Such ideation has been linked to a variety of poor medical outcomes, including poor health related quality of life [11] and completed suicide [8]. Moreover, suicide completers often visit their physician in the month before suicide. Of those dying by suicide, approximately 45% will have seen their primary care provider within the month before their death, while only 20% will have seen a mental health professional in that period [12]. A recent large representative longitudinal study found that 83% of suicide victims received health care services in the year prior to death, and 50% received services in the month prior [13]. The most common services were primary care and medical specialty based, with women and individuals 65 and older more likely to make such a visit.
Because of these observations, physician guidelines developed by regulatory agencies and professional organizations recommend that physicians routinely screen for depressive symptoms. These guidelines recommend screening for suicide risk, however, only among patients who screen positive for depression or substance abuse [14, 15]. As we will describe below, however, recommendations concerning the specifics of when and whom to screen are up for debate.
In the remainder of this article, we review risk factors for suicide and highlight recent research in the area. We then describe standardized screening instruments and present recent research developments regarding effective assessment. We offer a practical guide for how to clinically assess different levels of suicidality among older adults. Finally, we discuss the management of suicide risk among primary care older adults and recent research in the area.
Risk Factors for Suicide and Suicidality
The majority of older adults who attempt or die by suicide suffer from depression [16–19]. Depression alone, however, does not account for all cases of suicidal ideation or attempts. Other established risk factors for suicide in older adults include history of serious suicidal ideation [20], functional impairment [17], stressful life events (such as loss of spouse) [21], substance abuse [22], and physical illness [19]. Among those with physical illnesses, risk of suicide is highest early in the course of treatment for serious medical illnesses such as end-stage renal disease and dialysis initiation [23].
Recent publications have shown significant rates of suicidal ideation among patients with and without depressive disorder [24]. In analyses of 1,226 older adult primary care participants in the PROSPECT study (Prevention of Suicide in Primary Care Elderly: Collaborative Trial), 29% of patients with major depression and 11% of those with minor depression endorsed a wish to die, while 7% with no depression endorsed such a wish. From a public health perspective, a sizable proportion of patients exhibiting suicidal ideation in the primary care population will not meet criteria for a depressive disorder. This somewhat surprising finding calls further attention to the benefits of broader scale screening efforts.
Van Orden et al [20] similarly examined the characteristics of adults aged 85 and older who reported death ideation in a population-based study in Sweden. Using latent class analysis, they found two distinct groups: those who also reported high levels of depression and anxiety, and those without such distress but who reported histories of active suicidal ideation. Recent studies have also found a high prevalence of suicidal ideation in mental health conditions other than depression. Using data from a large RCT of mixed-age primary care patients with anxiety disorders (mean age=43.5), Bomyea and colleagues found that 26% endorsed passive suicidal ideation in the past month, and 16% had specific thoughts about suicide [25]. And in a large cross-sectional study of mixed-age primary care patients with somatoform disorders (mean age=45.5), 23.9% reported active suicidal ideation during the previous 6 months and 17.6% reported a lifetime history of suicide attempt [26].
Other recent findings have identified additional risk factors for suicidal ideation and suicide, though all require replication in other samples. In a cross-sectional study of 816 veterans at 4 VA sites, Magruder and colleagues found that those who were unemployed because of disability or who served in a warzone were most likely to report suicidal ideation [27]. In a large primary care sample of older adults in Australia [28], Almeida and colleagues found independent associations between suicidal ideation and smoking, living alone, limited social support, not practicing religion, and use of antidepressants. And in a secondary analysis of older primary care patients, those living in census tracts in the lowest quartile of family income for the area were almost 5 times more likely to report recurrent thoughts of death or recurrent suicidal ideation than those from the highest income tracts [29]. Similarly, in the PROSPECT study both depression severity and rates of suicidal ideation were significantly greater in those with annual incomes below $20,000 and those reporting financial strain [30]. These studies point to the role of chronic social and economic inequalities on suicidal ideation [31]. Personality traits may also have a role; in a mixed-age sample of primary care patients, optimism/pessimism was a significant predictor of suicidal behavior in adults independent of depression symptoms [32].
Taken together, these findings indicate that while depression is a major risk factor for suicidality, suicidal ideation can also be present among non-depressed individuals. Research is warranted on suicide prevention interventions that target this group of older, non-depressed primary care patients [24]. Suicide prevention strategies should thus extend beyond the treatment of those with mood disorders to specifically target other modifiable suicide risk factors, such as low social support [28].
Assessing Suicidality in Primary Care
In this section, we focus specifically on the screening and assessment of suicidal ideation, with recognition that determination of suicide risk should also incorporate consideration of other risk factors as identified in the previous section. Screening for suicidal ideation may be most appropriate in populations with these known risk factors. As noted above, broader scale screening may also be considered in light of findings that suicidality can occur even in the absence of major risk factors like depression. Decisions on how often, and who to screen should consider the primary care population and resources available for such screening. The U.S. Preventive Services Task Force emphasizes the importance of access to appropriate mental health treatment following screening [14], and many have urged that these systems integrate more intensive mental health services [33] (see following section on Management of Suicidality in Primary Care).
Assessment of suicidality can be initiated via clinical interview or via structured screening instruments such as the Patient Health Questionnaire (PHQ) [34], one of the most commonly used measures of depression symptoms in the primary care sector. The PHQ inquires about how often depression symptoms have bothered the patient in the last two weeks, with response options of “Not at all,” “Several days,” “More than half the days,” and “Nearly every day.” The first two items (“little interest or pleasure in doing things” and “feeling down, depressed or hopeless”) constitute the PHQ-2 and are often used as an initial screen for major depression. Many primary care practices use a two-stage process in which a positive screen on the PHQ-2 necessitates follow up with the remaining 7 items of the PHQ-9. These items tap other symptoms of depression (e.g., low energy, sleep), while item 9 inquires about “thoughts that you would be better off dead, or of hurting yourself in some way.” While a two-stage approach is efficient for identifying depression, it may miss a significant number of older adults who experience suicide ideation in the absence of depression. The PHQ-2 and PHQ-9 have been well-validated in the U.S. [34], and recent psychometric studies have been conducted internationally [35–38].
Recent research in assessment of suicidal ideation
A number of recent studies have examined the predictive value and utility of the PHQ for identifying suicidal ideation. For example, Pratt and Brody [39] investigated the optimal cutoff on the PHQ-2 for identifying mixed-age community-dwelling individuals with any level suicidal ideation, specifically a positive endorsement of PHQ-9 item 9. While a score of 3 or higher on the PHQ-2 has been recommended to indicate a positive screen for major depression [40], using this cutoff failed to identify half of individuals with suicidal ideation. Lowering the cutoff to 2 identified 76% of individuals with suicidal ideation. Restricting the sample to patients 60 and older, a cutoff of 2 identified 68% of such individuals.
Inagaki et al [36] similarly examined the ability of the PHQ-2 to identify suicidal ideation in mixed-age (mean age=73) primary care patients in Japan. Among 54 (11.3%) patients endorsing suicidal ideation on item 9, only 40% screened positive for depression on the PHQ-2. The authors also examined the validity of the 9th item of the PHQ-9 in detecting suicidal ideation using semi-structured clinical interviews. They found that positive responses on item 9 yielded a sensitivity of 0.70 and specificity of 0.97, providing support for this item’s ability to accurately detect clinician-judged suicidal ideation. Taking the results of the Inagaki et al and Pratt and Brody studies together, a sizable proportion of patients with suicidal ideation will not be identified unless a suicide-specific measure such as item 9 of the PHQ-9 is used. These findings are consistent with calls for broader-scale suicide risk screening even among individuals without psychiatric disorder.
Other research regarding assessment of suicidal ideation in primary care has investigated use of novel technologies that support routine screening for suicidal ideation. Lawrence et al [41] implemented routine, patient-administered suicidal ideation screening using touch screen computerized technology in an HIV primary care setting (mean age=44). Patients who reported experiencing suicidal ideation “nearly every day” on PHQ-9 item 9 were considered to be at highest risk, triggering automatic notification to a response team who performed more detailed suicide risk assessments. Results indicated that 170 patients in the sample (14%) endorsed item 9 positively, with 33 (3%) endorsing such thoughts “nearly every day.” Following further assessment by the response team of those flagged as highest risk, interventions ranged from immediate emergency department referral to facilitating appointments with mental health providers. This study supports use of self-report computerized screening as an accurate method to screen for suicidal ideation, and it demonstrated successful implementation of an automated system flagging those in greatest need of further evaluation to determine level of risk and need for further intervention. While targeting a mixed-age sample of HIV primary care patients, this work points to promising strategies for further development and study among older adults.
Recent studies have also examined the utility of other measures to assess suicidality in primary care. The Columbia-Suicide Severity Rating Scale consists of 18 items and has been shown to predict suicide attempts in suicidal and non-suicidal individuals [7]. Dube et al developed a brief 4-item measure to assess potential suicide risk, in consideration of competing demands in medical practice that may hinder use of longer scales [42]. For patients who endorse thoughts of self-harm, the “P4 Screener” inquires about past suicide attempts, presence of a current suicide plan, probability of completing suicide, and preventive factors. Based on responses, patients can be classified as minimal, lower, or higher risk for suicide. The authors found that rates of suicidal ideation were comparable to those found in other studies (about 17%), and that the measure was easily utilized by providers.
In a study of older adult primary care patients, Heisel and colleagues found both the 15-item Geriatric Depression Scale (GDS) and a five-item subset of GDS questions were sensitive and specific in identifying patients judged to be suicidal via semi-structured clinical interview [43]. These results are intriguing because the five-item subset did not include items directly assessing suicidal ideation, but related symptoms like hopelessness, worthlessness, and feeling life is empty. The authors posit that older adults with suicidal ideation might be more comfortable disclosing these related symptoms to physicians.
How to assess for suicidal ideation: a practical guide
In addition to the importance of conceptualizing suicidal ideation as a spectrum, another premise of this article is that directly inquiring about presence and severity of suicidal ideation is crucial in order to make clinical judgments. Patients do not always freely volunteer suicidal thoughts, or the degree of these thoughts, nor can one make determinations by simply observing the patient’s affect and behavior. Asking about thoughts of death or suicide has not been linked to increased risk of making an attempt. Rather this inquiry can increase patient-physician trust and can set the stage for the initiation of effective treatment.
If a standardized screen (e.g., item 9 of the PHQ-9) is used, we recommend that positive screens be followed up with a clinical interview to determine which area patients fall in the spectrum of suicidality. The first clinical decision to make is whether thoughts of death are present, and if so, whether they represent non-pathological thoughts that are normative from a developmental perspective or indicate some level of suicidal ideation. As Szanto et al [44] highlight, greater attention is needed for research on assessment strategies that attempt to differentiate “normal” thoughts of death from pathological ones.
We recommend that a clinical interview follow a structured format as presented in Table 1 (as reproduced from our previous paper [45]). This interview consists of a hierarchical set of questions to identify level of suicide risk. For example, if an individual responds positively to “thoughts that you would be better off dead,” the physician notes that at minimum passive suicidal ideation is present. To determine the presence of active ideation, he/she should clarify by asking “Have you had any thoughts about hurting yourself or suicide in the past couple of weeks?” A positive response to this inquiry necessitates continuing with additional questions to determine type of method, frequency and persistence of thoughts, life stress, presence of detailed plan, intention to commit suicide, reasons for living, and degree of impulse control. This type of inquiry will assist the physician in reaching a clinical judgment about immediacy of suicide risk and the necessity of emergency services.
Table 1.
Questions to determine level of suicide risk
| The following figure presents a series of sequential questions to determine level of suicide risk. |
| 1. “In the past couple of weeks, were things ever so bad that you had thoughts that life is not worth living or that you’d be better off dead?” [Passive suicide ideation] |
| If Yes, continue with Question 2 |
| 2. “Have you had any thoughts about hurting yourself or suicide in the past couple of weeks?” [Active suicide ideation] |
| If Yes, continue with Questions 2a–2g |
| 2a. “What have you been thinking of doing?” [Type of method] |
| 2b. “How often do you have these thoughts? How long do they stay on your mind?” [Frequency and persistence] |
| 2c. “What is going on in your life right now?” [Life stress (eg, loss, change in health status)] |
| 2d. “Do you have a plan for doing this?” [Specific detailed suicide plan] |
| 2e. “Do you intend to harm yourself?” [Suicide intention] |
| 2f. “Is anything preventing you from harming yourself? For example, how strong is your desire to live? Do you feel you have a purpose in life? Do you have hope for the future? Do you consider suicide morally wrong or against your religious beliefs? Do you want to avoid causing family and friends pain?” [Reasons for living] |
| 2g. “Do you feel you can resist these thoughts? Have you ever done anything to harm yourself? How often do you drink alcohol or use street drugs?” [Impulse control] |
Used with permission from Raue PJ, Brown EL, Meyers BS, Schulberg HC, Bruce ML: Does every allusion to possible suicide require the same response? The Journal of Family Practice. 55:7 2006 July, pg 605-12
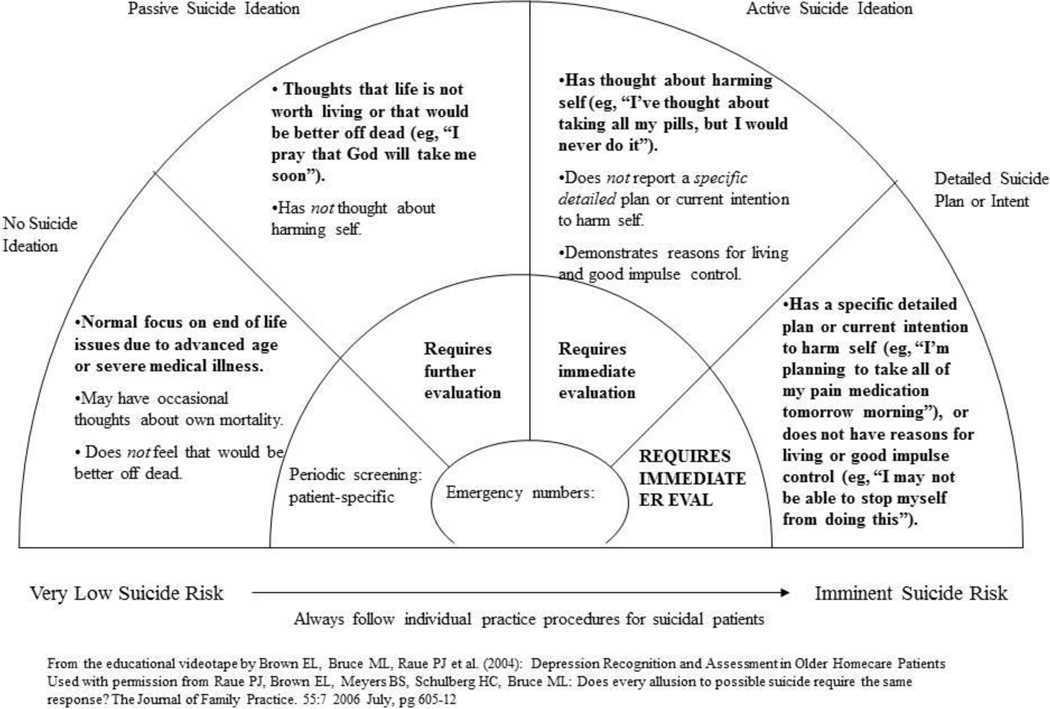
We present a visual tool in Figure 1 (as reproduced from our previous paper [45]), that places individuals at different risk levels depending on their responses to the structured inquiry. Based on risk level, corresponding action plans are recommended (copies available at www.mentalhealthtrainingnetwork.org).
FIGURE 1.
SUICIDE RISK AS A SPECTRUM: ASSESSMENT AND INTERVENTION STRATEGIES
From the educational videotape by Brown EL, Bruce ML, Raue PJ et al. (2004): Depression Recognition and Assessment in Older Homecare Patients Used with permission from Raue PJ, Brown EL, Meyers BS, Schulberg HC, Bruce ML: Does every allusion to possible suicide require the same response? The Journal of Family Practice. 55:7 2006 July, pg 605-12
Management of Suicidality in Primary Care
Recent research in management of suicidal ideation
A great deal of work has been done to develop and evaluate the impact of primary care-based interventions to identify and manage late life depression, a major risk factor for suicide risk [46]. Both the PROSPECT and IMPACT studies have focused on older adult primary care patients and are based on the collaborative model of care in which guideline-based care is provided by physicians with the support of a nurse, social worker, or psychologist depression care manager. The care manager serves as a liaison between patients and physicians and monitors symptoms, side effects, and treatment adherence and communicates this information to the physician, in addition to the need for more intensive psychiatric services. In PROSPECT and IMPACT, the care manager also offered brief evidence-based psychotherapy for those patients preferring this approach (i.e., Interpersonal Psychotherapy for PROSPECT and Problem Solving Treatment for IMPACT).
Both interventions have shown promising results in reducing not only depressive symptoms but the presence of suicidal ideation [47, 48]. For example, the PROSPECT study examined a sample of 599 adults aged 60 and above with major or minor depression from 20 diverse primary care practices and found that rates of overall suicidal ideation declined more in intervention (12.8% decrease) than in usual care patients (3.0% decrease) by 4 months [47]. And by 24 months, there was a 2.2 times greater decline in rates of suicidal ideation in intervention (18.3% decrease) compared to usual care patients (8.3% decrease).
Longer-term follow up of patients in the PROSPECT study over the course of 5 years has demonstrated an association of suicidal ideation with all-cause mortality [24]. Among patients in practices assigned to Usual Care, expressing a wish to die was associated with an increased risk of mortality across depressive status (i.e., major, minor, or no depression). In Intervention practices, this association was greater among the no depression compared to major depression group. These findings suggest that expressing a wish to die may be clinically significant and important to assess even in patients without depressive or other psychiatric disorder. The association of a wish to die and mortality was not observed among depressed patients in practices that implemented the PROSPECT intervention, highlighting the further downstream benefits of such an intervention.
The IMPACT intervention also included suicidal ideation as an outcome and demonstrated significant reductions in such ideation in comparison to Usual Care. Using a sample of 1,801 adults aged 60 and above from 18 diverse primary care clinics, intervention subjects had significantly lower rates of suicidal ideation than controls at 6 months (7.5% vs. 12.1%) and 12 months post-enrollment (9.8% vs. 15.5%). Differences persisted after the intervention ended at 12 months, with lower rates of suicidal ideation at 18 months (8.0% vs. 13.3%) and 24 months (10.1% vs. 13.9%) [48].
In another vein, Van Orden et al [49] have designed and are currently testing a peer companionship intervention called The Senior Connection that aims to prevent the development of suicidal ideation among at-risk older adults. Primary care patients who report a low sense of belongingness or feeling like a burden on others are linked to community-based aging service settings in which the peer-led intervention is provided. The Senior Connection is grounded in the Interpersonal Theory of suicide which proposes that social disconnectedness brings about the desire for suicide. The intervention involves companionship and supportive interpersonal interactions provided by an older adult peer volunteer; the authors posit that this intervention will lead to increased social connectedness and thereby reduced suicidal ideation and other risk factors for suicide. An innovative element of this program is the linkage of primary care patients to community-based social service settings, in which volunteer-based services are often embedded. The intervention’s focus on bolstering social connectedness is also consistent with approaches recommended by the National Strategy for Suicide Prevention, and represents a promising attempt to intervene early in path toward preventing the development of suicidal ideation and suicidal behavior.
Other innovative work conducted by Stanley and Brown [50] has targeted suicidal patients seen in emergency departments in an effort to prevent future suicidal crises. Their brief safety planning intervention consists of helping patients develop a written list of coping strategies and informal and formal supports for patients to use in preventing suicidal crises. Of note, this type of safety planning goes beyond simple “no suicide contracts,” which have not been shown to be effective in preventing suicide, by formulating a plan for how patients should respond when feeling suicidal. The specific elements of the plan include helping patients recognize warning signs of a suicide crisis; employing internal coping strategies; using social support for distraction or for more direct assistance; contacting mental health professionals; and restricting access to lethal means. We present this safety planning intervention here as we believe a brief psychosocial intervention of this type may also have merit for suicidal patients once discharged back to primary care.
How to respond to suicidal ideation: a practical guide
We offer several suggestions for how primary care physicians may assess and manage suicidality in older patients. As depicted in our visual tool (Figure 1), response and ongoing management of individuals with suicidal ideation depends on the assessment of risk level.
We have recommended [45] that individuals who endorse passive suicidal ideation require further evaluation to determine the presence of depression and other psychiatric disorders. While definitive data do not exist on when this evaluation should be conducted, we suggest that patients with passive suicide ideation be evaluated within a week. We also recommend that these patients be seen more frequently by the primary care physician and their level of suicide risk assessed at each office visit, particularly when an antidepressant has been initiated or its dosage changed.
Patients endorsing active suicide ideation even when lacking a specific plan or intention require immediate, same-day evaluation. Primary care clinicians may directly treat patients with active suicide ideation, or refer them to specialty mental health practitioners. Patients with active suicide ideation should be seen more frequently by the primary care clinician, and their level of suicide risk should be assessed at each office visit.
Patients endorsing a specific plan or intention to harm themselves require immediate psychiatric evaluation for safety at an emergency room. Following emergency room evaluation and possible inpatient hospitalization, these patients should be referred to a mental health specialist for ongoing treatment.
Conclusions
Suicidal ideation in older primary care patients exists on a continuum, with varying levels of suicidal ideation requiring different types of interventions from primary care providers. The use of evidence-based screens and structures clinical interviews can help physicians accurately identify cases. Guidelines for addressing each level of suicidal ideation may assist primary care physicians in making appropriate treatment and referral decisions.
Screening efforts require further study, particularly the utility and cost-effectiveness of focusing screening on those with known risk factors versus screening all older adults in primary care. Broader scale screening would capture cases of suicidality among those without known risk factors, but may create additional time and cost burdens on clinicians and practices.
Several intervention approaches, including collaborative care models, show evidence of efficacy in reducing suicidality in older adults. Future studies are needed to identify the most effective strategies to broadly disseminate and implement these approaches. Research is also needed to identify mediators and moderators of such interventions in order to understand mechanisms of action, and for which older adult subpopulations they are most effective.
In addition to these recommendations, the National Action Alliance for Suicide Prevention’s Research Prioritization Task Force [51] has identified other promising research areas such as: understanding when and how individuals transition from low-risk to high-risk states; testing new technologies for predicting level of risk and intervention response; documenting the impact of quality improvement efforts in health care systems; and testing interventions to reduce risk factors for suicide.
Primary care offers ample opportunities to reach older adults experiencing suicidality. With greater research and clinical attention to screening and treatment for suicidality in these settings, high rates of suicidal ideation and behavior among older adults and associated poor health outcomes can be reduced.
Acknowledgments
This work was supported by Grant Nos. R01 MH084872; R01 MH082425; R01 MH096441; P30 MH085943; T32 MH073553 from the National Institute of Mental Health.
Footnotes
Compliance with Ethics Guidelines
Conflict of Interest
Patrick J. Raue, Angela R. Ghesquiere, and Martha L. Bruce declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
REFERENCES
- 1.Centers for Disease Control and Prevention. [Accessed May 2014];FASTSTATS: Suicide and self-inflicted injury. Available at http://www.cdc.gov/nchs/fastats/suicide.htm.
- 2.De Leo D, Spathonis K. Suicide and suicidal behavior in late life. In: De Leo DB-B U, Kerkhof A, Schmidtke A, editors. Suicidal behavior: Theories and research findings. Ashland, OH: Hogrefe & Huber; 2004. pp. 253–286. [Google Scholar]
- 3.Shah A. The relationship between suicide rates and age: an analysis of multinational data from the World Health Organization. Int Psychogeriatr. 2007;19:1141–1152. doi: 10.1017/S1041610207005285. [DOI] [PubMed] [Google Scholar]
- 4.American Foundation for Suicide Prevention. [Accessed May 2014];Facts and figures: Suicide deaths. Available at http://www.afsp.org/understanding-suicide/facts-and-figures. [Google Scholar]
- 5.World Health Organization. Distribution of suicide rates (per 100,000) by gender and age. Geneva: [Accessed May 2014]. Available at http://www.who.int/mental_health/prevention/suicide/suicide_rates_charte/en/index.html. [Google Scholar]
- 6. U.S. Surgeon General and the National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and objectives for action. [Accessed May 2014]; Available at http://www.surgeongeneral.gov/library/reports/national-strategy-suicide-prevention/full-report.pdf. This report from the U.S. Surgeon General and the Action Alliance outlines goals and objectives for reducing suicides over the next 10 years.
- 7.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scocco P, Meneghel G, Caon F, et al. Death ideation and its correlates: survey of an over-65-year-old population. J Nerv Ment Dis. 2001;189:210–218. doi: 10.1097/00005053-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Skultety KM, Rodriguez RL. Treating geriatric depression in primary care. Curr Psychiatry Rep. 2008;10:44–50. doi: 10.1007/s11920-008-0009-2. [DOI] [PubMed] [Google Scholar]
- 10.Schulberg HC, Bruce ML, Lee PW, et al. Preventing suicide in primary care patients: the primary care physician's role. Gen Hosp Psychiatry. 2004;26:337–345. doi: 10.1016/j.genhosppsych.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Goldney RD, Fisher LJ, Wilson DH, et al. Suicidal ideation and health-related quality of life in the community. Med J Aust. 2001;175:546–549. doi: 10.5694/j.1326-5377.2001.tb143717.x. [DOI] [PubMed] [Google Scholar]
- 12.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29:870–877. doi: 10.1007/s11606-014-2767-3. Large representative sample of individuals who died by suicide that investigates health care contacts in the year prior to suicide, and whether a mental health condition was documented.
- 14.O'Connor E, Gaynes BN, Burda BU, Soh C, Whitlock EP. Screening for and treatment of suicide risk relevant to primary care: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:741–754. doi: 10.7326/0003-4819-158-10-201305210-00642. [DOI] [PubMed] [Google Scholar]
- 15.McNamee JE, Offord DR. Canadian Task Force on the Periodic Health Examination, Canadian guide to clinical preventive health care. Ottawa, Canada: CCG; 1994. Prevention of suicide; pp. 456–467. [Google Scholar]
- 16.Conwell Y, Duberstein PR, Cox C, et al. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153:1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- 17.Conwell Y, Thompson C. Suicidal behavior in elders. Psychiatr Clin North Am. 2008;31:333–356. doi: 10.1016/j.psc.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Connell H, Chin AV, Cunningham C, et al. Recent developments: suicide in older people. BMJ. 2004;329:895–899. doi: 10.1136/bmj.329.7471.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waern M, Rubenowitz E, Runeson B, et al. Burden of illness and suicide in elderly people: case-control study. BMJ. 2002;324:1355. doi: 10.1136/bmj.324.7350.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Van Orden KA, Simning A, Conwell Y, et al. Characteristics and comorbid symptoms of older adults reporting death ideation. Am J Geriatr Psychiatry. 2013;21:803–810. doi: 10.1016/j.jagp.2013.01.015. Population-based study in Sweden that investigates whether death ideation among older adults is associated with markers of increased risk for suicide, or reflects normal developmental processes.
- 21.Erlangsen A, Jeune B, Bille-Brahe U, et al. Loss of partner and suicide risks among oldest old: a population-based register study. Age Ageing. 2004;33:378–383. doi: 10.1093/ageing/afh128. [DOI] [PubMed] [Google Scholar]
- 22.Murphy GE. Suicide and substance abuse. Arch Gen Psychiatry. 1988;45:593–594. doi: 10.1001/archpsyc.1988.01800300091013. [DOI] [PubMed] [Google Scholar]
- 23.Robinson D, Renshaw C, Okello C, et al. Suicide in cancer patients in South East England from 1996 to 2005: a population-based study. Br J Cancer. 2009;101:198–201. doi: 10.1038/sj.bjc.6605110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raue PJ, Morales KH, Post EP, et al. The wish to die and 5-year mortality in elderly primary care patients. Am J Geriatr Psychiatry. 2010;18:341–350. doi: 10.1097/JGP.0b013e3181c37cfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bomyea J, Lang AJ, Craske MG, et al. Suicidal ideation and risk factors in primary care patients with anxiety disorders. Psychiatry Res. 2013;209:60–65. doi: 10.1016/j.psychres.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiborg JF, Gieseler D, Fabisch AB, et al. Suicidality in primary care patients with somatoform disorders. Psychosom Med. 2013;75:800–806. doi: 10.1097/PSY.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 27.Magruder KM, Yeager D, Brawman-Mintzer O. The role of pain, functioning, and mental health in suicidality among Veterans Affairs primary care patients. Am J Public Health. 2012;102(Suppl 1):S118–S124. doi: 10.2105/AJPH.2011.300451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Almeida OP, Draper B, Snowdon J, et al. Factors associated with suicidal thoughts in a large community study of older adults. Br J Psychiatry. 2012;201:466–472. doi: 10.1192/bjp.bp.112.110130. [DOI] [PubMed] [Google Scholar]
- 29.Cohen A, Chapman BP, Gilman SE, et al. Social inequalities in the occurrence of suicidal ideation among older primary care patients. Am J Geriatr Psychiatry. 2010;18:1146–1154. doi: 10.1097/JGP.0b013e3181dd1e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gilman SE, Bruce ML, Ten Have T, et al. Social inequalities in depression and suicidal ideation among older primary care patients. Soc Psychiatry Psychiatr Epidemiol. 2013;48:59–69. doi: 10.1007/s00127-012-0575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gensichen J, Teising A, Konig J, et al. Predictors of suicidal ideation in depressive primary care patients. J Affect Disord. 2010;125:124–127. doi: 10.1016/j.jad.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 32.Chang EC, Yu EA, Lee JY, et al. An examination of optimism/pessimism and suicide risk in primary care patients: does belief in a changeable future make a difference? Cognitive Therapy and Research. 2013;37:796–804. [Google Scholar]
- 33.Bostwick JM, Rackley S. Addressing suicidality in primary care settings. Curr Psychiatry Rep. 2012;14:353–359. doi: 10.1007/s11920-012-0286-7. [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen S, Chiu H, Xu B, et al. Reliability and validity of the PHQ-9 for screening late-life depression in Chinese primary care. Int J Geriatr Psychiatry. 2010;25:1127–1133. doi: 10.1002/gps.2442. [DOI] [PubMed] [Google Scholar]
- 36. Inagaki M, Ohtsuki T, Yonemoto N, et al. Validity of the Patient Health Questionnaire (PHQ)-9 and PHQ-2 in general internal medicine primary care at a Japanese rural hospital: a cross-sectional study. Gen Hosp Psychiatry. 2013;35:592–597. doi: 10.1016/j.genhosppsych.2013.08.001. Examined ability of the PHQ-2 to identify suicidal ideation, and validity of the suicidal ideation item in detecting suicidal ideation in Japanese patients.
- 37.Sung SC, Low CC, Fung DS, et al. Screening for major and minor depression in a multiethnic sample of Asian primary care patients: a comparison of the nine-item Patient Health Questionnaire (PHQ-9) and the 16-item Quick Inventory of Depressive Symptomatology - Self-Report (QIDS-SR16) Asia Pac Psychiatry. 2013;5:249–258. doi: 10.1111/appy.12101. [DOI] [PubMed] [Google Scholar]
- 38.Gelaye B, Williams MA, Lemma S, et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210:653–661. doi: 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pratt LA, Brody DJ. Implications of two-stage depression screening for identifying persons with thoughts of self-harm. Gen Hosp Psychiatry. 2014;36:119–123. doi: 10.1016/j.genhosppsych.2013.09.007. Investigated the optimal cutoff on the PHQ-2 for identifying individuals with suicidal ideation.
- 40.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 41.Lawrence ST, Willig JH, Crane HM, et al. Routine, self-administered, touch-screen, computer-based suicidal ideation assessment linked to automated response team notification in an HIV primary care setting. Clin Infect Dis. 2010;50:1165–1173. doi: 10.1086/651420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dube P, Kurt K, Bair MJ, et al. The p4 screener: evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. [Accessed May 2014];Prim Care Companion J Clin Psychiatry. 2010 12:e1–e8. doi: 10.4088/PCC.10m00978blu. Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3067996/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heisel MJ, Duberstein PR, Lyness JM, et al. Screening for suicide ideation among older primary care patients. J Am Board Fam Med. 2010;23:260–269. doi: 10.3122/jabfm.2010.02.080163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Szanto K, Lenze EJ, Waern M, et al. Research to reduce the suicide rate among older adults: methodology roadblocks and promising paradigms. Psychiatr Serv. 2013;64:586–589. doi: 10.1176/appi.ps.003582012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raue PJ, Brown EL, Meyers BS, et al. Does every allusion to possible suicide require the same response? J Fam Pract. 2006;55:605–612. [PubMed] [Google Scholar]
- 46. Lapierre S, Erlangsen A, Waern M, et al. A systematic review of elderly suicide prevention programs. Crisis. 2011;32:88–98. doi: 10.1027/0227-5910/a000076. Reviews the results of a number of interventions to prevent suicide among older adults, predominantly focused on reduction of risk factors and calls attention to the need for study of innovative interventions that aim to improve protective factors.
- 47.Alexopoulos GS, Reynolds CF, 3rd, Bruce ML, et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. Am J Psychiatry. 2009;166:882–890. doi: 10.1176/appi.ajp.2009.08121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Unutzer J, Tang L, Oishi S, et al. Reducing suicidal ideation in depressed older primary care patients. J Am Geriatr Soc. 2006;54:1550–1556. doi: 10.1111/j.1532-5415.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- 49. Van Orden KA, Stone DM, Rowe J, et al. The Senior Connection: design and rationale of a randomized trial of peer companionship to reduce suicide risk in later life. Contemp Clin Trials. 2013;35:117–126. doi: 10.1016/j.cct.2013.03.003. Presents a peer companionship intervention that aims to prevent the development of suicidal ideation among at-risk older adults by bolstering social connectedness.
- 50.Stanley B, Brown GK. Safety Planning Intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice. 2012;19:256–264. [Google Scholar]
- 51. National Action Alliance for Suicide Prevention RPTF. A prioritized research agenda for suicide prevention: An action plan to save lives. [Accessed May 2014]; Available at http://actionallianceforsuicideprevention.org/sites/actionallianceforsuicideprevention.org/files/Agenda.pdf. The Research Prioritization Task Force (RPTF) of the Action Alliance details key questions for suicide research to target and proposes a prioritized research agenda to prevent suicide.