Abstract
Purpose
The purpose of this study was to compare the effects of two different resistance exercise protocols on self-reported disability, fear avoidance beliefs, pain catastrophizing and back pain symptoms in obese, older adults with low back pain.
Methods
Obese adults (N=49; 60–85 years) with chronic low back pain (LBP) were randomized into a total body resistance exercise intervention (TOTRX), lumbar extensor exercise intervention (LEXT) or a control group (CON). Main outcomes included perceived disability (Oswestry Disability Index [ODI], Roland Morris Disability Questionnaire [RMDQ]). Psychosocial measures included the Fear Avoidance Beliefs (FAB) survey, Tampa Scale of Kinesiophobia (TSK), Pain Catastrophizing Scale (PCS). LBP severity was measured during three functional tasks: walking, stair climb and chair rise using an 11 point numerical pain rating scale (NRSpain).
Results
The TOTRX group had greater reductions in self-reported disability scores due to back pain (ODI, RMDQ) compared to LEXT (p<0.05). The PCS scores decreased in the TOTRX compared to CON by month four (64.3% vs 4.8%, p<0.05). Pain severity during chair rise activity, and walking pain severity was decreased in both LEXT and TOTRX relative to the CON group.
Conclusions
Greater reductions in perceived disability due to LBP can be achieved with TOTRX compared to LEXT. Pain catastrophizing and pain severity decreased most with TOTRX. The positive change in psychological outlook may assist obese, older adults with chronic back pain re-consider the harmfulness of the pain and facilitate regular participation in other exercise programs.
Keywords: Lumbar, Obesity, Pain, Resistance Training
Introduction
Pain-related fear and fear avoidance are psychosocial factors that are strongly related to long term disability in persons with chronic LBP.(1, 2) However, the relationships between pain-related fear, chronic low back pain and physical function in the obese, older adult are not known. The national obesity crisis is continuing, concurrent with the increased prevalence of low back pain(34) and physical disability,especially in the older demographic. Because the current socioeconomic impact of chronic LBP is large,(9) the additive burdens of obesity andLBP will further strainavailability of healthcare resources. There is a lack of understanding of the relationships between perceived disability, fear avoidance and painful movement, as well as potential interventions to address these factors is therefore a serious scientific deficit.
Previous studies that examined exercise interventions for back pain in this population have largely focused on the physical outcomes or pain symptoms, but less so on fear avoidance beliefs or pain catastrophizing. The levels of fear of movement among non-obese and obese persons who sought physical therapy for LBP have been characterized.(39) Fear avoidance beliefs were moderately elevated in obese, middle-aged individuals compared with their non-obese counterparts, and higher kinesiophobia levels were associated with higher disability scores in obese persons compared to non-obese counterparts.(39) Reducing pain-related fear avoidance beliefs and catastrophizing might be an under-examined strategy to prevent disability in the obese, older adult. Further, it has been shown that total body resistance exercise (including a lumbar extension exercise) improved low back strength in older, overweight adults.(41) Other studies have shown that different resistance exercise programs can reduce low back pain symptoms.(3, 16, 17, 26, 30) Resistance exercise also results in favorable psychosocial benefits such as reduction of anxiety and fear of falling, both of which can contribute to increased physical function and activity.(19, 22) It is unclear, however, if resistance exercise protocols reduce perceived disability due to LBP and fear avoidance beliefs and pain catastrophizing in the obese, older adult. Because earlier studies have used a variety of different resistance exercise protocols (isokinetic or dynamic machines, free weights or body weight) and many have not focused on the obese older population, it is not clear which specific components of exercise therapy are most effective in reducing pain and the minimizing the negative psychological effects such as pain catastrophizing. Therefore, the purpose of this study was to determine whether changes in fear avoidance beliefs, kinesiophobia or pain catastrophizing contributed to the changes in perceived disability due to LBP with either lumbar extension resistance exercise training or total body resistance training. A secondary purpose was to determine whether if either lumbar extension resistance exercise training or total body resistance training decreased disability due to back pain or pain with movement.
Methods
Participants
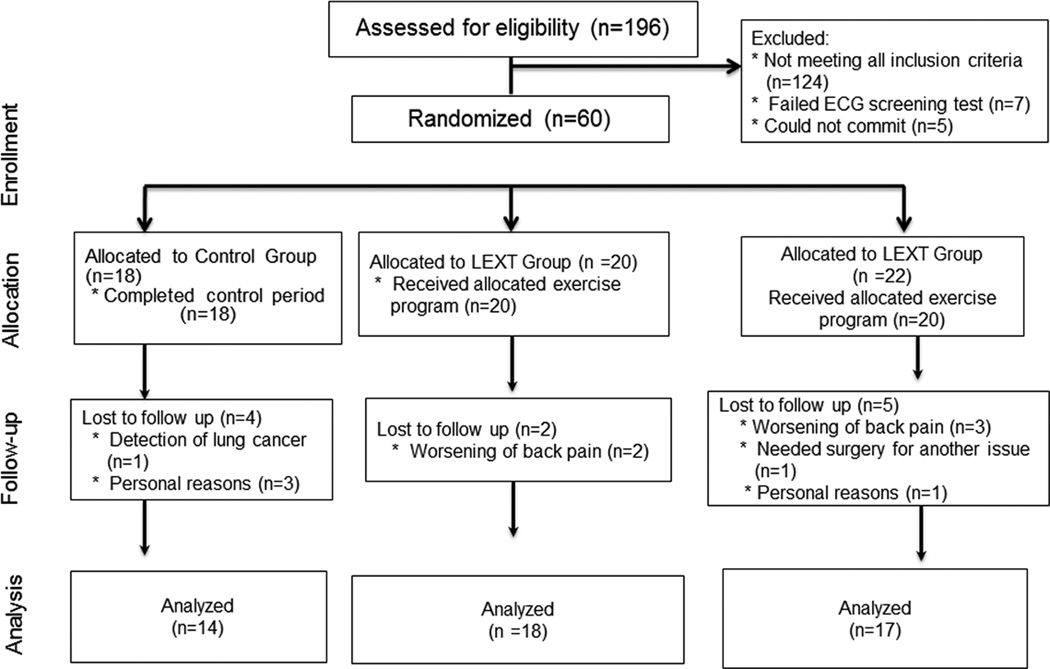
Older adults with chronic low back pain were recruited from the Gainesville area and surrounding regions using the UF Orthopaedics Clinics, the Clinical Trials Register, study flyers and newspaper advertisements, and a list of older adults provided by the UF Claude Pepper Aging Center from the time frame of December 2010 to August of 2012. Inclusion criteria. Men and women 60–85 years of age; suffering from LBP for ≥6 months,(12) abdominal obesity, free of abnormal cardiovascular responses during electrocardiogram (ECG) screening tests were eligible for the study. Exclusion criteria included being wheelchair bound, resistance training regularly (participating in resistance exercise 3 or more times per week within the last 6 months), presence of specific low back pain due to an acute back injury such as a lumbar disc hernation or rupture,(12) spinal stenosis with neurogenic claudication, back surgery within the previous two years(12) and the use of weight loss medication. LBP eligibility criteria were first reviewed on each potential participant by the study coordinator and next reviewed by the physicians on the study to ensure that appropriate participants were enrolled. This study was approved by the University of Florida Institutional Review Board, and all procedures on human subjects were conducted in accordance with the Helsinki Declaration of 1975, as revised in 1983. All participants provided written, informed consent. The study was registered as a clinical trial (NCT01250262). The study flow diagram is shown in Figure 1.
Figure 1.
Study flow diagram. LEXT = lumbar extension resistance exercise group, TOTRX = total body resistance exercise group.
A core group of coordinators and trained exercise physiologists conducted the testing sessions and assessments for the study. The physiologists and the physicians who provided coverage and interpretation of the testing were blinded to the randomization, group assignment and interventions. However, all members of the study team were aware of the screening procedures as part of the study design.
Psychological Assessment
Three scales (Tampa Scale of Kinesiophobia, Fear-Avoidance Beliefs Questionnaire, and Pain Catastrophizing Scale) were the primary outcomes and were used to measure changes in psychological characteristics over four months. The Tampa Scale of Kinesiophobia (TSK) was used to measure fear of movement or re-injury in chronic pain patients. The modified version of the TSK (comprised of 11 questions; TSK-11), was used in this study due to the invariant nature of the instrument across conditions and patient populations. Each item is provided with a 4-point Likert scale with scoring alternatives ranging from “strongly disagree” to “strongly agree”.(47) The TSK has been validated for use in patients with chronic low back pain.(42) This instrument is characterized by two lower order factors (somatic focus and activity avoidance focus).(27) The “Somatic Focus” represents the beliefs of underlying and serious medical problems, and the “activity avoidance focus” represents the belief that participation in activity could result in (re)injury or increased LBP.(27) These two lower order factors and the overall TSK score are presented in the results. The Fear-Avoidance Beliefs Questionnaire (FABQ) is a tool based on theories of fear and avoidance behavior and focuses specifically on beliefs about how physical activity and work affect LBP.(45) The FABQ consists of two scales, a four item FABQ physical activity scale and a seven item work scale. These scales will be reported separately, as has been described.(8) Internal consistency of the TSK and FABQ scores range from α=0.70 to 0.83 in persons with low back pain.(37) The pain catastrophizing scale (PCS)(36) is a 13 item scale that assessed the effect of the chronic back pain on rumination on pain symptoms and helplessness. Pain catastrophizing is the tendency to focus on and amplify pain sensations and feel helpless when pain occurs. For all instruments, higher scores represent higher fear of movement, fear avoidance beliefs and pain catastrophizing.
Perceived Disability Due to Back Pain
Two surveys were secondary outcomes and were used to assess self-report of disability due to low back pain: the modified Oswestry Disability Index (ODI)(6) and the Roland Morris Disability Questionnaire (RMDQ).(28) The modified version of the ODI is responsive to intervention treatments for low back pain, is reliable with an intraclass coefficient value of 0.90, and corresponds well with several global patient disability measures.(6, 28) The Roland Morris Disability Questionnaire (RMDQ) assesses physical disability and mental function with low back pain; this survey is sensitive to treatment interventions, and is reproducible (test-retest correlations 0.83–0.91) and consistent (Cronbach’s α =0.84–0.91) and correlated well with other global ratings and disability measures.(28)
Pain Assessments
Back pain severity with movement(s) was a secondary outcome and was self-reported using an 11 point numerical pain rating scale (NRSpain) with terminal descriptors (anchors of 0 = no pain; 10 = worst possible pain). The NRSpain measure is an established, well-accepted outcome for chronic pain conditions, as described in the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT).(5) This measurement is reliable and valid(44) for assessing pain intensity. NRSpain measures were collected pre-training at baseline and at month four, after the training intervention. Participants rated their back pain while rising from a chair, while climbing a set of stairs and while walking on a level surface. Three trials of each activity were performed, and pain ratings were collected during each trial. The average of the pain ratings was the functional pain score for that activity.
Resistance Exercise Interventions
Participants were randomly and equally assigned to one of three study groups: a total body resistance exercise group (TOTRX; includes lumbar extension), an isolated lumbar extension resistance exercise group (LEXT) or a non-exercise control group (CON). A computer generated list was used to randomly assign the group allocation; the assignments per participant number were placed in numbered sealed envelopes and each new enrolled participant opened an envelope to receive the group assignment. One study coordinator issued the assignment and the PI and other investigators were blinded to the allocation sequence. All exercises were performed on dynamic resistance exercise machines (MedX®). Exercise training sessions were performed in a supervised laboratory setting over a four month period. Before any study measures were collected, all participants were familiarized with all the testing equipment and performed a light exercise set on each of the exercise machines to determine seat adjustments and customize positioning. Details of each exercise session such as repetitions, load and perceived effort were recorded in a personalized training chart. Participants in the trained groups reported to the laboratory three times a week for one-on-one training sessions with an experienced exercise physiologist. Resistance loads were set using a percentage of the one Repetition Maximum (1 RM) technique for each exercise. (34) For each exercise, a warm up of five repetitions at a low weight was followed by three repetitions at a higher weight of each dynamic exercise. One lift was performed at progressively higher loads until the dynamic exercise could not be performed or performed with good form. 1RM values were secondary outcomes. Recovery periods between each left were 60 seconds. In our laboratory, the reliability of this technique is very high (Cronbach’s α range 0.92–0.98). Using this technique no adverse events occurred. Participants performed the training program in the same laboratory as where the testing occurred. Partitioned areas in the lab permitted multiple tests and training to occur at the same time. Participants were provided standardized training and were escorted to and from the training areas. Specific training times were established for each participant during the week to avoid exposure to other participants and contamination of data. Adverse events (AE) were tracked during the study. Any AE (whether directly related to the study or not) or unintended effects were documented from the time of enrollment to completion of the four month study for each participant, and were reviewed as they occurred and on a monthly basis with the study team.
Total Body Resistance Exercise (TOTRX)
For the TOTRX group, and one set of each exercise was completed during each training session: leg press, leg curl, leg extension, chest press, seated row, overhead press, triceps dip, lumbar extension, biceps curl, calf press, abdominal curl and the same lumbar extension exercise described below. Each set contained 15 repetitions performed at a resistance load of 60% of the 1 RM for that exercise to reduce the risk of injury. Participants subjectively rated the effort of the exercise set using the 6–20 point Borg scale (where 6= is no muscle effort at all, and 20= maximal muscle effort possible).(40) The resistance load was increased by ~2% per week for the set to maintain a relative level of muscle effort at ~16–18 for the exercise over time.(40) This was monitored by monthly assessment of 1RM values to ensure that an increase was occurring at the anticipated rate for this group.
Lumbar Extension Resistance Exercise (LEXT)
During the first two weeks, participants performed two sets of lumbar extensions as they acclimated to the exercise (15 repetitions until volitional fatigue) once a week. From two weeks until the end of the study, participants performed one set of lumbar extensions (15 repetitions) three times a week. Similar to the TOTRX group, the resistance load for the LEXT was set at 60% 1RM and was increased by ~2% per week for the set to maintain a relative level of muscle effort at ~16–18 for the exercise over time. The frequency for the LEXT was selected based on previous works which have showed inconsistent improvements in functional changes, lumbar muscle cross sectional area and self-reported functional improvement with training frequencies less than three times a week.(11, 21, 33, 46) The frequency of contact times was also chosen to match the TOTRX group between the study team and the participants. This was monitored by monthly assessment of 1RM values to ensure that an increase was occurring at the anticipated rate for this group.
Non-Exercise, Standard Care
The control group (CON) consisted of participants who received normal medical care and follow-up during the four month study, with no resistance exercise intervention. Educational recommendations from the Centers for Disease Control and Prevention and the American Heart Association regarding physical activity and diet were provided and reviewed with each participant as part of standard care. Administration of guidelines such as these have been used in control groups in similarly designed exercise studies.(29) Materials included information and demonstrations of strengthening body weight-based exercise for back health, healthy nutritional choices and information about back pain. These same educational materials given to the CON group were also provided to the participants in the two training groups. Control participants were offered the opportunity to complete a total body resistance exercise program after the control period. Participants visited the testing laboratory once a month for surveys and strength testing.
Sample Size estimation
Power analysis was calculated using previously published data regarding differences elicited in subjective lumbar pain ratings, the primary outcome measure, between control groups and MedX® resistance exercise in persons with chronic low back pain.(26) The self-reported pain rating was chosen because it is a major factor affecting fear avoidance beliefs and other outcome variables in the study, and is sensitive to change with lumbar strengthening interventions.(13, 26) While some studies have shown 30–60% reductions in lumbar pain with isolated lumbar exercise,(13, 20) these studies did not have a control group for a comparison. The results from a randomized, controlled short term study using adults with chronic back pain who participated in lumbar training revealed that self-reported pain values of the resistance exercise group were 3.4 points (baseline) and 2.9 points (post-training) versus the standard care non-exercise group of 3.7 points (baseline) and 4.1 (post-training) with pooled standard deviations of 1.6 points at baseline and 1.6 points post-training.(26) These improvements were accompanied by improvements in self-reported disability and physical function. The power analysis revealed that a total sample size of 48 participants (n=16 per group) would yield 85% power to detect these differences between groups at the alpha level of 0.05. In our earlier study of resistance exercise in overweight, older adults, the average drop-out rate was 25%.(41) Therefore the sample size has been increased to 20 persons per group for a total of 60 participants. Participants will be randomly assigned with equal probability to one of the three study groups: 1) standard care control (CON), 2) Isolated Lumbar Resistance Exercise (LEXT); or 3) Total Body Resistance Exercise (TOTRX). Potential confounders that might have contributed to changes in the primary outcomes included changes in habitual physical activity (tracked using a dual axis accelerometer over seven days [SAM; Cyma, Seattle, WA] at baseline and month four) and changes in pain medication use (number of pain medications used on a daily basis for chronic LBP monitored every four weeks).
Statistics
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS; v.21.0). Data were managed using REDCap (Research Electronic Data Capture).(10) Descriptive statistics and frequencies were obtained to characterize the study groups. Normality of the data was examined with Kolmogorov-Smirnov tests. Nonparametric methods were applied of data fell outside the normal distribution. Nonparametric tests (Kruskal-Wallis tests) were used to determine whether differences existed among the groups for categorical baseline variables and the study outcome measures. The between subject factor was study group (CON, LEXT, TOTRX) and the within subject variables were psychological survey responses. Repeated measures analyses of variance were performed on the secondary continuous variables of maximal strength to determine whether or not group by time interactions occurred. Secondary variables were pain with movement scores, perceived disability scores, 1RM values and potential confounders such as change in daily activity and pain medication number. The between subject factor was the treatment group (CON, LEXT, TOTRX) and the within group factor was time (baseline, month 4). Correlations were performed between the change scores in pain catastrophizing and the change scores in fear avoidance belief scores (work and activity), Oswestry Disability Index and the Roland Morris Disability Questionnaire. A Bonferroni correction was used to account for multiple comparisons. To determine whether the changes in scores of PCS, FABQ and TSK contributed to the change scores in self-reported disability (ODI and RMDQ), hierarchical regression models were generated. The models were generated by first entering factors that might have contributed to the disability score changes (age, sex, race) and the change in lumbar strength from baseline to month four. The PCS, FABQ and TSK scores were then added to the models. Different models were generated for each disability score. Significance was established at p<0.05 for all statistical tests.
Results
Participant Characteristics
Figure 1 shows the study flow diagram. A total of 196 people were screened by phone, and 124 candidates did not meet all the inclusion criteria or met one or more exclusion criteria. Baseline participant characteristics are shown in Table 1. There were no differences in the physiological characteristics among the three study groups.
Habitual physical activity levels were monitored for all participants, and medication number and type, were documented at baseline, monthly and at month four. The changes in the daily steps taken per day at baseline and month four was 3888±1974 to 4106±1800 steps (CON), 3607±1748 to 3470±1739 steps (LEXT) and 3730±1455 to 3289±1148 (TOTRX) steps, respectively (p=0.584). Pain medication number decreased in the TOTRX compared to the CON group from baseline to month four (1.9±1.0 to 0.8±0.8 medications versus 1.3±0.7 to 1.3±1.0 medications, respectively; p<0.05). The change in medication number did not achieve significance in the LEXT group over the four month study (1.6±1.0 to 1.1±1.1medications). The number of patients experiencing any AE was 8/22 enrolled in the TOTRX and 3/20 enrolled in the LEXT groups compared to 0 in the CON group. The proportion of patients experiencing a severe adverse event, as judged by the investigators, was similar between the training groups (9% in TOTRX and 10% in LEXT), and these were anticipated AE and not related to the study (worsening of back pain that required medical intervention).
The adherence to the study testing visits was 100% in all groups, and the percentage of exercise training sessions completed was 87% in both of the LEXT and TOTRX groups. Maximal strength (1RM values) significantly improved for key exercises such as lumbar extension and leg press by month four (p<0.05; Table 2). While there were improvements in the chest press in the TOTRX group, these did not reach significance (p=0.06).
Survey Responses
The responses to the perceived disability, fear avoidance and pain catastrophizing surveys are shown in Table 3. There was a significant interaction of group by time for the ODI scores and the Roland Morris Disability Questionnaire scores (both p<.05). The TOTRX group demonstrated the greatest reduction in perceived disability due to LBP among the three study groups by month four for both surveys. There was a significant interaction of group by time for the PCS scores (p<.05), where the TOTRX group demonstrated the greatest reduction in pain catastrophizing among the three study groups by month four. There were no significant interactions of group by time for the TSK or the FAB scores.
There were significant correlations between the changes in PCS scores and the change scores FAB activity scores (r=0.442, p=0.001), the Oswestry Disability Index (r=0.350, p=0.01) and change in pain with walking (r=0.35, p=0.014). The correlations between the change in PCS and the change in the Roland Morris Disability Questionnaire scores (r=0.320, p=0.025) or to the change in resting pain (r=0.19, p=0.18) did not achieve significance.
Pain With Movement
Pain severity was assessed during chair rise, stair climb and walking tasks. Baseline pain scores were in the mild to moderate range (Table 4). The absolute pain scores and the percentage change in pain from baseline to month 4 are presented in Table 4. Pain with chair rise was significantly decreased in the TOTRX group compared to the other two groups. Pain during walking was significantly decreased in the TOTRX and LEXT groups compared to the CON group.
Regressions
Table 5 provides the results of the hierarchical regression analyses. Among the change scores for PCS, FABQ work and activity and TSK, only PCS significantly contributed to the variance of the models for the Oswestry Disability Index scores and Roland Morris Disability Questionnaire scores (p<0.05).
Discussion
The purpose of this study was to compare the effects of two different resistance exercise protocols on fear avoidance beliefs, perceived disability and back pain symptoms and in obese, older adults with low back pain. A secondary purpose was to determine whether changes in FABQ, TSK or PCS scores contributed to the changes in perceived disability due to LBP. There were three main findings of this study. First, TOTRX was more efficacious than LEXT in reducing self-reported disability scores due to back pain (ODI, RMDQ) compared to LEXT. Second, pain catastrophizing levels decreased with resistance exercise, with concomitant reductions in self-reported disability values in the TOTRX group relative to the CON group. The change in PCS scores from baseline to month four corresponded with changes in self-reported disability due to back pain and pain with walking. Third, pain severity with the performance of activities of daily living was reduced by TOTRX and LEXT.
The finding that pain catastrophizing, but not other factors, emerged as a psychological factor that could be improved with exercise could be due to obesity itself. For example, severely obese persons with other joint pain (e.g., knee osteoarthritis) demonstrate ~30% higher average pain catastrophizing scores compared to overweight persons.(32) Other studies in overweight and obese persons with osteoarthritis show that higher pain catastrophizing leads to greater physical disability via lowered self-efficacy for physical function.(31) The fear avoidance model suggests that catastrophizing about pain initiates a debilitating cycle of pain related fear, impairment and disability.(43) An interpretation of our findings relative to this model is that short-term resistance exercise reduces pain catastrophizing, and additional training time may be required to alter the next stages of the fear avoidance cycle including kinesiophobia and the fear avoidance beliefs. Because we did not induce weight loss in this study, there could be remaining post-training mobility challenges or mild pain that require additional time to overcome.
While there are no direct comparative studies in this population at present, comprehensive rehabilitation programs in adults that have combined exercise with cognitive behavioral therapies can elicit reductions in RMDQ scores, TSK scores and numerical pain rating scores that can be maintained as long as two years.(23) Reductions in the RMDQ ranged from 15.3 to 1.4 points (rehabilitation) versus 15 to 11 points (control); the TSK score was reduced from 42 to 17.7points (rehabilitation) and from 41 to 40.9 points (control).(23) Workplace interventions for back pain two months in duration to that include strength training can reduce TSK scores by ~10% with reductions in NRSpain score by ~39%.(24) Other comparative intervention studies of physiotherapy, aerobic activity and muscle reconditioning with isoinertial loading have shown that while all groups demonstrated a reduction in NRSpain scores, RMDQ scores were improved most in the aerobics and isoinertial loading groups (16–18% improvement).(20) Our ~4–11 point improvements in the TSK in obese older adults, RMDQ and ODI are within the ranges of those presented in previous studies.
Published evidence shows that both high and low intensity lumbar extensor training programs (using a similar lumbar extension machine to that used in the present study) decreased TSK scores from 4.3%–12%, respectively over nine months of training, but not RMDQ and ODI scores.(12) Another study used a quota-based course of rehabilitation for chronic LBP and measured self-report disability, pain and kinesiophobia.(18) Each patient completed an average of 14 therapy visits and performed resistance exercise, flexibility and lifting activities. After the program, ODI, TSK and FABQ scores all improved; at a 12-month follow-up, all the improvements in these measures were maintained. Of relevance to our obese cohort with back pain, 12 weeks of limited range of motion lumbar extension RX reduced NRSpain values less than full range of motion (−30.3 mm versus −16.3 mm), but was shown to generate similar reductions in ODI scores (−18.2 points versus −12 points).(33) Many obese participants are unable to complete a full lumbar flexion to extension motion similar to that of non-obese persons. These previously published data show that strength exercise for the lumbar muscles in a limited range of motion can help reduce back pain severity even in persons with large waistlines and restricted trunk flexion/extension motion.
The clinical relevance of a reduction in pain catastrophizing with resistance exercise in the obese older adult is the potential for increased tolerance to physical activity and increased self-efficacy for physical function. Pain catastrophizing is a modifiable pain condition.(38) The reduction of pain catastrophizing is thus an appropriate treatment target as the measure is related to reductions in ambulatory pain severity and perceived disability. Achieving high quality mobility (low pain or pain free movement) is a primary goal for this population. The resistance exercise protocols in this study provided the opportunity for these participants to perform physical activities and exercises that they feared would aggravate pain. Progressive resistance exercise helped to reduce pain severity with specific activities such as chair rise and walking. In the fear avoidance model of chronic LBP, pain catastrophizing is the first step in the negative path of physical activity intolerance,(35) fear, fear avoidance, disuse and disability.(43) Decreasing pain catastrophizing levels may help obese older adults with back pain re-consider the harmfulness of the pain and develop confidence in over performing physical activities that may help them achieve life goals,(4) such as becoming physically active. We speculate that this positive change in psychological outlook may therefore facilitate regular participation in other exercise programs and activity for weight management.
Limitations and Strengths
Several limitations of the study should be mentioned. First, the results presented here are largely from Caucasian participants, and additional work should be performed in other races to improve generalization. Data show that African-Americans with chronic pain have different rehabilitation outcomes than Caucasians, (7, 14) and Asians (Chinese) have higher pain catastrophizing and pain severity than European Canadians.(15) Second, LBP severity at enrollment was not controlled. Participants had variations in the average LBP value ranging from mild to severe. It is possible that the initial pain severity level influenced perceived disability(25) and responsiveness to the resistance exercise protocols. Larger studies might consider performing exercise interventions in persons with mild, moderate and severe chronic LBP and evaluating changes in pain and perceived disability. Third, these resistance exercise interventions were relatively short-term interventions, and future investigations may consider which resistance exercise program characteristics (exercise set structure, frequency per week) can maintain improvements in psychosocial status over the long term. Fourth, the finding that CON group demonstrated some improvement in 1RM strength for the leg press and the lumbar extension was unanticipated. Given that the control participants did not increase habitual physical activity and did not report starting any new exercise programs during the study, it is possible that with the monthly 1RM testing and repeated exposures to the machines, some of these controls may have simply felt more comfortable fully engaging in the strength test knowing that their backs would not be injured because of the test. Finally, the generalizability of these findings to other populations with back pain or chronic musculoskeletal pain should be tested. The strengths included a study design that was in accordance with the Consolidated Standards of Reporting Trials statement to optimize internal validity and reduce any bias. Adherence to the training programs in both LEXT and TOTRX groups was excellent. The study used well established and validated survey instruments(5, 36, 37) to examine changes in fear avoidance beliefs and pain.
Conclusion
Total body resistance exercise (including lumbar extension exercise) was more effective than lumbar extension exercise alone in reducing self-reported disability scores due to back pain. Pain catastrophizing levels decreased with TOTRX, with concomitant reductions in self-reported disability values relative to the CON group. Pain severity was reduced in the TOTRX during chair rise activity, and walking pain severity was decreased in both LEXT and TOTRX relative to the CON group. Practitioners should include resistance exercise programs that include lumbar extension to help treat obese older adults with chronic LBP.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number AR057552-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work supported in part by the NIH/NCATS Clinical and Translational Science Award to the University of Florida UL1 TR000064. The results of this study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
Conflict of interest: none to report
References
- 1.Asmundson GJ, Norton GR, Allerdings MD. Fear and avoidance in dysfunctional chronic back pain patients. Pain. 1997;69(3):231–236. doi: 10.1016/S0304-3959(96)03288-5. [DOI] [PubMed] [Google Scholar]
- 2.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1–2):329–339. doi: 10.1016/s0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 3.Danneels LA, Cools AM, Vanderstraeten GG, Cambier DC, Witvrouw EE, Bourgois J, de Cuyper HJ. The effects of three different training modalities on the cross-sectional area of the paravertebral muscles. Scand J Med Sci Sports. 2001;11(3):335–341. doi: 10.1034/j.1600-0838.2001.110604.x. [DOI] [PubMed] [Google Scholar]
- 4.de Jong JR, Vlaeyen JW, Van Eijsden M, Loo C, Onhenga P. Reduction of pain-related fear and increased function and participation in work-related upper extremity pain (WRUEP): effects of exposure in vivo. Pain. 2012;153(10):2109–2118. doi: 10.1016/j.pain.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, Brandenburg N, Burke LB, Cella D, Chandler J, Cowan P, Dimitrova R, Dionne R, Hertz S, Jadad AR, Katz NP, Kehlet H, Kramer LD, Manning DC, McCormick C, McDermott MP, McQuay HJ, Patel S, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Revicki DA, Rothman M, Schmader KE, Stacey BR, Stauffer JW, von Stein T, White RE, Witter J, Zavisic S. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–112. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Forsythe LP, Thorn B, Day M, Shelby G. Race and sex differences in primary appraisals, catastrophizing, and experimental pain outcomes. J Pain. 2011;12(5):563–572. doi: 10.1016/j.jpain.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 8.George SZ, Calley D, Valencia C, Beneciuk JM. Clinical investigation of pain-related fear and pain catastrophizing for patients with low back pain. Clin J Pain. 2011;27(2):108–115. doi: 10.1097/AJP.0b013e3181f21414. [DOI] [PubMed] [Google Scholar]
- 9.Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D. The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine (Phila PA) 2012;37(11):E668–E677. doi: 10.1097/BRS.0b013e318241e5de. [DOI] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture [REDCap] – A metadriven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harts CC, Helmhout PH, de Bie RA, Staal JB. A high-intensity lumbar extensor strengthening program is little better than a low-intensity program or a waiting list control group for chronic low back pain: a randomised clinical trial. Aus J Physiother. 2008;54(1):23–31. doi: 10.1016/s0004-9514(08)70062-x. [DOI] [PubMed] [Google Scholar]
- 12.Helmhout PH, Harts CC, Staal JB, Candel MJ, de Bie RA. Comparison of a high-intensity and a low-intensity lumbar extensor training program as minimal intervention treatment in low back pain: a randomized trial. Eur Spine J. 2004;13(6):537–547. doi: 10.1007/s00586-004-0671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holmes B, Leggett S, Mooney V, Nichols J, Negri S, Hoeyberghs A. Comparison of female geriatric lumbar-extension strength: asymptotic versus chronic low back pain patients and their response to active rehabilitation. J Spinal Disord. 1996;9(1):17–22. [PubMed] [Google Scholar]
- 14.Hooten WM, Knight-Brown M, Townsend CO, Laures HJ. Clinical outcomes of multidisciplinary pain rehabilitation among african american compared with caucasian patients with chronic pain. Pain Med. 2012;13(11):499–508. doi: 10.1111/j.1526-4637.2012.01489.x. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh AY, Tripp DA, Ji LJ, Sullivan MJ. Comparisons of catastrophizing, pain attitudes, and cold-pressor pain experience between Chinese and European Canadian young adults. J Pain. 2010;11(11):1187–1194. doi: 10.1016/j.jpain.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 16.Kell RT, Asmundson GJ. A comparison of two forms of periodized exercise rehabilitation programs in the management of chronic nonspecific low-back pain. J Strength Cond Res. 2009;23(2):513–523. doi: 10.1519/JSC.0b013e3181918a6e. [DOI] [PubMed] [Google Scholar]
- 17.Kell RT, Risi AD, Barden JM. The response of persons with chronic nonspecific low back pain to three different volumes of periodized musculoskeletal rehabilitation. J Strength Cond Res. 2011;25(4):1052–1064. doi: 10.1519/JSC.0b013e3181d09df7. [DOI] [PubMed] [Google Scholar]
- 18.Kernan T, Rainville J. Observed outcomes associated with a quota-based exercise approach on measures of kinesiophobia in patients with chronic low back pain. J Orthop Sport Phys Ther. 2007;37(11):679–687. doi: 10.2519/jospt.2007.2480. [DOI] [PubMed] [Google Scholar]
- 19.Liu-Ambrose T, Khan KM, Eng JJ, Lord SR, McKay HA. Balance confidence improves with resistance or agility training. Increase is not correlated with objective changes in fall risk and physical abilities. Gerontology. 2004;50(6):373–382. doi: 10.1159/000080175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mannion AF, Muntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24(6):2435–2448. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]
- 21.McCartney N, Hicks AL, Martin J, Webber CE. Long-term resistance training in the elderly: effects on dynamic strength, exercise capacity, muscle, and bone. J Geront A Biol Sci Med Sci. 1995;50(2):B97–B104. doi: 10.1093/gerona/50a.2.b97. [DOI] [PubMed] [Google Scholar]
- 22.McLafferty CLJ, Wetzstein CJ, Hunter GR. Resistance training is associated with improved mood in healthy older adults. Percep Mot Skills. 2004;98(3 pt 1):947–957. doi: 10.2466/pms.98.3.947-957. [DOI] [PubMed] [Google Scholar]
- 23.Monticone M, Ferrante S, Rocca B, Baiardi P, Dal Farra F, Foti C. Effect of a long-lasting multidisciplinary program on disability and fear-avoidance behaviors in patients with chronic low back pain: results of a randomized controlled trial. Clin J Pain. 2013;29(11):929–938. doi: 10.1097/AJP.0b013e31827fef7e. [DOI] [PubMed] [Google Scholar]
- 24.Nassif H, Brosset N, Guillaume M, Delore-Milles E, Tafflet M, Buchholz F, Toussaint JF. Evaluation of a randomized controlled trial in the management of chronic lower back pain in a French automotive industry: an observational study. Arch Phys Med Rehab. 2011;92(12):1927–1936. doi: 10.1016/j.apmr.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 25.Peters ML, Vlaeyen JW, Weber WE. The joint contribution of physical pathology, pain-related fear and catastrophizing to chronic back pain disability. Pain. 2005;113(1–2):45–50. doi: 10.1016/j.pain.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 26.Risch SV, Norvell NK, Pollock ML, Risch ED, Langer H, Fulton M, Graves JE, Leggett SH. Lumbar strengthening in chronic low back pain patients. Physiologic and psychological benefits. Spine. 1993;18(2):232–238. [PubMed] [Google Scholar]
- 27.Roelofs J, Sluiter JK, Frings-Dresen MH, Goossens M, Thibault P, Boersma K, Vlaeyen JW. Fear of movement and (re)injury in chronic musculoskeletal pain: Evidence for an invariant two-factor model of the Tampa Scale for Kinesiophobia across pain diagnoses and Dutch, Swedish, and Canadian samples. Pain. 2007;131(1–2):181–190. doi: 10.1016/j.pain.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 28.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 29.Schmitz KH, Hannan PJ, Stovitz SD, Bryan CJ, Warren M, Jensen MD. Strength training and adiposity in premenopausal women: strong, healthy, and empowered study. Am J Clin Nutr. 2007;86(3):566–572. doi: 10.1093/ajcn/86.3.566. [DOI] [PubMed] [Google Scholar]
- 30.Sertpoyraz F, Eyigor S, Karapolat H, Capaci K, Kirazli Y. Comparison of isokinetic exercise versus standard exercise training in patients with chronic low back pain: a randomized controlled study. Clin Rehab. 2009;23(3):238–247. doi: 10.1177/0269215508099862. [DOI] [PubMed] [Google Scholar]
- 31.Shelby RA, Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Blumenthal JA. Domain specific self-efficacy mediates the impact of pain catastrophizing on pain and disability in overweight and obese osteoarthritis patients. J Pain. 2008;9(10):912–919. doi: 10.1016/j.jpain.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Somers TJ, Keefe FJ, Carson JW, Pells JJ, Lacaille L. Pain catastrophizing in borderline morbidly obese and morbidly obese individuals with osteoarthritic knee pain. Pain Res Manag. 2008;13(5):401–406. doi: 10.1155/2008/652453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steele J, Bruce-Low S, Smith D, Jessop D, Osborne N. A randomized controlled trial of limited range of motion lumbar extension exercise in chronic low back pain. Spine (Phila PA) 2013;38(15):1245–1252. doi: 10.1097/BRS.0b013e318291b526. [DOI] [PubMed] [Google Scholar]
- 34.Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthr Rheum. 2007;57(4):656–665. doi: 10.1002/art.22684. [DOI] [PubMed] [Google Scholar]
- 35.Sullivan MJ, Rodgers WM, Wilson PM, Bell GJ, Murray TC, Fraser SN. An experimental investigation of the relation between catastrophizing and activity intolerance. Pain. 2002;100(1–2) doi: 10.1016/s0304-3959(02)00206-3. 47-5. [DOI] [PubMed] [Google Scholar]
- 36.Sullivan MJL, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psyhc Assess. 7:432–524. [Google Scholar]
- 37.Swinkels-Meewisse EJ, Swinkels RA, Verbeek AL, Vlaeyen JW, Oostendorp RA. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8(1):29–36. doi: 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- 38.Thorn BE, Pence LB, Ward LC. A randomized clinical trial of targeted cognitive behavioral treatment to reduce catastrophizing in chronic headache sufferers. J Pain. 2007;8(12):938–949. doi: 10.1016/j.jpain.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 39.Vincent HK, Omli MR, Day TI, Hodges M, Vincent KR, George S. Fear of movement, quality of life and self-reported disability in obese patients with chronic lumbar pain. Pain Med. 2011;12(1):154–164. doi: 10.1111/j.1526-4637.2010.01011.x. [DOI] [PubMed] [Google Scholar]
- 40.Vincent KR, Braith RW, Feldman RA, Magyari PM, Cutler RB, Persin SA, Lennon SL, Gabr AH, Lowenthal DT. Resistance exercise and physical performance in adults aged 60 to 83. J Am Geriat Soc. 2002;50(6):1100–1110. doi: 10.1046/j.1532-5415.2002.50267.x. [DOI] [PubMed] [Google Scholar]
- 41.Vincent KR, Braith RW, Vincent HK. Influence of resistance exercise on lumbar strength in older, overweight adults. Arch Phys Med Rehab. 2006;87:383–389. doi: 10.1016/j.apmr.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 42.Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62(3):363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 43.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 44.Von Korff M, Jensen MP, Karoly P. Assessing global pain severity by self-report in clinical and health services research. Spine. 2000;25(24):3140–3151. doi: 10.1097/00007632-200012150-00009. [DOI] [PubMed] [Google Scholar]
- 45.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 46.Willemink MJ, van Es HW, Helmhout PH, Diederik AL, Kelder JC, van Heesewijk JP. The effects of dynamic isolated lumbar extensor training on lumbar multifidus functional cross-sectional area and functional status of patients with chronic nonspecific low back pain. Spine (Phila PA 1976) 2012;37(26) doi: 10.1097/BRS.0b013e318274fb2f. E1651-E165. [DOI] [PubMed] [Google Scholar]
- 47.Woby SR, Roach NK, Urmston M, Watson P. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale of Kinesiophobia. Pain. 2005;117(1–2):137–144. doi: 10.1016/j.pain.2005.05.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.