Abstract
Background:
It is common in medical practice to see patients having persistent pain and radiculopathy even after undergoing discectomy surgery. Inflammatory cytokines, such as interleukins are produced at the site of disc herniation and are now considered responsible for the pain perceived by the patient. This study has used high sensitive C-reactive protein (HSCRP) assay for predicting inflammation around the nerve roots on very same principle, which has used HSCRP for predicting coronary artery diseases in current clinical practice. Thus, purpose of this study is to test whether HSCRP can stand as an objective tool to predict postoperative recovery in patients undergoing lumbar discectomy. That is, to study association between preoperative HSCRP blood level and postoperative recovery with the help of modified Oswestry Back Disability Score.
Materials and Methods:
A study group consisting of 50 cases of established lumbar disc disease and control group of 50 normal subjects, matched with the study group. Both the study and control groups were subjected to detailed evaluation with the help of modified Oswestry Low Back Pain Scale both pre and postoperatively at 3 months, 6 months and 1-year. The preoperative blood samples were analyzed to assess the HSCRP concentration. All the cases underwent surgery over a period of 1-year by the same surgeon.
Results:
The level of HSCRP in the study group was between 0.050– and 0.710 mg/dL and in the control group, 0.005-0.020 mg/dL. There was highly significant positive correlation between preoperative HSCRP level and postoperative score at P < 0.005. Cases with HSCRP level in the range of 0.1820 ± 0.079 mg/dL, showed better recovery (score improved > 10 points), while those with HSCRP level in the range of 0.470 ± 0.163 mg/dL, showed poor recovery (score improved < 10 points).
Conclusion:
HSCRP will serve as a good supplementary prognostic marker for operative decision making in borderline and troublesome cases of lumbar disc disease.
Keywords: Lumbar disc disease, sciatica, discectomy, high sensitive C-reactive protein
MeSH terms: Lumbar, disc, herniated, sciatica, blood proteins
INTRODUCTION
It is common in medical practice to see patients having persistent pain and radiculopathy even after undergoing discectomy surgery.1,2 This has remained a significant source of dissatisfaction on the part of both patient as well as the surgeon. Hence, it has always been a surgical dilemma for a surgeon to do a proper case selection for disc surgery.3,4,5
Sciatic pain has been thought to be caused by the mechanical compression of nerve roots by the herniated nucleus pulposus.6 Now, it has increasingly become evident that intervertebral disc disease (IDD) also involves an underlying inflammatory component. Inflammatory cytokines, such as interleukin-1 (IL-1), IL-6 and tumor necrosis factor-α (TNF-α) are produced at the site of disc herniation and are now considered responsible for the pain perceived by patient.7,8,9,10,11,12 Hence, it is not only the mechanical compression of nerve root, but also the inflammation around the nerve roots, which unfortunately is responsible for postoperative pain, perceived by the patient in spite of surgeon doing his job of removing mechanical compression completely. We, in this study, have specifically tried to address this problem of predicting postoperative recovery in patients undergoing discectomy by using high sensitive C-reactive protein (HSCRP) levels as a prognostic marker. Underlying inflammation around disc herniation causes an increase in CRP level by the miniscule amount.13 Similar marginal increase in CRP has also been noted in atherosclerosis by various studies aimed at predicting risk of coronary and cerebrovascular disease in apparently healthy populations much before its occurrence.14,15,16,17 CRP usually is measured in clinical laboratories by either immunonephelometric or immunoturbidimetric assays.18 The current methods are generally reproducible, fully automated, and capable of measuring CRP with a detection limit of 3-5 mg/L.18 Although this detection limit is adequate for the traditional clinical utility of CRP in monitoring infection, it renders most of the current assays useless in assessing and measuring the amount of inflammation around disc or atherosclerosis in apparently otherwise healthy populations. Hence, this study has used HSCRP assay for predicting inflammation around the nerve roots on very same principle, which has used HSCRP for predicting coronary artery diseases. This ultrasensitive assay is capable of measuring HSCRP at a concentration of 0.00095 mg/dL using ultrasensitive latex-enhanced immunoassay (latex) on the BN II nephelometer.18 In this study, we evaluated the clinical utility of this immunoassay and compared its usefulness in predicting postoperative recovery in patients undergoing lumbar discectomy. We aimed to study association between preoperative HSCRP blood level and postoperative recovery with the help of modified Oswestry Back Disability Score.
MATERIALS AND METHODS
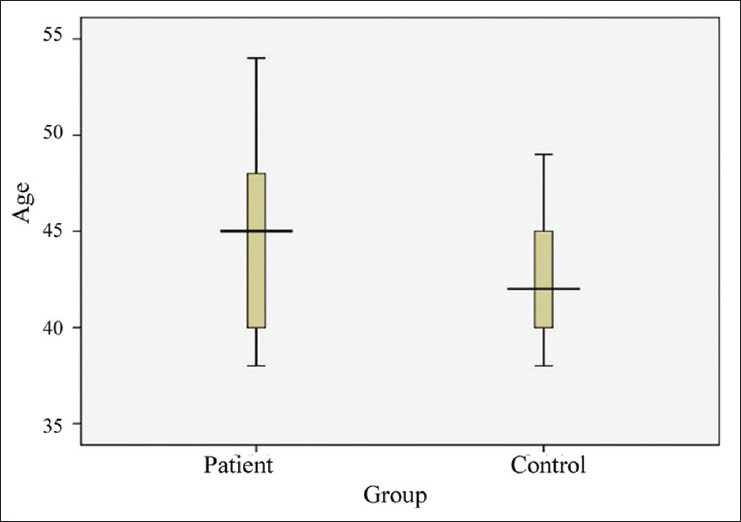
We selected a study group consisting of 50 cases of established lumbar disc disease that underwent disc surgery by the same surgeon over a period of 1-year. All patients were reevaluated at 3 months, 6 months and 1-year with modified Oswestry Back Disability Score [Table 1]. The control group consisted of 50 normal subjects matched with the study group for age, sex and body mass index. Study group had 17 cases of L4-L5 herniation, 22 cases of L5-S1 and 11 cases of combined L4-L5 with L5-S1 herniation [Figure 1]. Our inclusion criteria in the study group consisted of age between 20 and 60 years, clinical evidence of herniation in the form of disc related radicular pain of >3 months duration, not responding to conservative treatment and interfering with daily activities, radiological evidence of herniation: Magnetic resonance imaging (MRI) obtained during symptomatic period with 1.5 T using T2-weighted (TR/TE of 4000/90 ms) and T1W (TR/TE of 600/10 ms) sequences showing evidence of disc degeneration that is, dark nucleus pulpous after comparing its signal intensity with adjacent CSF that is, Grade 2 and above of Schneiderman's classification19 and disc protrusion in the spinal canal.
Table 1.
Modified oswestry back disability score
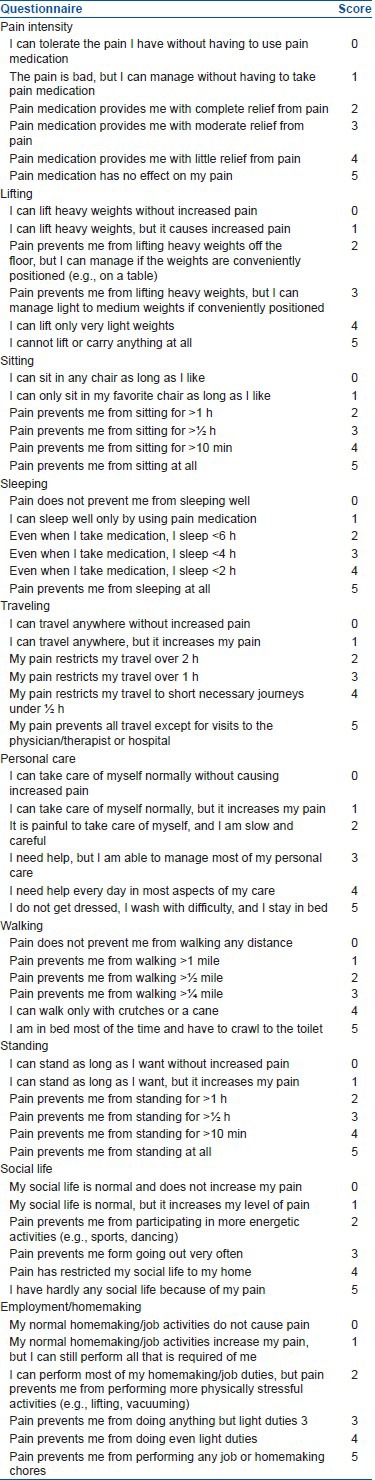
Figure 1.
Bar diagram showing level of lesion
Exclusion criteria consisted of patients who have chronic inflammatory diseases or malignancy, medically unfit for surgical intervention, patients having any local and systemic source of infection, chronic smokers, patients with ischemic heart disease and stroke (high baseline CRP levels). All cases were subjected to detailed evaluation with the help of modified Oswestry Low Back Pain Scale. It consisted of low back pain disability index questionnaire about pain intensity, personal care, lifting, standing, walking, sitting, sleeping, social life, travelling and employment/homemaking. Thus, total 10 points; each had score range of 0-5. Hence, total score had range of 0-50. Severe the disc disease, more is the disability score. Preoperative 2cc blood sample was collected under all aseptic precautions in plain bulb for estimation of HSCRP level from all cases and controls.
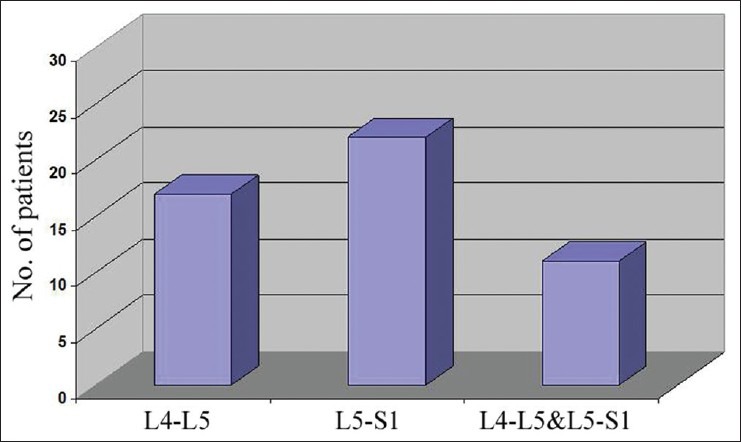
We have used radiological classification for disc degeneration severity that is, Schneiderman's classification for MRI which is Grade 1 (normal), normal height and signal intensity; Grade 2 (intermediate), speckled pattern or heterogeneous, decreased, signal intensity; Grade 3 (marked), diffuse loss of signal; Grade 4 (absent), signal void [Figure 2].
Figure 2.
Bar diagram showing radiographic grading
Written informed consent was obtained from all cases and controls participating in the study after explaining the nature of the test and study design. Institutional Ethics Committee clearance regarding study and collection of blood samples for CRP tests after informed consent of individuals was obtained.
The preoperative blood samples were analyzed to assess the HSCRP concentration, as measured by an ultrasensitive latex-enhanced immunoassay (N-latex CRPII).
RESULTS
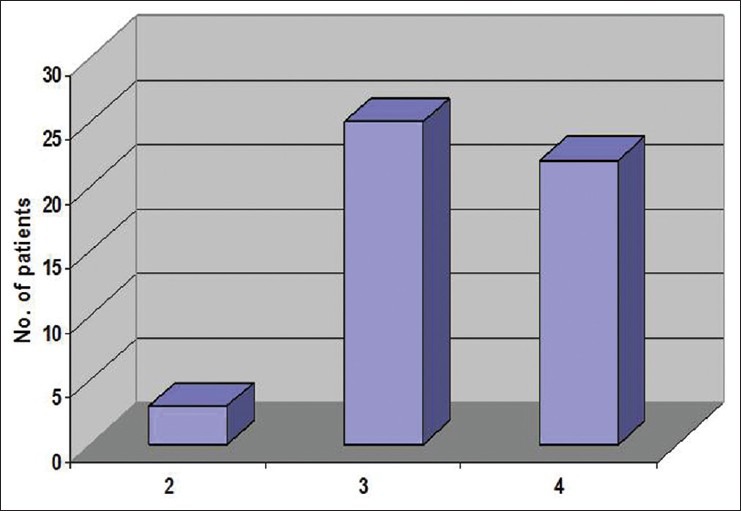
The mean age in the study group was 44.20 years with 31 males and 19 females in the study group. Both study and control group are comparable with respect to age and sex at P < 0.05 [Figures 3 and 4]. The level of HSCRP in the study group was between 0.050 and 0.710 mg/dL and in the control group, 0.005-0.020 mg/dL [Figure 5].
Figure 3.
Graph showing comparison of age distribution between two groups
Figure 4.
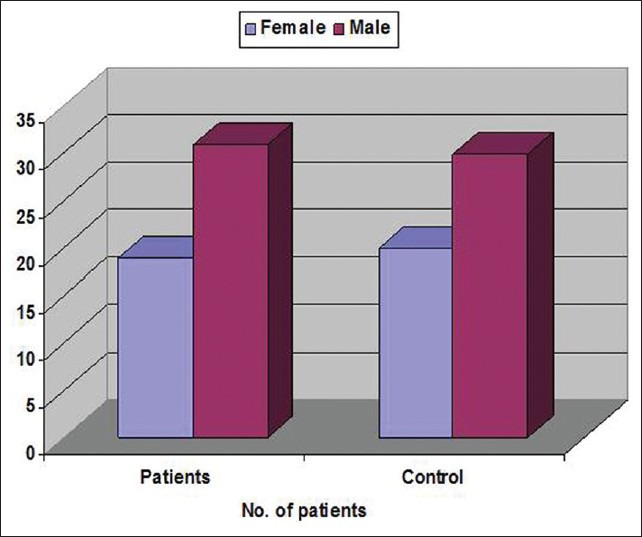
Bar diagram showing comparison of sex distribution between two groups
Figure 5.
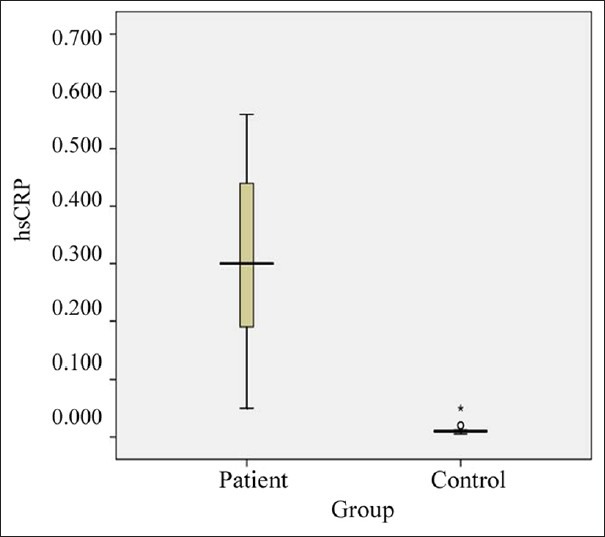
Graph showing comparison of high sensitive C-reactive protein levels between two groups
Statistical analysis
Data were entered using MS-Excel-2007 and analyzed using SPSS-16 software. Following statistical tests of significance are used. Un-paired t-test –for comparison between two group comparison (for comparison of mean between study and control groups). One-way ANOVA test with Bonferroni's posthoc test –for comparison between three groups (for comparison of mean between three groups –numerical data). Pearson's correlation –for Correlation between two numerical variables (e.g. HSCRP, pre and postscores etc.) Chi-square test (for comparison of proportions between two groups –categorical data).
The P < 0.05 was taken as statistically significant.
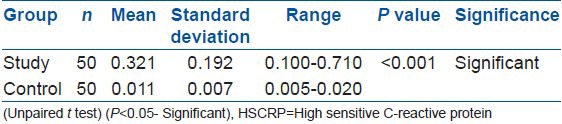
Mean HSCRP level in the study group was 0.321 mg/dL ± standard deviation (SD) 0.192 mg/dL, as compared to 0.011 mg/dL ± SD 0.007 mg/dL in the control group, which is Statistical significant at P < 0.01 [Table 2]. Mean postoperative score was 15.78 as compared with the mean preoperative score of 33.08.
Table 2.
Comparison of HSCRP levels between two groups
In the study group, there was no other correlation between preoperative score and level of disc herniation or radiological severity with the HSCRP level at P < 0.001.
However, there is highly significant positive correlation between preoperative HSCRP level and postoperative score at P < 0.005 (Pearson correlation) [Table 3]. Cases with HSCRP level in the range of 0.1820 ± 0.079 mg/dL, showed better recovery (score improved >10 points), while those with HSCRP level in the range of 0.470 ± 0.163 mg/dL, showed poor recovery (score improved <10 points) [Table 4 and Figure 6].
Table 3.
Correlation between HSCRP level and pre/postoperative score
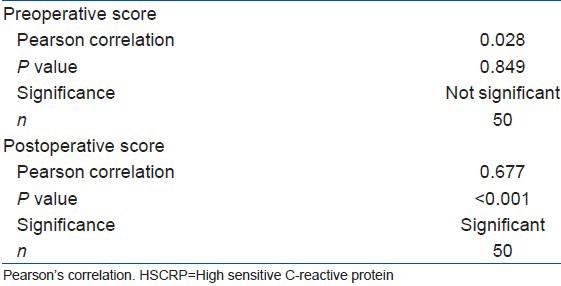
Table 4.
Correlation between HSCRP level and postoperative recovery
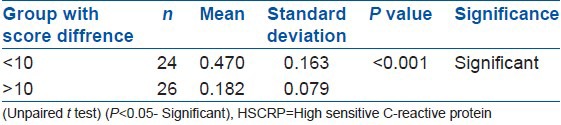
Figure 6.
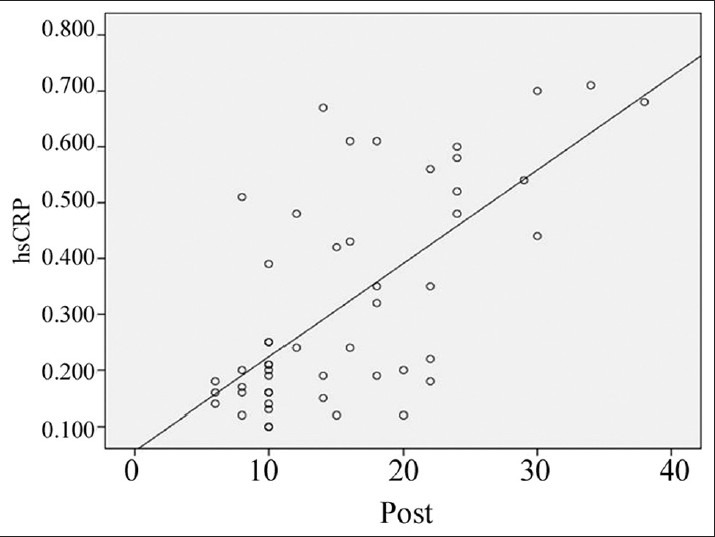
Graph showing comparison between high sensitive C-reactive protein levels and post operative score
DISCUSSION
C-reactive protein is an acute-phase reactant, the levels of which rise dramatically during infection/inflammatory processes occurring in the body. This increment in CRP is due to a rise in the plasma concentration of IL-6, which is produced predominantly by macrophages around the disc tissue.20 Hence, CRP is commonly used parameter for monitoring infection/inflammationhours after tissue injury/infection.16 This study shows that, those with higher HSCRP level preoperatively (in the range of 0.470 ± 0.163 mg/dL) showed poor recovery after surgery in the form of pain relief, which was assessed with modified Oswestry Back Disability Score. This may suggest that pre op inflammatory neuritis as suggested by high HSCRP level may determine the outcome of disc surgery. Contrary to expected, we did not find any relation between preoperative score or radiological grading severity with preoperative HSCRP level, which was similar to findings in related studies.21
Until now, only two studies by Sugimori et al.21 and Le Gars et al.,22 have studied the correlation of preoperative HSCRP level with postoperative scores. Both have found positive correlation between two as found out in our study. We have used modified Oswestry Back Disability Score as compared with Japanese Orthopedic Association score in these studies. In both these studies, there was no correlation found between the level of disc herniation and HSCRP level. Sugimori et al.21 used highly sensitive assay similar to one, which has been used in this study that is, ultrasensitive latex-enhanced immunoassay (N-latex CRPII), while Le Gars et al.22 used an enzyme-linked immunosorbent assay with limit detection of 0.0005 mg/dL. In both these methods, a systemic inflammatory response to local inflammation around the nerve roots was found using highly sensitive analysis of CRP. This inflammatory response is due to the inflammatory cytokines, which are produced by macrophages and monocytes, in response to nerve root inflammation. Many studies have shown and confirmed the inflammatory responses occurring in the herniated disc region. Hence, further research is necessary to explore the possibility of the use of agents, such as TNF-α blocker like Infliximab.23
A positive correlation between the preoperative concentration of HSCRP and the Back Disability Score postoperatively, indicate that patients with a higher preoperative level of HSCRP showed poor postoperative recovery due to persistent postoperative inflammatory neuritis in them. Thus, HSCRP will serve as a good supplementary prognostic marker for operative decision making in borderline and troublesome cases of sciatica. Thus, this risk stratification using HSCRP level is important because information about likely poor results after surgery may help the surgeon to reconsider treatment strategy and discuss same with patient while doing case selection for surgery.
To conclude, high sensitive C-reactive protein will serve as a good supplementary prognostic marker for operative decision-making in borderline and troublesome cases of Lumbar Disc Disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Segal R, Stacey BR, Rudy TE, Baser S, Markham J. Spinal cord stimulation revisited. Neurol Res. 1998;20:391–6. doi: 10.1080/01616412.1998.11740536. [DOI] [PubMed] [Google Scholar]
- 2.North RB, Ewend MG, Lawton MT, Kidd DH, Piantadosi S. Failed back surgery syndrome: 5-year followup after spinal cord stimulator implantation. Neurosurgery. 1991;28:692–9. [PubMed] [Google Scholar]
- 3.Hanley EN, Jr, Herkowitz HN, Kirkpatrick JS, Wang JC, Chen MN, Kang JD. Debating the value of spine surgery. J Bone Joint Surg Am. 2010;92:1293–304. doi: 10.2106/JBJS.I.01439. [DOI] [PubMed] [Google Scholar]
- 4.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA. 2006;296:2441–50. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Legrand E, Bouvard B, Audran M, Fournier D, Valat JP. Spine Section of the French Society for Rheumatology. Sciatica from disk herniation: Medical treatment or surgery? Joint Bone Spine. 2007;74:530–5. doi: 10.1016/j.jbspin.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Valat JP, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Pract Res Clin Rheumatol. 2010;24:241–52. doi: 10.1016/j.berh.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Saal JS, Franson RC, Dobrow R, Saal JA, White AH, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine (Phila Pa 1976) 1990;15:674–8. doi: 10.1097/00007632-199007000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Grönblad M, Virri J, Tolonen J, Seitsalo S, Kääpä E, Kankare J, et al. A controlled immunohistochemical study of inflammatory cells in disc herniation tissue. Spine (Phila Pa 1976) 1994;19:2744–51. doi: 10.1097/00007632-199412150-00002. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi H, Suguro T, Okazima Y, Motegi M, Okada Y, Kakiuchi T. Inflammatory cytokines in the herniated disc of the lumbar spine. Spine (Phila Pa 1976) 1996;21:218–24. doi: 10.1097/00007632-199601150-00011. [DOI] [PubMed] [Google Scholar]
- 10.O’Donnell JL, O’Donnell AL. Prostaglandin E2 content in herniated lumbar disc disease. Spine (Phila Pa 1976) 1996;21:1653–5. doi: 10.1097/00007632-199607150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Matsui Y, Maeda M, Nakagami W, Iwata H. The involvement of matrix metalloproteinases and inflammation in lumbar disc herniation. Spine (Phila Pa 1976) 1998;23:863–8. doi: 10.1097/00007632-199804150-00005. [DOI] [PubMed] [Google Scholar]
- 12.Rothoerl RD, Woertgen C, Holzschuh M, Rueschoff J, Brawanski A. Is there a clinical correlate to the histologic evidence of inflammation in herniated lumbar disc tissue? Spine (Phila Pa 1976) 1998;23:1197–200. doi: 10.1097/00007632-199806010-00002. [DOI] [PubMed] [Google Scholar]
- 13.Kang JD, Georgescu HI, McIntyre-Larkin L, Stefanovic-Racic M, Donaldson WF, 3rd, Evans CH. Herniated lumbar intervertebral discs spontaneously produce matrix metalloproteinases, nitric oxide, interleukin-6, and prostaglandin E2. Spine (Phila Pa 1976) 1996;21:271–7. doi: 10.1097/00007632-199602010-00003. [DOI] [PubMed] [Google Scholar]
- 14.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 15.Koenig W, Sund M, Fröhlich M, Fischer HG, Löwel H, Döring A, et al. C-reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: Results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99:237–42. doi: 10.1161/01.cir.99.2.237. [DOI] [PubMed] [Google Scholar]
- 16.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–43. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 17.Ridker PM. High-sensitivity C-reactive protein: Potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation. 2001;103:1813–8. doi: 10.1161/01.cir.103.13.1813. [DOI] [PubMed] [Google Scholar]
- 18.Rifai N, Tracy RP, Ridker PM. Clinical efficacy of an automated high-sensitivity C-reactive protein assay. Clin Chem. 1999;45:2136–41. [PubMed] [Google Scholar]
- 19.Schneiderman G, Flannigan B, Kingston S, Thomas J, Dillin WH, Watkins RG. Magnetic resonance imaging in the diagnosis of disc degeneration: Correlation with discography. Spine (Phila Pa 1976) 1987;12:276–81. doi: 10.1097/00007632-198704000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Castell JV, Gómez-Lechón MJ, David M, Fabra R, Trullenque R, Heinrich PC. Acute-phase response of human hepatocytes: Regulation of acute-phase protein synthesis by interleukin-6. Hepatology. 1990;12:1179–86. doi: 10.1002/hep.1840120517. [DOI] [PubMed] [Google Scholar]
- 21.Sugimori K, Kawaguchi Y, Morita M, Kitajima I, Kimura T. High-sensitivity analysis of serum C-reactive protein in young patients with lumbar disc herniation. J Bone Joint Surg Br. 2003;85:1151–4. doi: 10.1302/0301-620x.85b8.14538. [DOI] [PubMed] [Google Scholar]
- 22.Le Gars L, Borderie D, Kaplan G, Berenbaum F. Systemic inflammatory response with plasma C-reactive protein elevation in disk-related lumbosciatic syndrome. Joint Bone Spine. 2000;67:452–5. [PubMed] [Google Scholar]
- 23.Karppinen J, Korhonen T, Malmivaara A, Paimela L, Kyllönen E, Lindgren KA, et al. Tumor necrosis factor-alpha monoclonal antibody, infliximab, used to manage severe sciatica. Spine (Phila Pa 1976) 2003;15(28):750–3. [PubMed] [Google Scholar]


