Abstract
Background:
Distal radius fractures are one of the the most common adult fractures encountered during the clinical practice of an orthopedic surgeon.1,2 Although several methods of treatment are suggested for these fractures, there are still controversies about the best treatment approach in the literature. Volar plating of distal radius fracture is a method of treatment which has become increasingly popular. One of the complications of this technique is flexor tendon rupture. The purpose of this study was to evaluate the protectiveness of complete repair of pronator quadratus muscle against flexor tendon rupture.
Materials and Methods:
From September 2010 to September 2012, a consecutive series of 157 patients who were younger than 60 years with unstable distal radius fractures were included in the study. A standard volar approach to the distal radius was carried out. The radial and distal ends of pronator quadratus muscle were meticulously elevated from the radius and after volar plate fixation of the fracture, pronator quadratus muscle was restored to its normal insertion. We achieved full coverage of the plate with this muscle and followed the patients postoperatively.
Results:
A total of 135 patients were studied. The mean age of patients was 34 ± 10 years (range 20-60 years). One 55-year-old diabetic female patient with flexor tendon rupture was identified. The flexor pollicis longus tendon had ruptured 16 months after surgery.
Conclusions:
Pronator quadratus repair should be done in distal radius fracture to protect flexor tendons.
Keywords: Distal radius fracture, pronator quadratus, flexor tendon rupture, volar plate
MeSH terms: Radius fracture, tendon injuries, rupture, implants
INTRODUCTION
Distal radius fractures are one of the the most common adult fractures encountered during the clinical practice of an orthopedic surgeon.1,2 Although several methods of treatment are suggested for these fractures, there are still controversies about the best treatment approach in the literature. Currently, open reduction and internal fixation is indicated in active patients with normal demands for daily living; the goal of such treatments is a mobile and pain free wrist.3 Volar plating of distal radius fracture is a method of treatment which has become increasingly popular. Compared to dorsal plate fixation, the volar approach has a theoretical advantage in reducing complications of tendon irritation.4 Nevertheless, tendon rupture, after volar plate fixation, has been as high as 17%.5 The flexor tendon most commonly involved is the flexor pollicis longus (FPL), but there have been reports of other tendon ruptures or irritation after volar plate fixation.6,7
Suspected causes of tendon rupture include improper plate positioning, prominent screws, plate design, steroid use, loss of reduction or fracture collapse and inadvertent retention of drill guides.6,7,8,9 Watershed line is a prominent ridge in the most volar portion of distal radius. It is also well documented that plates distal to watershed line or prominent volarly have increased the possibility of contact with the flexor tendons than those proximal to the watershed line.10,11 Plates that lie proximal to the watershed line, nestled in the volar concavity, are at a further distance from the flexor tendons than those distal to the watershed line. Plates that only extend to the watershed line along both columns are more forgiving.10 Orbay has advocated restoration of the pronator quadratus (PQ) to its native position after volar plating of the radius, providing a layer of vascularized tissue between the plate and the flexor tendons, theoretically protecting the flexor tendons from friction and irritation that could lead to rupture.12,13 PQ repairs, after volar plate fracture fixation, are generally durable. They withstand forces which are generated at the distal radius throughout the healing process with a 4% failure rate.13 The purpose of this study was to evaluate the protectiveness of a complete repair of PQ against flexor tendon rupture.
MATERIALS AND METHODS
This prospective study was approved by our institutional review board. From September 2010 to September 2012, 157 consecutive patients (aged between 18 and 60 years) with unstable distal radius fractures were included in the study. Preoperative radiographs [posteroanterior (PA), lateral and oblique] were evaluated to determine unstable fractures. The criteria proposed by Lafontaine et al.14 and Altissimi et al.15 were used to determine unstable distal radius fractures. Besides this the presence of three or more of the following parameters if associated fractures were considered unstable: Radial dorsal angle more than 20°, dorsal fracture comminution, intraarticular fracture line, presence of ulnar fracture, patient's age more than 60 years and radial shortening of more than 4 mm.
Exclusion criteria included patients younger than 18 or older than 60 years, open fractures, previous surgery or fracture in the distal radius, patients who were unable to complete postoperative visits and patients with a history of traumatic brain injury. Our final study group comprised 135 patients [Figure 1].
Figure 1.
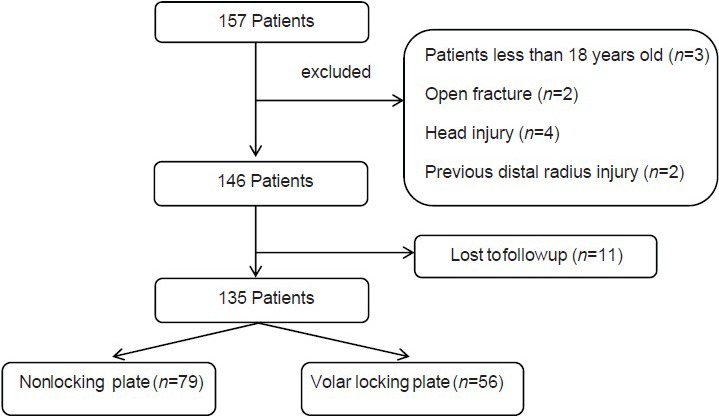
Summary of methodology for selecting patients
Operative procedure
All surgical procedures were performed by three orthopedic surgeons who were experienced in the treatment of distal radius fractures. A standard volar approach to the distal radius, through the flexor carpi radialis sheath, was carried out under general anesthesia. The radial and distal insertions of the PQ with a small rim of brachioradialis and volar capsule, respectively, were sharply incised and elevated from the radius subperiosteally. After exposing and reducing the fracture, the fragments were provisionally fixed with two or more k-wires and then volar plate was used for definite fixation.
For definite fixation, either volar locking plates or nonlocking T-plates were used. The position of plates was determined by fracture fragments, although the trend was to fit the plate proximal to the watershed line, if possible. [Figures 2A, 2B and 3].
Figure 2A.

Peroperative clinical photographs showing (a) exposure of PQ muscle (b) Detachment of PQ muscle with a rim of brachioradialis tendon (c) Detachment of PQ from distal insertion
Figure 2B.
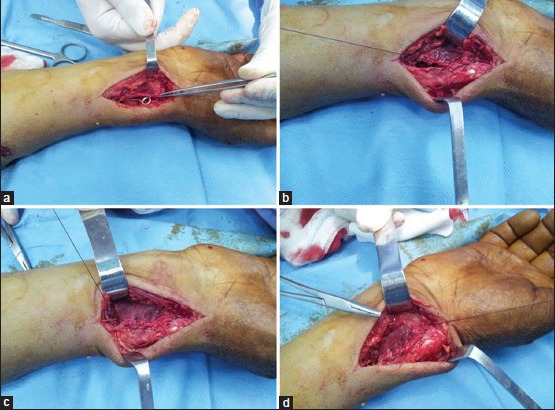
Peroperative clinical photograph showing (a) placement of volar plate (b) Reattachment of radial border of PQ to brachioradialis (c) Complete coverage of the plate at the radial side (d) Reattachment of PQ distal to a rim of volar capsule
Figure 3.

Radiograph of wrist with forearm anteroposterior (a) and lateral (b) views showing fracture has united and implant in situ
Since the PQ with preserved peripheral rim of connective tissues allows sufficient purchase of sutures for full coverage of the plate, the PQ muscle was sutured with absorbable materials (Vicryl) with the forearm in supination position in a tension free manner. The distal margin of the PQ repair is the most important and usually easy to do due to thickness of the tissue. Care must be taken to make the repair at this location continuous and tight and to avoid going too distally so as not to compromise the volar ligaments and wrist extension. The corner of the PQ incision is the second most important part of the repair and is most difficult because the tissue over the radial styloid is thin but is the key to closing the corner. Patients were followed up weekly during their postoperative course for the first 3 weeks and then 6 and 12 weekly and at 6, 12 and 18 months after surgery, Soong et al.'s grading system was used to evaluate plate position relative to the watershed line.9 For this classification, on the postoperative lateral radiographs, a line was drawn tangential to the most volar part of the volar rim, parallel to the volar cortex of radial diaphysis. Plates that did not extend volar to this line were recorded as grade 0. Plates volar to the line, but proximal to the volar rim, were recorded as grade I. Plates directly on or distal to the volar rim were recorded as grade II.
RESULTS
The mean age in our series was 34 ± 10 years (range 20-60 years). There were 92 males (68.1%) compared to 43 females (31.9%). The fractures were classified according to the AO classification, Volar locking plate was used in 56 (41.5%) patients compared to 79 (58.5%) patients in whom nonlocking plates were used. Independent t-test revealed that the average age of patients with locking and nonlocking plates was not statistically significant (P = 0.829).
Most of the patients had no major risk factors for tendon rupture. The authors identified 41 (30.4%) smokers, 4 (3%) patients with diabetes mellitus (DM) and 1 (0.7%) patient was on corticosteroid. The Soong et al. classification was used for identification of volar plate prominence. Chi-square tests showed that in this study, according to Soong et al.'s classification, the difference in the plate position between patients with or without locking plate was not statistically significant (P = 0.46). The mean followup of the patients was 18.4 ± 3.3 months (range 12-24 months). This period of followup of the patients with grade 0, I and II plates was not statistically significant by the Spearman's rank correlation coefficient (r = 0.06 and P = 0.51).
One 55-year-old diabetic female patient with flexor tendon rupture with AO type C fracture pattern was identified, whose FPL tendon had ruptured 16 months after surgery. In this patient, nonlocking plate with a grade I volar prominence with respect to the watershed line had been used.
DISCUSSION
Almost all orthopedic surgeons, particularly hand specialists, believe that the PQ muscle has a role in forearm stability and strength16,17,18 and repair of this muscle after volar plating, according to Swigart et al.'s findings, is reliable. In other words, restoring this muscle after volar plating can bear usual physiological forces with low probability of failure.13 Therefore, it can be expected that after complete coverage of the plate by this muscle, the friction between flexor tendons and the plate and the consequent rupture of flexor tendon can be avoided. Although in most recent studies, proper fitting of the plate proximal to the watershed line is considered the most important factor in prevention of flexor tendon rupture.1,19 Special attention must also be paid to other factors such as plate coverage with PQ muscle and medical comorbidities, which must not be neglected.
Having examined seven cases of cadaveric fresh frozen upper extremities, Tanaca suggested that the probability of damage to the flexor tendon will be reduced if the plate is fitted proximal to the watershed line.11 However, it must be noted that in the present study, by excision of the PQ muscle, its protective role against flexor tendon rupture has been ignored.
In a retrospective study of 165 patients conducted by Soong et al.,7 the PQ muscle had been restored in all patients and the authors had thus concluded that placing the plate on the distal radius plays a significant role in creating flexor tendon rupture; nevertheless, it must be noted that in their study, factors such as the quality and technique of restoring the PQ muscle and the accompanying medical risk factors (like smoking, steroids, or DM) have not been explained. On the other hand, White et al.2 could not find a significant relationship between volar plate position and flexor tendon rupture, which is similar to our study.
In our study, flexor tendon rupture occurred in the elderly patients and it thus appears that further research is essential to study the impact of age and other risk factors (such as taking corticosteroid and DM) on the quality of PQ muscle because it may affect the quality and process of restoring PQ muscle for plate coverage. These results are similar to those shown by Soong et al.7 and Brown.9
In the present study, we only had one case of flexor tendon rupture in which the patient was 55 years old and diabetic and attrition of FPL tendon was observable at the time of surgical exploration and correlated to the plate edge. The plate which had been used was nonlocking T-plate. According to Soong et al.'s grading system, plate location related to the watershed line was in grade I. PQ muscle seemed to have been damaged and did not cover the plate, which might probably be due to improper quality of the PQ muscle at the time of restoration. The true incidence of flexor tendon rupture may be higher, as in some reports, FPL tendon rupture as been reported after 6 years.20
The short followup period of patients was one of the limitations of our study. Another limitation of our study was lack of a control group. Further research is recommended on more patients and especially a randomized clinical trial, to not only better reveal the impact of PQ repair in preventing FPL ruptures but also identify the risk factors that might affect the quality of PQ muscle repair.
Footnotes
Source of Support: Nil
Conflict of Interest: No benefits in any form have been received or will be received directly or indirectly to the subject of this article
REFERENCES
- 1.Cherubino P, Bini A, Marcolli D. Management of distal radius fractures: Treatment protocol and functional results. Injury. 2010;41:1120–6. doi: 10.1016/j.injury.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 2.Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–7. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 3.Ng C, McQueen M. What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br. 2011;93:145–50. doi: 10.1302/0301-620X.93B2.25631. [DOI] [PubMed] [Google Scholar]
- 4.Brown EN, Lifchez SD. Flexor pollicis longus tendon rupture after volar plating of a distal radius fracture: Pronator quadratus plate coverage may not adequately protect tendons. Eplasty. 2011;11:461–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27:1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White BD, Nydick JA, Karsky D, Williams BD, Hess AV, Stone JD. Incidence and clinical outcomes of tendon rupture following distal radius fracture. J Hand Surg. 2012;37:2035–40. doi: 10.1016/j.jhsa.2012.06.041. [DOI] [PubMed] [Google Scholar]
- 7.Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–22. doi: 10.1097/BOT.0b013e318059b993. [DOI] [PubMed] [Google Scholar]
- 8.Soong M, van Leerdam R, Guitton TG, Got C, Katarincic J, Ring D. Fracture of the distal radius: Risk factors for complications after locked volar plate fixation. J Hand Surg. 2011;36:3–9. doi: 10.1016/j.jhsa.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Soong M, Earp BE, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg. 2011;93:328–35. doi: 10.2106/JBJS.J.00193. [DOI] [PubMed] [Google Scholar]
- 10.Zlotolow DA, Raven RB., III Avoiding complications with volar plating of distal radial fractures. Curr Orthop Pract. 2012;23:300–4. [Google Scholar]
- 11.Tanaka Y, Aoki M, Izumi T, Fujimiya M, Yamashita T, Imai T. Effect of distal radius volar plate position on contact pressure between the flexor pollicis longus tendon and the distal plate edge. J Hand Surg. 2011;36:1790–7. doi: 10.1016/j.jhsa.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 12.Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103–12. doi: 10.1142/s0218810400000223. [DOI] [PubMed] [Google Scholar]
- 13.Swigart CR, Badon MA, Bruegel VL, Dodds SD. Assessment of pronator quadratus repair integrity following volar plate fixation for distal radius fractures: A Prospective Clinical Cohort Study. J Hand Surg. 2012;37:1868–73. doi: 10.1016/j.jhsa.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208–10. doi: 10.1016/0020-1383(89)90113-7. [DOI] [PubMed] [Google Scholar]
- 15.Altissimi M, Mancini G, Azzara A, Ciaffoloni E. Early and late displacement of fractures of the distal radius. Int Orthop. 1994;18:61–5. doi: 10.1007/BF02484412. [DOI] [PubMed] [Google Scholar]
- 16.McConkey MO, Schwab TD, Travlos A, Oxland TR, Goetz T. Quantification of pronator quadratus contribution to isometric pronation torque of the forearm. J Hand Surg. 2009;34:1612–7. doi: 10.1016/j.jhsa.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Gofton WT, Gordon KD, Dunning CE, Johnson JA, King GJ. Soft-tissue stabilizers of the distal radioulnar joint: An in vitro kinematic study. J Hand Surg. 2004;29:423–31. doi: 10.1016/j.jhsa.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Gordon KD, Dunning CE, Johnson JA, King GJ. Influence of the pronator quadratus and supinator muscle load on DRUJ stability. J Hand Surg. 2003;28:943–50. doi: 10.1016/s0363-5023(03)00487-8. [DOI] [PubMed] [Google Scholar]
- 19.Schneppendahl J, Windolf J, Kaufmann RA. Distal radius fractures: Current concepts. J Hand Surg. 2012;37:1718–25. doi: 10.1016/j.jhsa.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Nunley JA, Rowan PR. Delayed rupture of the flexor pollicis longus tendon after inappropriate placement of the π plate on the volar surface of the distal radius. J Hand Surg. 1999;24:1279–80. doi: 10.1053/jhsu.1999.1279. [DOI] [PubMed] [Google Scholar]


