Abstract
Background:
Suction drain insertion is a common practice in orthopedic surgery, especially after joint arthroplasty to prevent the formation of a hematoma. Theoretically the use of a drain should diminish the volume of hematoma; however the literature has conflicting data. Some authors state that drainage evacuates fluid from a limited area only and can be a cause of infection due to retrograde migration of bacteria. It can also impair the early postoperative rehabilitation. The aim of this study was to evaluate the clinical outcome (especially postoperative pain) and intake of analgesics in patients who had undergone primary cemented total knee arthroplasty (TKA) with or without a postoperative drain.
Materials and Methods:
A prospective comparative study of 108 consecutive patients (121 knees) was conducted. They were divided into two groups: A study group, with no drainage and a control group with drain inserted at the end of surgery. A total of 121 patients were recruited into two groups. A study group consisted of 59 knees, in which we did not use drainage after TKA and a control group with 62 knees, in which drain was inserted post surgery. Both groups were comparable in terms of preoperative characteristics. The indication for TKA was osteoarthritis (n = 105) and rheumatoid arthritis (n = 16).
Results:
In patients without drainage we observed lower need for opioids, higher blood loss on the 1st postoperative day and a lower need for change of dressings. There were no statistically significant differences in terms of total blood loss, hidden blood loss, transfusion rate, range of motion, length of hospital stay or incidence of complications between the two groups. In 1 year observation there were no differences in clinical outcome between the two groups.
Conclusions:
The present study conclude that there is no rationale for the use of drain after primary TKA. There are benefits in terms of lower opioid intake, lower blood loss on the first postoperative day and lower need for dressing reinforcement during hospitalization.
Keywords: Blood loss, drain, dressing reinforcement, opioids, total knee arthroplasty
MeSH terms: Arthroplasty, replacement, knee, blood loss, surgical drainage suction
INTRODUCTION
The use of drain in joint arthroplasty is a matter of controversy. Suction drains had been traditionally used to prevent the formation of a hematoma which, in turn, may decrease joint mobility, reduce local tissue perfusion and increase the likelihood of an infection. However, there is a paucity of available studies supporting these traditional beliefs. Some authors state that drainage evacuates fluid only from a limited area and does not prevent infection if retrograde migration of bacteria occurs.1,2 It can also impair the early postoperative rehabilitation. In a recent metaanalysis, there is no clear advantage of the use of suction drains, apart from reduced need for change of dressing after total knee arthroplasty (TKA).3,4 Moreover, in patients who had undergone TKA with drainage, the risk of transfusion was higher.3
Majority of authors focus on blood loss and complication rate following TKA with or without drain insertion and there is a paucity of studies evaluating its impact on postoperative pain and intake of analgesics. Thus, we undertook a prospective, comparative study to assess the clinical outcome after primary cemented TKA in patients with or without postoperative drainage.
MATERIALS AND METHODS
124 elective primary TKA were performed in consecutive 111 patients (of them 13 subjects underwent non simultaneous bilateral surgery). The inclusion criteria were knee arthritis impeding daily activities. Exclusion criteria included significant bone loss that required augmentation, previous thromboembolism and intake of opioids preoperatively. We also excluded three patients for other reasons (a woman suffering from Alzheimer's disease, one man speaking a foreign language and one man who refused to participate in the study). The followup rates at 6 and 12 months were 100% and 96%, respectively.
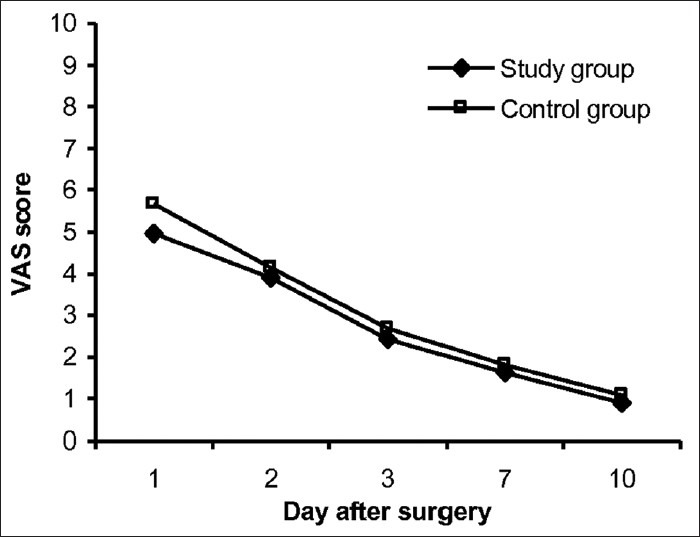
A total of 121 patients were recruited into two groups. A study group consisted of 59 knees, in which we did not use drainage after TKA and a control group with 62 knees, in which drain was inserted post surgery. Both groups were comparable in terms of preoperative characteristics [Table 1]. The indication for TKA was osteoarthritis in 105 and rheumatoid arthritis in 16 subjects.
Table 1.
Clinical details of the patients
The regional ethical committee approved the study protocol and all patients provided informed consent.
Operative procedure
All operations were performed by the senior surgeon (DW). We used two prosthesis systems: Genesis II (Smith and Nephew, Memphis, TN, USA) and Search Evolution (Aesculap, Tuttlingen, Germany). We implanted 100 posterior stabilized prostheses and 21 cruciate retaining (CR) prostheses, all stabilized with cement. Similar numbers of posterior stabilized and CR prostheses were implanted in both groups. A pneumatic tourniquet was applied to each patient. It was deflated after applying compression dressings at the end of the surgery.
Knee arthrotomy was performed through a midline skin incision and a medial parapatellar capsular incision. Patella was everted. In the control group, drainage was placed intraarticularly. It was removed within first 24 h postoperatively.
Apart from spinal anesthesia (119 patients) and general anesthesia (2 patients), in all patients we injected 0.25% bupivacaine solution with epinephrine intraoperatively in the joint capsule, rectus femoris tendon and the infrapatellar fat pad. Skin was closed with intracutaneous continuous sutures. After surgery all patients were monitored in the recovery room for 24 h, where the pain was controlled with intravenous morphine pump infusion. Analgesics were administered on patient's demand under the supervision of a doctor, starting with nonsteroidal anti inflammatory medication. When it was necessary, opioids were given to provide pain relief.
All patients received low molecular weight heparin, starting 12 h before surgery. They also wore compression stockings from the 2nd postoperative day. Antibiotics (cefuroxime 1.5 g and amikacin 0.5 g) were administered intravenously 30 min before surgery. If the operation had extended, antibiotics were continued up to 3 days. Patients were transfused, if their hemoglobin (Hb) level decreased to less than 7.5 g/dL and symptoms of anemia developed.
In each case proper knee alignment was restored. Rehabilitation protocol was the same in both groups. On the 1st postoperative day patients stood up with a walker, performed active flexion of the operated knee up to 90°. Exercises with continuous passive motion were commenced. From the 2nd postoperative day, patients were allowed to walk on crutches with full weight bearing as tolerable.
Assessment
Primary outcome factors
The primary outcome factors in our study were pain intensity and analgesic intake. Pain intensity was measured with the help of a visual analog scale (VAS). Intake of analgesics per patient were determined. The administered drugs were divided according to their membership in the World Health Organization analgesic ladder.
Blood loss and transfusions
In early postoperative period, we recorded Hb and the hematocrit (HCT) levels (preoperatively, then 8 h, 1 day and 2 days after surgery). We assessed the calculated blood loss (CBL), hidden blood loss (HBL), total measured blood loss (TMBL), transfusion rates. CBL was calculated using the Gross formula,5 which uses the maximum reduction in Hb and estimated blood volume, depending on patient's height, weight and gender.6 TMBL was the sum of the intraoperative blood loss noted by the anesthetists and drainage blood loss. HBL was determined by subtracting the TMBL from the CBL.
Dressing reinforcement
We evaluated requirement for dressing reinforcement and the length of hospital stay. During hospitalization all patients had dressings covering the site of drain exit in the control group and similar expected site on skin in the study group.
Radiographic examination
All patients were clinically and radiologically evaluated preoperatively, during hospitalization, then at followup, approximately 6 and 12 months after surgery. Radiographs in the anteroposterior and the lateral view were performed using the Knee Society Roentgenographic Evaluation System, any radiological findings suggesting prosthesis loosening at postoperative visits were determined.7
Range of movement of operated knee, wound problems and complications were assessed postoperatively and on control visits. A doctor performing followup examination was blinded to information about drain usage in a particular patient.
Questionnaires
In addition, patients were assessed with questionnaires, such as Knee Injury and Osteoarthritis Outcome Survey (KOOS) and SF-36 Health Survey version 2 (SF-36 v2) (preoperatively and at followup examinations).
Statistics
Statistical analysis was performed using the Student's t-test, Chi-squared test and Mann-Whitney test, depending on the nature of the variables. Results are expressed as mean and standard deviation (SD) or as mean with range. P <0.05 was considered to be significant.
RESULTS
Primary outcome factors
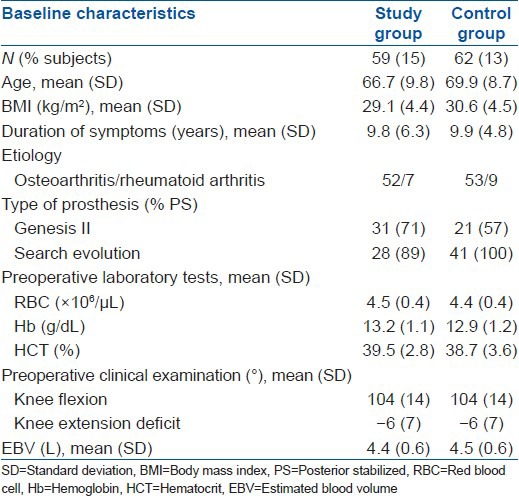
On the day of surgery the intake of analgesics, including i.v. morphine and any supplemental opioids was comparable between both the groups. From the 1st postoperative day up to discharge, we noted lower demand for opioids in the study group compared with the control group [Figure 1]. Patients in the study group required approximately three times less opioids than patients in the control group (mean analgesia request amounted 0.15 and 0.44/patient, respectively) (P < 0.01).
Figure 1.
Bar diagram showing intake of opioids per patient during hospitalization
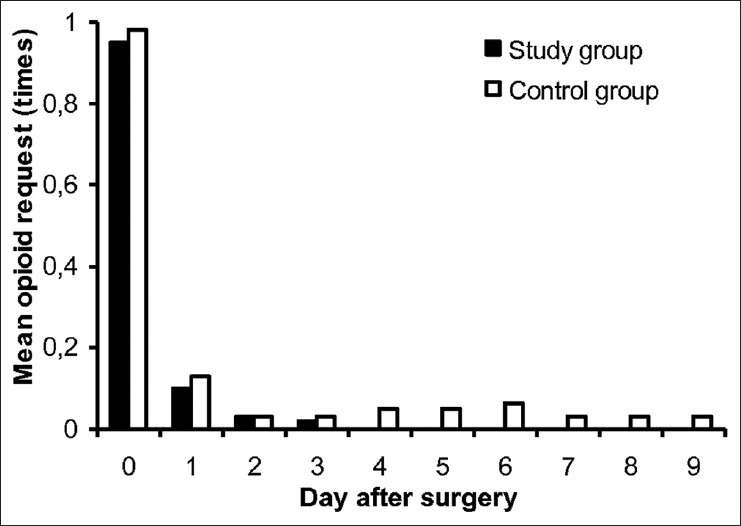
We observed differences in the mean VAS values between both groups, the biggest was seen on the 1st postoperative day, but these results were not significant. VAS values presented a decreasing trend up to discharge [Figure 2].
Figure 2.
Graph showing postoperative pain intensity
Blood loss and transfusions
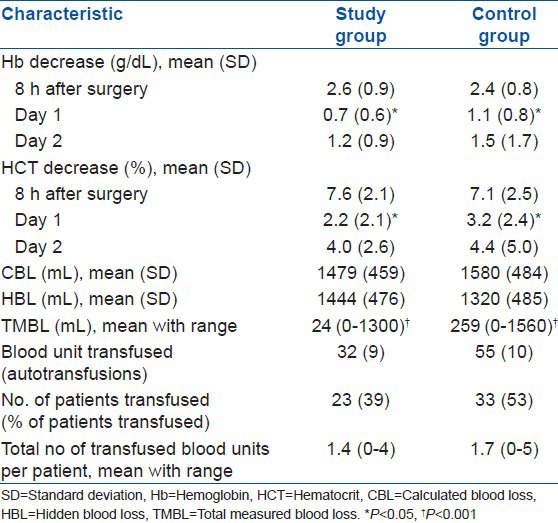
The mean of blood collection in the postoperative drain in the control group was 229 mL (SD 200 mL). In both groups, the values of Hb and HCT decreased during the 1st 2 postoperative days (P < 0.01). In addition, on the 1st postoperative day, we noted statistically significant average reduction in Hb and HCT levels in the control group compared with the study group (P < 0.05). There were no significant differences between both groups in CBL, HBL and transfusion rates. Evaluation of blood loss is shown in Table 2. CBL in patients who needed a blood transfusion compared with those, who did not need it, was 1542 mL (SD 557 mL) and 1438 mL (SD 384 mL) in the study group, whereas in the control group it was 1542 mL (SD 538 mL) and 1625 mL (SD 420 mL), respectively.
Table 2.
Blood loss and transfusion requirements
Dressing reinforcement
We recorded a significant difference in dressing reinforcement (P < 0.01). In the study group every patient needed the dressing to be changed at an average 4.5 ± 1.1 times during hospitalization compared with 5.0 ± 1.2 times in the control group. Each patient had at least three dressing reinforcements. We also noted that 7 patients from the control group required regular dressing changes due to prolonged oozing from the wound after drain removal.
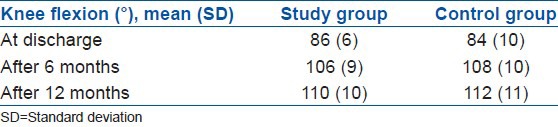
Range of motion
There were no significant differences between the groups in the range of motion or length of hospital stay. All patients achieved full extension of the operated knee at discharge. The knee flexion was comparable between the two groups [Table 3]. Patients from both groups were discharged after 10 days.
Table 3.
Range of motion in operated knee
Complications
Complications were observed in six patients from the study group namely; four wound related: prolonged wound healing (n = 3), prolonged healing of injured scar (n = 1) and two general: gastrointestinal hemorrhage and respiratory tract infection. There were 11 complications in the control group. We observed four wound-related problems: Superficial wound infection (1), prolonged wound healing demanding secondary suture (1), persistent leg edema (2) and seven general: Cerebrovascular accident (1), myocardial infarction (1), erysipelas (1), respiratory tract infection (1), and urinary tract infection (3). No knee required any aspiration. There were no other complications 6 and 12 months after surgery. In three patients from the control group, the drain was accidentally removed shortly after its insertion.
Questionnaires
The two groups were comparable in terms of preoperative KOOS and SF-36 outcomes, apart from KOOS activity of daily living subscale (ADL) and SF-36 bodily pain score (BP), which were significantly higher in the study group (P < 0.05). Average functional outcome in both groups improved during followup. The results obtained did not differ significantly between the two groups. Changes in questionnaires scores are displayed in Figures 3 and 4.
Figure 3.
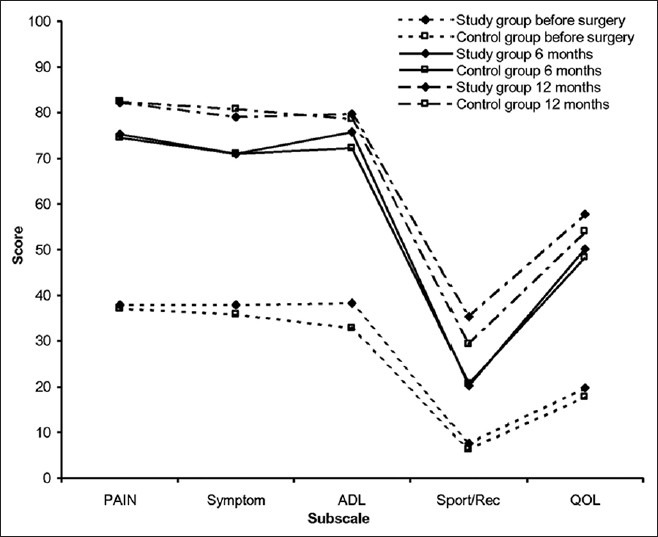
A line graph showing change over time in knee injury and osteoarthritis outcome survey scores. ADL = Function in daily living, Sport/Rec = Function in sport and recreation, QOL = Quality of life
Figure 4.
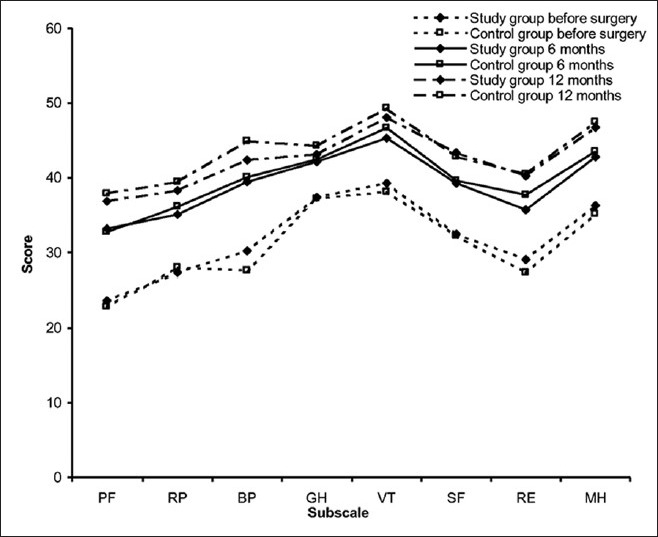
A line graph showing change over time in SF-36 scores. PF = physical functioning, RP = Role physical, BP = Bodily pain, GH = General health, VT = Vitality, SF = Social functioning, RE = Role emotional, MH = Mental health
DISCUSSION
Waugh and Stinchfield are the first authors who advocated the use of drains in modern orthopaedics.8 Most of the recent prospective randomized studies have shown no benefits with its use.9,10,11,12,13,14 Nevertheless, according to Chandratreya, 94% of British Orthopedic Association members use drains after TKA in their practice.15 Much of available reports concentrate on blood loss in the presence of a drain,10,11,12,14,16 while very few assess its influence on pain and analgesics requirement.1,17,18 In this study, we observed significantly higher need for opioids in patients with drain, which is distinct from prior reports. Slightly higher mean pain scores were seen in the control group, especially on the 1st postoperative day, when the drain was present but the difference was not significant.
To the best of our knowledge, this is the first study to show that patients after TKA who had a drain, need higher doses of opioids. A study done by Holt et al. observed no statistically significant difference in postoperative opioid consumption after TKA, regardless of the presence of a drain.17 Confalonieri et al. evaluated patients after unicompartmental knee arthroplasty and noted lower analgesic requirements on the 1st postoperative day in patients without drain.19 However, the authors did not specify what kind of analgesics was applied.
Disruption of continuity of skin and deeper tissues along with the application of the drain causes peripheral sensitization, resulting in a decrease of nociceptors threshold.20 In addition concentration of local inflammatory mediators increases and secondarily induces central sensitization. This two level action causes pain hypersensivity and persistent decrease in the pain threshold at the site of injured as well as surrounding uninjured tissues. Moreover, opioid receptors are present in inflamed tissues.21 It is possible that weaker analgesics are insufficient to control this pain. In contrast, opioid analgesics may sometimes cause adverse effects.22
Yiannakopoulos and Kanellopoulos emphasized the often neglected fact, that drain tube removal causes pain and discomfort.23 It is especially important, because proper pain management is considered to be fundamental for minimizing postoperative stress and improving the quality of life and comfort after surgery.
Although some articles suggest that a suction drain does not increase blood loss after TKA,10,16,18 other authors demonstrated higher blood loss when it was used.1,3,14 We confirm these results since we noted significant average reduction of Hb and HCT in drained patients on the first postoperative day. The possible explanation of this is that the presence of a drain reduces the tamponade effect.
The decrease of Hb concentration can lead to a higher probability of blood transfusion.12,14,16,18 Although we observed no significant differences in the overall transfusion rates in both groups, paradoxically in the drained group we have seen lower CBL in transfused patients compared to those who did not necessitate it. This may be associated with the fact that decision regarding transfusion was made not only by the orthopedic surgeon, but also by anesthetist. It seems that the presence of the drain was automatically treated by them as a risk factor for greater blood loss and regardless of indications, resulted in blood transfusion. It was not only our remark. Audet et al. established that blood transfusion after elective orthopedic surgery was reasonable in 68% cases on the day of surgery and in the next days it decreased to 35%.24 The drained blood volume recorded in our analysis was smaller compared with data from other authors.11,12 It may be a result of techniques to reduce blood loss which we used. These consist of tourniquet use, cementing of the prosthesis, local epinephrine infusion, minimally invasive manipulations on soft tissues.
In our study, we observed that significantly more changes of dressing were made in drained patients. Dora et al. had similar findings after total hip arthroplasty.13 Until date, most authors assessing this issue reported that in the absence of drain the need for dressing reinforcement was higher or at least did not differ significantly.12,17 Minnema et al. revealed that drainage is an independent risk factor for infection after TKA.2 On the other hand, Ovadia et al. evaluated 58 patients following TKA and found significantly higher serous wound discharge when the drain was not used.16 Nevertheless, it did not affect the complication rate. Our analysis of range of motion, length of hospital stay and other outcomes as assessed with KOOS and SF-36 questionnaires showed no differences between both the groups.
Our study has some limitations. The number of subjects were small but comparable to other studies.1,17 The difference in opinions on transfusion criteria between orthopedic surgeons and anesthetists might have affected the transfusion rate.
We conclude that there is no rationale for the use of drain after primary TKA. There are benefits in terms of lower opioid intake, lower blood loss on the first postoperative day and lower need for dressing reinforcement during hospitalization.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Esler CN, Blakeway C, Fiddian NJ. The use of a closed-suction drain in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 2003;85:215–7. doi: 10.1302/0301-620x.85b2.13357. [DOI] [PubMed] [Google Scholar]
- 2.Minnema B, Vearncombe M, Augustin A, Gollish J, Simor AE. Risk factors for surgical-site infection following primary total knee arthroplasty. Infect Control Hosp Epidemiol. 2004;25:477–80. doi: 10.1086/502425. [DOI] [PubMed] [Google Scholar]
- 3.Parker MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2004;86-A:1146–52. doi: 10.2106/00004623-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Tucci G, Amorese V, Romanini E. Closed suction drainage after orthopaedic surgery: evidence versus practice. J Orthop Traumatol. 2006;7:29–32. [Google Scholar]
- 5.Gross JB. Estimating allowable blood loss: Corrected for dilution. Anesthesiology. 1983;58:277–80. doi: 10.1097/00000542-198303000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Can J Surg. 2001;44:33–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 8.Waugh TR, Stinchfield FE. Suction drainage of orthopaedic wounds. J Bone Joint Surg Am. 1961;43-A:939–46. [PubMed] [Google Scholar]
- 9.Cobb JP. Why use drains? J Bone Joint Surg Br. 1990;72:993–5. doi: 10.1302/0301-620X.72B6.2246304. [DOI] [PubMed] [Google Scholar]
- 10.Ritter MA, Keating EM, Faris PM. Closed wound drainage in total hip or total knee replacement. A prospective, randomized study. J Bone Joint Surg Am. 1994;76:35–8. doi: 10.2106/00004623-199401000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Adalberth G, Byström S, Kolstad K, Mallmin H, Milbrink J. Postoperative drainage of knee arthroplasty is not necessary: A randomized study of 90 patients. Acta Orthop Scand. 1998;69:475–8. doi: 10.3109/17453679808997781. [DOI] [PubMed] [Google Scholar]
- 12.Niskanen RO, Korkala OL, Haapala J, Kuokkanen HO, Kaukonen JP, Salo SA. Drainage is of no use in primary uncomplicated cemented hip and knee arthroplasty for osteoarthritis: A prospective randomized study. J Arthroplasty. 2000;15:567–9. doi: 10.1054/arth.2000.6616. [DOI] [PubMed] [Google Scholar]
- 13.Dora C, von Campe A, Mengiardi B, Koch P, Vienne P. Simplified wound care and earlier wound recovery without closed suction drainage in elective total hip arthroplasty. A prospective randomized trial in 100 operations. Arch Orthop Trauma Surg. 2007;127:919–23. doi: 10.1007/s00402-006-0260-0. [DOI] [PubMed] [Google Scholar]
- 14.Li C, Nijat A, Askar M. No clear advantage to use of wound drains after unilateral total knee arthroplasty: A prospective randomized, controlled trial. J Arthroplasty. 2011;26:519–22. doi: 10.1016/j.arth.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 15.Chandratreya A, Giannikas K, Livesley P. To drain or not drain: Literature versus practice. J R Coll Surg Edinb. 1998;43:404–6. [PubMed] [Google Scholar]
- 16.Ovadia D, Luger E, Bickels J, Menachem A, Dekel S. Efficacy of closed wound drainage after total joint arthroplasty. A prospective randomized study. J Arthroplasty. 1997;12:317–21. doi: 10.1016/s0883-5403(97)90029-2. [DOI] [PubMed] [Google Scholar]
- 17.Holt BT, Parks NL, Engh GA, Lawrence JM. Comparison of closed-suction drainage and no drainage after primary total knee arthroplasty. Orthopedics. 1997;20:1121–4. doi: 10.3928/0147-7447-19971201-05. [DOI] [PubMed] [Google Scholar]
- 18.Jenny JY, Boeri C, Lafare S. No drainage does not increase complication risk after total knee prosthesis implantation: A prospective, comparative, randomized study. Knee Surg Sports Traumatol Arthrosc. 2001;9:299–301. doi: 10.1007/s001670100220. [DOI] [PubMed] [Google Scholar]
- 19.Confalonieri N, Manzotti A, Pullen C. Is closed-suction drain necessary in unicompartmental knee replacement? A prospective randomised study. Knee. 2004;11:399–402. doi: 10.1016/j.knee.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Busch CA, Shore BJ, Bhandari R, Ganapathy S, MacDonald SJ, Bourne RB, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006;88:959–63. doi: 10.2106/JBJS.E.00344. [DOI] [PubMed] [Google Scholar]
- 21.Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995;332:1685–90. doi: 10.1056/NEJM199506223322506. [DOI] [PubMed] [Google Scholar]
- 22.Bonnet F, Marret E. Postoperative pain management and outcome after surgery. Best Pract Res Clin Anaesthesiol. 2007;21:99–107. doi: 10.1016/j.bpa.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Yiannakopoulos CK, Kanellopoulos AD. Innoxious removal of suction drains. Orthopedics. 2004;27:412–4. doi: 10.3928/0147-7447-20040401-19. [DOI] [PubMed] [Google Scholar]
- 24.Audet AM, Goodnough LT, Parvin CA. Evaluating the appropriateness of red blood cell transfusions: The limitations of retrospective medical record reviews. Int J Qual Health Care. 1996;8:41–9. doi: 10.1093/intqhc/8.1.41. [DOI] [PubMed] [Google Scholar]


