Abstract
The present study looked at the emergence of clinically significant problems in behavior, executive function skills (EF), and social competence during the initial 18 months following TBI in young children relative to a cohort of children with orthopedic injuries (OI) and the environmental factors that predict difficulties postinjury. Children, ages 3-7 years, hospitalized for severe TBI moderate TBI, or OI were seen shortly after their injury (M = 40 days) and again 6 months, 12 months, and 18 months postinjury. Behavioral parent self-reports, demographic data, family functioning reports, and home environment reports were collected at injury baseline and each time point post injury. Results suggest that, compared to the OI group, the severe TBI developed significantly more externalizing behavior problems and EF problems following injury that persisted through the 18-month follow-up. Minimal social competence difficulties appeared at the 18-month follow-up, suggesting a possible pattern of emerging deficits rather than a recovery over time. Predictors of the emergence of clinically significant problems included permissive parenting, family dysfunction, and low SES. The findings are similar to those found in school-aged children.
Keywords: Traumatic Brain Injury, Early Childhood, Behavior Problems
Traumatic brain injury (TBI) is the leading cause of acquired disability in children in the United States. As many as 435,000 children between the ages of 0 and 14 are treated in the emergency department each year with TBI. An additional 37,000 are hospitalized for a TBI and 2,685 die annually (Langlois, Rutland-Brown, & Thomas, 2006). In addition to cognitive and behavioral problems during the acute phase of TBI, persistent patterns of behavioral problems can be observed many months or even years postinjury (Anderson, Morse, Catroppa, Haritou, & Rosenfeld, 2004; Fay et al., 2009; Max et al., 2005; Schwartz et al., 2003; Yeates et al., 2005). Although a wealth of information exists regarding the effect of TBI on school-aged children, the relationship between early childhood TBI and subsequent behavioral problems is less well-established.
Evidence suggests that school-aged children suffering from TBI have increased behavioral, executive functioning (EF; i.e. planning, problem solving, organization, working memory), and social problems. Secondary onset attention deficit hyperactivity disorder (SADHD) is a significant behavior problem affecting children with TBI, leading to the development of inattention, hyperactivity, and impulsivity, often occurring with comorbid externalizing behavior problems (Max et al., 2005b). Researchers have found that within 1 year of injury, a large percentage of children suffering from severe TBI developed increased behavior problems, compromised self-regulatory behaviors, and/or clinically significant levels of executive dysfunction (Fletcher, Ewing-Cobbs, Miner, Levin, & Eisenberg, 1990; Ganesalingam et al., 2006; Sesma et al., 2008; Schwartz et al., 2003). Deficits in a wide range of domains have been found in severe TBI in early childhood, such as attentional problems and social skill difficulties (Anderson and colleagues, 2004; Catroppa, Anderson, Morse, Haritou, & Rosenfeld, 2007; Fletcher, Ewing-Cobbs, Miner, Levin, & Eisenberg, 1990; Landry, Swank, Stuebing, Prasad, & Ewing-Cobbs, 2004), but these results have been less well-established and relatively few studies have focused on behavioral outcomes of early childhood TBI.
Evidence from longitudinal studies suggests that internalizing symptoms tend to increase over time post injury, with less marked changes following moderate TBI (Anderson, Catroppa, Dudgeon, Morse, & Rosenfeld, 2006). Similarly, children with severe TBI have persisting deficits relative to children with less severe TBI or control groups without TBI in social problem-solving skills, parent ratings of executive function, and adaptive behavior (Anderson, Catroppa, Dudgeon, Morse, & Rosenfeld, 2006; Janusz, Kirkwood, Yeates, & Taylor, 2002; Landry et al., 2004). Past studies have found that these behavioral outcomes are related to both TBI severity and to environmental factors, such as family functioning, home environment, and psychosocial adversity (Anderson et al., 2006; Max et al., 2005a; Max et al., 2005b; Wade et al., 1996; Nadebaum, Anderson, & Catroppa, 2007; Sesman et al., 2008). Although persistent cognitive and learning problems having been documented following early TBI, behavioral difficulties are a more significant source of family distress and burden (Anderson et al., 2004; Arroyos-Jurado, Paulsen, Merrell, Lindgren, & Max, 2000; Max et al., 2005a; Max et al., 2005b; Yeates et al., 2005).
Studies examining clinically significant problems over time provide valuable information about the effects of TBI on children's everyday functioning. Because most existing studies have examined children injured at school age, investigations of outcomes following TBI in young children are especially critical. While pediatric injury has been linked to higher incidence of internalizing and externalizing symptoms in school-aged children (Anderson, Catroppa, Dudgeon, Morse, & Rosenfeld, 2006; Schwartz et al., 2003; Yeates et al., 2003), there is evidence that secondary-ADHD is a significant problem that should also be investigated in a younger sample of children (Max et al., 2005; Max et al., 2005b). Similarly, although there has been less of a focus on social competence and executive functions in young children, TBI has been shown to adversely affect social functioning, social problem-solving, and executive functioning in school-aged children (Anderson, Catroppa, Dudgeon, Morse, & Rosenfeld, 2006; Janusz, Kirkwood, Yeates, & Taylor, 2002; Landry et al., 2004). For this reason, we thought to examine levels of internalizing, externalizing, ADHD-like symptoms, executive function, and social competence in a sample of younger children. Examination of environmental factors in relation to these outcomes is also needed to understand how these factors influence behavioral recovery and to identify potential targets for intervention. To further these aims, the present study examined rates of postinjury behavior problems reported by parents on standardized measures of behavior problems, executive function, and social competence in a cohort of 3- to 6-year-old children with TBI relative to a cohort of children with orthopedic injuries (OI). Specific aims were to: 1) examine rates of new behavior problems across the initial 18 months post injury as a function of injury type (TBI vs. OI) and severity; and 2) identify non-injury factors associated with these outcomes by investigating associations of preinjury child functioning and characteristics of the family environment on emerging behavior disorders. We chose self-report measures that would individually assess the different aspects of behavior problems, executive dysfunction, and social competence difficulties that have been found in school-aged children in previous research. Based on aforementioned research, we hypothesized that children with severe TBI (sevTBI) would have higher rates of internalizing, externalizing, and ADHD-like behavior problems as well as executive dysfunction and social competence difficulties than children with OI. We anticipated that children with moderate TBI (modTBI) would also have higher rates of these outcomes compared to the OI group, though we expected these differences to be less pronounced that those between the sevTBI and OI groups. We further hypothesized that rates of persisting behavior problems would be higher in children with premorbid behavior problems and in children from less advantaged family environments, as defined by greater family dysfunction, lack of physical resources (i.e. age-appropriate toys, money), and permissive or authoritarian parenting style. We also explored the possibility that the effects of TBI on behavioral outcomes would be moderated by these non-injury factors, with more pronounced effects of TBI in children with preinjury behavior problems and less advantaged family environments.
Methods
Sample
The sample consisted of 198 participants recruited from a prospective, longitudinal investigation of recovery from early childhood TBI. Individuals were recruited from three children's hospitals and one general hospital in Ohio. All participants underwent assessments during the post-acute period (no longer than 3 months post injury) which included neuropsychological examination and parent-based ratings of preinjury child behavior and functioning, preinjury family environment, current caregiver functioning, and injury-related burdens.
Inclusionary criteria included TBI between 36 and 83 months of age at the time of injury, no evidence of child abuse as cause of the injury, no history of documented neurological problems or developmental delays pre-injury, and English as the primary language in the home. The sample was divided into three diagnostic groups: severe TBI (sevTBI), moderate TBI (modTBI), and OI. Children in both TBI groups were hospitalized for at least one night. Additional eligibility criteria included an alteration of neurological functioning as measured by a Glasgow Coma Scale (GCS) of < 13 and/or evidence of neurological insult as seen on magnetic resonance imaging (MRI) or computerized tomography (CT). Children in the sevTBI group had had a GCS score of ≤ 8 as the lowest post-resuscitation score, whereas those in the modTBI group had either a GCS score of 9-12 or a GCS score of 13-15 accompanied by evidence of neurological insult on imaging. The OI group included children who sustained a bone fracture (other than to the skull), had no alterations in consciousness or other symptoms of head trauma, and who were hospitalized overnight due to the injury. Recruitment of a comparison group of children with OI controlled for the experience of hospitalization for a traumatic injury as well as for preinjury behavioral and family characteristics that may contribute to the risk for injury. Fifteen children with mild TBI (GCS score of 13 or 14 without evidence of imaging abnormalities) were excluded from the current analyses in order to focus on more severe injuries.
From a total sample of 84 children with TBI and 114 with OI, 18 dropped out of the study after the baseline visit and 11 (3 modTBI, 2 sevTBI, 6 OI) had been formally evaluated for behavior problems (primarily ADHD) prior to injury and were thus excluded from the analyses. The final sample consisted of 169 children, including 21 with sevTBI (M age = 4.93; SD = .96), 55 with modTBI (M age = 4.94; SD = 1.19), and 90 with OI (M age = 5.01; SD = 1.08). The demographic characteristics of the sample are summarized in Table 1. No significant differences were found between study participants included in data analyses and those not included because they had a history of pre-injury behavior problems in terms of group membership (sevTBI, modTBI, OI) or demographic characteristics. Among the individuals included in the study, the TBI group was hospitalized significantly longer than the OI group. The groups also differed significantly on average IQ scores as assessed postinjury, and overall injury severity.
Table 1.
Demographic Information by Injury Group
| Injury Group | F | |||
|---|---|---|---|---|
| SevTBI | ModTBI | OI | ||
| Number in sample | 21 | 55 | 93 | |
| Average Age at Injury (yrs) | 4.93 (0.96) | 4.94 (1.19) | 5.01 (1.08) | 0.09 |
| Sex (% male) | 67% | 58% | 53% | 1.49a |
| Race (% non-white) | 29% | 33% | 24% | 1.46a |
| Avg. Hospital Stay (days) | 9.74 (20.79) | 2.09 (1.91) | 0.77 (1.09) | 11.91* |
| Family Income (SD) | $53,362.32 ($16,346.13) | $60,412.38 ($25,872.85) | $64,596.47 ($24,216.61) | 1.89 |
| ISSb | 13.50 (8.04) | 14.72 (7.67) | 7.03 (2.48) | 37.82* |
| Avg. estimated IQc | 85.37 (15.97) | 98.15 (15.98) | 102.44 (14.45) | 10.20* |
p< .01
Chi-Square value
ISS is an injury severity scale used to assess individuals who have sustained multiple injuries
IQ was estimated using the two subtest Wechsler Abbreviated Scale of Intelligence
Procedures
Informed consent was obtained from the parent or legal guardian of each child once the child was stabilized in the hospital. Medical charts were reviewed for relevant injury and imaging information. Baseline visits were conducted as soon as possible following medical stabilization, at which time parents/guardians were interviewed to obtain background, demographic, and injury information. At each subsequent follow assessment (6, 12, and 18 months post injury), parents completed questionnaires assessing familial characteristics and dysfunction, parental distress as a result of the injury, and ratings of child behavior, executive function (EF), and social competence. Although the present study focuses on parent-based measures of behavior, neuropsychological tests were also administered to the children at the baseline visit and at each follow-up (Taylor et al., 2008).
Self-Report Measures
Child Behavior/Performance Measures
The Child Behavior Checklist (CBCL, Achenbach & Rescorla, 2000; Achenbach & Rescorla, 2001) is a widely used parent rating of child behavior problems. For purposes of this study, T-scores from the CBCL Internalizing Problem Scale, Externalizing Problem Scale, and ADHD Problems (DSM-oriented) Subscale were used in data analysis to focus on those behaviors that are most problematic within family and school settings. As in previous studies (Schwartz et al., 2003), we used the clinical cutoff score of T=63 as an index of clinically significant behavior problems. This T score corresponds to ratings obtained by less than 10% of the normative sample. Parents with children younger than the age of 6 received the CBCL 1 ½ - 5 version and those with children 6 or older received the CBCL 6 - 18.
Parents also completed the Behavior Rating Inventory of Executive Function (BRIEF), with the preschool version (Gioia, Espy, & Isquith, 2000) employed for children 2 to nearly 6 years of age and the school-age version (Gioia, Isquith, Guy, & Kenworthy, 2000) for children 5 to 18 years of age. For the purposes of this study, parents with children younger than 6 received the preschool version and those with children 6 or older received the school-age version. The BRIEF is a parent rating of children's executive function that demonstrates high levels of internal consistency and stability, and acceptable levels of interrrater reliability and test-retest reliability. The total score from this scale, or General Executive Composite (GEC), was used in this study as a broad-based measure of executive function. A clinical cutoff of T=63 was also used for the BRIEF-GEC, a score that corresponds to ratings given by less than 10% of the normative sample.
The Preschool and Kindergarten Behavior Scales Second edition (PKBS-2, Merrell, 2002) and the Home and Community Social and Behavior Scales (HCSBS, Merrell, 2002) are measures of social competence and antisocial behaviors in preschool (ages 3 – 6 years) and school-aged children (ages 5-18 years), respectively. For the purposes of this study, parents of children younger than 6 received the preschool version and those with children 6 or older received the school-aged version. The PKBS-2 has strong internal consistency reliability, moderate to high test-retest reliability, and adequate interrater reliability (Merrell, 2002). The HCSBS also demonstrates strong internal consistency and high interrater reliability (Merrell, 2002). For this study, the composite of the social scales of the PKBS-2, that included social cooperation, social interaction, and social independence subscales, was used; for the HCSBS, the social competence total was employed. To enable comparisons across measures, the corresponding summary scales from each measure were transformed to sample z scores (i.e., those from the PKBS-2 for children 3-4 years and those from the HCSBS for children 5 years and older). Evidence in support of the assumption that the two sets of z scores provided equivalent measures was provided by the substantial correlations of these scores across time. Z-scores less than or equal to -1.33 were considered clinically elevated.
Family Functioning Measures
The 12-item General Functioning subscale of the McMaster Family Assessment Device (FAD-GF, Byles, Byrne, Boyle, & Oxford, 1988; Miller, Bishop, Epstein, & Keitner, 1985) was used to assess family functioning. The FAD-GF scores range from 1.0 (healthy) to 4.0 (unhealthy). The measure has adequate reliability and is related to outcomes of TBI (Taylor, Yeates, Wade, Drotar, & Klein, 1999). To further assess the family environment, we also administered the Life Stressors and Social Resources Inventory – Adult Form (LISRES-A, Moos & Moos, 1994). The LISRES is widely used in stress and support research and has established reliability and both concurrent and predictive validity (Moos & Moos, 1994; Taylor et al., 2002). In the current study, we considered only parental interpersonal stressors, defined as the average of the T scores for each of the relationship stressors domains (spouse, extended, family, friends, co-workers). Finally, to assess influences of parenting styles on behavioral outcomes, we administered the 62-item Parenting Practices Questionnaire (PPQ; Robinson, Mandleco, Olsen, & Hart, 1995), a retrospective, Likert scale assessing the extent to which parents characterize themselves along the dimensions of authoritative, authoritarian, and permissive parenting prior to the injury as assessed at the baseline visit. Correlations of the three subscales of the PPQ with Baumrind's parenting typology provide evidence for construct validity (Robinson, Hart, Mandleco, Olsen, Russell, Aloa et al., 1996). Research on this typology indicates that both authoritarian and permissive parenting styles are associated with more child behavior problems than authoritative parenting styles (Querido, Warner, & Eyberg, 2002; Bayer, Sanson, & Hemphill, 2006; Deater-Decker & Dodge, 1997).
Home Environment
The Home Observation for Measures of the Environment (HOME, Bradley & Caldwell, 1984; Caldwell & Bradley, 1984) was administered at children's homes to assess the extent to which the home environment was conducive to positive interactions with children and supportive of their development. The HOME consists of information obtained via parent interview and direct observations of parent-child interactions and play or learning materials in the home. The HOME has satisfactory levels of interrater reliability and validity in predicting children's cognitive and social/emotional development (Bradley & Caldwell, 1984; Caldwell & Bradley, 1984). The total score from the HOME was used in analysis as an index of the degree of stimulation provided to the child in the home environment.
Socioeconomic Status (SES)
SES was defined in terms of a composite of maternal education and median income for the census tract in which the family resided. The composite was computed by averaging the sample z scores of the two variables. This composite score has been shown to function well as a proxy measure of SES in previous TBI studies (Taylor, Yeates, Wade, Drotar, Stancin, & Minich, 2002).
Data Analysis
General estimating equations (GEE) logistic regression analysis was used to examine differences between injury groups (sevTBI, modTBI, and OI) in rates of behavior problems and deficits in executive function and social competence at each follow-up assessment. Each individual received a dichotomous score indicating whether he or she had clinically elevated ratings for each dependent variable at each time point. Continuous ratings of preinjury functioning for each of the outcomes, obtained at the baseline assessment, were included as covariates in the analysis to control for premorbid behavioral symptoms and thereby enabling us to examine postinjury change. Analysis of the data revealed trends for racial and SES differences between the groups, so they were added into the models as covariates to statistically control for the association of these factors with the dependent measures. Our goal was to treat race and SES as covariates while examining the main and moderating influences of proximal social environmental characteristics such as parenting and home environment. Alpha rates were set at .05 overall, but were Bonferroni adjusted for the CBCL to .017 to control for multiple comparisons using subscales from the same measure,
Preliminary analysis revealed higher rates of preinjury problems in the sevTBI group than in the OI group on one measure (i.e., PKBS/HCSBS), even after excluding children with premorbid behavior problems. However, the baseline assessment took place as long as 3 months after injury, so it is possible that some baseline assessments of preinjury status were biased by the children's postinjury behavior or the groups actually differed premorbidly. To test the hypothesis that children with higher preinjury rates of symptoms were more likely to develop clinically significant problems postinjury, we examined interactions involving each premorbid measure raw score by injury group using GEE logistic regression analysis.
After examining group differences in rates (or odds) of behavior problems, environmental factors were included in mixed models logistic regression analyses to determine if these factors contributed to outcomes independent of injury group or if they moderated injury effects. To understand the relationship between injury, environmental factors, and significant behavior problems postinjury, mixed model logistic regression analyses were conducted with family functioning, stresses and resources, home environment and parenting practices as potential moderators, that is, including their interactions with TBI, and linear and quadratic terms for time. Starting with a full model including all of the aforementioned terms, the final, most parsimonious model was selected using Akaike's information criterion (AIC). AIC sums the negative log (Likelihood) and twice the total number of parameters in the model, k (AIC = -log(L) + 2k), so that models with smaller AIC are considered more parsimonious. AIC has been shown to provide robust selection of parsimonious models, given a set of candidate models and is preferred over null-hypothesis testing approaches (e.g., F-tests) when attempting to evaluate many competing models (Burnham & Anderson, 2002; Burnham & Anderson, 2004). AIC is less conservative than the Bayesian Information Criterion and allowed for us to select a single model that retained the most terms. The most parsimonious model was then fit with Bayesian methods to get estimates of effects and Bayesian credible intervals on those effect sizes (Gelman et al. 2004). We used uninformative priors, where initial parameter estimates (priors) were drawn from normal distributions with means of zero and variances of 1000. A 95% Bayesian credible interval is the interval in which we are 95% sure the true estimate lies.
Results
Correlation analyses were conducted to determine the intercorrelations of the five behavior, executive function, and social competence ratings (CBCL: Internalizing, CBCL: ADHD, CBCL: Externalizing, BRIEF: GEC, and PKBS/HCSBS). All five measures were significantly correlated at the p<.01 level. The intercorrelations between the CBCL scales ranged from .54 to .74. Correlations between the CBCL scales and the BRIEF GEC scales ranged from .64 to .78. Correlations between the CBCL scales and BRIEF GEC with the PKBS/HCSBS scores ranged from -.42 to -.55.
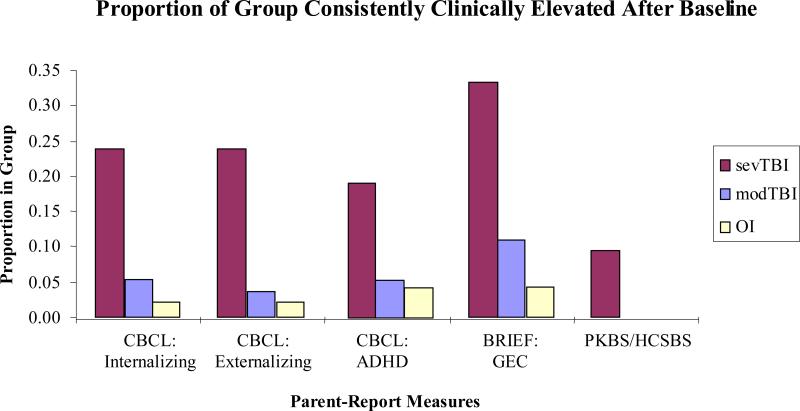
SevTBI was a significant predictor of clinically significant elevations on the CBCL: Externalizing (p<.0001) and ADHD scales (p = .002), BRIEF: GEC scale (p = .01), and PKBS/HCSBS (p = .01, see Table 2). No significant interactions were detected between injury group and time at testing on any behavioral measures, suggesting a relatively stable level of impairment across time (see Table 3 for N and percentages of kids elevated at each time point). Sixty-two percent of the sevTBI group, 42% of the modTBI group, and 29% of the OI group experienced clinically significant elevations on one or more of the measures at some point postinjury. The sevTBI group had a higher proportion of children consistently elevated (i.e., above the cut-off at all 3 postinjury assessments; see Figure 1 for consistent patterns of impairment within each group for each parent-report measure). The same GEE analyses were conducted with this sample, but this time including the children who were initially excluded due to previous behavior problem diagnoses to see if model results changed. There were no changes in the GEE logistic regression models; sevTBI remained the only significant predictor of clinically significant elevations.
Table 2.
Generalized Estimation Equation Analysis with Baseline as Continuous Covariate
| Estimate | St.Error | Lower CI | Upper CI | Z | p | |
|---|---|---|---|---|---|---|
| CBCL: Internalizing | ||||||
| Baseline Score | 0.16 | 0.03 | 0.09 | 0.23 | 4.63 | <.0001 |
| sevTBI | 1.62 | 0.79 | 0.07 | 3.16 | 2.04 | 0.04 |
| modTBI | 0.51 | 0.60 | −0.66 | 1.68 | 0.86 | 0.39 |
| Race | −0.15 | 0.53 | −1.19 | 0.88 | −0.29 | 0.77 |
| SES | −0.49 | 0.29 | −1.05 | 0.07 | −1.71 | 0.09 |
| CBCL: Externalizing | ||||||
| Baseline Score | 0.17 | 0.03 | 0.12 | 0.23 | 5.77 | <.0001 |
| sevTBI | 3.22 | 0.75 | 1.74 | 4.69 | 4.27 | <.0001 |
| modTBI | 0.70 | 0.59 | −0.45 | 1.85 | 1.20 | 0.23 |
| Race | 0.00 | 0.57 | −1.11 | 1.12 | 0.00 | 1.00 |
| SES | 0.16 | 0.28 | −0.39 | 0.71 | 0.56 | 0.57 |
| CBCL: ADHD | ||||||
| Baseline Score | 0.16 | 0.03 | 0.09 | 0.23 | 4.69 | <.0001 |
| sevTBI | 2.01 | 0.66 | 0.71 | 3.31 | 3.03 | 0.00 |
| modTBI | 0.49 | 0.51 | −0.51 | 1.48 | 0.96 | 0.34 |
| Race | 0.10 | 0.53 | −0.94 | 1.14 | 0.19 | 0.85 |
| SES | −0.59 | 0.27 | −1.12 | −0.06 | −2.19 | 0.03 |
| PKBS/HCSBS | ||||||
| Baseline Score | −0.99 | 0.22 | −1.43 | −0.56 | −4.45 | <.0001 |
| sevTBI | 2.27 | 0.84 | 0.63 | 3.91 | 2.71 | 0.01 |
| modTBI | 1.08 | 0.79 | −0.47 | 2.64 | 1.37 | 0.17 |
| Race | −0.71 | 0.61 | −1.90 | 0.49 | −1.16 | 0.25 |
| SES | −0.47 | 0.42 | −1.30 | 0.36 | −1.11 | 0.27 |
| BRIEF: GEC | ||||||
| Baseline Score | 0.13 | 0.02 | 0.09 | 0.18 | 6.17 | <.0001 |
| sevTBI | 1.63 | 0.65 | 0.36 | 2.90 | 2.52 | 0.01 |
| modTBI | 0.56 | 0.45 | −0.32 | 1.44 | 1.24 | 0.21 |
| Race | −0.62 | 0.48 | −1.57 | 0.33 | −1.28 | 0.20 |
| SES | −0.37 | 0.23 | −0.81 | 0.07 | −1.63 | 0.10 |
Table 3.
Number and Percentage of Kids Elevated on Each Measure at Each Time Point
| CBCL: Internalizing | CBCL: Externalizing | CBCL: ADHD | BRIEF: GEC | PKBS/HCSBS | |
|---|---|---|---|---|---|
| Baseline | |||||
| sevTBI N (%) | 4 (20) | 4 (20) | 3 (15) | 4 (21) | 3 (16) |
| modTBI N (%) | 4 (7) | 4 (7) | 4 (7) | 8 (15) | 1 (2) |
| OI N (%) | 5 (5) | 5 (5) | 6 (6) | 10 (11) | 2 (2) |
| 6 month | |||||
| sevTBI N (%) | 5 (29) | 8 (47) | 7 (41) | 8 (47) | 2 (12) |
| modTBI N (%) | 5 (10) | 7 (14) | 6 (12) | 10 (21) | 2 (4) |
| OI N (%) | 3 (3) | 4 (4) | 5 (6) | 10 (11) | 1 (1) |
| 12 month | |||||
| sevTBI N (%) | 4 (22) | 8 (44) | 9 (50) | 6 (33) | 2 (11) |
| modTBI N (%) | 4 (8) | 5 (10) | 4 (8) | 10 (20) | 2 (4) |
| OI N (%) | 3 (4) | 3 (4) | 5 (6) | 8 (10) | 1 (1) |
| 18 month | |||||
| sevTBI N (%) | 5 (26) | 6 (32) | 6 (32) | 8 (42) | 4 (21) |
| modTBI N (%) | 4 (9) | 4 (9) | 6 (13) | 9 (20) | 1 (2) |
| OI N (%) | 4 (5) | 4 (5) | 6 (7) | 8 (10) | 0 (0) |
Figure 1.
The proportion of each group rated as consistently clinically elevated at every time point postinjury separated by parent-report measure. The proportion of sevTBI elevations differed significantly from the proportion of OI elevations on every parent-report measure. This was also true when comparing the sevTBI elevation proportions to the modTBI elevation proportions with the exception of the CBCL: ADHD subscale.
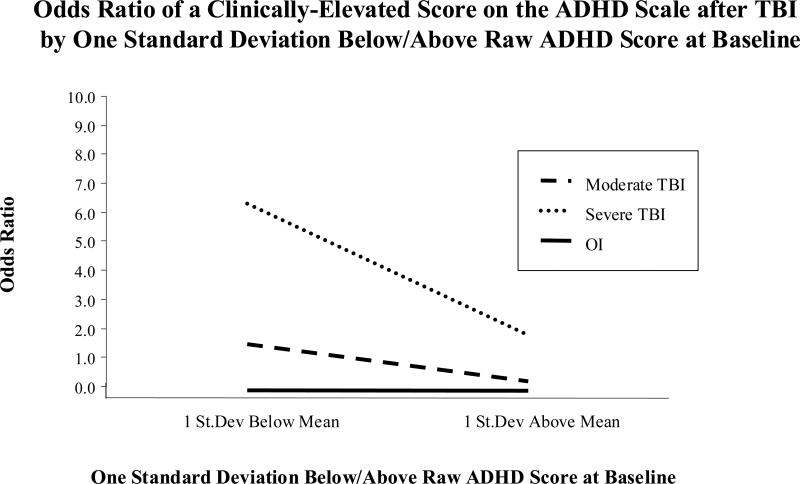
Interaction terms were added to the models to examine the influence of preinjury functioning on emerging behavior disorders. The CBCL: ADHD subscale was the only measure for which the interaction between premorbid scores and injury group was significant. The interaction suggests that children with lower premorbid CBCL: ADHD subscale scores had a higher odds ratio of being clinically elevated postinjury in the sevTBI group (odds ratio = 6.3, CI = 0.80 - 3.64; see Figure 2 for graphical representation of odds ratios and Table 4 for values of each group). In an effort to better understand the relationship between premorbid scores and injury group in relation to emerging ADHD symptoms, pre-injury CBCL: ADHD scores were entered as a continuous variable into the model. When this was done, the interaction between premorbid CBCL: ADHD score and injury group was no longer significant. Examination of scores at an individual level revealed that eight individuals in the sevTBI group had scores clustering around 50 at baseline, but became elevated at one or more time points postinjury.
Figure 2.
Trend lines of the odds ratios that individuals in each group will be clinically elevated postinjury on the CBCL: ADHD subscale as a function of their baseline score. The groups were divided into individuals who were 1 standard deviation below the mean and those who were 1 standard deviation above the mean based on their preinjury score on the ADHD subscale. Those individuals in the sevTBI group and who had a score one standard deviation below the mean were 6.3 times more likely than children in the OI group with the same preinjury scores to be elevated postinjury on the CBCL: ADHD subscale.
Table 4.
Generalized Estimation Equation Analyses with Interaction between Premorbid ADHD Score and Injury Group
| Low Baseline ADHD Score |
|||||||
|---|---|---|---|---|---|---|---|
| Estimate | Lower CI | Upper CI | Z | Odds Ratio | Elev. Postinjury | Not Elev. Postinjury | |
| Group | |||||||
| SevTBI | 1.84 | 0.80 | 3.64 | 3.06* | 6.30 | 39% | 9% |
| ModTBI | 0.37 | −0.37 | 1.90 | 1.32 | 1.45 | 29% | 33% |
| OI | 0.00 | 0.00 | 0.00 | 31% | 58% | ||
| SES | −0.72 | −1.26 | −0.17 | −2.59* | |||
| Time | |||||||
| 6 Months | 0.08 | −0.70 | 0.86 | 0.20 | |||
| 12 Months | −0.15 | −0.81 | 0.52 | −0.44 | |||
| 18 Months | 0.00 | 0.00 | 0.00 | ||||
| High Baseline ADHD Score |
|||||||
|---|---|---|---|---|---|---|---|
| Estimate | Lower CI | Upper CI | Z | Odds Ratio | Elev. Postinjury | Not Elev. Postinjury | |
| Group | |||||||
| SevTBI | 0.57 | −1.79 | 2.37 | 0.27 | 1.77 | 36% | 13% |
| ModTBI | −1.75 | −4.92 | 2.15 | −0.77 | 0.17 | 14% | 53% |
| OI | 0.00 | 0.00 | 0.00 | 50% | 33% | ||
| SES | 0.09 | −1.06 | 1.25 | 0.16 | |||
| Time | |||||||
| 6 Months | 0.19 | −1.38 | 1.77 | 0.24 | |||
| 12 Months | 0.80 | −0.58 | 2.19 | 1.14 | |||
| 18 Months | 0.00 | 0.00 | 0.00 | ||||
p<.01
To identify environmental influences on the development of clinically significant problems, mixed model logistic regression analyses were conducted with family functioning, stresses and resources, home environment, and parenting practices included as potential moderators. The resulting models showed strong evidence that increased permissive parenting, increased family dysfunction as measured by the FAD, and lower socioeconomic status all increased the probability of developing clinically significant behavior problems postinjury in the sample as a whole (see Table 5 for Bayesian analysis parameters). None of the interactions between the injury group contrasts and social environmental characteristics was significant suggesting that these variables of family dysfunction, permissive parenting, and home environment did not moderator the relationship between injury severity and emerging behavior problems.
Table 5.
Bayesian Estimates and 95% Credible Intervals for the Trimmed Model
| Mean | 2.5% | 97.5% | |
|---|---|---|---|
| SES | −1.30 | −2.39 | −0.43 |
| FAD (Family Functioning) | 1.20 | 0.24 | 2.27 |
| Permissive Parenting | 1.20 | 0.30 | 2.36 |
| modTBI | 1.80 | 0.08 | 3.92 |
| sevTBI | 2.40 | −0.42 | 5.67 |
Discussion
The purpose of this study was to document postinjury rates of clinically significant behavior problems, EF difficulties, and deficient social competence in children who sustained a TBI between the ages of 3 and 7 years of age, relative to children who sustained orthopedic injuries (OI) at the same age. Results support the hypothesis that children suffering from a severe TBI have significantly higher rates of new onset behavioral impairments when compared to children with OI comparison even up to 18 months postinjury. However, consistent with prior studies, there were no significant differences in new behavior problems between children with moderate TBI and those with OI (Fletcher, Ewing-Cobbs, Miner, Levin, & Eisenberg, 1999). Externalizing problems as measured by the CBCL ADHD and Externalizing scales were reported as being significantly elevated in children with severe TBI across the measured time points, suggesting a long-term effect of severe TBI on externalizing behavior that is consistent with previous research (Max et al., 2005; Schwartz et al., 2003; Yeates et al., 2003), as long as 30 months postinjury (Anderson, Catroppa, Dudgeon, Morse, & Rosenfeld, 2006).
A unique aspect of this study is that the children injured at a young age were found to have an increased frequency of externalizing behavior problems across the follow-up visits. In fact, a significantly higher proportion of the sevTBI group were elevated on one or more of the measures at each point postinjury compared to the modTBI or OI groups. Although the sevTBI group had increased levels of preinjury behavior problems, this group exhibited increasing rates of behavior problems over time, even after controlling for baseline/pre-injury symptom levels in the models. The clinical elevations remained stable across time in the sevTBI group, suggesting the postinjury impairments were chronic in nature and should not be treated as a transitory effect of the TBI. In contrast, the modTBI and OI groups had a significantly higher proportion of individuals who were never elevated on any measure postinjury, suggesting relatively few clinically significant changes after injury. The level of preinjury elevations in the sevTBI group is in contrast to previous studies that failed to find premorbid differences in the proportion of children with clinical elevations (Fletcher et al., 1990; Donders, 1992). The uniqueness of the current sevTBI group suggests that the findings be interpreted with caution. The possibility that increasing time between the injury and the baseline visit may have biased parents’ ratings of pre-injury functioning was tested by examining the correlations between baseline (pre-injury) scores on each self-report measure and the time between injury and the baseline visit separately for each group. All p values were greater than or equal to .44, suggesting that pre-injury ratings were not biased by the length of time between the injury and initial assessment. Although it is still possible that parents of children with severe TBI have biased recall of their child's premorbid status, it is also possible that the severe TBI group differs from the other groups with respect to premorbid characteristics and status. Families of children with TBI in this study were likely to be of lower SES and single-parent households. The quality of parental supervision and other environmental and neighborhood characteristics may have contributed to the child's injury in a way that wasn't seen in the OI group. Additionally, pre-existing behavior problems may have also increased the likelihood of sustaining a severe TBI. Because enrolled children did not differ from potential eligible children in terms of SES and race, there is reason to believe that this sample is representative. Thus, although the reasons for higher rates of pre-injury problems in children with severe TBI are unclear, the results suggest that these children are at risk for substantially elevated rates of post-injury problems, even after taking pre-morbid status into account.
The finding that lower premorbid CBCL: ADHD scores were associated with greater odds of clinically elevated postinjury scores in the sevTBI group when the outcomes were measured as dichotomous variables (clinically elevated or not) is the opposite of what was found by Max and colleagues (Max et al., 2005; (2) Max et al., 2005) although must be interpreted with caution given the small sample size that actually changed from not elevated pre-injury to clinically elevated postinjury. The non-significant group by time interactions that were found when the scores were entered as a continuous variable suggests that the association between lower premorbid ADHD scores and an increased likelihood of post-injury elevations may be in part an artifact of the small sample size and restricted range of pre-injury scores. Examination of individual scores of the sevTBI group revealed that a large portion of the children who were elevated postinjury on the CBCL: ADHD scale had a baseline score that clustered around 50 while only three had elevated scores at baseline. This restriction in range may account for the initial finding that lower premorbid CBCL: ADHD scores were more likely to result in clinically significant elevations post injury than higher premorbid scores. Therefore, it is important for these results to be replicated with a larger sample of children with severe TBI.
Consistent with previous research, EF skills as measured by the BRIEF were impaired more often in the sevTBI group than the OI group across the entire 18 months post injury. As children grow older and demands for higher cognitive functions, such as regulation of behaviors, in day to day functioning increase, the importance of executive function becomes more salient. School-age children are required to monitor their behaviors and proper emotional responses to situations to a greater extent than preschool aged children. Failure to develop executive function skills can lead to increased difficulty in social functioning and academic functioning. Whether these difficulties are a result of executive dysfunction alone or a combination of executive dysfunction and attention problems is difficult to discern, but regardless it will be important to monitor the relationship of these deficits to every day functioning as academic and social demands increase with age.
In accordance with previous research, severe TBI also had some adverse effects on social competency, although small, even at a young age (Anderson et al., 2006; Janusz et al., 2002). Notably, a significant deficit relative to ratings of pre-injury functioning appeared to become apparent only around 18 months post-injury in one child, suggesting very tentative evidence of a pattern of emerging deficits rather than recovery over time, although larger samples will be necessary to confirm this possibility. Extended longitudinal follow-up is necessary to determine whether these skills will go on to develop adequately as the child ages or whether the child will develop a pronounced deficit. Given the early age at brain injury, the extent of social problems may not be apparent until social expectations increase and the child is placed into situations that require well-developed social skills. Since social competency following traumatic brain injury has not been studied to the same extent as cognitive functioning, there is a need for increased knowledge in this area (Yeates et al., 2007). Future research should follow a cohort of children longitudinally throughout the elementary and middle school years as social demands increase to determine the long-term impact of early TBI on social development, especially given the chronic nature of clinically elevated behavior problems postinjury in the sevTBI group.
In using mixed model regression analyses to look at predictors of clinical problems, SES, family functioning, and permissive parenting style were identified as significant contributors to the likelihood of developing behavior or executive functioning problems. This is consistent with previous research that found psychosocial adversity, poorer family functioning, and maladaptive parenting styles were significant predictors of behavior and executive functioning difficulties over a prolonged period of time following TBI (Nadebaum, Anderson, & Catroppa, 2007; Taylor et al., 2001; Anderson et al., 2007). Permissive parenting styles lack consistency, clear boundaries, and structure that may result in the exacerbation of postinjury difficulties. Similarly, family dysfunction may entail a lack of structure and consistency but may also result in less than clear expectations for behavior and functioning. Inconsistent discipline, unclear expectations, and limited structure in a child's life may serve as targets for potential interventions designed to teach parents and families how to create an optimal environment to reduce the chance of developing more problems postinjury (Wade, Carey, & Wolfe, 2006; Wade, Oberjohn, Burkhardt, & Greenberg, in press).
The fact that postinjury behavior problems were much more likely to be found in children with TBI who had less than optimal environmental factors begs the question whether the problems are a result of the environment or whether the family environment deteriorates because of the behavior problems and stress of the TBI. Stancin and colleagues (2008) found that family and caregiver functioning was adversely affected following early traumatic brain injury. Chronic life stresses and interpersonal resources were important determinants of future burden and distress, as were coping strategies involving denial. Injury severity alone may not be sufficient to identify families at risk for increased burdens, and other family and personal factors probably should be assessed (Stancin, Wade, Walz, Yeates, & Taylor, 2008). Taylor and colleagues (2001) indicated that a bidirectional relationship may exist between postinjury behavior problems and poor family functioning. Another possibility is that parents of children from impoverished environments may have been unable to access the resources needed in order to intervene and stop the persistent behavior and executive functioning problems.
Future research should look at the effectiveness of interventions in curbing the behavior problems of TBI in children with early traumatic brain injuries. Promising research (Wade, Carey, & Wolfe, 2006) suggests that interventions focused on problem-solving in the family setting may lead to improved behavioral functioning in children who sustained a TBI as compared to families who did not undergo the intervention. Interventions focusing on parenting skills may also contribute to improved behavioral functioning following early TBI (Wade, Oberjohn, Burkhardt, & Greenberg, in press).
Limitations
Several limitations should be noted. Although a large percentage of the sevTBI group were reported to display problematic behaviors and executive functioning difficulties, the relatively small size of the sevTBI group limits the generalizability of the results to the population at large. Attrition reduced statistical power, potentially limiting our ability to detect differences between the moderate TBI and OI groups. Another limitation of the current study was the presence of elevated behavior and executive functioning scores for sevTBI at the baseline measurement. Although the baseline assessment took place within 3 months of the injury, we cannot know for certain whether the scores reported by parents were unbiased ratings of preinjury functioning. For example, the stress of the injury to the child or changes in the child's behavior may have influenced parental reports. To control for the effects of preinjury problems on postinjury functioning, we excluded children who been evaluated for or diagnosed with a behavior problem prior to their injury from further analyses. Additionally, all statistical analyses were conducted controlling for preinjury scores on the dependent variable of interest. Future research should more clearly identify individuals with behavior problems through careful review of school documentation and medical charts. Also, a shorter time between injury and baseline evaluation would help reduce the chance of falsely elevated baseline scores, although medical complications may prohibit an earlier evaluation.
Another limitation to the current study was the use of different test versions for different age ranges. This is a problem faced by researchers who use measures normed for subsets of child age ranges. On tests such as the PKBS and HCSBS, as well as the BRIEF and CBCL, many children were too old for preschool version of the test and were therefore administered the school-aged version. As a result, direct comparison between the scores of the different versions was limited. However, review of children whose age changed throughout testing resulting in administration of different test versions failed to reveal significant changes in clinical caseness across the groups. To address this limitation, future studies could use structured interviews to identify clinically significant symptoms. This would reduce the reliance upon parent report measures, potentially yielding additional information regarding diagnostic profiles following TBI, while enabling investigators to use the same interview across the age range.
Results of this study indicate that children who suffer from TBI at a young age show similar acute and longer-term behavioral consequences of their injuries as children who experience a TBI at an older age. This study adds to the limited literature on the effects of TBI in young children by demonstrating the prolonged trajectory of behavior and executive functioning difficulties experienced by young children and the role the environment plays in the development and maintenance of the problems. Most importantly, the results illustrate the need to follow these children as they continue in the school setting to understand the long-term effects of these behavioral, executive functioning, and social competence difficulties. As the demands required of the children increase, deficits may become more evident in social and educational settings.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/rep.
Contributor Information
Leah A. Chapman, University of Cincinnati
Shari L. Wade, Cincinnati Children's Hospital and Medical Center
Nicolay C. Walz, Cincinnati Children's Hospital and Medical Center
H. Gerry Taylor, Rainbow Babies and Children's Hospital and Case Western Reserve University.
Terry Stancin, MetroHealth Medical Center and Case Western Reserve University.
Keith O. Yeates, Nationwide Children's Hospital and the Ohio State University
References
- Achenbach TM, Rescorla LA. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2000. Manual for ASEBA Preschool Forms & Profiles. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Aged Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Anderson VA, Morse SA, Catroppa C, Haritou F, Rosenfeld JV. Thirty month outcome from early childhood head injury: A prospective analysis of neurobehavioural recovery. Brain. 2004;127(12):2608–2620. doi: 10.1093/brain/awh320. [DOI] [PubMed] [Google Scholar]
- Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20(1):42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- Arroyos-Jurado E, Paulsen JS, Merrell KW, Lindgren SD, Max JE. Traumatic brain injury in school-aged children academic and social outcome. Journal of School Psychology. 2000;38(6):571–587. [Google Scholar]
- Bayer JK, Sanson AV, Hemphill SA. Parent influences on early childhood internalizing difficulties. Journal of Applied Developmental Psychology. 2006;27(6):542–559. [Google Scholar]
- Bradley RH, Caldwell BM. The HOME Inventory and family demographics. Developmental Psychology. 1984;20(2):315–320. [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multi-model inference: A practical information-theoretic approach. Springer; New York: 2002. [Google Scholar]
- Burnham KP, Anderson DR. Multimodel inference – understanding AIC and BIC in model selection. Sociological Methods & Research. 2004;33(2):261–304. [Google Scholar]
- Byles J, Byrne C, Boyle MH, Oxford OR. Ontario child health study: Reliability and validity of the General Functioning subscale of the McMaster Family Assessment Device. Family Process. 1988;27(1):97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- Caldwell B, Bradley R. Home Observation for Measurement of the Environment. University of Arkansas at Little Rock; Little Rock: 1984. [Google Scholar]
- Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Childrens attentional skills 5-years post TBI. Journal of Pediatric Psychology. 2007;32(3):354–369. doi: 10.1093/jpepsy/jsl019. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, Dodge KA. Externalizing behavior problems and discipline revisited: Non-linear effects and variation by culture, context, and gender. Psychological Inquiry. 1997;8(3):161–175. [Google Scholar]
- Donders J. Premorbid behavioral and psychosocial adjustment of children with traumatic brain injury. Journal of Abnormal Child Psychology. 1992;20(3):233–246. doi: 10.1007/BF00916690. [DOI] [PubMed] [Google Scholar]
- Fay TB, Yeates KO, Wade SL, Drotar D, Stancin T, Taylor HG. Predicting longitudinal patterns of functional deficits in children with traumatic brain injury. Neuropsychology. 2009;23(3):271–282. doi: 10.1037/a0014936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM, Ewing-Cobbs L, Miner ME, Levin HS, Eisenberg HM. Behavioral changes after closed head injury in children. Journal of Consulting and Clinical Psychology. 1990;58(1):93–98. doi: 10.1037//0022-006x.58.1.93. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self regulation and social and behavioral functioning following childhood traumatic brain injury. Journal of the International Neuropsychological Society. 2006;12(5):609–621. doi: 10.1017/S1355617706060796. [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Rubin DB. Texts in statistical science: Bayesian data analysis. 2nd ed. Chapman & Hall/CRC; Boca Raton, FL: 2004. 2004. [Google Scholar]
- Gioia GA, Espy KA, Isquith PK. Behavior Rating Inventory of Executive Function – Preschool Version. Psychological Assessment Resources, Inc.; Lutz, FL: 2000. [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function. Psychological Assessment Resources; Odessa, FL: 2000. [Google Scholar]
- Gioia GA, Isquith PK, Retzlaff PD, Espy KA. Confirmatory factor analysis of the behavior rating inventory of executive function (BRIEF) in a clinical sample. Child Neuropsychology. 2002;8(4):249–257. doi: 10.1076/chin.8.4.249.13513. [DOI] [PubMed] [Google Scholar]
- Janusz JA, Kirkwood MW, Yeates KO, Taylor HG. Social problem-solving skills in children with traumatic brain injury: Long-term outcomes and prediction of social competence. Child Neuropsychology. 2002;8(3):179–194. doi: 10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- Landry SH, Swank P, Stuebing K, Prasad M, Ewing-Cobbs L. Social competence in young children with inflicted traumatic brain injury. Developmental Neuropsychology. 2004;26(3):707–733. doi: 10.1207/s15326942dn2603_4. [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths. National Center for Injury Prevention and Control; Atlanta: 2006. [Google Scholar]
- Max JE, Schachar RJ, Levin HS, Ewing-Cobbs L, Chapman SB, Dennis M, Saunders A, Landis J. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(10):1032–1040. doi: 10.1097/01.chi.0000173293.05817.b1. [DOI] [PubMed] [Google Scholar]
- 2.Max JE, Schacher RJ, Levin HS, Ewing-Cobbs L, Chapman SB, Dennis M, Saunders A, Landis J. Predictors of secondary attention-deficit/hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(10):1041–1049. doi: 10.1097/01.chi.0000173292.05817.f8. [DOI] [PubMed] [Google Scholar]
- Merrell K. Preschool and Kindergarten Behavior Scales. second edition. PRO-ED, Inc.; Austin: 2002. [Google Scholar]
- Miller IW, Bishop DS, Epstein NB, Keitner GI. The McMaster family assessment device: Reliability and validity. Journal of Marital and Family Therapy. 1985;11(4):345–356. [Google Scholar]
- Moos RH, Moos BS. Life Stressors and Social Resources Inventory – Adult Form manual. Psychological Assessment Resources; Odessa, FL: 1994. [Google Scholar]
- Nadebaum C, Anderson V, Catroppa C. Executive function outcomes following traumatic brain injury in young children: A five year follow-up. Developmental Neuropsychology. 2007;32(2):703–728. doi: 10.1080/87565640701376086. [DOI] [PubMed] [Google Scholar]
- Querido JG, Warner TD, Eyberg SM. Parenting styles and child behavior in African American families of preschool children. Journal of Clinical Child and Adolescent Psychology. 2002;31(2):272–277. doi: 10.1207/S15374424JCCP3102_12. [DOI] [PubMed] [Google Scholar]
- Robinson CC, Hart CH, Mandleco BL, Olsen SF, Russell A, Aloa V, et al. Psychometric support for a new measure of authoritative, authoritarian, and permissive parenting: Cross-cultural connections.. Paper presented at the Biennial Conference of the International Society for the Study of Behavioral Development; Quebec City, Quebec, Canada. 1996. [Google Scholar]
- Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: Prevalence, predictors, and correlates. Journal of Pediatric Psychology. 2003;28(4):251–263. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- Sesma HW, Slomine BS, Ding R, McCarthy ML. Executive functioning in the first year after pediatric traumatic brain injury. Pediatrics. 2008;121(6):e1686–e1695. doi: 10.1542/peds.2007-2461. [DOI] [PubMed] [Google Scholar]
- Stancin T, Wade SL, Walz NC, Yeates KO, Taylor HG. Traumatic brain injuries in early childhood: Initial impact on the family. Journal of Developmental and Behavioral Pediatrics. 2008;29(4):253–261. doi: 10.1097/DBP.0b013e31816b6b0f. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Klein SK. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999;13(1):76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. Journal of the International Neuropsychological Society. 2001;7(6):755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16(1):15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: Postacute effects on cognitive and school readiness skills. Journal of the International Neuropsychological Society. 2008;14(5):734–745. doi: 10.1017/S1355617708081150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade SL, Carey J, Wolfe CR. An online family intervention to reduce parental distress following traumatic brain injury. Journal of Consulting and Clinical Psychology. 2006;74(3):445–454. doi: 10.1037/0022-006X.74.3.445. [DOI] [PubMed] [Google Scholar]
- Wade SL, Michaud L, Brown TM. Putting the pieces together: Preliminary efficacy of a family problem-solving intervention for children with traumatic brain injury. Journal of Head Trauma Rehabilitation. 2006;21(1):57–67. doi: 10.1097/00001199-200601000-00006. [DOI] [PubMed] [Google Scholar]
- Wade SL, Oberjohn K, Burkhardt A, Greenberg I. Preliminary feasibility and efficacy of a positive parenting intervention for young children with TBI. Journal of Head Trauma Rehabilitation. doi: 10.1097/HTR.0b013e3181ad6680. in press. [DOI] [PubMed] [Google Scholar]
- Wade SL, Taylor HG, Drotar D, Stancin T, Yeates K. Childhood traumatic brain injury: Initial impact on the family. Journal of Learning Disabilities. 1996;29(6):652–666. doi: 10.1177/002221949602900609. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Armstrong K, Janusz J, Taylor HG, Wade S, Stancin T, Drotar D. Long-term attention problems in children with traumatic brain injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(6):574–584. doi: 10.1097/01.chi.0000159947.50523.64. [DOI] [PubMed] [Google Scholar]