Abstract
Acute esophageal necrosis or black esophagus is an uncommon clinical entity, diagnosed at the upper gastrointestinal endoscopy with the presence of strikingly black necrotic esophagus. Very often no definite etiology will be identified even though a large list of potential associations has been postulated. Upper gastrointestinal bleeding is the most common clinical presentation, others being epigastric pain, retrosternal chest discomfort and dysphagia. Only about a hundred cases of acute esophageal necrosis have been described in medical literature till this date. We report a case of acute esophageal necrosis in an elderly female who had presented with hematemesis.
Keywords: Acute esophageal necrosis, Acute necrotizing esophagitis, Black esophagus, Upper gastrointestinal bleed, Upper gastrointestinal endoscopy
Introduction
Acute esophageal necrosis (AEN) also referred as acute necrotizing esophagitis or black esophagus, which is a rare entity and was first described postmortem in 1967 by Brennan.1 The condition was first described using endoscopy by Goldenberg et al in 1990.2 Once thought an exceedingly rare condition is now more frequently diagnosed, perhaps due to the widespread availability and utilization of endoscopy. AEN has a reported prevalence of 0.2% and an incidence of 0.01 - 0.0125% among Caucasians undergoing esophagogastroduodenal endoscopy (EGD).3,4 At EGD endoscopy, the condition is characterized by strikingly black necrotic esophagus.3,5 We report a case of AEN and briefly review the literature about the condition.
Case Report
A 62 year old lady presented with nausea, hematemesis and retrosternal chest discomfort for a duration of 3 days. Her past medical history includes diabetes mellitus and hypertension, for which she was on insulin and losartan. No history of any other co-morbid illnesses. Also, there was no history of corrosive intake or other medications in the past. During admission, she was hemodynamically stable and physical examination was unremarkable except for pallor and minimal epigastric tenderness. Hemogram revealed anemia and polymorphonuclear cell predominant leukocytosis (hemoglobin 8.6 gm/dl, total leukocyte count 14600 cell/cmm with 81% polymorphs). Blood sugar was 286 mg/dl with normal renal function tests and serum electrolytes. Liver function tests and coagulation profile were also normal. Electrocardiogram revealed left ventricular hypertrophy with strain. Chest X-ray revealed unfolding of aortic arch with no parenchymal shadows or effusions.
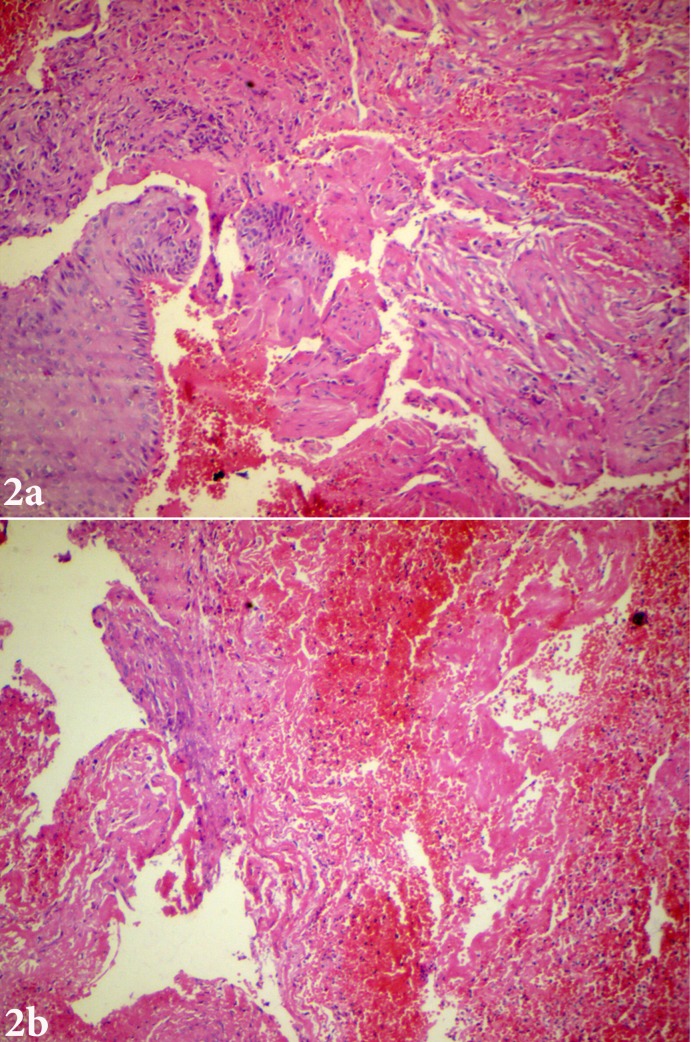
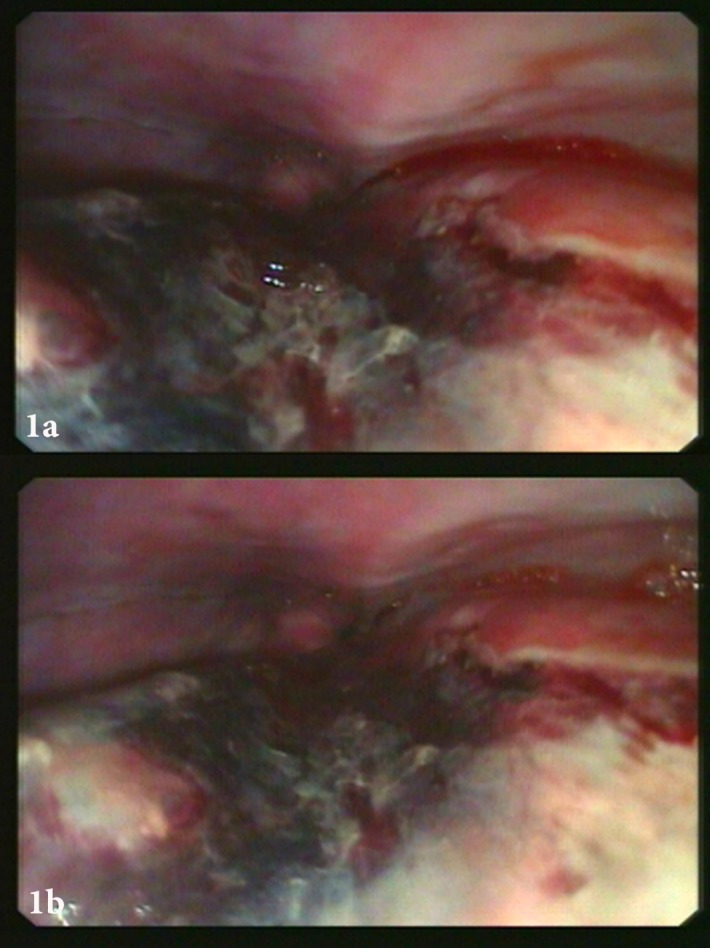
EGD revealed black distal esophagus (Figs. 1a, 1b) with a normal gastric and duodenal mucosa. Biopsies revealed necrotic tissue debris, inflammatory infiltrates and focal hemorrhages (Figs. 2a, 2b). Biopsy from the adjacent mucosa also revealed intense subepithelial inflammatory infiltration and hemorrhage. Immunostaining for cytomegalovirus and herpes viruses were negative. The patient was managed with intravenous fluids, parenteral nutrition, parenteral proton pump inhibitors, antiemetics and sucralfate. The patient improved symptomatically with the treatment. Repeat EGD after 1 month revealed normal esophageal mucosa with no residual areas of necrosis or ulceration. (Fig. 3)
Figures 1a & 1b.
EGD images showing black necrotic distal esophagus.
Figures 2a & 2b.
EGD biopsy from necrotic zone; Eosin & Hematoxylin staining (100 ×) showing extensive areas of tissue necrosis, focal areas of hemorrhage and inflammatory infiltration. Fragments of apparently normal appearing epithelium also seen.
Figure 3.

EGD images showing mucosal healing.
Discussion
AEN often described as black esophagus is a rare clinical entity that most often described in elderly. A review of reported cases by Day A et al. showed that the condition predominantly affects men (male to female ratio of 4:1) with a mean age presentation of 68.44 years.3 Vast majority of patients present with upper gastrointestinal bleeding (65%), while other manifestations includes; retrosternal discomfort, epigastric pain and dysphagia.3 The precise etiology of this condition still remains unclear, but probably multifactorial. The most widely postulated mechanism is mucosal ischemia.2,3,6 Day A et al. review had demonstrated co-morbidities in most of the affected individuals and the most common co-morbidity identified was hypotension.3 Esophagus has diverse blood supply, upper esophagus supplied by branches of inferior thyroid artery, mid esophagus by vascular twigs from aorta and intercostals. In distal esophagus, the least vascular segment derives its arterial supply from the esophageal branches of left gastric artery. Having the least blood supply, the distal esophagus is more susceptible to ischemic injury and in majority of cases of AEN and the necrotic changes is most prominent in this region. Published literature on AEN till date shows an extremely high predilection to involve the distal esophagus.3,7 The condition is often associated with a wide variety of risk factors like diabetes mellitus, infections, medications, vascular diseases, hypotension, malnutrition and advanced malignancies.3,6,7 The hallmark endoscopic feature is the presence of circumferentially black esophagus with an abrupt transition to normal mucosa at gastroesophageal junction and a normal gastric mucosa.5
The diagnostic criteria for AEN by Moreta et al.4 includes the following; (a) circumferential black esophagus with or without exudates, (b) distal esophageal involvement, ending sharply at the gastroesophageal junction and (c) absence of caustic ingestion. Histology reveals necrosis of mucosa with occasional extension to submucosa, and muscularis propria with intense inflammatory infiltration.3-5 Vascular thrombosis may also be demonstrable histologically.3,4 Differential diagnosis includes other causes of black colored esophagus with melanosis, pseudomelanosis, malignant melanoma and acanthosis nigricans.3,6 Treatment is often non-specific and includes fluid resuscitation, short term parenteral nutrition, gastric acid suppression (often with proton pump inhibitors) and sucralfate suspension.3,6-9 Complete mucosal healing and an uneventful recovery is the general rule, but can rarely be complicated with esophageal perforation, mediastinitis and esophageal stricture.6,8 Death due to esophageal necrosis occurs fewer than 6% of the cases.9 Mortality is more often due to the concurrent comorbidities, which is as high as 32%.9
Our patient as described classically was an elderly lady with comorbid illnesses who had presented with upper gastrointestinal bleed and consistent with AEN on endoscopy and histology. As with most other cases reported in medical literature, the exact etiology of AEN remains obscure as well as in this case. The patient had no history of any antecedent medications excluding insulin and losartan nor had any corrosive ingestion. Other potential causes of black esophagus were ruled out histologically. The response to treatment and disappearance of lesions on subsequent endoscopy also supports the diagnosis of AEN in this case.
Conclusion
AEN is a serious but uncommon condition and is to be included in the list of differentials in an elderly patient with multiple comorbid illnesses presenting with upper gastrointestinal bleed. Early diagnosis with endoscopy and prompt treatment can improve the outcome in patients with AEN.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
- 1.Brennan JL. Case of extensive necrosis of the oesophageal mucosa following hypothermia. J Clin Pathol 1967. Jul;20(4):581-584 10.1136/jcp.20.4.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology 1990. Feb;98(2):493-496 [DOI] [PubMed] [Google Scholar]
- 3.Day A, Sayegh M. Acute oesophageal necrosis: a case report and review of the literature. Int J Surg 2010;8(1):6-14 10.1016/j.ijsu.2009.09.014 [DOI] [PubMed] [Google Scholar]
- 4.Moretó M, Ojembarrena E, Zaballa M, Tánago JG, Ibánez S. Idiopathic acute esophageal necrosis: not necessarily a terminal event. Endoscopy 1993. Oct;25(8):534-538 10.1055/s-2007-1009121 [DOI] [PubMed] [Google Scholar]
- 5.Burtally A, Gregoire P. Acute esophageal necrosis and low-flow state. Can J Gastroenterol 2007. Apr;21(4):245-247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katsinelos P, Pilpilidis I, Tsolkas P, Galanis I, Katsiba D, Arvaniti M, et al. Acute Esophageal Necrosis: Is it a so Uncommon Endoscopic Finding? Ann Gastroenterol. 2004;17:313-316 [Google Scholar]
- 7.Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007. Jan;42(1):29-38 10.1007/s00535-006-1974-z [DOI] [PubMed] [Google Scholar]
- 8.Augusto F, Fernandes V, Cremers MI, Oliveira AP, Lobato C, Alves AL, et al. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy 2004. May;36(5):411-415 10.1055/s-2004-814318 [DOI] [PubMed] [Google Scholar]
- 9.Lacy BE, Toor A, Bensen SP, Rothstein RI, Maheshwari Y. Acute esophageal necrosis: report of two cases and a review of the literature. Gastrointest Endosc 1999. Apr;49(4 Pt 1):527-532 10.1016/S0016-5107(99)70058-1 [DOI] [PubMed] [Google Scholar]