Abstract
Context:
The modern living life-style is known to produce various physical and psychological stresses resulting in increased blood pressure (BP) and heart rate (HR). This can lead to increased myocardial oxygen demand (MVO2). MVO2 correlated best with rate pressure product (RPP). RPP is a product of HR and systolic BP.
Objective:
The present study was conducted to evaluate the effect of relaxation in the form of pranayama on RPP in mild hypertensives.
Materials and Methods:
Mild hypertensive patients were divided into two groups. Group A received antihypertensive drugs for 6 weeks and Group B received antihypertensive drugs along with pranayama training for 6 weeks.
Results:
BP decreased significantly in Group B (148 ± 8.09-127 ± 12.10 mm of Hg) where pranayama was added. The decrease was significant as compared to Group A. HR decreased significantly in both the groups as compared to baseline, however the decrease was similar in both groups. RPP decreased significantly in both groups as compared to baseline, however the decrease was significantly more (P < 0.01) when pranayama was added to antihypertensive drugs (96.73 ± 20.53) when compared to antihypertensive drugs alone (114.66 ± 26.30).
Conclusion:
The pranayama produces relaxed state and in this state parasympathetic activity overrides sympathetic activity. Hence, addition of pranayama can be a useful addition to antihypertensive drugs for better control of hypertension in mild hypertensives.
Keywords: Myocardial oxygen demand, pranayama, rate pressure product, stress
INTRODUCTION
Hypertension is the most important modifiable risk factor for coronary heart disease, stroke, congestive heart failure, end-stage renal disease and peripheral vascular disease.[1] It accounts for a major part of morbidity and mortality due to cardiovascular diseases (CVD).[2] As per World Health Organization (WHO), CVD will be the largest cause of death and disability in India by 2020 and nearly half of this mortality will be in young and middle-aged individuals. Currently, Indians experience CVD deaths at least a decade earlier than their counterparts in countries with well-established market economies.[3] Out of so many risk factors for essential hypertension, stress is one of modifiable risk factors as recently reviewed by WHO scientific group. Chronic psychological stress and negative affective states contribute significantly to the pathogenesis and progression of hypertension.[4] Since stress is nowhere defined, the hypothesis is untestable. However, it is an accepted fact that psychosocial factors operate through mental processes, consciously or unconsciously, to produce hypertension. Virtually all studies on blood pressure (BP) and catecholamine levels revealed significantly higher noradrenaline levels in hypertensives than normotensives. This supports the contention that over activity of sympathetic nervous system has an important part to play in the pathogenesis of hypertension.[1] Psychosocial stress has also been shown to induce endothelial dysfunction and atherosclerosis. Scientists have tried to study the pathophysiological mechanisms induced by stress in experimental models and laboratory induced stress in volunteers.[5,6] These studies have demonstrated increased heart rate (HR) and BP and thus an increase in oxygen demand.[7]
These hypertensive patients also display acute peaks in BP as per circadian rhythm. These peaks are associated with work stress and psychobehavioral responses to stress such as anger, anxiety, tension and nervousness.[8] Numerous approaches are available for stress management that can decrease these patient's suffering and enhance their quality of life.[9] Relaxation methodologies in the form of yoga (asanas, pranayama, transcendental meditation and progressive muscular relaxation) has become more popular recently, though these techniques have been practiced in the past. Yoga is an ancient system of relaxation, exercise and healing with origins in India. Pranayama, the formal practice of controlling the breath, lies at the heart of yoga. The Sanskrit word pranayama consists of two parts: Prana and ayama. Ayama means “stretch” or “extend” and describes the action of pranayama.[10] Pranayama breathing has shown to alter autonomic activity as it increases parasympathetic activity.[11] If hypertensive patients could adopt a simple relaxation technique that would reduce stress and its physiological effects, they may be able to control their BP better, decrease the requirements for antihypertensive drugs and respond better during such physiologically stressful events. Studies have shown a decrease in BP with pranayama.[11] However, in hypertensive patients, myocardial oxygen demand (MVO2) can be a better marker of predicting CVD. Rate pressure product (RPP) is an index of MVO2. RPP is calculated as product of systolic BP and HR.[12] The studies have shown different effects of relaxation therapies on BP in different populations.[13] Hence, this study was designed to evaluate the effect of pranayama on RPP in mild hypertensive patients.
MATERIALS AND METHODS
The present study was carried out on both males and females of age group 20-50 years having mild hypertension. Patient diagnosed with mild hypertension (stage I) according to criteria developed by European Society of hypertension were enrolled.[14] Patients with secondary hypertension or with previous experience of yoga or history of major cardiac/renal/pulmonary disease or history of any surgery in the recent past or history of major medical illness in the past such as tuberculosis, diabetes mellitus, bronchial asthma were excluded. Subjects were divided in two groups. Group A (n = 25) was a control group and received antihypertensive drugs for 6 weeks. Group B (n = 25) was study group which received pranayama along with antihypertensive drugs for 6 weeks. The study was approved by Institute Ethics Committee and written informed consent was obtained from all patients.
Training schedule of pranayama
The philosophy of Yoga is sometimes pictured as a tree with eight branches: Pranayama (breathing exercises), Asana (physical postures), Yama (moral behavior), Niyama (healthy habits), Dharana (concentration), Prathyahara (sense withdrawal), Dhyana (contemplation) and Samadhi (higher concoiusness).[15] Pranayama is a method of relaxation, which involves minimal training, can be learnt quickly and more importantly can be applied immediately to everyday situations. There are hundred different styles of pranayama from beginners to advanced. The following pranayama are easy and safe. The techniques of the following pranayama were taught to the patients of Group B and practiced regularly for 6 weeks. All of them were given written instructions.
Pranayamas taught were:
Nadi-shodhana pranayama: Patient was instructed to use right thumb for right nostril and right third finger for left nostril. He was told to close the right nostril and inhale deeply through left nostril to the count of 4. Then he was told to block both nostrils and hold the breath for 2 counts. This was followed by blocking of the left nostril and exhalation through the right nostril to the count of 4. This act was repeated with the other nostril also. The time duration was at least 2 min at first, progressively increasing the duration up to 10 min[16]
Chandar Bhedi pranayama: The patient was asked to close the right nostril, inhale through the left nostril. Then he was told to close the left nostril and exhale through the right nostril without any pause. Time duration was at least for 2 min at first, progressively increasing the duration up to 10 min[17]
Bhramari pranayama: The patient was asked to close eyes with four fingers over each eye and thumbs blocking the ears. Then he was told to inhale deeply through both nostrils and with the mouth closed exhale through both the nostrils producing a continuous humming sound until the exhalation has exhausted. This was repeated for 10 cycles[16]
Omkar chanting: The patient was asked to inhale deeply with both nostrils followed by a loud chanting of sound of omkar from the mouth during exhalation in the ratio of a: o; ma as 1:4;2. This was repeated for 10 cycles.[18]
The following parameters were recorded at baseline and after 6 weeks of interventions in both control and study group. These were explained to the subject in simple terms.
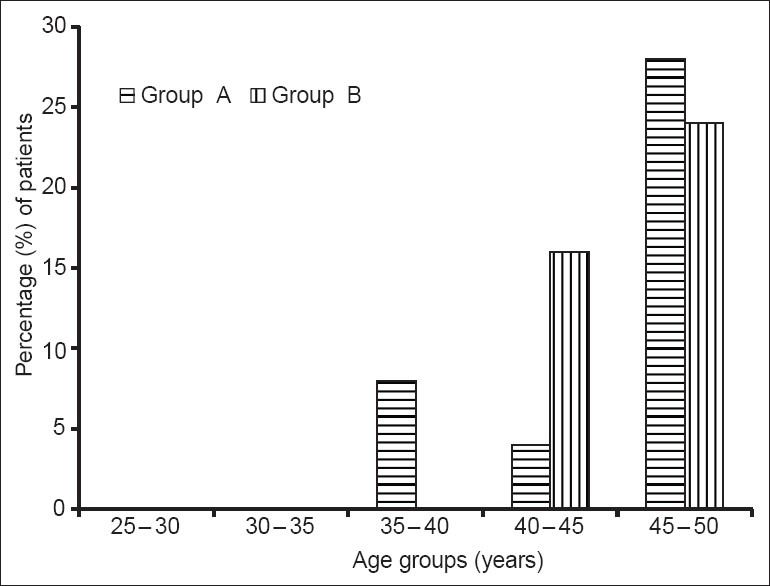
HR: Subject was made to lie down while continuous electrocardiographic (ECG) on cardiofax machine (limb lead-II) was recorded. The R-R interval was measured on ECG with a ruler, HR was calculated[19] as:
BP recording was done by standard sphygmomanometer.
RPP was calculated as:
RPP = HR × SBP × 10-2mmHg
SBP: Systolic BP in mmHg
HR: Heart rate in beats per minutes
The value thus obtained was expressed as mmHg beats per min.[12] RPP is an easily measurable index of MVO2 and load on heart. This hemodynamic parameter has been shown to follow a circadian pattern similar to that observed with cardiovascular events.[20]
Statistical analysis
Data were analyzed using unpaired t-test for comparison of RPP between control and study group. The paired t-test was used for comparison among the same group between pre-treatment and post-treatment values.
RESULTS
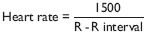
The demographic characteristics were comparable in both groups [Table 1]. Males were more in both groups (60% in Group A and 64% in Group B). Most of the patients were in the age group of 35-50 years [Figure 1]. There were only 8% patients in Group A in the age group of 30-35 years and none in Group B. As can be seen in Table 2 and Figure 2, HR decreased significantly in both groups. This decrease was not significantly different between groups. Although there was a decrease in BP in both groups when compared to baseline, the decrease was not statistically significant in Group A. The decrease was statistically significant in Group B when compared to baseline (P < 0.001). The decrease was significantly more in Group B as compared to Group A (P < 0.001).
Table 1.
Demographic characteristics of subjects in both groups
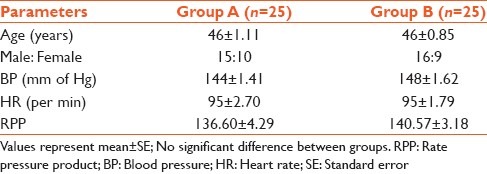
Figure 1.
Age wise distribution of subjects in both groups
Table 2.
Cardiovascular parameters in both groups (mean±SE)
Figure 2.
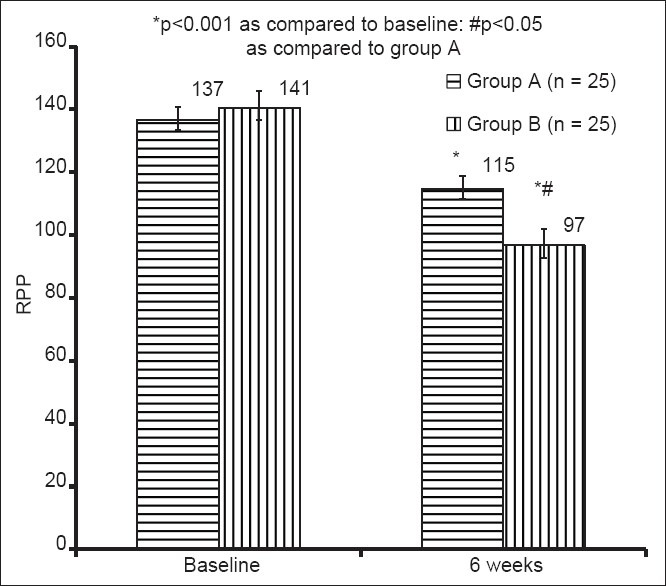
Comparison of changes in rate pressure product at baseline and 6 weeks post-intervention. RPP: Rate pressure product
RPP which is a product of BP and HR decreased significantly in both groups (P < 0.001). The decrease was significantly more in Group B where pranayama was added to antihypertensive therapy.
DISCUSSION
Among the various approaches to reduce the level of anxiety, pranayama is one that combines the physical elements of a healthy life-style with prescriptions for abiding mental piece. Further, the growth of psychoneuroimmunology has strengthened the scientific foundations of mind-body technique. As tools for influencing the mind positively have assumed extensive application in a wide variety of illness, it is important to examine their efficacy.
In the present study, we measured effect of pranayama on RPP in mild hypertensives. RPP is a reliable index of myocardial oxygen consumption and cardiac work and it correlates well with the oxygen consumption of normal subjects as well as patients with angina pectoris.[21]
In the present study, demographic were comparable in both groups and cardiac parameters measured (BP, HR, RPP) were also similar in both groups at baseline. The proportion of male patients was more in both groups. This is expected as hypertension affects male gender more in the age groups we compared.[22] Most of the patients were in the age group of 35-50 years and this is in accordance with changing trends where hypertension is affecting more younger people especially due to life-style pressures and high demanding professions. Earlier studies also reported more incidence of hypertension in younger individuals.[23]
BP decreased in both groups when compared to baseline levels, however the decrease was significant in the Group B where pranayama was added to regular antihypertensive therapy. The decrease was more in Group B as compared to Group A given only antihypertensive drugs. This indicates that pranayama has led to more decrease in BP. One of the earlier study reported that treatment by anti-hypertensive drugs produce the greatest lowering of BP.[19] Treatment by weight reduction, yoga and muscle relaxation each produced smaller, but appreciable, changes in BP and salt reductions were inferior to those of other regimens and were not significantly different to the effect of placebo treatment.[24] Similarly HR decreased significantly in both groups, however this decrease was comparable in both groups indicating that antihypertensive drugs alone and along with pranayama decreased HR to a similar extent. Earlier studies have shown that pranayama can lead to decrease in BP and HR.[13]
The isolated changes in BP and HR sometimes may not convey the overall effect of pranayama on the disease process. Hence, RPP which is a product of systolic BP and HR and is a better index of MVO2 and is very useful parameter.[21] RPP is especially important in patient care as this is an indirect indicator of myocardial oxygen consumption and load on the heart, thereby signifying a lowering of strain on the heart. The RPP also provides a simple measure of overall HR variability (HRV) in hypertensive patients and is a surrogate marker in situations where HRV analysis is not available.[25,26] Hence, the reduction in RPP in our study implies better autonomic regulation of the heart in hypertensive patients. A previous study from our laboratories reported that pranayama training of 3 months duration modulates ventricular performance by increasing parasympathetic activity and simultaneously decreasing sympathetic activity.[27] This may explain significant decreases in HR and BP observed in the present study with pronounced effects on the heart.
In the present study, RPP decreased significantly in both the groups indicating that antihypertensive drugs alone as well as along with pranayama decreased RPP. This is in accordance with the earlier study showing that antihypertensive drugs were effective in controlling the variables of hypertension.[28] The decrease in RPP in both groups, indicates the fact that antihypertensive drugs alone as well as along with pranayama decrease MVO2, which decreases the load on heart and hence cardiovascular morbidity and mortality. The decrease in RPP was more in group which practiced pranayama for 6 weeks along with antiyhypertensive drugs. These finding indicate that pranayama adds on to antihypertensive action of drugs and more decrease in RPP than antihypertensive drugs alone.
The significant reduction in RPP indicates a decrease in myocardial oxygen consumption and load on heart. This can be explained on the basis of decrease in sympathetic drive to the heart. A practitioner of pranayama not only tries to breath, but at the same time, also tries to keep his/her attention on the act of breathing, leading to concentration. These acts of concentration remove his attention from worldly worries and de-stress him/her. Stress free individual adapts better to the daily emotional, physical and mental stress. This stress free state of mind evokes relaxed responses. In this relaxed state, there is dominance of parasympathetic nerve activity. Our findings are in consistent with an earlier study which reported that yogic training produces a significant decrease in BP associated with improvement of baroreflex sensitivity and attenuation of sympathetic and rennin-angiotensin activity.[29] This was also in accordance with the results of earlier studies where they observed a significant reduction in resting HR after 2 weeks of yogasanas and pranayama training.[30] Systolic BP, diastolic BP and mean pressure showed a significant reduction at 3 weeks of the training period. Whereas in another study, pranayama training produced a decrease in basal HR but systolic, diastolic BP did not change in either pranayama group or control group though there was a significant reduction in RPP in pranayama group.[27]
Hence, the results of the present study conclude that pranayama leads to better control of BP in mild hypertensive patients. The further studies are needed to explore the effects of these techniques in various stages of hypertension.
Footnotes
Source of Support: Nill.
Conflict of Interest: None declared.
REFERENCES
- 1.Park K. Textbook of Preventive and Social Medicine. 19th ed. Jabalpur: Banarsidas Bhanot; 2007. Epidemiology of communicable diseases; pp. 310–3. [Google Scholar]
- 2.Schoen FJ. Blood vessels. In: Kumar V, Abbas AK, Fausto N, editors. Robbins and Cotran Pathologic Basis of Disease. India: WB Saunders Company; 2005. pp. 525–6. [Google Scholar]
- 3.Global Burden of Disease: 2004 Update. Geneva: WHO; [Last accessed on 2013 Jun 30]. Who's certified. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf . [Google Scholar]
- 4.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: A systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 5.Naomi G. Hypertensive vascular disease. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison's Principles of Internal Medicine. 16th ed. USA: McGraw Hill; 2005. pp. 1463–8. [Google Scholar]
- 6.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 7.Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992;267:520–4. [PubMed] [Google Scholar]
- 8.Smolensky MH, Hermida RC, Castriotta RJ, Portaluppi F. Role of sleep-wake cycle on blood pressure circadian rhythms and hypertension. Sleep Med. 2007;8:668–80. doi: 10.1016/j.sleep.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Fokkema DS. The psychobiology of strained breathing and its cardiovascular implications: A functional system review. Psychophysiology. 1999;36:164–75. [PubMed] [Google Scholar]
- 10.Pranayama. Wikipedia. [Last accessed on 2013 Jun 30]. Available from: http://www.en.wikipedia.org/wiki/Pranayama .
- 11.Bhavanani AB, Madanmohan, Sanjay Z. Immediate effect of chandra nadi pranayama (left unilateral forced nostril breathing) on cardiovascular parameters in hypertensive patients. Int J Yoga. 2012;5:108–11. doi: 10.4103/0973-6131.98221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madanmohan, Udupa K, Bhavanani AB, Vijayalakshmi P, Surendiran A. Effect of slow and fast pranayams on reaction time and cardiorespiratory variables. Indian J Physiol Pharmacol. 2005;49:313–8. [PubMed] [Google Scholar]
- 13.Bhavanani AB, Sanjay Z, Madanmohan Immediate effect of sukha pranayama on cardiovascular variables in patients of hypertension. Int J Yoga Therap. 2011;21:73–6. [PubMed] [Google Scholar]
- 14.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 15.Umm.edu. Yoga: Overview University of Maryland Medical Centre; [Last cited on 2011 Jan 1]. Available from: http://www.umm.edu/altmed/articles/yoga-000364htm . [Google Scholar]
- 16.Subbalakshmi NK, Saxena SK, Urmimala, D’Souza UJA. Immediate effect of ‘nadi-shodhana pranayama’ on some selected parameters of cardiovascular, pulmonary and higher functions of brain. J Physiol Sci. 2005;18:10–6. [Google Scholar]
- 17.Pal GK, Velkumary S, Madanmohan Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- 18.Sivanand S. P.O. Shivanandanagar, District Tehri-Garhwal. 4th ed. Uttar Pradesh: A Divine Life Society Publication; 1998. The Science of Pranayama. [Google Scholar]
- 19.Luthra A. ECG Made Easy. 4th ed. New Delhi: Jaypee Publishers; 2012. [Google Scholar]
- 20.Gobel FL, Norstrom LA, Nelson RR, Jorgensen CR, Wang Y. The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation. 1978;57:549–56. doi: 10.1161/01.cir.57.3.549. [DOI] [PubMed] [Google Scholar]
- 21.Murugesan R, Govindarajulu N, Bera TK. Effect of selected yogic practices on the management of hypertension. Indian J Physiol Pharmacol. 2000;44:207–10. [PubMed] [Google Scholar]
- 22.Tom F, Knut S. High blood pressure. In: Jones R, Britten N, Culpepper L, Gass D, Grol R, Mant D, editors. Oxford textbook of Primary Medical Care. Vol. 2. Oxford: Oxford University Press; 2004. pp. 653–58. [Google Scholar]
- 23.National Institute of Health Medline Plus [Internet]More young adults at risk of high blood pressure. [Cited 14 May 2013];NIH Medline Plus. 2011 6:10–1. Available from: http://www.nlm.nih.gov/medlineplus/magazine/issues/fall11/articles/fall11pg10-11.html . [Google Scholar]
- 24.Andrews G, MacMahon SW, Austin A, Byrne DG. Hypertension: Comparison of drug and non-drug treatments. Br Med J (Clin Res Ed) 1982;284:1523–6. doi: 10.1136/bmj.284.6328.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Madanmohan, Udupa K, Bhavanani AB, Shatapathy CC, Sahai A. Modulation of cardiovascular response to exercise by yoga training. Indian J Physiol Pharmacol. 2004;48:461–5. [PubMed] [Google Scholar]
- 26.Prakash ES, Madanmohan, Sethuraman KR, Narayan SK. Cardiovascular autonomic regulation in subjects with normal blood pressure, high-normal blood pressure and recent-onset hypertension. Clin Exp Pharmacol Physiol. 2005;32:488–94. doi: 10.1111/j.1440-1681.2005.04218.x. [DOI] [PubMed] [Google Scholar]
- 27.Udupa K, Madanmohan, Bhavanani AB, Vijayalakshmi P, Krishnamurthy N. Effect of pranayam training on cardiac function in normal young volunteers. Indian J Physiol Pharmacol. 2003;47:27–33. [PubMed] [Google Scholar]
- 28.Vijayalakshmi P, Madanmohan, Bhavanani AB, Patil A, Babu K. Modulation of stress induced by isometric handgrip test in hypertensive patients following yogic relaxation training. Indian J Physiol Pharmacol. 2004;48:59–64. [PubMed] [Google Scholar]
- 29.Selvamurthy W, Sridharan K, Ray US, Tiwary RS, Hegde KS, Radhakrishan U, et al. A new physiological approach to control essential hypertension. Indian J Physiol Pharmacol. 1998;42:205–13. [PubMed] [Google Scholar]
- 30.Konar D, Latha R, Bhuvaneswaran JS. Cardiovascular responses to head-down-body-up postural exercise (Sarvangasana) Indian J Physiol Pharmacol. 2000;44:392–400. [PubMed] [Google Scholar]


