Abstract
Objectives:
The primary objective of the following study is to determine the demographic patterns of women presenting as sterilization-failure and secondary is to evaluate possible etiological factors for failure and lay standard guidelines to reduce failure rate.
Materials and Methods:
The present study is retrospective study conducted in Department of Obstetrics and Gynecology, Government Medical College and Hospital-based on the case records maintained in our institution over a decade (April 2002-March 2012).
Results:
Over a decade, 140 cases of sterilization-failure with longest interval of 20 years have been documented out of 80 (57.14%) cases were of minilaparotomy (minilap), 53 (37.86%) laparoscopic tubal ligation and 5 (3.57%) were lower segment cesarean section. In 84 cases (60%) sterilization were performed in Primary Health Centre (PHC). Only 58 (41.43%) patients reported failure in 1st trimester (<12 weeks). 14 cases (10%) were of ectopic pregnancy. There were 25 cases (17.86%) of spontaneous recanalization. In 27 cases (19.29%) failure was due to improper surgical procedure and rest 54 (38.57%) have conceived due to tuboperitoneal fistula.
Conclusion:
Female sterilization even though considered as permanent method of contraception, recanalization is possible even 20 years after procedure. Maximum cases of failure were with minilap and those were performed at PHC. The most common cause of failure was tuboperitoneal fistula. Ectopic pregnancies were seen in 10% of cases. Proper counseling of patient is must. There is a need to stick to standards of sterilization procedure to prevent future failure.
Keywords: Laparoscopic tubal ligation, minilaparotomy, spontaneous tubal recanalization, sterilization-failure, tubal ligation, tubal sterilization
INTRODUCTION
Female sterilization or tubal ligation is the most accepted method of contraception in India. Almost 5-6 million sterilization procedures are performed annually contributing to 98% of all sterilizations and roughly 62% of all contraceptive use. The most popular method used in female sterilization in India is the laparoscopic tubal occlusion. Over 85.3% of all persons who have adopted this method of contraception availed this service from government facilities. Although, tubal sterilization is considered a permanent method of fertility control, pregnancy can occur in 1 in 200, according to international sources. In the 1st year after tubal sterilization, the estimated failure rate is 0.1-0.8% respectively. In our study, we have tried to evaluate the etiological factors for sterilization-failure and also to discuss preventive measures to avoid unwanted pregnancies and maternal morbidities as a result of sterilization-failure specifically in developing countries like India where sterilization-failure is a genuine medical issue.
MATERIALS AND METHODS
This study is a retrospective study which includes all women who have reported or referred as tubal sterilization-failure to Department of Obstetrics and Gynecology, Government Medical College and Hospital at our institute during the period of 10 years from April 2002 to March 2012. Luteal phase pregnancies are not included as sterilization-failure in our study. Information has been collected from case records of these patients maintained in the institution after approval by ethics committee. Informed consent form was not needed as identity of patient has not been revealed anywhere. Important aspects of case history includes age, obstetric score, type of sterilization, place of sterilization, sterilization-failure interval, gestational age at the time of diagnosis, decision of couple regarding further management of present pregnancy and re-sterilization. Pregnancy was further managed depending on couple's decision, gestational age, obstetric history and maternal condition. Those patients who were not ready or fit for re-sterilization were discharged. During the re-sterilization, previous sterilization procedure was assessed for correct performance, recanalization, intactness and other associated findings. Re-sterilization was performed depending on their intra-operative findings.
RESULTS
During the selected period, April 2002-March 2012 (10 years) 140 women have reported to the institution as tubal sterilization-failure making an average of 14 cases/year. Year-wise distribution is projected in Figure 1.
Figure 1.
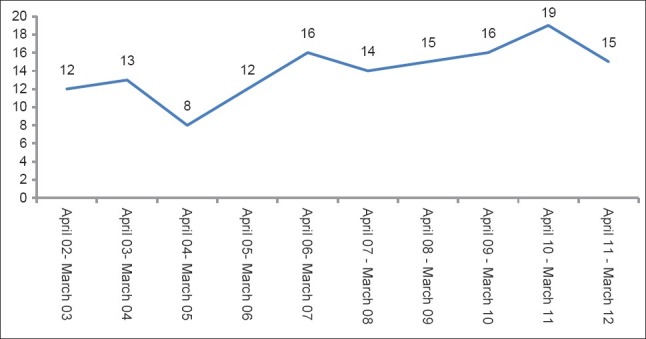
Year-wise distribution of cases
Women of age group 25-29 years (49%) constituted the largest group [Figure 2]. The eldest patient documented was of 42 years. In parity comparison, 50% of women were para 2 [Figure 3]. We have also reported a patient with parity 6 who had conceived thrice after sterilization. When we compared type of surgery [Figure 4], minilaparotomy (minilap) failure constituted 59% followed by laparoscopic tubal ligation (Lap TL) - 38% and lower segment cesarean section (LSCS) - 3%. Sterilization-failure interval [Figure 5] was <1 year in 22 (15.71%) cases, 1-5 years in 80 patients (57.14%), 6-10 years in 30 (21.43%) and >10 years in eight patients (5.71%). The longest documented sterilization-failure interval was 20 years in our study presented with ruptured ectopic.
Figure 2.
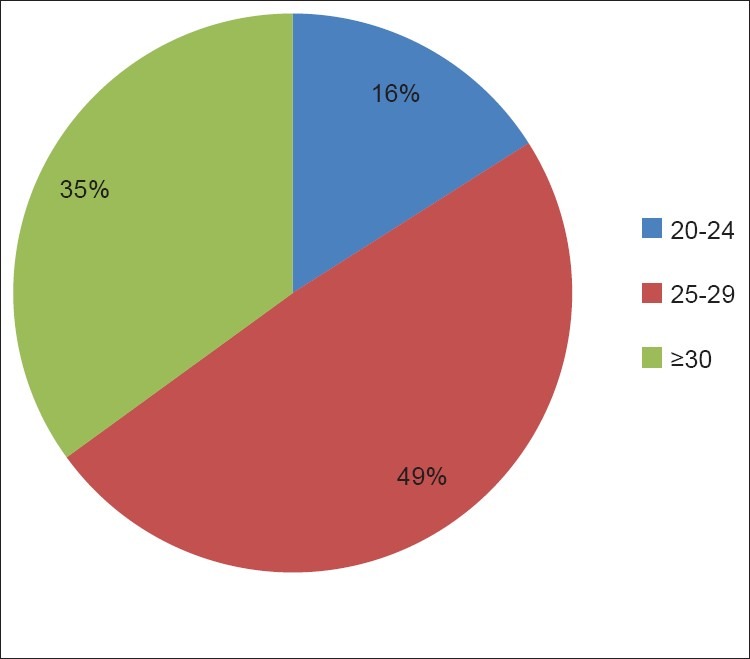
Age wise distribution of cases
Figure 3.
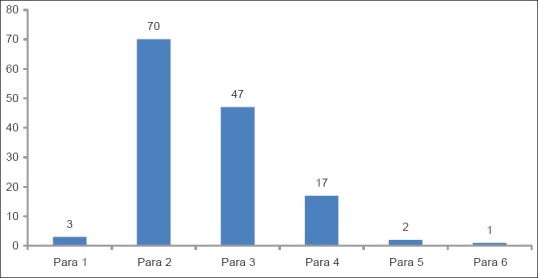
Obstetric score
Figure 4.
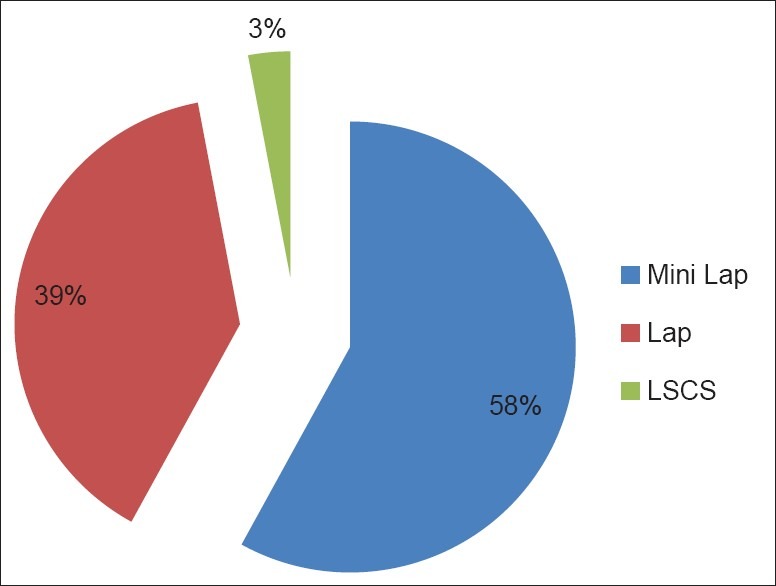
Type of surgery
Figure 5.
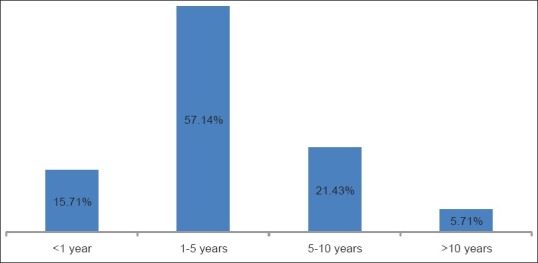
Sterilization-failure interval
In whom sterilization-failure interval was <1 year, initial non-occlusion due to improper procedure was responsible for failure in 12 cases (54.55%). There was recanalization and an ectopic 1 each (4.55%). Failure occurred due to tuboperitoneal fistula in five patients (22.72%) and three patients couldn’t be evaluated as either unfit or not ready for re-sterilization. Interval of 1-5 years was in 80 patients (57.14%) with recanalization in 14 cases (17.5%), improper procedure in 11 (13.75%), ectopic in 6 (7.5%) and failure due to tuboperitoneal fistula in 38 (47.5%). Evaluation was not possible in 11 cases as either there were not ready or unfit for re-sterilization.
When we compared patients in sterilization-failure interval 6-10 years, out of 30, recanalization was seen in 8 cases (26.67%), tuboperitoneal fistula in 10 (33.33%), ectopic and improper procedure in 4 each (13.33%). Those patients in which sterilization-failure interval was >10 years, ectopic was found in 3 cases (37.5%), recanalization in 2 (25%), tuboperitoneal fistula in 1 (12.5%) and 2 cases (25%) couldn’t be evaluated.
When place of previous sterilization was compared [Figure 6], 84 cases (60%) were from Primary Health Center (PHC) followed by tertiary center 19 (13.57%), rural hospital 16 (11.43%), private hospital 15 (10.71%) and camp 6 (4.29%) in descending order.
Figure 6.
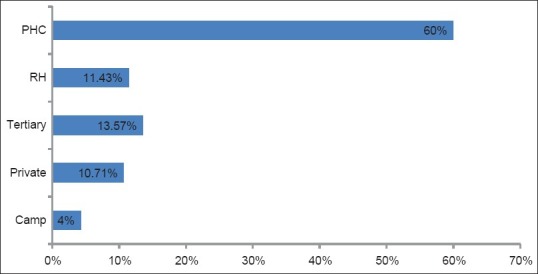
Place of surgery
Only 58 patients (41.43%) reported failure in 1st trimester, out of 44 (31.43%) underwent 1st trimester medical termination of pregnancy (MTP), rest 14 (10%) underwent laparotomy for an ectopic pregnancy. There were 48 patients with gestational age of 12-20 weeks (34.29%), 41 (29.29%) had 2nd trimester MTP and 7 (5%) needed hysterotomy due to obstetric conditions. In rest 34 patients where pregnancy was >20 weeks (24.29%), 22 delivered vaginally at term (15.71%), 4 were preterm deliveries (2.86%) and 8 required LSCS (5.71%) as demonstrated in Figure 7.
Figure 7.
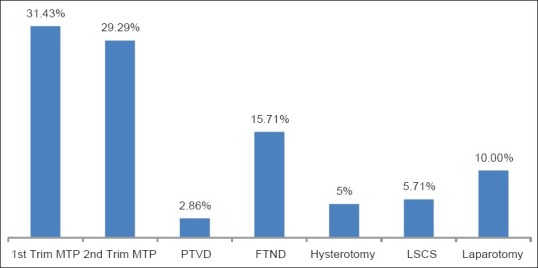
Final management
To summarize, recanalization was seen in 25 cases (17.86%) along with 14 cases (10%) of ectopic pregnancies. Recanalization was documented on the right side in 19, on the left side in 12 and both sides in eight patients. Improper procedure was noted in 27 (19.29%) and in 54 (38.57%) failure occurred due to tuboperitoneal fistula. Evaluation of cause for failure was not possible in 20 patients (14.28%) as given in Figure 8.
Figure 8.
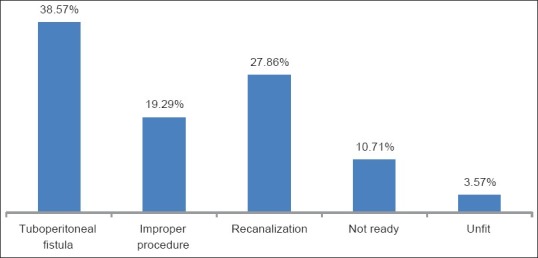
Etiology of failure
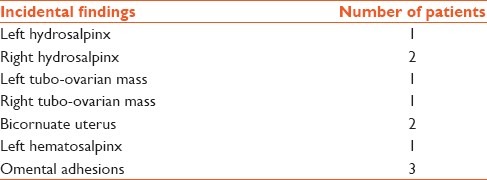
Details regarding improper procedures are described in Table 1. Methods performed during re-sterilization were specified in Table 2 along with incidental findings enumerated in Table 3.
Table 1.
Improper procedure details
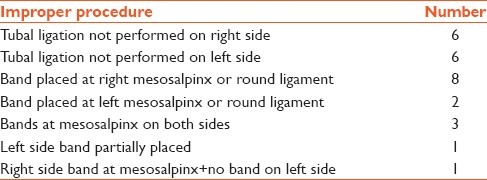
Table 2.
Re-sterilization procedure details
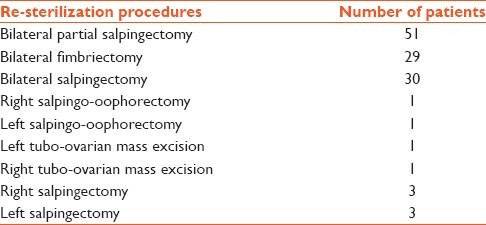
Table 3.
Incidental findings
In comparison related to type of sterilization, 78% (21 cases) improper procedures were observed in Lap TL where 22% (6 cases) in case of minilap. When recanalization was distributed, 52% cases (13) were with minilap, 44 (11) with Lap TL and rest 4% were LSCS cases while %tuboperitoneal fistula distribution as given in chart 12. Similarly, ectopic pregnancies were plotted as 79% (11 cases) in minilap, 14% (2) in Lap TL and 7% in LSCS.
DISCUSSION
Chances of failure are more in younger age as almost 65% failures documented were <30 years which correlates with previous study of Trussell et al. and Peterson et al.[1,2]
In our study, failure with minilap was more (59%) compared to Lap TL (38%) as contrary to Kulier et al. where there was no significant difference in failure rate between two and Hughes who described higher failure rate with Lap TL.[3,4] We came across a case with sterilization-failure documented twice similar to Vessey et al.[5] Patient underwent Lap TL and had failure which was due to improper procedure followed by minilap. This time failure was due to recanalization and during re-sterilization bilateral salpingectomy was performed but there was documented case of spontaneous pregnancy after bilateral salpingectomy in literature.[6]
Failure interval was between 1 and 10 years in 78% of patients which coincides with Vessey et al. and Lassner et al.[5,7] The longest documented failure interval was 23 years[8] whereas in our study it was reported to be 20 years.
A greater proportion of early failures (<1 year) were mainly due to initial non-occlusion of tube due to improper procedure compared with late failures where tubal regeneration leading to spontaneous tubal reapproximation associated with tubal reanastomosis and recanalization or formation of tuboperitoneal fistula were likely factors similar to study of Varma and Gupta.[9] When failure due to improper procedure was further analyzed 78% contribution was from occlusive methods with laparoscopy. In resectional methods with minilap, failure was prominently due to spontaneous luminal regeneration. Both findings were comparable with Soderstrom.[10]
There is an evidence that anatomical tubal patency can occur following a correctly undertaken sterilization methods.[11,12,13,14] However, persisting anatomical tubal patency does not necessarily imply sterilization failure, as tubal patency rates of 1-2% at 3 months and 16% at 5 years have been noted following correctly applied tubal ligation, with the actual pregnancy occurrence of 1-2% over this time period.[10]
When place of previous surgery was evaluated, 60% cases were from PHC. This could be explained with Hughes, Roy et al. and Stovall et al. studies[4,15,16] mentioning that untrained surgeons being constant factor in sterilization-failures. According to study carried out by Premalatha and Tripathi standards of sterilization were followed in <17% of patients.[17]
Pre-existing gynecological pathology or mullerian anomalies were documented as predisposing factors for sterilization-failure[18,19] which were also seen in few of our cases narrated in detail in incidental findings [Table 3].
Ectopic pregnancies constituted 4.55% and 7.5% in <1 year and 1-5 year group similar to Shah et al. and Bhatnagar[20,21] but for higher intervals it had contributed up to 37.5% comparable to Varma and Gupta.[9] These findings can be correlated in simpler terms as initial non-occlusion leading to early failure and as it is less likely to damage the tube, resulting pregnancy is likely to be intrauterine whereas late failures developing due to spontaneous tubal regeneration resulting in abnormal luminal anatomy increasing chances of ectopic pregnancy. This can also explain how 79% ectopics were due to minilap failure.
Almost 60% cases were reported when pregnancy was >12 weeks and out of >20% required major surgical interventions such as hysterotomy, LSCS, laparotomy for ectopic. 30% patients underwent 2nd trimester MTP.
Guidelines are given in standards for female sterilization services, ministry of health and Family Welfare, Government of India, 2006 October. They are as follows. The operating surgeon should identify each fallopian tube clearly, tracing right up to fimbria. Excision of 1 cm of fallopian tube should be done. The site of the occlusion of tube must be in isthmic portion 2-3 cm away from uterine cornu.
CONCLUSION
Female sterilization-failure is well-known and proven entity and no age, method and interval is failure free. Although, it is not completely preventable, failure due to improper procedure can be avoided if we will follow standard guidelines for tubal ligation. Proper counseling of patient regarding chances of failure and early reporting if menses are delayed can help in diagnosing failure in early gestation and to reduce related morbidities.
Footnotes
Source of Support: Nill.
Conflict of Interest: None declared.
REFERENCES
- 1.Trussell J, Guilbert E, Hedley A. Sterilization failure, sterilization reversal, and pregnancy after sterilization reversal in Quebec. Obstet Gynecol. 2003;101:677–84. doi: 10.1016/s0029-7844(02)03156-3. [DOI] [PubMed] [Google Scholar]
- 2.Peterson HB, Xia Z, Hughes JM, Wilcox LS, Tylor LR, Trussell J. The risk of pregnancy after tubal sterilization: Findings from the U.S. collaborative review of sterilization. Am J Obstet Gynecol. 1996;174:1161–8. doi: 10.1016/s0002-9378(96)70658-0. [DOI] [PubMed] [Google Scholar]
- 3.Kulier R, Boulvain M, Walker D, Candolle G, Campana A. Minilaparotomy and endoscopic techniques for tubal sterilisation. Cochrane Database Syst Rev. 2004;3:CD001328. doi: 10.1002/14651858.CD001328.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes GJ. Sterilisation failure. Br Med J. 1977;2:1337–9. doi: 10.1136/bmj.2.6098.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vessey M, Huggins G, Lawless M, McPherson K, Yeates D. Tubal sterilization: Findings in a large prospective study. Br J Obstet Gynaecol. 1983;90:203–9. doi: 10.1111/j.1471-0528.1983.tb08609.x. [DOI] [PubMed] [Google Scholar]
- 6.Bollapragada SS, Bandyopadhyay S, Serle E, Baird C. Spontaneous pregnancy after bilateral salpingectomy. Fertil Steril. 2005;83:767–8. doi: 10.1016/j.fertnstert.2004.07.970. [DOI] [PubMed] [Google Scholar]
- 7.Lassner KJ, Chen CH, Oberle MW, da Trindade TC, Aguinaga H. Analysis of sterilization failure in Brazil. Int J Gynaecol Obstet. 1988;27:255–63. doi: 10.1016/0020-7292(88)90017-3. [DOI] [PubMed] [Google Scholar]
- 8.Huddleston HT, Dunnihoo DR. Long-term sterilization failure: Twenty-three years. J La State Med Soc. 2000;152:427–8. [PubMed] [Google Scholar]
- 9.Varma R, Gupta JK. Failed sterilisation: Evidence-based review and medico-legal ramifications. BJOG. 2004;111:1322–32. doi: 10.1111/j.1471-0528.2004.00281.x. [DOI] [PubMed] [Google Scholar]
- 10.Soderstrom RM. Sterilization failures and their causes. Am J Obstet Gynecol. 1985;152:395–403. doi: 10.1016/s0002-9378(85)80148-4. [DOI] [PubMed] [Google Scholar]
- 11.Grunert GM. Late tubal patency following tubal ligation. Fertil Steril. 1981;35:406–8. [PubMed] [Google Scholar]
- 12.Stock RJ. Histopathologic changes in fallopian tubes subsequent to procedures. Int J Gynecol Pathol. 1983;2:13–27. doi: 10.1097/00004347-198301000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Ayers JW, Johnson RS, Ansbacher R, Menon M, LaFerla JJ, Roberts JA. Sterilization failures with bipolar tubal cautery. Fertil Steril. 1984;42:526–30. doi: 10.1016/s0015-0282(16)48133-1. [DOI] [PubMed] [Google Scholar]
- 14.Cook CL. Evaluation of Falope Ring sterilization by hysterosalpingogram. J Reprod Med. 1982;27:243–5. [PubMed] [Google Scholar]
- 15.Roy KK, Banerjee N, Takkar D. Pregnancy following tubal sterilization: An 11-year survey. Int J Gynaecol Obstet. 2000;68:53–4. doi: 10.1016/s0020-7292(99)00186-1. [DOI] [PubMed] [Google Scholar]
- 16.Stovall TG, Ling FW, Henry GM, Ryan GM., Jr Method failures of laparoscopic tubal sterilization in a residency training program. A comparison of the tubal ring and spring-loaded clip. J Reprod Med. 1991;36:283–6. [PubMed] [Google Scholar]
- 17.Premalatha R, Tripathi MS. A study on the reversal of sterilisation in women over two decades. J Obstet Gynaecol India. 2012;62:62–7. doi: 10.1007/s13224-012-0144-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma D, Singhal SR, Singhal SK. Uterus didelphys, a rare cause for tubal sterilization failure. Aust N Z J Obstet Gynaecol. 1998;38:327–8. doi: 10.1111/j.1479-828x.1998.tb03078.x. [DOI] [PubMed] [Google Scholar]
- 19.McCausland A. Endosalpingosis ("endosalpingoblastosis") following laparoscopic tubal coagulation as an etiologic factor of ectopic pregnancy. Am J Obstet Gynecol. 1982;143:12–24. doi: 10.1016/0002-9378(82)90677-9. [DOI] [PubMed] [Google Scholar]
- 20.Shah JP, Parulekar SV, Hinduja IN. Ectopic pregnancy after tubal sterilization. J Postgrad Med. 1991;37:17–20. [PubMed] [Google Scholar]
- 21.Bhatnagar S. Risk of ectopic pregnancy following tubectomy. Indian J Med Res. 1982;75:47–9. [PubMed] [Google Scholar]


