Abstract
Objective:
The undergraduate teaching in pharmacology has always been a challenging task for medical teachers. Traditional lecture format is monotonous and a passive way of learning. There is a need to shift the educational focus from content centered to case based. In an effort to create interest and further improve the student learning, we have introduced simulated bedside teaching sessions as case based learning (CBL) module (modified CBL-[mCBL]) for 2nd professional MBBS students.
Materials and Methods:
A case scenario of a clinical disease condition was prepared in consultation with a clinician. During the session, the case was presented along with discussion on the disease process, its management and rational drug use. Students were encouraged to participate actively. After the session, students were requested to fill the feedback questionnaire anonymously (both open-ended questions and responses on Likert scale).
Results:
According to the students, factors such as clinical orientation, interactivity and re-enforcement of important points helped them to learn better. Majority of the students (76.09%) found the sessions to be better than theory lectures and tutorials. The fact that the interactive component of departmental feedback (taken at the institutional level) has improved during the last 2 years could be attributed to the introduction of these sessions.
Conclusion:
mCBL (in the presence of departmental faculty and concerned clinician) is a good method of integrating pharmacology with clinical subjects. To make such sessions more reliable, the next planned step is to assess the knowledge gained by the students during such sessions in the future.
Keywords: Case based learning, feedback, pharmacology, questionnaire, undergraduates
INTRODUCTION
Pharmacology, a subject in 2nd professional MBBS, is generally considered as a dry and overburdening subject. Due to its vast and ever-advancing nature, it usually becomes difficult to keep the contents interesting, meaningful and clinically relevant. A number of reforms have been tried in the undergraduate pharmacology curriculum by various institutes, but we have not been able to thoroughly achieve this objective. Clinical orientation of MBBS teaching in pharmacology is essential as it has a bearing on their further training in final professional and internship training program. A good training in pharmacology entails the acquiring of the skill of rational prescribing. However, this goal is not adequately met with by the prevailing curricula. Urrutia-Aguilar et al. in 2012 conducted a study to measure the effectiveness of pharmacology teaching in undergraduate medical students and found that there was an urgent need to review undergraduate training in pharmacology.[1] Pilot surveys conducted among interns by Jaykaran et al. and Akat et al. showed that interns favor bedside teaching of pharmacology for better retention and application in future practice.[2,3]
A lot of stress has been laid on adapting interactive student-centered approaches to learning including problem based learning (PBL) and case based learning (CBL). In active learning, the focus is on the student rather than the teacher. Hence, the student is responsible for their own learning. Both PBL and CBL use a clinical situation that provokes interest in the students on the basis of knowledge that they already have and identifies knowledge gaps that will be addressed during the learning process.[4] The aim of CBL is to teach basic medical sciences in a coherent manner closely related to topics in clinical sciences and re-enforcing the reasoning, collaborative and communication skills of the students.[5,6,7]
It has been our constant endeavor to engrain the subject thoroughly in the minds of the students and to make the subject clinically relevant. Certain changes have already been introduced in the MBBS pharmacology practical curriculum including practicals on pharmacoeconomics, selection of P-drugs, drug interactions, prescription writing etc.[8]
Keeping in mind the prevailing medical curriculum, we introduced CBL in a modified manner (mCBL) which was feasible in our set-up. These sessions have been planned with an aim to help the students inculcate the habit of treating the patient as a whole rather than the disease or symptoms. This way they get trained in individualization of drug therapy. Such sessions have been conducted for topics which are important as per the health care needs of the community.
MATERIALS AND METHODS
The study was conducted in 2nd professional MBBS students (batch of 70 students) after obtaining permission from Institutional Ethics Committee (IEC). A waiver for written informed consent was also taken from IEC.
Preparation
Before each session, a departmental meeting was held to choose the topic and plan the session. After a didactic theory lecture and a standardized tutorial were conducted on the selected topic, a session was planned within the next few days. We prepared a factual case scenario of both complicated and uncomplicated stages of the clinical disease condition. Relevant points of history, general physical examination, investigations and diagnosis were included. The treatment options were discussed in detail. The level of complexity was increased at each step. A clinician of concerned field was invited to take part in the discussion and provide a clinical orientation to the subject. The prepared case scenario was discussed with the clinician and his suggestions were incorporated before the presentation was actually carried out. Students were informed beforehand and were required to come prepared with the topic hence that they could participate actively.
Session
A post-graduate resident of our department presented the case scenario. The discussion was moderated by the faculty (both from pharmacology and the concerned clinical department) who stressed upon the important aspects and also interacted with UGs by asking questions. Stress was laid on rational drug treatment, keeping in mind the patient profile. Students participated actively and were free to clarify their doubts. It was taken care that the environment was friendly, non-threatening and productive. The pharmacologists and clinicians complemented each other in the information provided to students. Before concluding the session, emphasis was laid upon the take home message for the UG students.
Data collection
To assess the perception of students regarding mCBL, at the end of 1 h session, they were requested to fill the feedback questionnaire anonymously. The questionnaire consists of both structured (based on Likert scale) and open-ended questions regarding the suitability and usefulness of the session.
One such trial session was conducted for 2nd professional MBBS students in 2011, on the topic of “tuberculosis.” Upon evaluating the feedback, the response by students was found to be very encouraging. Keeping this in view, we organized three such sessions for the next batch in 2012 on the topics of “epilepsy,” “diabetes mellitus” and “malaria.” The responses obtained in the feedback questionnaires were analyzed using descriptive statistics.
RESULTS
The results from the three sessions held in 2012 were pooled together for the purpose of analysis. Out of the total 188 responses obtained, 183 (97.3%) liked the session, whereas 5 (2.7%) did not like the session. According to the students, the major factors which favored learning included correlation of the topic with clinical scenario, reinforcement of the important points in a particular topic, presence of clinicians and their view-point and the interactive nature of the discussion. Only a few students (2.7%) felt that the presence of too many teachers made the atmosphere a bit threatening which could hamper the learning. The students were also requested to give some suggestions for further improvement of the sessions. These suggestions included; increase in duration and frequency of such sessions (27.4% students), more pictures and videos to be incorporated in the presentation (8.6%) and the photocopy of the case-scenario to be provided to the students for better understanding (3.3%). The students also gave the feedback on the preferred sequence for the didactic lecture, tutorial and case discussion. The majority of the students (74.7%) felt that the ideal sequence is lecture followed by tutorial and then the case discussion. On being asked about the additional topics that the students would like to be covered as case discussions, the suggestions included anti-epileptics, bronchial asthma, hypertension, antimicrobials, tuberculosis, thyroid disorders and others. The responses to some other questions were obtained on Likert scale (strongly disagree - 1, disagree - 2, neither agree nor disagree - 3, agree - 4, strongly agree - 5). The data of the above responses pooled from the three sessions is presented in Table 1. Majority of the students (76.09%) found the sessions to be better than theory lectures and tutorials. Nearly 89.61% of students felt that the sessions stimulated their interest in the subject and reinforced the clinical aspects of the topics discussed. The pattern of individual student response in mCBL-session 1 (on epilepsy) is depicted in Figure 1, mCBL-session 2 (on diabetes mellitus) in Figure 2 and mCBL-session 3 (on malaria) in Figure 3. The question statements for the above responses are provided in Table 1.
Table 1.
Responses of undergraduate students in various sessions
Figure 1.
Pattern of student response in modified case based learning-1 (on epilepsy)
Figure 2.
Pattern of student response in modified case based learning-2 (on diabetes mellitus)
Figure 3.
Pattern of student response in modified case based learning-3 (on malaria)
DISCUSSION
For an effective undergraduate teaching, it should essentially be horizontally and vertically integrated. As per the Vision 2015 document of Medical Council of India (MCI), emphasis should be on the introduction of case scenarios for classroom discussion/case-based learning.[9] In future, this might become an essential part of the medical curriculum. A survey by Vasundara et al. to assess the clinical application of pharmacology knowledge in patient care found that pharmacology teaching needs radical changes.[10] A number of methods and new techniques have been tried by various academicians elsewhere. Rao and Kate introduced problem solving interactive clinical seminars for undergraduates to make the learning process more effective.[11] A number of researchers have also tried to integrate two or more subjects in UG curriculum and found encouraging results.[12,13]
No method of teaching and learning in medicine is ideal since each method is associated with its own benefits and flaws. Didactic lecture format is used most commonly but, it being a passive form of learning, fails to motivate the students to learn more. In an active learning environment, teachers facilitate students’ learning. CBL is an interactive student centered instructor led learning approach.[14] Several researchers compared CBL with didactic form of teaching.[15,16,17] Pearson et al. found CBL to be an effective adjunct to the traditional lecture format.[15] Kassebaum et al. in their study showed that CBL made the learning more enjoyable and improved the interactive ability of the students.[16] Another comparative study conducted by Kamat et al. assessed the impact of case based teaching on learning rational prescribing when compared with the traditional method of teaching and found them to be better in facilitating the learning process.[18]
A literature review of CBL was done by Williams and its role in basic sciences teaching was explored.[4] The article concluded that CBL is an exciting educational prospect which allows students to develop a collaborative, team based approach to their education. Rodrāguez-Barbero and López-Novoa had a positive experience in using CBL in physiology.[19] A study from Manipal indicated that CBL sessions enhanced active learning in microbiology.[20]
The opinion of the students is also highly valuable. They are the best ones to judge if a new methodology is of any benefit to them or not. Hence, student evaluation on the impact of CBL was done by a number of researchers.[17,21] They summarized that the students enjoyed the sessions and felt that it enhanced their understanding. However, the feedback from faculty taken in another study[17] showed that the faculty favored didactic lectures over these sessions, keeping in mind the attentiveness of the students.
In our setup, a formal written feedback from the faculty was not taken, but as per the verbal feedback, the faculty found the students to be more involved, engaged and interested in the sessions. But the importance of didactic lectures could not be undermined.
Tayem concluded that CBL led to a significant improvement in students' self-reported analytical and communication skills, confidence, satisfaction, motivation and engagement.[22]
mCBL is an excellent method for integrating pharmacology with clinical subjects. It enhances the ability of students to understand the concepts and assimilate the knowledge in an effective manner. As the faculty of both the departments is present, it is an excellent opportunity for students to clarify their doubts, if any. They understand that whatever is being taught in pharmacology is actually being practiced in clinical departments and hence pharmacology is not merely a theoretical subject. This would be one of the important ways to integrate basic and clinical subjects. In a way, it is like bringing the patient bedside to classroom.
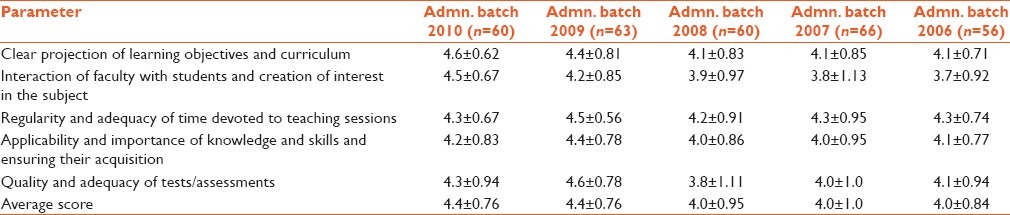
In addition to this, in our institute, an anonymous feedback is taken from UG students at the central level, regarding the subjects taught to them after they clear their University Professional exams.[23] There has been a remarkable improvement in the departmental score depicting the interaction component [parameter 2 of Table 2] over the last few years (18.29% increase on comparing the score of Admn Batch 2010 with the average score of Admn Batch 2008, 2007 and 2006). This could be attributed partly to the introduction of mCBL during this tenure. The students have also given very encouraging comments regarding these sessions in this feedback form. Comments such as “Good sessions as doctors from various specialties taught the importance of application of drugs” and “CBL led to better learning and retention of basic principles of treatment” have further reinforced the usefulness of these sessions.
Table 2.
Departmental feedback score (out of five each) by undergraduate students during the last 5 years
As with any other teaching methodology, this method is also not flawless. This method requires a lot of planning, co-ordination and organization in advance, not only at the departmental, but also inter-departmental level. Hence, feasibility may be an issue in conducting such sessions. Furthermore, it is difficult to discuss all the aspects of the therapy in this format; for example, pharmacokinetics and pharmacodynamics of the drugs may be missed out. It is not wise to cover the entire syllabus in the form of case scenarios as it is not an exam oriented activity. Also, the time consumed for three sessions in a sequence on a particular topic, i.e. lecture followed by tutorial and then a case discussion, may be too much as per the number of teaching hours available according to MCI guidelines. However, this may be justified by the fact that the practicals in pharmacology (pharmacy and animal experiments) have been reduced to a great extent as per MCI guidelines. These practicals can be replaced by the case discussions. Moreover, the entire syllabus need not be covered in this manner. Only the important topics can be included initially and later on, if found suitable by the departmental faculty, either of the didactic lecture or tutorial for a particular topic may be replaced by a case discussion. Hence, the aspect of time consumption is manageable to a great extent.
Another aspect is that we are looking only at short-term impact of the intervention. To look at the long-term effects, i.e., whether this knowledge translates into better prescribing skills, we need to take another feedback when these students become interns.
We need to look not only toward the students' attitudes but also any difference in their knowledge levels. For this, we plan to introduce pre- and post-session questionnaires based upon the content of the topic. This will help us to evaluate whether these sessions have led to any improvement in score and better understanding of the students. Then, we can establish mCBL as an alternative method of teaching pharmacology and make it an essential part of the curriculum.
Recently, MCI has proposed to introduce some reforms in the MBBS curriculum including a decrease in the number of teaching hours in pharmacology. In these settings, these sessions can be very useful as they can reduce a number of theory lectures to be taken on a particular subject, although this may require a great deal of preparation on the part of teachers as well as the students. However, the positive aspect is that such an exercise can be introduced in any institution without any administrative hassles. Such exercises require close co-ordination between the two departments. On the basis of our experience, we can say that mCBL has good acceptance and recognition by students and a high level of satisfaction on the part of teachers. It is a good addition to the armamentarium of pharmacology teaching tools. But whether it can replace the conventional methods requires further studies.
ACKNOWLEDGMENTS
We are thankful to our Principal Dr. Daljit Singh for his valuable guidance and allowing us to share the institutional data regarding departmental feedback. Thanks are also due to the undergraduate students for their efforts in providing a sincere feedback.
Footnotes
Source of Support: Nill.
Conflict of Interest: None declared.
REFERENCES
- 1.Urrutia-Aguilar ME, Martinez-Gonzalez A, Rodriguez R. Measuring the effectiveness of pharmacology teaching in undergraduate medical students. J Patient Saf. 2012;8:26–9. doi: 10.1097/PTS.0b013e31823d0661. [DOI] [PubMed] [Google Scholar]
- 2.Jaykaran, Chavda N, Yadav P, Kantharia ND. Intern doctors' feedback on teaching methodologies in pharmacology. J Pharmacol Pharmacother. 2010;1:114–6. doi: 10.4103/0976-500X.72359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akat PB, Karande VB, Murthy MB, Burute SR. Interns opinion on ‘bedside pharmacology clinics’ and its incorporation in undergraduate curriculum. J Pharmacol Pharmacother. 2012;3:56–8. doi: 10.4103/0976-500X.92519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams B. Case based learning - A review of the literature: Is there scope for this educational paradigm in prehospital education? Emerg Med J. 2005;22:577–81. doi: 10.1136/emj.2004.022707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsou KI, Cho SL, Lin CS, Sy LB, Yang LK, Chou TY, et al. Short-term outcomes of a near-full PBL curriculum in a new Taiwan medical school. Kaohsiung J Med Sci. 2009;25:282–93. doi: 10.1016/S1607-551X(09)70075-0. [DOI] [PubMed] [Google Scholar]
- 6.Malher X, Bareille N, Noordhuizen JP, Seegers H. A case-based learning approach for teaching undergraduate veterinary students about dairy herd health consultancy issues. J Vet Med Educ. 2009;36:22–9. doi: 10.3138/jvme.36.1.22. [DOI] [PubMed] [Google Scholar]
- 7.Engel FE, Hendricson WD. A case-based learning model in orthodontics. J Dent Educ. 1994;58:762–7. [PubMed] [Google Scholar]
- 8.Kaushal S, Chopra SC, Arora S. Modifications in the undergraduate MBBS pharmacology practical curriculum: The DMCH model. Indian J Pharmacol. 2007;39:57–9. [Google Scholar]
- 9.MCI-Vision. 2015. [Last accessed on 2013 Mar 20]. Available from: http://www.mciindia.org/tools/announcement/MCI_booklet.pdf .
- 10.Vasundara K, Kanchan P, Pundarikaksha HP, Girish K, Prassana S, Jyothi R. An imperative need to change pharmacology curriculum: A pilot survey. Indian J Pharmacol. 2010;42:420. doi: 10.4103/0253-7613.71901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao BB, Kate V. Problem solving interactive clinical seminars for undergraduates. J Pharmacol Pharmacother. 2012;3:205–6. doi: 10.4103/0976-500X.95539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vyas R, Jacob M, Faith M, Isaac B, Rabi S, Sathishkumar S, et al. An effective integrated learning programme in the first year of the medical course. Natl Med J India. 2008;21:21–6. [PubMed] [Google Scholar]
- 13.Kate MS, Kulkarni UJ, Supe A, Deshmukh YA. Introducing integrated teaching in undergraduate medical curriculum. Int J Pharm Sci Res. 2010;1:18–22. [Google Scholar]
- 14.Thistlethwaite JE, Davies D, Ekeocha S, Kidd JM, MacDougall C, Matthews P, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach. 2012;34:e421–44. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 15.Pearson TA, Barker WH, Fisher SG, Trafton SH. Integration of the case-based series in population-oriented prevention into a problem-based medical curriculum. Am J Prev Med. 2003;24:102–7. doi: 10.1016/s0749-3797(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 16.Kassebaum DK, Averbach RE, Fryer GE., Jr Student preference for a case-based vs. lecture instructional format. J Dent Educ. 1991;55:781–4. [PubMed] [Google Scholar]
- 17.Hansen WF, Ferguson KJ, Sipe CS, Sorosky J. Attitudes of faculty and students toward case-based learning in the third-year obstetrics and gynecology clerkship. Am J Obstet Gynecol. 2005;192:644–7. doi: 10.1016/j.ajog.2004.10.595. [DOI] [PubMed] [Google Scholar]
- 18.Kamat SK, Marathe PA, Patel TC, Shetty YC, Rege NN. Introduction of case based teaching to impart rational pharmacotherapy skills in undergraduate medical students. Indian J Pharmacol. 2012;44:634–8. doi: 10.4103/0253-7613.100400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodríguez-Barbero A, López-Novoa JM. Teaching integrative physiology using the quantitative circulatory physiology model and case discussion method: Evaluation of the learning experience. Adv Physiol Educ. 2008;32:304–11. doi: 10.1152/advan.00107.2008. [DOI] [PubMed] [Google Scholar]
- 20.Ciraj AM, Vinod P, Ramnarayan K. Enhancing active learning in microbiology through case based learning: Experiences from an Indian medical school. Indian J Pathol Microbiol. 2010;53:729–33. doi: 10.4103/0377-4929.72058. [DOI] [PubMed] [Google Scholar]
- 21.Massonetto JC, Marcellini C, Assis PS, de Toledo SF. Student responses to the introduction of case-based learning and practical activities into a theoretical obstetrics and gynaecology teaching programme. BMC Med Educ. 2004;4:26. doi: 10.1186/1472-6920-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tayem YI. The impact of small group case-based learning on traditional pharmacology teaching. Sultan Qaboos Univ Med J. 2013;13:115–20. doi: 10.12816/0003204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh D, Ahluwalia G, Kaushal S. Increasing the acceptability of student feedback for curriculum revision. Presented at FAIMER; October 2005; Philadelphia, USA. [Google Scholar]


