Abstract
Objective. This study of severely obese adults participating in a two-year lifestyle intervention investigates associations between the independent variables: change in self-efficacy for physical activity (PA) in the face of psychological barriers, perceived behavioural control over PA, and PA self-identity and the dependent variable of change in objectively assessed PA. The intervention comprised four residential periods in a rehabilitation centre and combined diet, physical activity, and cognitive behavioural therapy.
Materials and Methods. Forty-nine severely obese adults (37 women, mean body mass index 42.1 kg/m2) were included in the study. Assessment was done four times using questionnaires and an accelerometer. A linear mixed model based on restricted maximum likelihood was used in analyses for change over time. Associations were studied using linear regression analyses. Age, gender, and change in body mass index were used as control variables.
Results. In the adjusted analyses, change in perceived behavioural control over PA was associated with change in PA (Stand. coeff. = 0.32, p = .005). Change in PA was not associated with either change in self-efficacy over PA in the face of psychological barriers (Stand. coeff. = 0.13, p = .259) or PA self-identity (Stand. coeff. = −0.07, p = .538).
Conclusion. Perceived behavioural control may be a valid target to increase and maintain PA in severely obese adults participating in lifestyle interventions. More research is needed to investigate the process of behaviour change in this population.
Keywords: Severe obesity, Physical activity, Lifestyle intervention, Self-identity, Self-efficacy, Perceived behavioural control, Accelerometer
Introduction
A web of political, societal, and environmental factors contributes to the growing prevalence of overweight and obesity in Western countries (Swinburn et al., 2011). Alarmingly, the group classified as severely obese has increased the most (Sturm, 2007; Midthjell et al., 2013). In obesogenic societies (Swinburn et al., 2011), the health services have responsibility to ameliorate the ailing health, functioning, and quality of life experienced by severely obese individuals (van Nunen et al., 2007). Thus, various obesity surgeries and lifestyle interventions have been developed. Obesity surgery brings about physiological and functional changes, enforcing altered eating behaviours and thus leading to weight loss (Kissler & Settmacher, 2013). By contrast, lifestyle interventions work exclusively through individual modifications and self-management of health-related behaviour (Kirk et al., 2012). A weight loss of 5–10% is regarded as sufficient to gain health effects and reduce the risk of obesity-related comorbidities (Tsigos et al., 2008; Dalle Grave, Calugi & El Ghoch, 2013). The most extensive weight losses are obtained through obesity surgery (Karlsen et al., 2013), whereas subjects attending lifestyle interventions seem to develop more favourable dietary patterns (Johnson et al., 2013). Both intervention types improve health-related quality of life (Karlsen et al., 2013).
In combination with diet modification, physical activity (PA) constitutes a core component of many lifestyle interventions for severely obese adults (Kirk et al., 2012; Dalle Grave, Calugi & El Ghoch, 2013). Studies have shown that PA impacts on weight loss and its maintenance (Catenacci & Wyatt, 2007; Butryn, Webb & Wadden, 2011), improves body composition (Lee et al., 2005; Kay & Fiatarone Singh, 2006; Goodpaster et al., 2010), reduces risk of cardio-metabolic comorbidities (Fogelholm, 2010; Goodpaster et al., 2010), and is positively associated with quality of life (Bond et al., 2006; Lerdal et al., 2011; Jepsen et al., 2013) in severely obese subjects. Thus, given the chronic nature of severe obesity, adherence to PA is important (Tsigos et al., 2008), but unfortunately PA decreases with increasing body mass index (BMI) (Tudor-Locke et al., 2010; Hansen et al., 2013). Severely obese subjects face many barriers to PA, such as the excess body weight itself (Wiklund, Olsén & Willén, 2011; Christiansen, Borge & Fagermoen, 2012) and exposure in public (Wiklund, Olsén & Willén, 2011). A persistent increase of PA seems to be difficult (Borg et al., 2002; Tate et al., 2007). Thus, lifestyle interventions should target and strengthen patients’ resources for PA through provision of knowledge and skills and reinforcement of psychological factors that are likely to influence PA. Hence, self-efficacy for PA, perceived behavioural control over PA, and PA self-identity have been proposed as targets for PA interventions (Hagger, Chatzisarantis & Biddle, 2002; Jackson, Smith & Conner, 2003; Lorentzen, Ommundsen & Holme, 2007; Hansen et al., 2014).
According to Bandura (1997), self-efficacy covers “a belief about what one can do under different sets of conditions with whatever skills one possesses” (p. 37). Self-efficacy is dynamic and modifiable (Bandura, 1997), and in relation to PA, it includes the capability of adoption and maintenance of PA in the face of psychological barriers such as feeling depressed, worried, angry, or stressed (Lorentzen, Ommundsen & Holme, 2007). Self-efficacy for PA in the face of psychological barriers has shown positive associations with change in PA in community samples (Lorentzen, Ommundsen & Holme, 2007). The related concept of perceived behavioural control refers to a person’s “belief as to how easy or difficult performance of the behaviour is likely to be” (Ajzen & Madden, 1986, p. 457). Perceived behavioural control predicts PA behaviour (Hagger, Chatzisarantis & Biddle, 2002) and plays a role in PA behaviour change in community samples (Lorentzen, Ommundsen & Holme, 2007). Identity is a third factor influencing human behaviour. Hence, there is a reciprocal reinforcing relationship between a behaviour-specific identity and repetition of that behaviour. Furthermore, identity is a product of interaction with others (Charng, Piliavin & Callero, 1988). PA identity, i.e., “identifying oneself as a physically active person” (Lorentzen, Ommundsen & Holme, 2007, p. 95), has shown positive associations with self-reported PA (Jackson, Smith & Conner, 2003) and change in PA (Lorentzen, Ommundsen & Holme, 2007) in community samples.
Common outcome variables in research on lifestyle interventions for severely obese adults are body weight and risk factors for medical comorbidities (Anderson, Conley & Nicholas, 2007; Goodpaster et al., 2010; Danielsen et al., 2013; Karlsen, Sohagen & Hjelmesaeth, 2013). Because the pathway for these outcomes is behaviour change, it is pivotal to understand factors involved in the behaviour change process. However, to our knowledge, no studies have investigated associations in patterns of change between psychological factors and objectively assessed PA in severely obese adults during a lifestyle intervention. Thus, the aim of this study was to investigate associations between the independent variables: change (Δ) in self-efficacy, Δ perceived behavioural control, and Δ self-identity and the dependent variable of Δ PA. The study hypothesis was that there would be positive associations in the patterns of change between self-efficacy for PA in the face of psychological barriers, perceived behavioural control over PA, and PA identity and objectively assessed PA in severely obese adults participating in a two-year lifestyle intervention.
Materials and Methods
Participants and setting
The Haugland Obesity Study has a two-year prospective design. We assessed severely obese patients before, during, and between residential periods in Red Cross Haugland Rehabilitation Centre (RCHRC) in Norway, where they participated in a two-year lifestyle intervention. The programme was funded by the public health services. For those with jobs, the social welfare system paid sick leave benefits during the residential periods. Referral to RCHRC was done by general practitioners. Referred patients were called in to a two-week stay, wherein motivation for change and ability to function in a group were assessed and participation in the programme was decided. Due to limited capacity of the centre, the time from referral to this assessment stay was up to two years. Fifty-three patients, divided in four groups, started the actual intervention (the time point which constituted the baseline of the present study) and were all offered inclusion in the present study. After the intake of these four groups, the public health services reduced the funding to RCHRC and cut the intervention for new patients to a one-year programme with shorter residential stays. Thus, we had to discontinue inclusion of participants.
Inclusion criteria for the intervention were age between 18 and 60 years, and BMI ≥ 40 kg/m2 with or without comorbidities, or ≥ 35 kg/m2 with comorbidities, such as type 2 diabetes, treatment-resistant hypertension, and sleep apnoea (Norwegian Directorate of Health, 2009). Exclusion criteria were: referral to, or, previous obesity surgery; pregnancy; severe cardiovascular disease; alcohol or substance abuse; and mental illness or physical impairment that would prevent adherence to the intervention.
Intervention
The lifestyle intervention was a multi-component programme developed by the health professionals at RCHRC, built on recommendations for best practice (Shaw et al., 2005; Kirk et al., 2012; Dalle Grave, Calugi & El Ghoch, 2013; Olander et al., 2013) and prior experience. The objective was to strengthen favourable PA and diet-related behaviour. The intervention covered 15 weeks over two years with four residential periods of six, three, three, and three weeks’ duration. A team of physicians, nurses, physiotherapists, exercise therapist, and dietician–many with training in cognitive behavioural therapy (CBT) (Shaw et al., 2005)–delivered mandatory practical and theoretical sessions on PA, diet, and CBT. The PA consisted of supervised and un-supervised out- and indoor activities, in groups and individually. Brisk walking, swimming, strength training, ball games, and aerobics were the predominant activities during the residential periods, bringing on moderate to high intensities of PA. The scheduled PA lasted 20–60 min per session, in total nine to eleven hours per week. In addition, the patients were encouraged to carry out PA on their own initiative. Taking preferences, limitations, and sustainability into account, each patient developed a plan for PA for home periods and discussed it with staff. Patients were recommended to combine endurance and strength training and undertake at least 60 daily minutes of PA, which could be divided in intervals of down to ten minutes (Becker et al., 2004). Thus, no standard exercise programme was performed in the home periods. The main goal regarding diet was adaptation to a sustainable, healthy diet and a favourable eating-pattern. The meal plan at RCHRC was based on the Nordic Nutrition Recommendations (Becker et al., 2004) with three low-fat, high-fibre, and energy-reduced meals and two to three snacks per day. Most of the meals were provided by the canteen. However, the patients prepared some of their meals in supervised groups, and they ate together. They were advised to follow the same dietary principles at home. Thus, severe energy-restriction was not applied. In total, eleven group sessions of CBT, led by members of the health care team, took place, five during the six-week residential period and two during each of the subsequent three three-week periods. Before the end of each session, home work was given, and the following session started with a review of that. In sessions 1–5, during the first stay, the methods and instruments of CBT were introduced and related to change in PA and eating. When the patients came back for the subsequent periods, experiences from the home periods were discussed in sessions 6–11 within the framework of CBT. For eight patients who expressed a need, individual CBT was also provided.
Planning, barrier identification, and relapse prevention and management were practiced to strengthen self-management of PA and eating (Olander et al., 2013). The group-based activities aimed at stimulating peer support (Olander et al., 2013). Self-monitoring in home periods was promoted using PA diaries (Olander et al., 2013) in which patients reported on PA and a few added information on diet and success stories. All patients sent their diaries to RCHRC every month. There was no other structured follow-up between the residential periods. Patients were encouraged to contact their general practitioner if they needed more support and relatives were not involved in the intervention.
Measures and procedures
Data were collected four times between February 2010 and October 2012 (Fig. 1). The first collection, baseline, was done prior to the start of the intervention, the second at the end of the first residential stay and the third before the third stay, one year from baseline. The final data collection took place before the fourth and last stay, two years from baseline. Socio-demographic data in this study are baseline data.
Figure 1. Flow chart for the two-year follow-up study of severely obese adults in a lifestyle intervention.
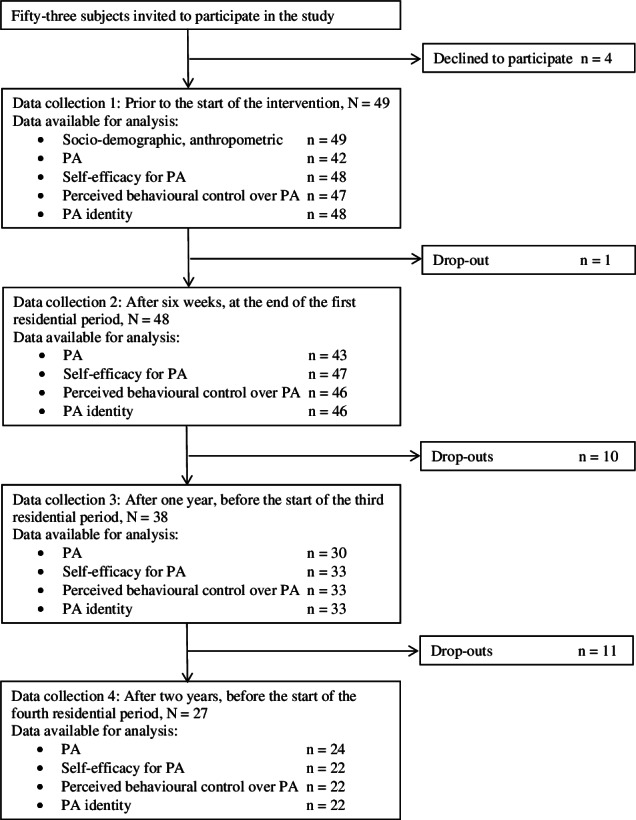
PA, physical activity.
Psychological factors
The psychological factors were assessed using self-reported questionnaires. Self-efficacy for PA was assessed using a five-item measure. The participants indicated the extent to which they were confident in their ability to perform planned PA in the face of psychological barriers (i.e., feeling tired, depressed, anxious, angry, and stressed) on a seven-point scale from 1 (“not at all confident”) to 7 (“very confident”). The scale is a shortened and moderated version of the original instrument developed by Bandura (2001). The version used in this study has demonstrated excellent internal consistency with a Cronbach alpha coefficient of 0.91 (Hansen et al., 2014). Another five-item measure was used to assess perceived behavioural control. The participants rated their agreement with three positive (e.g., “I have total control over being regularly physically active”) and two negative statements (e.g., “Being regularly physically active is difficult for me”) on a seven-point scale from 1 (“totally agree”) to 7 (“don’t agree at all”). The scale is an extended and moderated version of the original instrument developed by Norman & Smith (1995). The version used in this study has demonstrated acceptable internal consistency with a Cronbach alpha coefficient of 0.67 (Hansen et al., 2014). PA self-identity was assessed using a three-item measure. The participants indicated the extent to which they agreed with statements such as “Being physically active is a big part of who I am” on a five-point scale from 1 (“fits poorly”) to 5 (“fits well”). The scale is a shortened and moderated version of the original instrument developed by Anderson & Cychosz (1994). The version used in this study has demonstrated excellent internal consistency with a Cronbach alpha coefficient of 0.91 (Hansen et al., 2014). All three instruments have shown positive cross-sectional associations with objectively assessed PA in adults (Hansen et al., 2014).
Physical activity
PA was measured using the accelerometer Actigraph GTI M (Actigraph, Fort Walton Beach, FL, USA), which is a hip-worn electronic movement sensor that converts acceleration into the arbitrary unit “counts”. The counts increase with the magnitude of the work rate for walking. The participants were instructed to wear the accelerometer on the right hip for seven consecutive days, except while sleeping or during water activities. The second assessment was completed towards the end of the first residential stay whereas the others took place in home periods (Fig. 1). The data were analysed with the Actigraph software ActiLife v. 5.3. A wear-time of ≥ ten hours per day for ≥ four days was the criterion for a valid measure. Periods of ≥60 consecutive minutes without counts were defined as non-wear-time, allowing for up to two minutes of counts greater than zero within these 60 min (Trost, McIver & Pate, 2005; Sirard et al., 2011). The counts were summed and averaged over the total wear-time to indicate the overall PA in counts per minute (CPM). The accelerometer has been found to be valid in severely obese adults (Aadland & Anderssen, 2012) and accelerometer-assessed PA has superior validity compared to self-reported data (Prince et al., 2008).
Socio-demographic information and anthropometry
Socio-demographic information was obtained from questionnaires. Height was measured without shoes to the nearest 0.5 cm with a wall mounted stadiometer (SECA, Germany). Weight was measured on a bioelectrical impedance analysis device (BC 420S MA, Tanita Corp, Tokyo, Japan) and reported to the nearest 0.1 kg.
Ethics
Written informed consent was obtained from all participants prior to the data collection, in accordance with the Helsinki Declaration. Ethical approval was obtained from the Regional Committee for Medical and Health Research Ethics for South-East Norway (registration number 2010/159).
Statistical analysis
Before calculating the mean values for the psychological factors, the three positively worded items for perceived behavioural control were reversed. Thus, higher mean values indicated stronger self-efficacy, perceived control, and identity. Cronbach alpha was used to determine the internal consistency of the instruments.
Data on civil status were dichotomized into “married/cohabiting” vs “single/divorced”, educational level into “<15 years of education” vs. “≥15 years of education” (i.e., college/university), and employment into “not working” (i.e., being unemployed or receiving pensions or benefits) vs. “working”. BMI was calculated as weight in kilograms divided by the square of the height in meters.
A linear mixed model based on restricted maximum likelihood estimation with random intercept for subjects was used in all analyses for change over time (Twisk, 2003), using least significant difference from baseline. Effect size (ES) for change was calculated by subtracting the two-year score from the baseline score, divided by the standard deviation (SD) at baseline. ES were judged against the standard criteria proposed by Cohen: Small change (0.2 to <0.5), moderate change (0.5 to <0.8), and large change (≥0.8) (Ellis, 2011).
The associations between the independent variables: Δ self-efficacy for PA in the face of psychological barriers, Δ perceived behavioural control over PA, and Δ PA self-identity and the dependent variable of Δ PA were analysed using linear regression, applying delta scores between time points (Δy1 = y1−y0; Δx1 = x1−x0; Δy2 = y2−y1, etc.) (Twisk, 2003). For the independent and dependent variables and BMI, the differences between baseline and week six (Δ1), between week six and year one (Δ2), and between year one and year two (Δ3) were used. The linear mixed model was omitted because the interpretation of the regression coefficients in such a model is difficult, due to mixing of longitudinal (with-in subject) changes and the cross-sectional (between-subject) differences (Twisk, 2003). Age, gender, and Δ BMI served as covariates in the multiple regression analyses. A total of N = 71 observations was included in the regression analyses. Residuals were normally distributed in all models.
Baseline subject characteristics are presented as percentages for categorical data and mean values (SD) for continuous variables. The estimates, obtained from the linear mixed model, for the psychological factors, PA, and BMI are presented as means with 95% confidence intervals (CI) for the four assessment points. We performed a drop-out analysis with the chi-squared test for difference in gender and the independent samples t-test for differences in other variables.
The statistical analyses were done using SPSS v. 20.0 (SPSS Inc., Chicago, USA). A two-sided p-value ≤ 0.05 indicated statistical significance.
Results
Forty-nine patients (37 women, 75.5%) consented to participate in the study. Baseline characteristics are presented in Table 1. Other details of the participants have been presented previously (Jepsen et al., 2013; Aadland et al., 2014).
Table 1. Characteristics of the study sample at baseline, N = 49.
| Age, mean (SD) | 43.6 (9.4) |
| Gender, n (%) | |
| Women | 37 (75.5) |
| Socio-demographic status, n (%) | |
| Married/cohabiting | 30 (61.2) |
| Having children | 27 (55.1) |
| Formal education ≥ 15 years | 22 (44.9) |
| Employed | 41 (83.7) |
| Anthropometrics, mean (SD) | |
| Body mass index, kg/m2 | 42.1 (6.0) |
Notes.
- SD
- Standard deviation
Drop-outs and available data for all time points are displayed in Fig. 1. At year two, twenty-two participants (44.9%, 16 women and six men) were lost to follow-up. Reasons for dropping out of the intervention included pregnancy, referral to obesity surgery, having reached personal weight goal, health problems, or obligations that interfered with the intervention. Six participants dropped out for unknown reasons and five withdrew from the study due to problems with the study protocol (repeated blood tests and assessments of maximal oxygen consumption which were included in the Haugland Obesity Study). The participants lost to follow-up did not differ from those who completed the study with regards to gender, age, BMI, PA, or psychological factors at baseline, or initial changes (during the first six weeks) in BMI, PA, or psychological factors. Missing data for psychological factors resulted from participants being absent when the questionnaires were administered at RKHRC. Furthermore, some of the accelerometer-obtained data failed to fulfil the validity requirements.
The internal consistency of the measures of self-efficacy, perceived behavioural control, and self-identity, calculated at baseline, were acceptable to excellent using Cronbach alpha coefficients of 0.92, 0.67, and 0.93, respectively.
Table 2 shows that PA increased significantly from baseline to the end of the first residential period and remained increased at the one-year follow-up. However, after two years the increase in PA was not maintained (ES = 0.24). All three psychological factors were significantly strengthened at the end of the first residential period (Table 2). However, self-efficacy for PA in the face of psychological barriers decreased thereafter and at one year the improvement had vanished (ES = 0.14). In contrast, perceived behavioural control over PA (ES = 0.51) and PA self-identity (ES = 0.74) remained stronger at year one and two. Compared to baseline, BMI was significantly lower at the three subsequent assessments. However, the weight loss achieved during the first year was only partly maintained at year two (Table 2). The mean weight loss from baseline constituted 4.8% after six weeks, 6.4% at year one, and 3.3% at year two.
Table 2. Mixed-effect model estimates: psychological factors, PA, and BMI during the two-year lifestyle intervention for severely obese adults.
| Baseline | Week six | Year one | Year two | ||||
|---|---|---|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | p d | Mean (95% CI) | p d | Mean (95% CI) | p d | |
| Psychological factors | |||||||
| Self-efficacy for PA in the face of psychological barriersa |
5.1 (4.7, 5.5) | 5.6 (4.1, 6.0) | .029 | 5.4 (5.0, 5.9) | .141 | 5.5 (5.0, 6.0) | .154 |
| Perceived behavioural control over PAb | 4.8 (4.5, 5.1) | 5.4 (5.0, 5.7) | .003 | 5.3 (4.9, 5.7) | .026 | 5.4 (4.9, 5.8) | .022 |
| PA identityc | 2.7 (2.5, 3.0) | 3.1 (2.9, 3.4) | .001 | 3.2 (2.9, 3.5) | <.001 | 3.4 (3.1, 3.7) | <.001 |
| Accelerometer assessed PA, counts per minute | 276 (241, 311) | 452 (417, 486) | <.001 | 327 (286, 368) | .036 | 290 (244, 335) | .606 |
| BMI, kg/m2 | 42.1 (40.3, 43.8) | 40.1 (38.4, 41.8) | <.001 | 39.4 (37.6, 41.1) | <.001 | 40.7 (38.9, 42.5) | .001 |
Notes.
Scale 1–7; higher scores represent stronger self-efficacy for PA in the face of psychological barriers.
Scale 1–7; higher scores represent stronger perceived behavioural control over PA.
Scale 1–5; higher scores represent stronger PA identity.
p-values for change from baseline.
- PA
- Physical activity
- BMI
- Body mass index
- CI
- Confidence interval
Significant p-values (≤0.05) in bold.
Table 3 shows the associations between change in the psychological factors and Δ PA over the two-year intervention. Δ perceived behavioural control was the only independent variable that was significantly associated with Δ PA during the two years.
Table 3. Simple and multiple linear regression analysis with Δ counts per minute as the dependent variable.
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
| Reg. coeff. (95% CI) | Stand. coeff. | p | Reg. coeff. (95% CI) | Stand. coeff. | p | |
| Age | −1.95 (−6.45, 2.54) | −.09 | .390 | −1.21 (−5.66, 3.25) | −.06 | .590 |
| Gender (refer to women) | 34.73 (−66.26, 135.72) | .08 | .496 | 13.93 (−83.85, 111.70) | .03 | .777 |
| Δ BMI | −44.63 (−65.53, −23.74) | −.44 | <.001 | −39.08 (−61.81, −16.36) | −.38 | .001 |
| Δ self-efficacy for PA | 28.29 (−12.56, 69.15) | .16 | .172 | 21.84 (−16.48, 60.17) | .13 | .259 |
| Δ perceived behavioural control over PA | 66.51 (31.40, 101.63) | .41 | <.001 | 51.11 (16.17, 86.06) | .32 | .005 |
| Δ PA identity | 40.78 (−25.11, 106.68) | .14 | .221 | −20.14 (−85.07, 44.80) | −.07 | .538 |
Notes.
Number of observations: 71.
- Δ
- Change
- Reg. coeff.
- Regression coefficients
- CI
- Confidence interval
- Stand. coeff.
- Standardized coefficients
- BMI
- Body mass index
- PA
- Physical activity
Age, gender, Δ BMI were included as covariates in the adjusted model.
Significant p-values in bold.
Discussion
In the present two-year study of associations between change in psychological factors for PA and Δ PA in severely obese adults, we found that Δ perceived behavioural control was associated with Δ PA. By contrast, Δ self-efficacy and Δ self-identity showed no association with Δ PA. Although not directly comparable, our findings differ from a cross-sectional study using the same measures which revealed positive relationships between PA and all the three psychological factors, with self-identity for PA showing the strongest association (Hansen et al., 2014).
It has been proposed that scales on perceived behavioural control reveal aspects of two different dimensions, namely control and difficulty (Sparks, Guthrie & Shepherd, 1997). With respect to the instrument used in this study, the positively worded items may capture control while the negative tap into difficulties, which could explain the Cronbach alpha of 0.67. Still, perceived behavioural control over PA was the only independent variable that worked as hypothesised. Not only was it strengthened during the intervention with a moderate ES (Ellis, 2011), but the change of it was also associated with Δ PA. Perceived behavioural control has shown cross-sectional associations with self-reported PA in adult obesity surgery patients (Hunt & Gross, 2009) and overweight and obese adolescents (Plotnikoff et al., 2013). However, to our knowledge, no studies have examined this variable during lifestyle interventions and related it to Δ PA.
Although self-efficacy, as such, is a global concept (Bandura, 1997) the measure used in this study was limited to self-efficacy in the face of psychological barriers to PA. The initial strengthening had disappeared at later assessments and was not associated with behaviour change. This could be interpreted as if the intervention did not target or succeed in strengthening self-efficacy in the face of psychological barriers, or it may indicate that psychological barriers did not play a central role in the PA of these subjects. Other barriers, such as time limitations, which we have not investigated, may be of greater significance (Biddle & Fox, 1998). Still, a longitudinal study found a positive relationship between moods and PA in overweight to obese adults with diabetes. However, the data were reported by lifestyle coaches, not patients (Venditti et al., 2014), implying a possible responder bias (Ahmed et al., 2012).
Next, the intervention strengthened the PA self-identity with a moderate ES (Ellis, 2011). Embarrassment, poor experience, and non-identification with PA may be obstacles to PA in obese adults (Biddle & Fox, 1998; Hills & Byrne, 2006). So the strengthening of PA identity could be regarded as positive (Biddle & Fox, 1998). However, in our study we could not confirm that strengthened identity translates into more PA. In community samples, PA identity has shown positive correlations with objectively measured (Hansen et al., 2014) and self-reported (Jackson, Smith & Conner, 2003) PA. Thus, this phenomenon deserves attention in future research and in clinical practice.
Regarding the impact of body weight, cross-sectional data have demonstrated an adverse relationship between BMI and objectively assessed PA (Hansen et al., 2013) and BMI and perceived behavioural control over PA (Caperchione et al., 2008). However, when controlling for Δ BMI, Δ perceived behavioural control and Δ PA still showed associations in the present study.
Overall, the findings suggest that factors associated with PA in community samples (Jackson, Smith & Conner, 2003; Lorentzen, Ommundsen & Holme, 2007; Hansen et al., 2014) should not be generalised to samples of severely obese adults in lifestyle interventions without caution and testing. Social and environmental factors, including family, work place, and community, may predict and mediate the mechanisms of change in PA in this population (Vartanian & Shaprow, 2008; Wiklund, Olsén & Willén, 2011). Thus, future research could take broader perspectives and adopt an ecological approach (Bauman et al., 2012).
Our study confirms the findings from other studies (Borg et al., 2002; Tate et al., 2007) that maintenance of PA is an unresolved challenge. With regards to the overall PA, the initial and year two PA (Table 2) were similar to the PA of American obese adults (288 CPM) (Tudor-Locke et al., 2010) and their Norwegian counterparts (women: 276 CPM, men: 290 CPM) (Hansen et al., 2013), whereas the mean value from the second assessment (Table 2) was well above the 344 CPM for American normal weight (Tudor-Locke et al., 2010) and 352 CPM for women and 368 CPM for men of normal weight in Norway (Hansen et al., 2013).
Regarding weight loss, the one-year reduction of BMI (Table 2) was within the criterion for success, defined as 5–10% reduction from the start of an intervention (Tsigos et al., 2008; Dalle Grave, Calugi & El Ghoch, 2013). However, patients had regained some of the weight at year two which is a common challenge in lifestyle interventions (Dalle Grave, Calugi & El Ghoch, 2013).
The present study offered novelty and strength as it used data from four time points and therefore could provide information about patterns of change throughout the two-year intervention. In addition, assessing PA objectively with accelerometers is superior to self-reported PA (Prince et al., 2008). However, accelerometers fail to capture water activities, bicycling, and strength training (Warren et al., 2010). For the present study, this limitation probably caused a 25% underestimation of the true overall PA for the second assessment (Aadland et al., 2014), as such activities were common during the residential period. Still, for the purpose of the study, we decided to avoid reporting of intensity-specific PA, due to difficulties of interpretation when applying count thresholds to separate different intensities of PA generally (Orme et al., 2014) and in the severely obese population specifically (Aadland & Steene-Johannessen, 2012). Underestimation of PA was probably a minor problem when assessing trends over the home periods, because patients generally did not engage in such activities (Aadland & Robertson, 2012), and because the underestimation would be equally distributed over time.
The main weakness of this study was the relatively high proportion of drop-outs and missing data. Although the drop-out analysis did not reveal differences between the completers and the non-completers, bias cannot be ruled out. However, by using the mixed model based on maximum likelihood estimation and including all valid observations from all four time points, the statistical power increased. Still, our results are based on associations and thus, causal relationships cannot be inferred. Lastly, the participants were a self-selected, treatment-seeking group, participating in a specific intervention programme and there was no control group. While common in clinical studies, these weaknesses limit the generalisability of our results. For transparency and usefulness, we have therefore attempted to report rigorously on the intervention and the flow of the participants (Vandenbroucke et al., 2007).
Conclusion
Little is known about factors related to the process of change of PA behaviour in severely obese adults participating in lifestyle interventions. We hypothesised that the independent variables: Δ self-efficacy for PA, Δ perceived behavioural control over PA, and Δ PA self-identity would be associated with the dependent variable of Δ PA in the sample of severely obese adults who participated in a two-year programme. However, such an association was only confirmed between Δ perceived behavioural control and Δ PA. More research is required to investigate PA behaviour change processes in severely obese both in non-residential and residential settings and with larger samples and stronger design. An ecological framework may provide a good structure (Bauman et al., 2012), with both quantitative and qualitative methods being suitable.
The findings of the present study indicate that perceived behavioural control may be a valid target for increase and maintenance of PA in severely obese adults.
Acknowledgments
We thank the staff at RCHRC for their assistance in the data collection and express our sincere gratitude to the participants.
Funding Statement
The study was financially supported by the Faculty of Health Studies, Sogn og Fjordane University College, Norway. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
Lesley Robertson is employed by the Red Cross Haugland Rehabilitation Centre and John Roger Andersen is employed by the Førde Health Trust. The authors declare there are no competing interests.
Author Contributions
Randi Jepsen conceived and designed the experiments, performed the experiments, analyzed the data, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Eivind Aadland conceived and designed the experiments, performed the experiments, analyzed the data, reviewed drafts of the paper.
Lesley Robertson reviewed drafts of the paper.
Merete Kristiansen analyzed the data, reviewed drafts of the paper.
John Roger Andersen and Gerd Karin Natvig conceived and designed the experiments, analyzed the data, reviewed drafts of the paper.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Ethical approval was obtained from the Regional Committee for Medical and Health Research Ethics for South-East Norway (registration number 2010/159).
References
- Aadland & Anderssen (2012).Aadland E, Anderssen SA. Treadmill calibration of the Actigraph GT1M in young-to-middle-aged obese-to-severely obese subjects. Journal of Obesity. 2012;2012 doi: 10.1155/2012/318176. Article 318176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aadland et al. (2014).Aadland E, Jepsen R, Andersen JR, Anderssen SA. Differences in fat loss in response to physical activity among severely obese men and women. Journal of Rehabilitation Medicine. 2014;46:363–369. doi: 10.2340/16501977-1786. [DOI] [PubMed] [Google Scholar]
- Aadland & Robertson (2012).Aadland E, Robertson L. Physical activity is associated with weight loss and increased cardiorespiratory fitness in severely obese men and women undergoing lifestyle treatment. Journal of Obesity. 2012;2012 doi: 10.1155/2012/810594. Article 810594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aadland & Steene-Johannessen (2012).Aadland E, Steene-Johannessen J. The use of individual cut points from treadmill walking to assess free-living moderate to vigorous physical activity in obese subjects by accelerometry: is it useful? BMC Medical Research Methodology. 2012;12:172. doi: 10.1186/1471-2288-12-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed et al. (2012).Ahmed S, Berzon RA, Revicki DA, Lenderking WR, Moinpour CM, Basch E, Reeve BB, Wu AW, International Society for Quality of Life Research The use of patient-reported outcomes (PRO) within comparative effectiveness research: implications for clinical practice and health care policy. Medical Care. 2012;50:1060–1070. doi: 10.1097/MLR.0b013e318268aaff. [DOI] [PubMed] [Google Scholar]
- Ajzen & Madden (1986).Ajzen I, Madden TJ. Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology. 1986;22:453–474. doi: 10.1016/0022-1031(86)90045-4. [DOI] [Google Scholar]
- Anderson & Cychosz (1994).Anderson DF, Cychosz CM. Development of an exercise identity scale. Perceptual and Motor Skills. 1994;78:747–751. doi: 10.2466/pms.1994.78.3.747. [DOI] [PubMed] [Google Scholar]
- Anderson, Conley & Nicholas (2007).Anderson JW, Conley SB, Nicholas AS. One hundred pound weight losses with an intensive behavioral program: changes in risk factors in 118 patients with long-term follow-up. American Journal of Clinical Nutrition. 2007;86:301–307. doi: 10.1093/ajcn/86.2.301. [DOI] [PubMed] [Google Scholar]
- Bandura (1997).Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997. [Google Scholar]
- Bandura (2001).Bandura A. Guide for constructing self-efficacy scales. Stanford: Stanford University; 2001. [Google Scholar]
- Bauman et al. (2012).Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW, Lancet Physical Activity Series Working Group Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- Becker et al. (2004).Becker W, Lyhne N, Pedersen AN, Aro A, Fogelholm M, Phórsdottir I, Alexander J, Anderssen SA, Meltzer HM, Pedersen JI. Nordic nutrition recommendations 2004—integrating nutrition and physical activity. Scandinavian Journal of Nutrition. 2004;48:178–187. doi: 10.1080/1102680410003794. [DOI] [Google Scholar]
- Biddle & Fox (1998).Biddle SJ, Fox KR. Motivation for physical activity and weight management. International Journal of Obesity and Related Metabolic Disorders. 1998;22(Suppl 2):S39–S47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- Bond et al. (2006).Bond DS, Evans RK, DeMaria E, Wolfe L, Meador J, Kellum J, Maher J, Warren BJ. Physical activity and quality of life improvements before obesity surgery. American Journal of Health Behavior. 2006;30:422–434. doi: 10.5993/AJHB.30.4.8. [DOI] [PubMed] [Google Scholar]
- Borg et al. (2002).Borg P, Kukkonen-Harjula K, Fogelholm M, Pasanen M. Effects of walking or resistance training on weight loss maintenance in obese, middle-aged men: a randomized trial. International Journal of Obesity and Related Metabolic Disorders. 2002;26:676–683. doi: 10.1038/sj.ijo.0801962. [DOI] [PubMed] [Google Scholar]
- Butryn, Webb & Wadden (2011).Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatric Clinics of North America. 2011;34:841–859. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caperchione et al. (2008).Caperchione CM, Duncan MJ, Mummery K, Steele R, Schofield G. Mediating relationship between body mass index and the direct measures of the Theory of Planned Behaviour on physical activity intention. Psychology, Health & Medicine. 2008;13:168–179. doi: 10.1080/13548500701426737. [DOI] [PubMed] [Google Scholar]
- Catenacci & Wyatt (2007).Catenacci VA, Wyatt HR. The role of physical activity in producing and maintaining weight loss. Nature Clinical Practice: Endocrinology & Metabolism. 2007;3:518–529. doi: 10.1038/ncpendmet0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charng, Piliavin & Callero (1988).Charng HW, Piliavin JA, Callero PL. Role-identity and reasoned action in the prediction of repeated behavior. Social Psychology Quarterly. 1988;51:303–317. doi: 10.2307/2786758. [DOI] [Google Scholar]
- Christiansen, Borge & Fagermoen (2012).Christiansen B, Borge L, Fagermoen MS. Understanding everyday life of morbidly obese adults-habits and body image. International Journal of Qualitative Studies on Health and Well-being. 2012;7:17255. doi: 10.3402/qhw.v7i0.17255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalle Grave, Calugi & El Ghoch (2013).Dalle Grave R, Calugi S, El Ghoch M. Lifestyle modification in the management of obesity: achievements and challenges. Eating and Weight Disorders. 2013;18:339–349. doi: 10.1007/s40519-013-0049-4. [DOI] [PubMed] [Google Scholar]
- Danielsen et al. (2013).Danielsen KK, Svendsen M, Maehlum S, Sundgot-Borgen J. Changes in body composition, cardiovascular disease risk factors, and eating behavior after an intensive lifestyle intervention with high volume of physical activity in severely obese subjects: a prospective clinical controlled trial. Journal of Obesity. 2013;2013 doi: 10.1155/2013/325464. Article 325464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis (2011).Ellis PD. The essential guide to effect sizes: statistical power, meta-analysis and the interpretation of research results. Cambridge: Cambridge University Press; 2011. [Google Scholar]
- Fogelholm (2010).Fogelholm M. Physical activity, fitness and fatness: relations to mortality, morbidity and disease risk factors. A systematic review. Obesity Reviews. 2010;11:202–221. doi: 10.1111/j.1467-789X.2009.00653.x. [DOI] [PubMed] [Google Scholar]
- Goodpaster et al. (2010).Goodpaster BH, DeLany JP, Otto AD, Kuller L, Vockley J, South-Paul JE, Thomas SB, Brown J, McTigue K, Hames KC, Lang W, Jakicic JM. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA. 2010;304:1795–1802. doi: 10.1001/jama.2010.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger, Chatzisarantis & Biddle (2002).Hagger MS, Chatzisarantis NLD, Biddle SJH. A meta-analytic review of the theories of reasoned action and planned behavior in physical activity: predictive validity and the contribution of additional variables. Journal of Sport & Exercise Psychology. 2002;24:3–32. [Google Scholar]
- Hansen et al. (2013).Hansen BH, Holme I, Anderssen SA, Kolle E. Patterns of objectively measured physical activity in normal weight, overweight, and obese individuals (20–85 years): a cross-sectional study. PLoS ONE. 2013;8:e505. doi: 10.1371/journal.pone.0053044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen et al. (2014).Hansen BH, Ommundsen Y, Holme I, Kolle E, Anderssen SA. Correlates of objectively measured physical activity in adults and older people: a cross-sectional study of population-based sample of adults and older people living in Norway. International Journal of Public Health. 2014;59:221–230. doi: 10.1007/s00038-013-0472-3. [DOI] [PubMed] [Google Scholar]
- Hills & Byrne (2006).Hills AP, Byrne NM. State of the science: a focus on physical activity. Asia Pacific Journal of Clinical Nutrition. 2006;15(Suppl):40–48. [PubMed] [Google Scholar]
- Hunt & Gross (2009).Hunt HR, Gross AM. Prediction of exercise in patients across various stages of bariatric surgery: a comparison of the merits of the theory of reasoned action versus the theory of planned behavior. Behavior Modification. 2009;33:795–817. doi: 10.1177/0145445509348055. [DOI] [PubMed] [Google Scholar]
- Jackson, Smith & Conner (2003).Jackson C, Smith RA, Conner M. Applying an extended version of the theory of planned behaviour to physical activity. Journal of Sports Sciences. 2003;21:119–133. doi: 10.1080/0264041031000070976. [DOI] [PubMed] [Google Scholar]
- Jepsen et al. (2013).Jepsen R, Aadland E, Andersen JR, Natvig GK. Associations between physical activity and quality of life outcomes in adults with severe obesity: a cross-sectional study prior to the beginning of a lifestyle intervention. Health and Quality of Life Outcomes. 2013;11:187. doi: 10.1186/1477-7525-11-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson et al. (2013).Johnson LK, Andersen LF, Hofso D, Aasheim ET, Holven KB, Sandbu R, Roislien J, Hjelmesaeth J. Dietary changes in obese patients undergoing gastric bypass or lifestyle intervention: a clinical trial. British Journal of Nutrition. 2013;110:127–134. doi: 10.1017/S0007114512004631. [DOI] [PubMed] [Google Scholar]
- Karlsen et al. (2013).Karlsen TI, Lund RS, Roislien J, Tonstad S, Natvig GK, Sandbu R, Hjelmesaeth J. Health related quality of life after gastric bypass or intensive lifestyle intervention: a controlled clinical study. Health and Quality of Life Outcomes. 2013;11:17. doi: 10.1186/1477-7525-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsen, Sohagen & Hjelmesaeth (2013).Karlsen TI, Sohagen M, Hjelmesaeth J. Predictors of weight loss after an intensive lifestyle intervention program in obese patients: a 1-year prospective cohort study. Health and Quality of Life Outcomes. 2013;11:165. doi: 10.1186/1477-7525-11-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay & Fiatarone Singh (2006).Kay SJ, Fiatarone Singh MA. The influence of physical activity on abdominal fat: a systematic review of the literature. Obesity Reviews. 2006;7:183–200. doi: 10.1111/j.1467-789X.2006.00250.x. [DOI] [PubMed] [Google Scholar]
- Kirk et al. (2012).Kirk SF, Penney TL, McHugh TL, Sharma AM. Effective weight management practice: a review of the lifestyle intervention evidence. International Journal of Obesity. 2012;36:178–185. doi: 10.1038/ijo.2011.80. [DOI] [PubMed] [Google Scholar]
- Kissler & Settmacher (2013).Kissler HJ, Settmacher U. Bariatric surgery to treat obesity. Seminars in Nephrology. 2013;33:75–89. doi: 10.1016/j.semnephrol.2012.12.004. [DOI] [PubMed] [Google Scholar]
- Lee et al. (2005).Lee S, Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Graham TE, Ross R. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without Type 2 diabetes. Journal of Applied Physiology. 2005;99:1220–1225. doi: 10.1152/japplphysiol.00053.2005. [DOI] [PubMed] [Google Scholar]
- Lerdal et al. (2011).Lerdal A, Andenaes R, Bjornsborg E, Bonsaksen T, Borge L, Christiansen B, Eide H, Hvinden K, Fagermoen MS. Personal factors associated with health-related quality of life in persons with morbid obesity on treatment waiting lists in Norway. Quality of Life Research. 2011;20:1187–1196. doi: 10.1007/s11136-011-9865-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorentzen, Ommundsen & Holme (2007).Lorentzen C, Ommundsen Y, Holme I. Psychosocial correlates of stages of change in physical activity in an adult community sample. European Journal of Sport Science. 2007;7:93–106. doi: 10.1080/17461390701456122. [DOI] [Google Scholar]
- Midthjell et al. (2013).Midthjell K, Lee CM, Langhammer A, Krokstad S, Holmen TL, Hveem K, Colagiuri S, Holmen J. Trends in overweight and obesity over 22 years in a large adult population: the HUNT Study, Norway. Clinical Obesity. 2013;3:12–20. doi: 10.1111/cob.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman & Smith (1995).Norman P, Smith L. The theory of planned behavior and exercise: an investigation into the role of prior behavior, behavioral intentions and attitude variability. European Journal of Social Psychology. 1995;25:403–415. doi: 10.1002/ejsp.2420250405. [DOI] [Google Scholar]
- Norwegian Directorate of Health (2009).Norwegian Directorate of Health . Sykelig overvekt: prioriteringsveileder. Oslo: Norwegian Directorate of Health; 2009. [Google Scholar]
- Olander et al. (2013).Olander EK, Fletcher H, Williams S, Atkinson L, Turner A, French DP. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: a systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity. 2013;10:29. doi: 10.1186/1479-5868-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orme et al. (2014).Orme M, Wijndaele K, Sharp SJ, Westgate K, Ekelund U, Brage S. Combined influence of epoch length, cut-point and bout duration on accelerometry-derived physical activity. International Journal of Behavioral Nutrition and Physical Activity. 2014;11:34. doi: 10.1186/1479-5868-11-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plotnikoff et al. (2013).Plotnikoff RC, Lubans DR, Costigan SA, McCargar L. A test of the theory of planned behavior to predict physical activity in an overweight/obese population sample of adolescents from Alberta, Canada. Health Education and Behavior. 2013;40:415–425. doi: 10.1177/1090198112455642. [DOI] [PubMed] [Google Scholar]
- Prince et al. (2008).Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw et al. (2005).Shaw K, O’Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database of Systematic Reviews. 2005:CD003818. doi: 10.1002/14651858.CD003818.pub2. [DOI] [PubMed] [Google Scholar]
- Sirard et al. (2011).Sirard JR, Forsyth A, Oakes JM, Schmitz KH. Accelerometer test-retest reliability by data processing algorithms: results from the Twin Cities Walking Study. Journal of Physical Activity & Health. 2011;8:668–674. doi: 10.1123/jpah.8.5.668. [DOI] [PubMed] [Google Scholar]
- Sparks, Guthrie & Shepherd (1997).Sparks P, Guthrie CA, Shepherd R. The dimensional structure of the perceived behavioral control construct. Journal of Applied Social Psychology. 1997;27:418–438. doi: 10.1111/j.1559-1816.1997.tb00639.x. [DOI] [Google Scholar]
- Sturm (2007).Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121:492–496. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinburn et al. (2011).Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- Tate et al. (2007).Tate DF, Jeffery RW, Sherwood NE, Wing RR. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? American Journal of Clinical Nutrition. 2007;85:954–959. doi: 10.1093/ajcn/85.4.954. [DOI] [PubMed] [Google Scholar]
- Trost, McIver & Pate (2005).Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Medicine and Science in Sports and Exercise. 2005;37:S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- Tsigos et al. (2008).Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, Zahorska-Markiewicz B, Obesity Management Task Force of the European Association for the Study of Obesity Management of obesity in adults: European clinical practice guidelines. Obesity Facts. 2008;1:106–116. doi: 10.1159/000126822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke et al. (2010).Tudor-Locke C, Brashear MM, Johnson WD, Katzmarzyk PT. Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese U.S. men and women. International Journal of Behavioral Nutrition and Physical Activity. 2010;7:60. doi: 10.1186/1479-5868-7-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twisk (2003).Twisk JWR. Applied longitudinal data analysis for epidemiology: a practical guide. Cambridge: Cambridge University Press; 2003. [Google Scholar]
- van Nunen et al. (2007).van Nunen AM, Wouters EJ, Vingerhoets AJ, Hox JJ, Geenen R. The health-related quality of life of obese persons seeking or not seeking surgical or non-surgical treatment: a meta-analysis. Obesity Surgery. 2007;17:1357–1366. doi: 10.1007/s11695-007-9241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbroucke et al. (2007).Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, Strobe Initiative Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Medicine. 2007;4:e505. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartanian & Shaprow (2008).Vartanian LR, Shaprow JG. Effects of weight stigma on exercise motivation and behavior: a preliminary investigation among college-aged females. Journal of Health Psychology. 2008;13:131–138. doi: 10.1177/1359105307084318. [DOI] [PubMed] [Google Scholar]
- Venditti et al. (2014).Venditti EM, Wylie-Rosett J, Delahanty LM, Mele L, Hoskin MA, Edelstein SL, Diabetes Prevention Program Research Group Short and long-term lifestyle coaching approaches used to address diverse participant barriers to weight loss and physical activity adherence. International Journal of Behavioral Nutrition and Physical Activity. 2014;11:16. doi: 10.1186/1479-5868-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren et al. (2010).Warren JM, Ekelund U, Besson H, Mezzani A, Geladas N, Vanhees L, Experts Panel Assessment of physical activity—a review of methodologies with reference to epidemiological research: a report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. European Journal of Preventive Cardiology. 2010;17:127–139. doi: 10.1097/HJR.0b013e32832ed875. [DOI] [PubMed] [Google Scholar]
- Wiklund, Olsén & Willén (2011).Wiklund M, Olsén MF, Willén C. Physical activity as viewed by adults with severe obesity, awaiting gastric bypass surgery. Physiotherapy Research International. 2011;16:179–186. doi: 10.1002/pri.497. [DOI] [PubMed] [Google Scholar]


