Abstract
Context:
Postural stability assessment is included as part of the diagnostic and monitoring process for sports-related concussions. Particularly, the relatively simple Balance Error Scoring System (BESS) and more sophisticated force plate measures like the Sensory Organization Test (SOT) are suggested.
Evidence Acquisition:
Relevant studies were identified via the following electronic databases: PubMed, MEDLINE, EMBASE, Web of Science, ScienceDirect, and CINAHL (1980 to July 2013). Inclusion was based on the evaluation of postural sway or balance in concussed athletes of any age or sex and investigating the reliability or validity of the included tests.
Study Design:
Clinical review.
Level of Evidence:
Level 4
Results:
Both the SOT and the BESS show moderate reliability, but a learning effect due to repetitive testing needs to be considered. Both tests indicate that postural stability returns to baseline by day 3 to 5 in most concussed athletes. While the BESS is a simple and valid method, it is sensitive to subjectivity in scoring and the learning effect. The SOT is very sensitive to even subtle changes in postural sway, and thus, more accurate than the BESS; however, it is a rather expensive method of balance testing.
Conclusion:
Both tests serve the purpose of monitoring balance performance in the concussed athlete; however, neither may serve as a stand-alone diagnostic or monitoring tool.
Strength of Recommendation Taxonomy:
B
Keywords: concussion, sports, balance, Balance Error Scoring System, Sensory Organization Test
As concussion awareness and diagnosis has changed significantly, there is wide variability in the literature on the epidemiology of concussion. The incidence of sports-related concussion in high school and collegiate athletes is 0.28 per 1000 athlete-exposures, or 5% of the total number of injuries across different sports.11,24 This equates to 1.6 to 3.8 million concussions annually in the United States alone.26
Despite this already alarming number, there is growing concern that concussion may be underreported in sports.2,31 Apart from athletes failing to report a concussion for various reasons,31 team physicians may employ too high thresholds for44 or simply miss the diagnosis.
A fast and accurate diagnosis of concussion is important, particularly in light of potential long-term neurological deficits originating from head trauma,8,52 and various test batteries have been presented and refined over the years.28,32,34 In addition, postural stability assessment has been included in the diagnostic and monitoring process, as many concussed athletes present with balance impairments.22
Postural control requires a complex interaction of musculoskeletal and neural systems.45 The neural components that contribute essentially to postural stability include motor processes organizing neuromuscular synergies; sensory/perceptional processes that organize and integrate visual, vestibular, and somatosensory systems; and higher level processes essential for mapping sensation to action.47 Recommended balance tests challenge the balance system with postural tasks of varying difficulty, including the modification of sensory input, unstable/moving surfaces, or single-leg stance to quantify any concussion-induced impairment.
Since 2001, the International Consensus Conference on Concussion in Sports has issued recommendations, which were updated and revised by the 2012 Zurich Consensus Statement,34 and the American Medical Society for Sports Medicine has provided evidence-based best-practice recommendations in the evaluation and management of sports-related concussions.23 These statements recommend balance testing to diagnose and monitor concussion. Specifically, a modified version of the Balance Error Scoring System (BESS) is included in the Sideline Concussion Assessment Tool (SCAT3) as part of the sideline assessment. The Sensory Organization Test (SOT) is another test based on force plate measurements to detect and monitor balance impairments following concussion.39
Methods
Balance Error Scoring System
The BESS is an inexpensive, noninstrumented, clinical tool for assessing balance. The test consists of 6 separate 20-second balance tests performed under 3 stance conditions (double-leg, single-leg, and tandem stance) on 2 different surfaces (firm and compliant).1 For the single-leg stance, the nondominant leg is selected. This test is easy to administer and takes approximately 5 minutes.41
The BESS test score is recorded as a quantitative measurement that equals the total number of errors committed by the athlete during the tests. A higher score indicates a more severe postural instability. Error points are given when the athlete is opening the eyes; stepping, stumbling, or falling from the original test position; removing the hands from his or her hips; moving the hip into more than 30° of flexion or abduction; lifting the toes or heels from the test surface; or remaining out of the test position for more than 5 seconds.41 Because of the number of tests and surfaces, the number of possible error points ranges from 0 to 60 and is expressed as a cumulative score.
A modified (simplified) on-field screening version of the BESS, which omits the 3 tests completed on foam, is included in the SCAT3. Accordingly, the maximum error score is 30.34
Sensory Organization Test
Developed by Nashner and Peters,36 the SOT is the most commonly used technical balance test in concussion research. It was designed to systematically disrupt the sensory selection process while a force plate measures vertical ground reaction forces produced by the body’s center of pressure (COP) during involuntary sway. While other approaches have been used in past and recent studies,16,19 the SOT remains the most established test, and new approaches to analyze the results have been proposed.9
Three 20-second trials each are performed under 6 different sensory conditions of increasing difficulty (18 measurements total) that manipulate the information received from the somatosensory, visual, and vestibular systems.21 Measurements are conducted (1) with eyes open, firm surface; (2) eyes closed, firm surface; (3) sway referenced visual surround, firm surface; (4) sway referenced support surface, eyes open; (5) sway referenced support surface, eyes closed; and (6) sway referenced visual and support surface.39 A percentage score is calculated for each trial, including ratios based on the ability to use visual, vestibular, and somatosensory pathways and a composite score to determine overall postural stability.38 Computer-generated equilibrium scores range between 100 (no postural sway at all) and 0 (representing a fall).39
The major advantage of force plate measures in general is the objectivity and precision in quantifying and describing the sway path of the athlete, which potentially allows the detection of balance impairments for twice as long as the BESS. The aspect of objectivity may be especially important in elite sports, where flawless documentation is essential when justifying return-to-play decisions. The downside of the SOT is the limited clinical availability, as the required complex instrumentation does not allow an easy transfer of the tests to other force plate systems available.
Search Strategy
A comprehensive and systematic literature search strategy was developed by identifying all potentially relevant search terms, categorizing these terms into specific search phases, and subsequently combining them by using Boolean terms (concussion, mild traumatic brain injury, mTBI, balance, postural sway, sensory organization test, SOT, balance error scoring system, BESS). This search strategy was applied to different electronic databases: PubMed, MEDLINE, EMBASE, Web of Science, ScienceDirect, and CINAHL (1980 to June 2013). The inclusion criteria were (1) studies that were fully or partially concerned with the analysis of postural sway or balance in concussed athletes of any age and sex and (2) studies investigating the reliability and validity of the included balance tests.
Occasionally, mild traumatic brain injury (mTBI) and concussion are used interchangeably in the literature, although these 2 terms refer to different injury constructs.33 To not miss potentially relevant studies, the terms mild traumatic brain injury and mTBI were included in the literature search.
Initially, the online search strategy identified 114 studies, of which abstracts were screened individually and independently by the reviewers. The application of inclusion criteria eliminated 84 papers. Seven studies met the inclusion criteria for the postural sway assessment, while another 24 dealt with aspects of reliability or validity and were included in this review.
Results
Balance Error Scoring System
Reliability and Validity
Only 3 studies applied the BESS to investigate postural sway following concussion, all of which included collegiate athletes of similar age but engaged in different sports (Table 1).21,30,42 For most college-aged athletes, error scores return to preseason baseline levels by day 3 to 5 postconcussion (Figure 1). More errors were observed during the more challenging tasks on the foam surface, and these error scores returned to baseline by day 5.42 However, results may vary in juvenile or older individuals.
Table 1.
Postural stability in concussed athletes: Balance Error Scoring System
| Participants |
||||||
|---|---|---|---|---|---|---|
| Concussed |
Controls |
|||||
| Study | Sport | Competitive Level | Sex (Age,a y) | No. | Sex (Age,a y) | No. |
| McCrea et al30 | Football | Collegiate, Divisions I, II, and III | Male (20.0 ± 1.4)b | 94 | Male (20.0 ± 1.4)b | 56 |
| Riemann et al41 | Unclear | Collegiate | Mixed (19.2 ± 2.3) | 16: 15 males, 1 female | — | — |
| Guskiewicz et al21 | Various | Collegiate, Division I | Mixed (19.5 ± 1.3) | 72: 50 males, 22 females | Mixed (20.0 ± 2.4) | 36: 25 males, 11 females |
The age in years is expressed as mean ± standard deviation.
Combined age for both concussed and control group.
Figure 1.
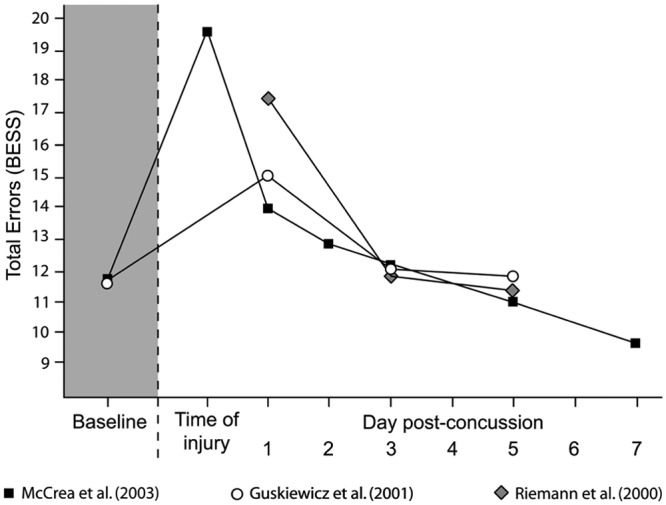
Mean Balance Error Scoring System (BESS) error score at baseline and following concussion.
Four studies investigated the intrarater reliability by means of the intraclass correlation coefficient (ICC).14,25,49,51 Only 1 study included collegiate athletes (mean age, 21.3 ± 2.7 years),49 the results of which integrate best in the age range of studies investigating postural sway following concussion (Table 1). In contrast, the other 3 studies included high school athletes25,51 or did not provide any demographic information.14
Overall, the BESS shows moderate overall test-retest reliability (ICC, 0.50-0.75), irrespective of who conducts the test and whether it is on the same occasion or at different times (Appendix 1, available at http://sph.sagepub.com/content/suppl).7,14,25,41,49,51
As may be expected for a clinical test with rather subjective error scoring, the interpretation of results is complicated by studies showing conflicting data (Appendix 1).
Depending on the severity of neurological impairment and the associated clinical symptoms, the clinician may expect an increase of 6 to 20 error points immediately following injury. At day 1, this drops by 2 to 3 error points, further decreasing by another 1 to 2 error points at day 3 (Figure 1).21,29,30,42 The threshold at which a BESS score represents a significant change compared with baseline as opposed to a measurement error is around 7 points (when conducted by the same clinician) or around 9 error points (when conducted by various examiners).14 In contrast, an increase of ≥3 error points represented a significant change indicative of concussion-related balance impairments.51
Broglio et al7 observed learning effects with repetitive testing in a group of 48 young adults and found that improvements of 3 to 4 error points may be expected for 3 repetitions over a 5-day period. Mulligan et al35 recorded 2 to 5 fewer error points at a 2-week follow-up, while 20% showed a learned response exceeding 7 points. This renders the clinical use of the BESS for such individuals highly questionable. To avoid any overinterpretation of the error scores, multiple baseline testing may help to alleviate these learned responses. For this purpose, Broglio et al7 recommend averaging 3 consecutive repetitions7 at any occasion, which may also reduce the measurement error at the same time. While there is no accepted recommendation, previous studies performed follow-up testing at days 1, 3, 5, and 7 postconcussion, which may offer good insight into the athlete’s recovery.21,29,30,42
Sensory Organization Test
Reliability and Validity
Five studies investigated postural sway following concussion using the SOT, 4 of which enrolled collegiate athletes involved in different sports (Table 2).5,20,21,39,42
Table 2.
Postural stability in concussed athletes: Sensory Organization Test
| Participants |
||||||
|---|---|---|---|---|---|---|
| Concussed |
Controls |
|||||
| Study | Sport | Competitive level | Sex (Age,a y) | No. | Sex (Age, y) | No. |
| Gusciewicz et al20 | Unclear | Collegiate, Division I | Mixed (18.6 ± 2.0) | 11: 8 males, 3 females | Mixed (20.2 ± 1.3) | 11: 8 males, 3 females |
| Riemann et al41 | Unclear | Collegiate | Mixed (19.2 ± 2.3) | 16: 15 males, 1 female | — | — |
| Gusciewicz et al21 | Various | Collegiate, Division I | Mixed (19.5 ± 1.3) | 72: 50 males, 22 females | Mixed (20.0 ± 2.4) | 36 (“sex matched”) |
| Peterson et al39 | Mixed, mostly football | Collegiate, Division I | Mixed (19.3 ± 1.3) | 24: 18 males, 6 females | Unclear (20.2 ± 1.6) | 18 |
| Broglio et al5 | Mixed, mostly football | Unclear | Mixed (unclear) | 75 | — | — |
The age in years is expressed as mean ± standard deviation.
Most research utilizing the SOT has identified deficits lasting an average of 3 to 5 days postconcussion,5,20,21,39,42 but the test may be capable of demonstrating impaired balance for up to 10 days (Figure 2).20,39 However, Broglio et al5 observed that in 75 concussed athletes, nearly 40% did not show decreased balance.
Figure 2.
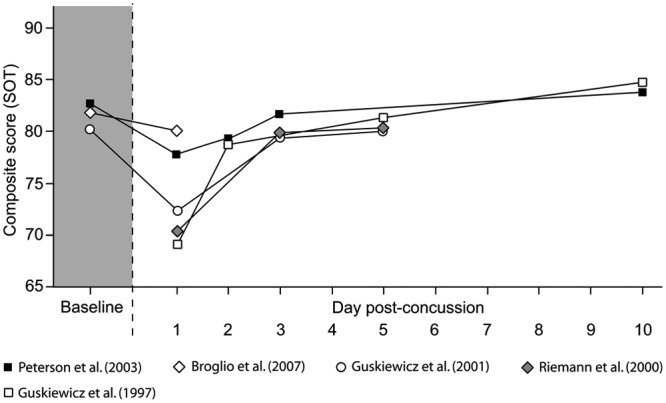
Mean Sensory organization Test (SOT) composite scores at baseline and following concussion.
The SOT shows moderate overall reliability with greatly varying results for the 6 individual test conditions.4,13,15,27,40,50,53 Like the BESS, the SOT is not suitable as a stand-alone diagnostic tool for concussions, although it is very good at identifying those athletes without a concussion. The sensitivity increases with concussion severity.4
A change in composite balance score of 4 to 8 points compared with baseline may indicate a significant change in concussed athletes.5,20,46 Accounting for the reliability of the SOT, the clinician may want to look for changes of around 7 points in the athlete’s composite ratio. The corresponding individual values for somatosensory, visual, and vestibular ratios are 7, 6, and 17, respectively (Appendix 2, available at http://sph.sagepub.com/content/suppl).4
At postinjury day 1, 40% of concussed athletes showed impaired postural stability, as expressed by the composite score, whereby the somatosensory ratio was affected in 40% and the visual ratio in 30%. The vestibular system was impaired in just more than 20%.5 In contrast to the BESS, where about 35% of concussed individuals were identified as showing postural abnormalities,29 the SOT demonstrated impaired balance in at least 1 test component in more than 60% of affected athletes.5
As with the BESS, learning effects have also been observed with repetitive SOT testing53 and may correspond to a 10% improvement in balance composite scores.21,39 Wrisley et al53 showed that this effect reaches a plateau after 3 to 4 repetitions in healthy, young individuals. Consequently, 3 repetitions of the full SOT sequence (18 trials each) may be advisable within a few days to establish baseline values. Postconcussion measurements can then be compared with these results, whereby a single-session improvement of 8 points may be indicative of recovery, taking into account the expected learning effects.53
Discussion
Balance is only 1 aspect of assessing the concussed athlete, and its impairment may not always be present.18 As one of few objective measures, balance testing plays a role in a multifaceted approach in diagnosing and managing sports-related concussion.17
Clinicians need to be aware of the clinical and practical applications and limitations in using either clinical or force plate balance tests.
Balance Error Scoring System
While the BESS is a valid clinical balance test,41 it is unsuitable in isolation to identify concussed athletes both at the time of injury and at follow-up.29 In the light of conflicting results, error scores may only be of clinical value at the time of injury. However, conflicting data originate from calculations depending on the reliability of the BESS, which may be affected by scoring variability and differences in foam thickness and resistance. Therefore, averaging several tests may allow more confidence in any observed differences, as reliability generally increases with the number of repetitions.
It is difficult to determine a clinically (and statistically) significant difference when compared with baseline values given the issues of the learning effects and the measurement errors, which render the BESS a less reliable clinical test. A return to baseline values may therefore not necessarily mean a full recovery. Also, because of the expected learning response, failure to improve at follow-up may be indicative of concussion-related impairments.
Normative values of 11 errors7 to 19 errors49 have been reported for college-aged individuals. This great variation between studies enrolling otherwise similar participants underlines the difficulty with subjective scoring. It remains questionable whether normative values can replace baseline testing, especially in an athlete population where significant individual differences are observed between sports.3 Also, sex differences have to be considered,10 whereby males score worse than females do.51 Accordingly, we recommend that repetitive individual tests at baseline should be performed.
The scoring system of the BESS appears to be rather simple. However, it may account for the moderate interrater (and probably also intrarater) reliability. Accurately visually assessing when hip abduction or flexion exceeds 30° or whether the forefoot or heel is lifted, particularly on a foam surface, requires practice.14 To overcome this issue of subjective rating, assessing sway data of the BESS conducted on any force plate may be an option worth exploring.
Practical Considerations
Using the BESS (modified or original) as a sideline test may also encounter several practical issues depending on how baseline values were established. Wearing of protective equipment by players often renders the test impractical as a quick screening tool because the gear may modify the athlete’s ability to maintain static balance. Athletic tape or ankle braces may also require removal.6
Athletes tend to score significantly worse on sideline assessment because of external distractions. In 21 healthy collegiate athletes, 11.0 ± 6.6 and 14.3 ± 5.7 errors were reported in a locker room and at the sideline, respectively.37 Therefore, BESS baseline values should be obtained in the environment in which injury testing will most likely be conducted.37
The athlete’s level of exhaustion must be considered when comparing sideline data with baseline values.49 If baseline testing was performed when the athlete is well rested, the results can be expected to deviate from those obtained in the middle of a game or practice. This effect may last 20 minutes postexercise.49
Sensory Organization Test
Reported normative composite scores for college-aged athletes range from 80 (Schmidt et al46) to 92 (Sosnoff et al48). As Sosnoff et al48 enrolled the highest number of participants (n = 224), the latter value may more accurately reflect the mean baseline performance. Despite strong theoretical rationale for using individual baseline measures for comparison postinjury, normative values may be acceptable.46
Pain affects postural stability.12,43 Since subtle changes in body sway are registered, pain may influence the force plate measures more than a clinical balance test like the BESS.
Conclusion
There is an easy, low-cost, and quick-to-administer sideline balance test (BESS), with the weakness of subjective scoring. The expensive but objective force plate systems (SOT) have limited mobility. Both tests show moderate reliability and learning effects due to repetitive testing. Both suggest that postural stability returns to baseline by day 3 to day 5 in most concussed college-aged athletes. Because of the subjectivity in scoring, the learning effect, and the moderate reliability in the BESS, it is unclear what constitutes a relevant and reliable change in error scores after injury. The SOT is more objective and quantitates subtle changes in postural stability. The detection rate for some form of postconcussion postural impairment is nearly twice with SOT. However, its complexity and limited mobility renders it less attractive to the field clinician.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Bell DR, Guskiewicz KM, Clark MA, Padua DA. Systematic review of the balance error scoring system. Sports Health. 2011;3:287-295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Benson BW, Meeuwisse WH, Rizos J, Kang J, Burke CJ. A prospective study of concussions among National Hockey League players during regular season games: the NHL-NHLPA Concussion Program. CMAJ. 2011;183:905-911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bressel E, Yonker JC, Kras J, Heath EM. Comparison of static and dynamic balance in female collegiate soccer, basketball, and gymnastics athletes. J Athl Train. 2007;42:42-46 [PMC free article] [PubMed] [Google Scholar]
- 4. Broglio SP, Ferrara MS, Sopiarz K, Kelly MS. Reliable change of the sensory organization test. Clin J Sport Med. 2008;18:148-154 [DOI] [PubMed] [Google Scholar]
- 5. Broglio SP, Macciocchi SN, Ferrara MS. Sensitivity of the concussion assessment battery. Neurosurgery. 2007;60:1050-1057 [DOI] [PubMed] [Google Scholar]
- 6. Broglio SP, Monk A, Sopiarz K, Cooper ER. The influence of ankle support on postural control. J Sci Med Sport. 2009;12:388-392 [DOI] [PubMed] [Google Scholar]
- 7. Broglio SP, Zhu W, Sopiarz K, Park Y. Generalizability theory analysis of balance error scoring system reliability in healthy young adults. J Athl Train. 2009;44:497-502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(43 suppl):84-105 [DOI] [PubMed] [Google Scholar]
- 9. Cavanaugh JT, Guskiewicz KM, Giuliani C, Marshall S, Mercer VS, Stergiou N. Recovery of postural control after cerebral concussion: new insights using approximate entropy. J Athl Train. 2006;41:305-313 [PMC free article] [PubMed] [Google Scholar]
- 10. Covassin T, Elbin RJ, Harris W, Parker T, Kontos A. The role of age and sex in symptoms, neurocognitive performance, and postural stability in athletes after concussion. Am J Sports Med. 2012;40:1303-1312 [DOI] [PubMed] [Google Scholar]
- 11. Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med. 2012;30:1-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. della Volpe R, Popa T, Ginanneschi F, Spidalieri R, Mazzocchio R, Rossi A. Changes in coordination of postural control during dynamic stance in chronic low back pain patients. Gait Posture. 2006;24:349-355 [DOI] [PubMed] [Google Scholar]
- 13. Dickin DC, Clark S. Generalizability of the sensory organization test in college-aged males: obtaining a reliable performance measure. Clin J Sport Med. 2007;17:109-115 [DOI] [PubMed] [Google Scholar]
- 14. Finnoff JT, Peterson VJ, Hollman JH, Smith J. Intrarater and interrater reliability of the Balance Error Scoring System (BESS). PM R. 2009;1:50-54 [DOI] [PubMed] [Google Scholar]
- 15. Ford-Smith CD, Wyman JF, Elswick RK, Jr, Fernandez T, Newton RA. Test-retest reliability of the sensory organization test in noninstitutionalized older adults. Arch Phys Med Rehabil. 1995;76:77-81 [DOI] [PubMed] [Google Scholar]
- 16. Gao J, Hu J, Buckley T, White K, Hass C. Shannon and Renyi entropies to classify effects of mild traumatic brain injury on postural sway. PLoS One. 2011;6(9):e24446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guskiewicz KM. Postural stability assessment following concussion: one piece of the puzzle. Clin J Sport Med. 2001;11:182-189 [DOI] [PubMed] [Google Scholar]
- 18. Guskiewicz KM. Balance assessment in the management of sport-related concussion. Clin Sports Med. 2011;30:89-102 [DOI] [PubMed] [Google Scholar]
- 19. Guskiewicz KM, Perrin DH, Gansneder BM. Effect of mild head injury on postural stability in athletes. J Athl Train. 1996;31:300-306 [PMC free article] [PubMed] [Google Scholar]
- 20. Guskiewicz KM, Riemann BL, Perrin DH, Nashner LM. Alternative approaches to the assessment of mild head injury in athletes. Med Sci Sports Exerc. 1997;29(suppl):S213-S221 [DOI] [PubMed] [Google Scholar]
- 21. Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36:263-273 [PMC free article] [PubMed] [Google Scholar]
- 22. Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643-650 [DOI] [PubMed] [Google Scholar]
- 23. Harmon KG, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Clin J Sport Med. 2013;23:1-18 [DOI] [PubMed] [Google Scholar]
- 24. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311-319 [PMC free article] [PubMed] [Google Scholar]
- 25. Hunt TN, Ferrara MS, Bornstein RA, Baumgartner TA. The reliability of the modified Balance Error Scoring System. Clin J Sport Med. 2009;19:471-475 [DOI] [PubMed] [Google Scholar]
- 26. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375-378 [DOI] [PubMed] [Google Scholar]
- 27. Leitner C, Mair P, Paul B, et al. Reliability of posturographic measurements in the assessment of impaired sensorimotor function in chronic low back pain. J Electromyogr Kinesiol. 2009;19:380-390 [DOI] [PubMed] [Google Scholar]
- 28. Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13(2):9-26 [DOI] [PubMed] [Google Scholar]
- 29. McCrea M, Barr WB, Guskiewicz K, et al. Standard regression-based methods for measuring recovery after sport-related concussion. J Int Neuropsychol Soc. 2005;11:58-69 [DOI] [PubMed] [Google Scholar]
- 30. McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290:2556-2563 [DOI] [PubMed] [Google Scholar]
- 31. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14:13-17 [DOI] [PubMed] [Google Scholar]
- 32. McCrea M, Kelly JP, Randolph C. The Standardized Assessment of Concussion: Manual for Administration, Scoring and Interpretation. 2nd ed. Waukesha, WI: CNS; 2000 [Google Scholar]
- 33. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Br J Sports Med. 2009;43(suppl 1):i76-i90 [DOI] [PubMed] [Google Scholar]
- 34. McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47:250-258 [DOI] [PubMed] [Google Scholar]
- 35. Mulligan IJ, Boland MA, McIlhenny CV. The balance error scoring system learned response among young adults. Sports Health. 2013;5:22-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nashner LM, Peters JF. Dynamic posturography in the diagnosis and management of dizziness and balance disorders. Neurol Clin. 1990;8:331-349 [PubMed] [Google Scholar]
- 37. Onate JA, Beck BC, Van Lunen BL. On-field testing environment and balance error scoring system performance during preseason screening of healthy collegiate baseball players. J Athl Train. 2007;42:446-451 [PMC free article] [PubMed] [Google Scholar]
- 38. Parsons TD, Notebaert AJ, Shields EW, Guskiewicz KM. Application of reliable change indices to computerized neuropsychological measures of concussion. Int J Neurosci. 2009;119:492-507 [DOI] [PubMed] [Google Scholar]
- 39. Peterson CL, Ferrara MS, Mrazik M, Piland S, Elliott R. Evaluation of neuropsychological domain scores and postural stability following cerebral concussion in sports. Clin J Sport Med. 2003;13:230-237 [DOI] [PubMed] [Google Scholar]
- 40. Register-Mihalik JK, Guskiewicz KM, Mihalik JP, Schmidt JD, Kerr ZY, McCrea MA. Reliable change, sensitivity, and specificity of a multidimensional concussion assessment battery: implications for caution in clinical practice. J Head Trauma Rehabil. 2013;28:274-283 [DOI] [PubMed] [Google Scholar]
- 41. Riemann BL, Guskiewicz K, Shiels EW. Relationship between clinical and forceplate measures of postural stability. J Sports Rehabil. 1999;8:71-82 [Google Scholar]
- 42. Riemann BL, Guskiewicz KM. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000;35:19-25 [PMC free article] [PubMed] [Google Scholar]
- 43. Ruhe A, Fejer R, Walker B. Is there a relationship between pain intensity and postural sway in patients with non-specific low back pain? BMC Musculoskelet Disord. 2011;12:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ruhe A, Gaensslen A, Klein W, Hamade N. Basic knowledge on concussion in the German Ice Hockey League (DEL) [in German]. Sportverletzung Sportschaden. 2013;27:201-206 [DOI] [PubMed] [Google Scholar]
- 45. Saether R, Jorgensen L. Intra- and inter-observer reliability of the Trunk Impairment Scale for children with cerebral palsy. Res Dev Disabil. 2011;32:727-739 [DOI] [PubMed] [Google Scholar]
- 46. Schmidt JD, Register-Mihalik JK, Mihalik JP, Kerr ZY, Guskiewicz KM. Identifying impairments after concussion: normative data versus individualized baselines. Med Sci Sports Exerc. 2012;44:1621-1628 [DOI] [PubMed] [Google Scholar]
- 47. Shumway-Cook A, Woollacott MH. Normal postural control. In: Motor Control: Translating Reseach Into Clinical Practice. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:157-186 [Google Scholar]
- 48. Sosnoff JJ, Broglio SP, Shin S, Ferrara MS. Previous mild traumatic brain injury and postural-control dynamics. J Athl Train. 2011;46:85-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Susco TM, Valovich McLeod TC, Gansneder BM, Shultz SJ. Balance recovers within 20 minutes after exertion as measured by the Balance Error Scoring System. J Athl Train. 2004;39:241-246 [PMC free article] [PubMed] [Google Scholar]
- 50. Tsang WW, Wong VS, Fu SN, Hui-Chan CW. Tai Chi improves standing balance control under reduced or conflicting sensory conditions. Arch Phys Med Rehabil. 2004;85:129-137 [DOI] [PubMed] [Google Scholar]
- 51. Valovich McLeod TC, Leach C. Psychometric properties of self-report concussion scales and checklists. J Athl Train. 2006;47:221-223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Vanderploeg RD, Curtiss G, Belanger HG. Long-term neuropsychological outcomes following mild traumatic brain injury. J Int Neuropsychol Soc. 2005;11:228-236 [DOI] [PubMed] [Google Scholar]
- 53. Wrisley DM, Stephens MJ, Mosley S, Wojnowski A, Duffy J, Burkard R. Learning effects of repetitive administrations of the sensory organization test in healthy young adults. Arch Phys Med Rehabil. 2007;88:1049-1054 [DOI] [PubMed] [Google Scholar]