Abstract
Background
This study examined predictors associated with readmission to detoxification in a sample of adult Alaska Native patients admitted to inpatient alcohol detoxification. Even though Alaska Native people diagnosed with alcoholism have been identified as frequent utilizers of the health care system and at elevated risk of death, little is known about factors associated with readmission to detoxification for this group.
Methods
We sought to predict readmission using a retrospective cohort study. The sample included 383 adult Alaska Native patients admitted to an inpatient detoxification unit and diagnosed with alcohol withdrawal during 2006 and 2007. Cox proportional hazard modeling was used to estimate unadjusted and adjusted associations with time to readmission within one year.
Results
Forty-two percent of the patients were readmitted within one year. Global Assessment Functioning (GAF; Axis V in the multi-axial diagnostic system of the Diagnostic and Statistical Manual of Mental Disorders [DSM IV]) score measured at the time of intake was associated with readmission. A one point increase in the GAF score (HR = .96, 95% CL = .94, .99, P = .002) was associated with a four percent decrease in readmission. The results also indicated that the GAF mediated the relationship between readmission and: employment and housing status.
Conclusions
The GAF measures both illness severity and adaptive functioning, is part of standard behavioral health assessments, and is easy to score. Readmission rates potentially could be decreased by creating clinical protocols that account for differences in adaptive functioning and illness severity during detoxification treatment and aftercare.
Keywords: Readmission, Detoxification, Substance abuse treatment, Alaska Native People, American Indian
1. Introduction
Detoxification represents the initial step in patient preparation for long-term treatment or rehabilitation (Hayashida, 1998). It is intended to manage acute intoxication and withdrawal and is distinct from substance abuse treatment (Miller and Kipnis, 2006). The Center for Substance Abuse Treatment defined detoxification as having three objectives: evaluation, stabilization and advocation of patient entry into substance abuse treatment (Miller and Kipnis, 2006).
Although detoxification is the first step in long-term substance abuse treatment, few studies have focused specifically on factors associated with readmission to detoxification. Known predictors of substance abuse treatment outcomes have not predicted accurately detoxification outcomes. For example, sociodemographics (gender, age, living situation, ethnic background), psychopathology, and coping style – which often are associated with substance abuse treatment outcomes – have not been associated with detoxification treatment outcomes (Franken and Hendriks, 1999).
1.1. Review of literature
Rates of readmission to detoxification programs differ by time since discharge. Short term readmission rates range from 4% to 52% between one and six months post-discharge (Annis and Liban, 1979; Carrier et al., 2011; Li et al., 2008). Rates of readmission within one year range from 34% to 48% (Callaghan, 2003; Li et al., 2008; Mark et al., 2006; Ponzer et al., 2002). Longer term readmission (>2 years and ≤4 years) rates range from 32% to 61% (Booth and Blow, 1993; Callaghan et al., 2006; Ponzer et al., 2002; Tomasson and Vaglum, 1998).
Various predictors of readmission to detoxification have been reported and differ depending upon length of study. Predictors of short-term readmission (≤6 months) include discharged against medical advice (Li et al., 2008), homeless, urban residence, and fee-for-service Medicaid (Carrier et al., 2011). Three studies focused on readmission within one year (Callaghan, 2003; Li et al., 2008; Mark et al., 2006). Among Canadian Aboriginals previous history of detoxification and residential instability predicted readmission (Callaghan, 2003). In the second study, state of residence, gender, race, Medicaid eligibility, an index inpatient detoxification admission and follow-up treatment predicted readmission (Mark et al., 2006). In the most recent study, hepatitis C, polydrug use and those with a preferred primary substance of alcohol were more likely to be readmitted within one year (Li et al., 2008).
Factors predicting longer term readmission include agoraphobia/panic disorder, (Tomasson and Vaglum, 1998), unemployment, homelessness, failing to complete treatment (i.e., discharge nursing assessment indicated the patient did not complete their detoxification based on substances they used and recommended length of treatment, including the treating physician’s recommendation for length of stay), Aboriginal ethnicity, and alcohol as primary drug (Callaghan et al., 2006). Evidence suggests indicators of severe alcohol use also increases risk of readmission including heavy drinking, polysubstance use, a combination of sensation-seeking behavior with low platelet monoamine oxidase levels (Ponzer et al., 2002) and seizures (Booth and Blow, 1993; Worner, 1996). On the other hand, clinical case-management was associated with an increased use of rehabilitation services and a decrease in detoxification readmissions (McLellan et al., 2005).
1.2. Conceptual model of readmission/background
Fig. 1 displays the conceptual model that guided this study of readmission to alcohol detoxification. Concepts proposed in other models (Arbaje et al., 2008; Hasan et al., 2010; Solomon and Doll, 1979) were incorporated; however, our approach is based primarily on Sullivan’s (1989) work. The conceptual model has 6 components (demographic, access to care, social and environmental characteristics, clinical characteristics/health status, utilization of the health care system, and the health care system) each theorized as equally impacting readmission to detoxification. Constructs associated with each component of the conceptual model are listed within each box (see Fig. 1 and cited models for more details). Although we recognize the importance of the health care system for readmission, we were unable to study these indicators due to data limitations.
Fig. 1.
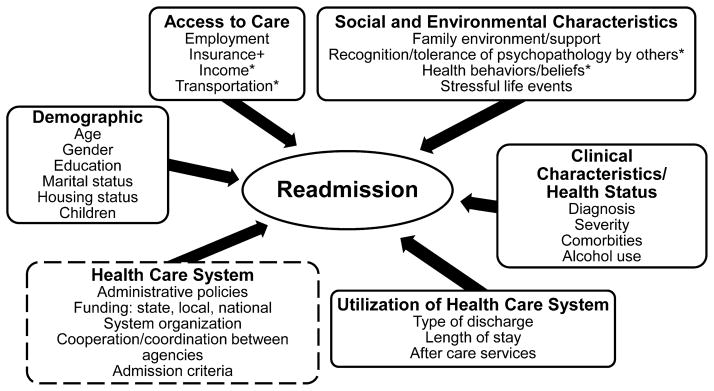
Conceptual model of readmission to detoxification. The conceptual model used to guide the study of readmission to detoxification has six distinct components. The Health Care System component within the dashed box was not studied as data were not available to measure these constructs. Similarly, those elements with an asterisk (*) were not studied due to unavailability of data. Insurance (+) was not studied as these services were funded by the Indian Health Service without regard to insurance status.
Alaska Native people comprise 14% (US Census Bureau, 2014) of the population in Alaska, yet they account for 47% of substance abuse treatment admissions (SAMHSA, 2012). Alcohol abuse is the 3rd leading cause of death for Alaska Native people aged 25–44; the death rate is 47 per 100,000 compared to 2 per 100,000 for US Caucasians (Day et al., 2011). Alaska Native people diagnosed with alcoholism are high utilizers (15+ visits in 1 year) of ambulatory services and at increased risk of death (Nighswander, 1984). Although service utilization by Alaska Native people diagnosed with alcohol dependence has been studied, to date no one has examined readmission to detoxification. Accordingly, we considered predictors of readmission to detoxification and hypothesized that unstable housing, a secondary drug diagnosis, not entering treatment after detoxification and withdrawal severity measured by seizures/delirium tremens and the GAF (global assessment functioning) would significantly increase the risk of readmission to detoxification. Based upon our conceptual model of readmission, we also explored the contribution of other key variables to readmission.
2. Methods
2.1. Study setting and design
Patients included in this study were treated in a tribally owned and managed 6 bed detoxification unit in Southcentral Alaska that served almost exclusively Alaska Native people and was funded by the Indian Health Service (IHS) and a small grant from the State of Alaska. The unit was part of comprehensive substance abuse treatment services that spanned a continuum of care including outreach, screening, assessment, brief intervention, detoxification, outpatient treatment, intermediate residential treatment and continuing care. The unit had one part-time physician’s assistant with medical doctor oversight, one registered nurse supervisor, one registered nurse, one licensed practical nurse or certified medical assistant or certified nursing assistant, one part-time pharmacist, one Bachelor of Arts counselor certified in substance abuse counseling and supervised by a Masters of Arts clinical supervisor. All staff received routine training and supervision on procedures for collection of patient information and documentation in the electronic medical record (EMR) including rating the GAF. Admission criteria was Alaska Native, adult and at risk of withdrawal requiring medical management. The unit recommended a length of stay (LOS) between 4 and 7 days. Patients who left prior to completion of their detoxification were ineligible to return for 30 days. Patients who completed their stay could return at any point after discharge. The unit prioritized treatment for pregnant women and intravenous drug users. The majority of patients were referred for treatment from the Alaska Native Medical Center (ANMC). Only one other detoxification facility specifically served Alaska Native people but was located several hundred miles away in a more rural setting. During the study period, the Salvation Army also provided detoxification services on an intermittent basis to all individuals within the catchment area. The human service organization that managed the detoxification unit was not directly connected to the ANMC but worked in partnership with it to deliver services.
The ANMC is jointly owned and managed by the Alaska Native Tribal Health Consortium (ANTHC) and Southcentral Foundation (SCF). The ANMC houses urgent, specialty and tertiary care and the only level II trauma center in Alaska (Alaska Native Tribal Health Consortium, 2013a,b; South Central Foundation, 2013). ANMC also houses primary care services operated by SCF serving Alaska Native people in the Anchorage, Matanuska-Susitna Valley and 55 rural villages within the Anchorage Service Unit (Southcentral Foundation, 2013). In Alaska 99% of IHS funds and programs are under tribal ownership and management. Their health care system is described as a system administered by Alaska Native people for Alaska Native people (Sherry, 2004). Health care delivery can be challenging. The distance from some communities to the nearest medical facility is over 800 miles (U.S. Department of Health and Human Services and Indian Health Services, 2007). Many Alaska Native villages are off the road system and accessible only by air, water, or snow vehicles.
This study employed a retrospective cohort design that included patients discharged from the detoxification unit between January 1, 2006 and December 31, 2007. Patients were followed for one year after discharge, with data available through the end of 2008. When multiple discharges and admissions existed for a patient only the first discharge date and the subsequent readmission were included in the analyses. The study cohort included adult (≤21) Alaska Native people with a primary diagnosis of alcohol withdrawal. During the study period, 419 adult patients were discharged from the unit; 18 were neither Alaska Native nor American Indian; 19 were admitted for a primary diagnosis of drug withdrawal (one met both exclusion criteria). This resulted in a final study population of 383.
2.2. Data sources
Data used in these analyses were collected at the detoxification unit by program staff during standard admission and discharge procedures and recorded in the EMR system. The unit employed quality control staff who notified providers of incomplete or discrepant information recorded in the EMR. Information was corrected by providers and reviewed again by quality control staff to ensure completeness. For this study, the data were extracted from the EMR and provided de-identified. The Alaska Native organization from which the data were obtained completed a thorough examination of the data to confirm it was de-identified to their criteria. Research approval was obtained from the Alaska Area Institutional Review Board (full board review) and the Colorado Multiple Institutional Review Board (certificate of exemption). Tribal review of this manuscript was completed by SCF and reviewed by the Alaska Native human service organization from which this data came.
2.3. Measures
2.3.1. Outcome variable
The outcome variable measured readmission within one year of discharge and had two components: whether the readmission occurred within one year (yes = 1/no = 0), and the time to the event (i.e., subsequent readmission). Time to event was a continuous variable operationalized as days between the first discharge date occurring in the study time period and the subsequent readmission occurring within one year. Individuals not readmitted within 365 days of discharge were censored.
2.3.2. Independent variables
See the supplemental material1 for a more detailed description of variables used in the analyses. Demographic characteristics included age, gender, education, number of children, marital status, and housing status. The only access to care variable studied was employment status. Social/environment characteristics included primary support problems, social environment problems, legal problems, and household composition.
Clinical characteristics/health status included a secondary drug diagnosis, number of mental health conditions, and number of physical health conditions. History of DTs/seizures and the GAF were used as measures of withdrawal severity. The GAF from Axis V of the multi-axial diagnostic system of the Diagnostic and Statistical Manual of Mental Disorders [DSM IV]) was collected at admission. It is a continuous score (0–100) representing the patient’s overall level of functioning and was assigned by the clinician based upon their assessment of the patient (American Psychiatric Association, 2000). The score is a single measure inclusive of both symptom severity and adaptive function that takes into account social, psychological, and occupational function but not physical or environmental impairment (American Psychiatric Association, 2000). A higher score indicates a greater level of functioning and less serious symptomatology, while a lower score indicates lower functioning and more serious symptomatology. Use-related behaviors consisted of the days alcohol was use in the 30 days prior to admission, age of first use and days abstinent prior to initiation of the patient’s last drinking episode, categorized as: 0–30, 31–60, 61–90 and 91+.
Health care utilization variables included detoxification completion status, length of stay, discharge destination, referral to treatment, and entry to treatment. Discharge destination was categorized into treatment and non-treatment. Treatment included discharges directly to medical care or substance abuse treatment facilities. Patients discharged to self-care or shelters were classified as non-treatment. Referral to treatment indicated the patient was referred to a treatment program upon discharge while entered treatment indicated that the unit confirmed patient admission into a treatment program after discharge.
2.4. Statistical methods
Descriptive statistics characterize all patients combined and stratified by readmission status. To compare the readmitted and not readmitted groups, t-tests were used for continuous variables and Chi-square or Fisher’s exact tests for categorical variables. Cox proportional hazard modeling estimated unadjusted and adjusted risk associations of each variable with time to readmission. Confounding was assessed in the multivariate model by a change in parameter estimates of at least 15 percent when compared to the full model (Bursac et al., 2008). Purposeful selection described by Bursac et al. (2008) was used for model building.
Initial multivariate models indicated potential mediation between the GAF and certain demographic characteristics. Mediation was evaluated post hoc by the commonly used criteria outlined in Baron and Kenny (1986). First, the association between a given independent variable and readmission was assessed. Second, the association between a given independent variable and the presumed mediating variable was assessed. Lastly, the relationship between the independent variable and readmission was assessed while controlling for the potential mediating variable (Baron and Kenny, 1986; MacKinnon et al., 2000). The Sobel test was used to confirm mediation effects (Preacher and Leonardelli, 2012; Sobel, 1982).
2.5. Missing data
Twenty-seven percent of the study cohort had data missing for one or more variables. A sensitivity analysis was conducted to compare patients with and without missing data. Patients who completed detoxification treatment, had a longer LOS, and problems with their social environment had less missing data (p-values ≤.01). Full information maximum likelihood (FIML) was therefore used to estimate the Cox proportional hazard model in order to address the moderate amount of missing data. SAS (SAS Institute Inc., 2011) and NCSS PASS (Hintze, 2005) were used to manage the data and calculate descriptive statistics, while MPlus (Muthén and Muthén, 1998–2011) was used to estimate the FIML Cox model.
3. Results
The readmission rate within one year was 42% and the average number of days to readmission was 131 (SD = 94 days, median = 105). Study cohort characteristics appear in Table 1. The average age was 43 years (SD = 10.35). Approximately half were male, high school educated, and single (never married). Forty-two percent had unstable housing; the average number of children was 2 (SD = 1.93). The average GAF score was 44 (SD = 8.89), indicating serious symptoms or serious impairment in social and occupational, or educational functioning (American Psychiatric Association, 2000). The average length of stay was 5 days (SD = 2.44). Slightly more than one-third were referred to treatment and 58% of those referred entered treatment. About half used alcohol every day during the month prior to admission; the average age at first use was 14.59 (SD = 4.75).
Table 1.
| Characteristics of patients readmitted and not readmitted
|
Cox proportional hazard
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Entire sample
|
Readmitted
|
Not readmitted
|
Unadjusted
|
||||||
| (n = 383)
|
(n = 162)
|
(n = 221)
|
Hazard | CL | P-value | ||||
| n | % | n | % | n | % | Ratio | |||
| Age (mean, sd) | 42.77 | 10.35 | 43.38 | 9.82 | 42.32 | 10.70 | 1.01 | .99, 1.02 | 0.45 |
| Gender | |||||||||
| Female | 165 | 43% | 65 | 40% | 100 | 45% | 1.00 | ||
| Male | 218 | 57% | 97 | 60% | 121 | 55% | 1.18 | .87, 1.62 | 0.29 |
| Education | |||||||||
| Less than high school | 97 | 25% | 42 | 26% | 54 | 24% | 1.06 | .73, 1.54 | 0.77 |
| High school education | 179 | 47% | 79 | 49% | 100 | 45% | 1.00 | ||
| More than high school | 107 | 28% | 41 | 25% | 67 | 30% | 0.87 | .60, 1.28 | 0.48 |
| Marital status | |||||||||
| Living as married | 65 | 17% | 21 | 13% | 44 | 20% | 0.67 | .42, 1.09 | 0.11 |
| Single never married | 173 | 45% | 75 | 46% | 98 | 44% | 1.00 | ||
| Divorced, separated, widowed | 145 | 38% | 66 | 41% | 79 | 36% | 1.02 | .73, 1.42 | 0.91 |
| Housing status | |||||||||
| Stable | 214 | 56% | 75 | 46% | 137 | 62% | 1.00 | ||
| Unstable | 169 | 44% | 87 | 54% | 84 | 38% | 1.65 | 1.22, 2.25 | 0.001 |
| Number of children (mean, sd) | 1.99 | 1.93 | 1.94 | 1.91 | 2.04 | 1.94 | 0.97 | .91, 1.04 | 0.49 |
| Employment status | |||||||||
| Employed | 61 | 16% | 17 | 11% | 44 | 20% | 0.51 | .30, .87 | 0.01 |
| Seasonal work | 15 | 4% | 11 | 5% | 6 | 3% | 1.25 | .68, 2.30 | 0.47 |
| Seeking employment | 163 | 42% | 76 | 47% | 85 | 38% | 1.00 | ||
| Not in labor force | 140 | 36% | 57 | 36% | 83 | 37% | 0.82 | .58, 1.14 | 0.24 |
| Other | 4 | 1% | 1 | 1% | 3 | 2% | 0.38 | .04, 3.42 | 0.39 |
| Primary support problems | 298 | 78% | 123 | 76% | 175 | 79% | 0.92 | .62, 1.38 | 0.70 |
| Social environment problems | 341 | 89% | 148 | 91% | 193 | 87% | 1.50 | .85, 2.65 | 0.16 |
| Legal problems | 65 | 17% | 29 | 18% | 38 | 17% | 1.07 | .70, 1.64 | 0.75 |
| Patient lives with | |||||||||
| Alone | 168 | 44% | 79 | 49% | 90 | 41% | 1.35 | .96, 1.91 | 0.09 |
| Family | 138 | 36% | 54 | 33% | 84 | 38% | 1.00 | ||
| Non-family | 77 | 20% | 29 | 18% | 47 | 21% | 0.99 | .63 1.54 | 0.96 |
| Secondary diagnosis drug related | 107 | 28% | 45 | 28% | 62 | 28% | 1.01 | .72, 1.41 | 0.97 |
| Number of diagnosed psychiatric problems (mean, sd) | 0.18 | 0.51 | 0.18 | 0.50 | 0.18 | 0.52 | 1.08 | .79, 1.48 | 0.64 |
| Number of medical conditions (mean, sd) | 0.76 | 0.96 | 0.77 | 0.92 | 0.74 | 0.99 | 1.05 | .89, 1.23 | 0.58 |
| GAF on admission (mean, sd) | 43.63 | 8.89 | 41.38 | 7.86 | 45.36 | 9.25 | 0.96 | .94, .99 | 0.002 |
| History of delirium tremens or seizures | 119 | 31% | 56 | 35% | 63 | 29% | 1.26 | .91, 1.74 | 0.17 |
| Alcohol use in the last 30 days | |||||||||
| < = 29 | 195 | 51% | 84 | 52% | 119 | 54% | 1.00 | ||
| =30 | 188 | 49% | 78 | 48% | 102 | 46% | 1.17 | .86, 1.60 | 0.31 |
| Age first use (mean, sd) | 14.59 | 4.75 | 14.20 | 4.71 | 14.86 | 4.77 | 0.97 | .94, 1.01 | 0.17 |
| Number of days abstinent prior to last use | |||||||||
| 0–30 | 246 | 64% | 96 | 59% | 151 | 68% | 1.00 | ||
| 31–60 | 27 | 7% | 10 | 6% | 16 | 7% | 1.00 | .49, 2.07 | 0.99 |
| 61–90 | 24 | 6% | 10 | 6% | 16 | 7% | 1.02 | .51, 2.06 | 0.96 |
| 91+ | 86 | 22% | 46 | 29% | 38 | 17% | 1.80 | 1.26, 2.57 | 0.001 |
| Treatment completion status | |||||||||
| Complete | 287 | 75% | 124 | 77% | 166 | 75% | 1.00 | ||
| Incomplete | 96 | 25% | 38 | 23% | 55 | 25% | 0.92 | .64, 1.31 | 0.63 |
| Length of stay (mean, sd) | 5.11 | 2.44 | 5.35 | 2.46 | 4.94 | 2.42 | 1.04 | .99, 1.10 | 0.10 |
| Discharge destination | |||||||||
| Non-treatment | 313 | 82% | 133 | 82% | 179 | 81% | 1.00 | ||
| Treatment center/Medical care | 70 | 18% | 29 | 18% | 42 | 19% | 0.92 | .62, 1.34 | 0.65 |
| Referred to treatment | 138 | 36% | 58 | 36% | 80 | 36% | 0.96 | .70, 1.32 | 0.80 |
| Entered treatment (of those referred to treatment) | 80 | 58% | 34 | 59% | 46 | 58% | 0.94 | .55, 1.59 | 0.81 |
A one point increase in the GAF score was associated with a 4% decrease in readmission (HR = .96, 95% CL = .94, .99, p-value = .002; Table 1). Statistically significant (p-value = .01) bivariate relationships (housing, employment and number of days abstinent prior to last use) with readmission became non-significant once GAF was added to the model, suggesting the GAF score statistically mediated their relationships with readmission, which we then explored. Employment and unstable housing were significantly associated with GAF (p-values = <.001), further supporting its role as a mediator. The Sobel test (Preacher and Leonardelli, 2012; Sobel, 1982) further confirmed that GAF mediated the relationship between employment and readmission (p-value = .005), and between housing and readmission (p-value = .02). Fig. 2 presents the mediated relationships. It displays the coefficients and p-values for the bivariate relationships between unstable housing and employment and the GAF, as well as the associations of unstable housing and employment and readmission.
Fig. 2.
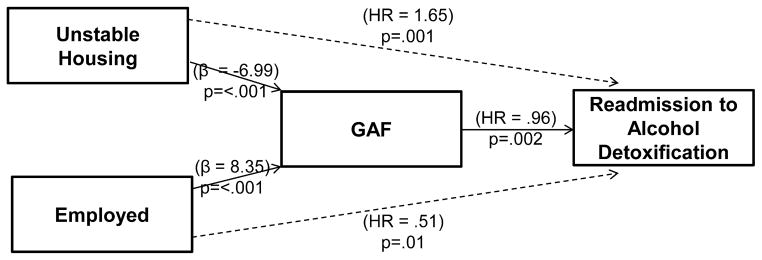
GAF mediating the effect of unstable housing and employment on readmission to detoxification. Fig. 2 depicts the GAF score mediating the effect of unstable housing and employment on readmission. This figure graphically shows the relationship between unstable housing, employment, and the GAF score assigned by the clinician, which in turn is related to readmission. Unstable housing and employment (employed versus not employed) are bivariately associated with readmission (p-values ≤.01). These relationships become non-significant when the GAF score is included in the model. Unstable housing and employment are also associated with the GAF score (p-values ≤.001), which supports the GAF score as a mediator. Cox proportional hazard modeling was used to determine coefficients for the relationships between readmission with unstable housing and employment. Linear regression was used to determine the coefficients for the relationships between the GAF with unstable housing and employment.
4. Discussion
4.1. Key results
Our study of readmission to alcohol detoxification among Alaska Native people found a readmission rate of 42% within one year. This is similar to studies among other populations reporting one year detoxification rates (Li et al., 2008; Ponzer et al., 2002) but higher than the study among Canadian Aboriginals (Callaghan, 2003) which reported 35% were readmitted within a year. We hypothesized unstable housing, a secondary drug diagnosis, not entering treatment after detoxification, and withdrawal severity measured by seizures/delirium tremens and the GAF would significantly increase the risk of readmission to detoxification. Of these, unstable housing and the GAF were significantly related to readmission to detoxification. Though employment (a measure of access to care in our conceptual model) and days abstinent (a measure of clinical characteristics/health status) were also significantly related to readmission, these were exploratory analyses. Associations of readmission with unstable housing, employment status, and number of days abstinent became non-significant once GAF was added to the model.
We suspected mediation when we observed statistically significant relationships with readmission no longer existed when GAF was in the model. Therefore, we tested for mediation post hoc after examining the primary analytical results. GAF did mediate the relationship of employment status and unstable housing with readmission. Mediating variables are frequently internal, psychological and process variables (Baron and Kenny, 1986; Kenny, 2008), like the GAF that encompasses social, occupational, psychological functioning, and symptom severity. Our mediation model indicated that unstable housing and employment, examined individually, underpinned the effect of the GAF. The clinician’s ratings of patient illness severity and adaptive functioning were likely impacted by knowing the patient’s housing and employment status, perhaps adding to the predictive value of the GAF score for readmission to detoxification.
4.2. Treatment Implications
The GAF is a comprehensive score based upon many dimensions of a patient’s life and includes illness severity as well as adaptive functioning. It is used widely in clinical settings, but prior studies of readmission to detoxification have not examined measures of functioning similar to the GAF. For alcohol detoxification patients, the GAF may prove to be a quick and accurate means for clinicians to assess the risk for readmission and should be reviewed at the time of discharge. Post-discharge planning should address housing and employment issues as these are likely to affect patient functioning which, in turn, influences readmission.
The GAF has been criticized as being unable to distinguish the relative contributions of illness severity and adaptive functioning to overall score (Smith et al., 2011). Its validity has also been questioned. Most agree the GAF measures functioning, symptoms, and psychosocial problems as originally intended (Hilsenroth et al., 2000; Tungström et al., 2005), but inter-rater reliability issues are of particular concern (Vatnaland et al., 2007). Therefore, careful calibration and fidelity of administration are especially important (Hilsenroth et al., 2000; Startup et al., 2002). Since clear, consistent, and written guidelines for scoring the GAF are strongly related to reliable administration, we recommend training for clinicians who regularly use it in treatment settings. Emphases should include timing of collection, where to begin scoring (top, middle, bottom), and guidelines for scoring specific heath conditions (Aas, 2011). Clinic procedures should indicate the exact timing at which the GAF is scored. Patient functioning and symptomology may change rapidly, even within a twenty-four hour time period (Vatnaland et al., 2007), making it important to score patients during a specific time period. In addition, scoring should begin at the same point on the GAF scale for all patients, affording clinicians a consistent initial referent. For example, starting at a low score and moving up the scale or vice versa. GAF scoring guidelines should be specific to the health condition for which it is being used. Specific health-related scoring guidelines can take into account the types of functioning and symptoms directly related to the health condition for which it is used, providing a more meaningful assessment of illness severity and adaptive functioning.
4.3. Methodological issues and limitations
Measuring readmission was a limitation in this study and could have led to an underestimation of those readmitted to alcohol detoxification. Information about previous detoxification admissions was unknown prior to the index admission. A small number of patients may have been readmitted elsewhere, but this was unlikely given the limited detoxification options nearby for these patients.
There are specific limitations of these data worth noting. First, this was a retrospective study that relied upon EMR data collected for treatment purposes. Consequently, data recorded in the EMR may not include important indicators of readmission to detoxification. Second, the analyses relied on several variables that were patient self-reported to detoxification unit staff. Third, some patients may have been reluctant to report certain types of information. In particular, staff questioned the under-report of number of medical and number of diagnosed psychiatric conditions. Other information available, but not included in the study because of likely under-reporting included court mandated treatment, acculturation issues, and physical as well as sexual abuse.
We were unable to fully study access to care, part of the conceptual model of readmission, due to data limitations. Access is important to consider when studying readmission to detoxification in the state of Alaska, particularly distance to health care services and transportation. There are over 300 communities throughout the state; approximately 75% are not connected by a road to a community with a hospital (State of Alaska, 2010). One-fourth of the population reside in locations only reached by aircraft or boat (State of Alaska, 2010). Transportation to the nearest hospital from a neighboring community can cost more than $100 and transportation from the most remote locations to the ANMC can cost upwards of $1200 (State of Alaska, 2010). The costs of transportation, a sparse population living in remote areas across an expansive land base with fluctuating weather conditions and diverse terrain seem likely to contribute to access to care issues. Additionally, substance abuse treatment workforce and services are limited (Hesselbrock et al., 2003).
This study, like others of readmission to detoxification, lacked detailed clinical measures of withdrawal management and severity. For instance, moderate symptoms of withdrawal such as insomnia, anxiety, headache, gastrointestinal upset, irritability and agitation have not been included in previous studies of readmission to detoxification. More severe indicators of withdrawal such as seizures are linked to readmission and likely require further investigation (Booth and Blow, 1993; Worner, 1996). Severity of symptoms may be an indicator of chronic illness. Patients with more complex illnesses experience worse health outcomes, develop more complications (Iezzoni, 2003), and may be readmitted more often. Accounting for withdrawal severity in readmission to detoxification is important element for future study.
4.4. Future directions
Recently, the GAF was replaced in the DSM V with the World Health Organization Disability Assessment Schedule (WHODAS; American Psychiatric Association, 2013). The WHODAS is a 36-item assessment based upon six domains of functioning (understanding and communicating, getting around, self-care, getting along with people, life activities, participation in society) (American Psychiatric Association, 2013). The assessment can produce a single scale score, a more complex computer generated scale score, and domain specific scores. The GAF is based upon the clinician’s assessment of the patient while the WHODAS is patient self-reported, but permits the clinician to correct the score if deemed necessary. In contemplating the use of the WHODAS in a fast paced setting like detoxification, patient and provider burden should be considered. With training, the GAF is a very quick, easy, and accurate assessment with no patient burden and minimal provider burden. The WHODAS will require more patient time to complete as well as provider time to review and correct if necessary. The GAF was a powerful predictor of readmission to detoxification in this study; whether the WHODAS has similar properties requires future investigation. Regardless of instrumentation, measures of patient functioning should be incorporated into future studies.
Future studies should seek to capture the full spectrum of withdrawal symptoms in detoxification patients as these may be important predictors of readmission. Patients with higher scores on the Clinical Institute Withdrawal Assessment–Alcohol Revised protocol were more likely to have multiple admissions to a tertiary referral hospital (Larson et al., 2012). Including similar measures of withdrawal symptomology in studies of readmission to detoxification is an important next step and may yield similar findings.
Richman and Neumann (1984) argued the need for new treatment approaches for patients who are frequently readmitted to alcohol detoxification. The GAF may have important clinical implications if used to measure a patient’s level of functioning upon entry into treatment. The ability to improve patient functioning during treatment and aftercare may decrease the risk of readmission, particularly if a program addresses employment and housing issues. Providing housing to homeless individuals with severe alcohol problems reduces health care costs (Larimer et al., 2009). Reducing repeated readmissions ultimately promises to lower treatment costs and overall health expenditures. Additional studies using patient functioning as a predictor of readmission to detoxification will further clarify the generalizability of these results and their implications for improved aftercare.
Supplementary Material
Acknowledgments
Role of funding source
There was no funding source for the conduct of this research. Dr. Manson’s efforts in the development and contributions of this manuscript were support by the National Institute for Minority Health and Health Disparities, P60 MD000507 (SM Manson, PI). Dr. Prochazka’s efforts in the development and contributions of this manuscript were supported by NIH/NCATS Colorado CTSI Grant Number UL1 TR000154. NIMHD and NIH/NCATS had no further role in the study; design, analysis, interpretation of the data, writing of the manuscript or decision to submit the paper for publication
We wish to thank the detoxification unit that provided the data for this analysis, as well as the National Institute for Minority Health and Health Disparities (P60 MD000507, SM Manson, PI) for the infrastructural support that facilitated the management and analyses of the data.
Appendix A. Supplementary data Description
Supplementary data description associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.drugalcdep.2014.04.018.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
Dr. Running Bear performed the literature search, completed the statistical analysis, and drafted sections of the manuscript. Dr. Manson assisted in the design of the study, facilitated access to the agency that housed the data, assisted in obtaining the necessary human subjects approvals, and edited the manuscript. Dr. Novins and Dr. Anderson assisted in the design of the study, selection of appropriate statistical analyses, and edited the manuscript. Dr. Shore and Dr. Prochazka assisted in the design of the study and edited the manuscript. All authors contributed to and approved the final manuscript.
Conflict of interest
Drs. Running Bear, Anderson, Manson, Shore, Prochazka and Novins have no actual or potential conflicts that could inappropriately influence their contribution to this manuscript.
References
- Aas IH. Guidelines for rating global assessment functioning (GAF) Ann Gen Psychiatry. 2011;10:1–11. doi: 10.1186/1744-859X-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaska Native Tribal Health Consortium. Alaska Native Medical Center; 2013a. Retrieved 12/2/2013, 2013, from http://www.anmc.org/ [Google Scholar]
- Alaska Native Tribal Health Consortium. Alaska Native Tribal Health Consortium; 2013b. Retrieved December 21, 2013, from http://anthctoday.org/about/serve.html. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. APA; Washington, D.C: 2000. text rev. ed. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders: DSM-5. APA; Washington, DC: 2013. [Google Scholar]
- Annis HM, Liban CB. A follow-up study of male halfway-house residents and matched nonresident controls. J Stud Alcohol. 1979;40:63–69. doi: 10.15288/jsa.1979.40.63. [DOI] [PubMed] [Google Scholar]
- Arbaje AI, Woff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48:495–504. doi: 10.1093/geront/48.4.495. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Booth BM, Blow FC. The kindling hypothesis: further evidence from a U.S. national study of alcoholic men. Alcohol Alcoholism. 1993;28:593–598. [PubMed] [Google Scholar]
- Bursac Z, Gauss CH, Williams DK, Hosmer DH. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17–24. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan RC. Risk factors associated with dropout and readmission among First Nation individuals admitted to an inpatient alcohol and drug detoxification program. CMAJ. 2003;169:23–27. [PMC free article] [PubMed] [Google Scholar]
- Callaghan RC, Cull R, Vettese LC, Taylor L. A gendered analysis of Canadian aboriginal individuals admitted to inpatient substance abuse detoxification: a three-year medical chart review. Am J Addict. 2006;15:380–386. doi: 10.1080/10550490600860270. [DOI] [PubMed] [Google Scholar]
- Carrier E, McNeely J, Lobach I, Tay S, Gourevitch MN, Raven MC. Factors associated with frequent utilization of crisis substance use detoxification services. J Addict Dis. 2011;30:116–122. doi: 10.1080/10550887.2011.554776. [DOI] [PubMed] [Google Scholar]
- Day G, Holck P, Provost E. Alaska Native Mortality Update: 2004–2008. Alaska Native Epidemology Center. Alaska Native Tribal Health Consortium; 2011. [Google Scholar]
- Franken IH, Hendriks VM. Predicting outcome of inpatient detoxification of substance abusers. Psychiatr Serv. 1999;50:813–817. doi: 10.1176/ps.50.6.813. [DOI] [PubMed] [Google Scholar]
- Hasan O, Meltzer DO, Shaykevich SA, Bell CM, Kaboli PJ, Auerback AD, Wetterneck TB, Arora VM, Zhang J, Schnipper JL. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25:211–219. doi: 10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashida M. An overview of outpatient and inpatient detoxification. Alcohol Health Res World. 1998;22:44–46. [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN, Segal B. Alcohol dependence among Alaskan Natives and their health care utilization. Alcohol Clin Exp Res. 2003;27:1353–1355. doi: 10.1097/01.ALC.0000080167.17411.21. [DOI] [PubMed] [Google Scholar]
- Hilsenroth MJ, Ackerman SJ, Blagys MD, Baumann BD, Baity MR, smith SR, Price JL, Smith CL, Heindselman TL, Mount MK, Holdwick DJ. Reliability and validity of DSM-IV Axis V. Am J Psychiat. 2000;157:1858–1863. doi: 10.1176/appi.ajp.157.11.1858. [DOI] [PubMed] [Google Scholar]
- Hintze J. NCSS PASS 2005. NCSS, LLC; Kaysville, UT: 2005. [Google Scholar]
- Iezzoni LI. Reasons for risk adjustment. In: Iezzoni LI, editor. Risk Adustment for Measuring Health Care Outcomes. Health Administration Press; Chicago, Illinois: 2003. [Google Scholar]
- Kenny DA. Reflections on mediation. Organ Res Method. 2008;11:353–358. [Google Scholar]
- Larimer ME, Malone DK, Garnder MD, Atkins DC, Burlingham B, Lonczak HS, Tanzer K, Ginzler J, Clifasefi SL, Hobson WG, Marlatt GA. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;30:1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- Larson SA, Burton MC, Kashiwagi DT, Hugo SP, Cha SS, Lapid MI. Multiple admission for alcohol withdrawal. J Hosp Med. 2012;7:617–621. doi: 10.1002/jhm.1953. [DOI] [PubMed] [Google Scholar]
- Li X, Sun H, Marsh DC, Anis AH. Factors associated with seeking readmission among clients admitted to medical withdrawal management. Subst Abuse. 2008;29:65–72. doi: 10.1080/08897070802418519. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suprression effect. Prev Sci. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Vandivort-Warren R, Montejano LB. Factors affecting detoxification readmission: analysis of public sector data from three states. J Subst Abuse Treat. 2006;31:439–455. doi: 10.1016/j.jsat.2006.05.019. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Weinstein RL, Shen Q, Kendig C, Levine M. Improving continuity of care in a public addiction treatment system with clinical case managment. Am J Addict. 2005;14:426–440. doi: 10.1080/10550490500247099. [DOI] [PubMed] [Google Scholar]
- Miller NS, Kipnis SS. Detoxification and Substance Abuse Treatment. Treatment Improvement Protocol (TIP) Series 45. (SMA 06–4131) Substance Abuse and Mental Health Services Administration; Rockville, MD: 2006. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Muthén & Muthén; Los Angeles, CA: 1998–2011. [Google Scholar]
- Nighswander TS. High utilizers of ambulatory care services: 6-year followup at Alaska Native Medical Center. Public Health Rep. 1984;99:400–404. [PMC free article] [PubMed] [Google Scholar]
- Ponzer S, Johansson SE, Bergman B. A four-year follow-up study of male alcoholics: factors affecting the risk of readmission. Alcohol. 2002;27:83–88. doi: 10.1016/s0741-8329(02)00203-3. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Leonardelli GJ. Calculation for the sobel test: an interactive calculation tool for mediation tests. 2012 Retrieved November 1, 2012, 2012, from http://quantpsy.org/sobel/sobel.htm.
- Richman A, Neumann B. Breaking the ’detox-loop’ for alcoholics with social detoxification. Drug Alcohol Depend. 1984;13:65–73. doi: 10.1016/0376-8716(84)90033-4. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® 9.3 User’s Guide. SAS Institute Inc; Cary, NC: 2011. [Google Scholar]
- Sherry P. Health care delivery for Alaska Natives: a brief overview. Int J Circumpolar Health. 2004;63:54–62. doi: 10.3402/ijch.v63i0.17786. [DOI] [PubMed] [Google Scholar]
- Smith GN, Ehmann TS, Flynn SW, MacEwan GW, Tee K, Kopala LC, Thornton AEHSC, Honer WG. The assessment of symptom severity and functional impairment with DSM-IV Axis V. Psychiatr Serv. 2011;62:411–417. doi: 10.1176/ps.62.4.pss6204_0411. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Soc Method. 1982;13:290–312. [Google Scholar]
- Solomon P, Doll W. The varieties of readmission: the case against the use of recidivism rates as a measure of program effectiveness. Am J Orthopsychiat. 1979;49:230–239. doi: 10.1111/j.1939-0025.1979.tb02604.x. [DOI] [PubMed] [Google Scholar]
- South Central Foundation. 2013 Retrieved 12/3/2013, 2013, from http://www.scf.cc/index.cfm.
- Startup M, Jackson MC, Bendix S. The concurrent validity of the Global Assessment of Functioning (GAF) Br J Clin Psychol. 2002;41:417–422. doi: 10.1348/014466502760387533. [DOI] [PubMed] [Google Scholar]
- State of Alaska. Transforming Health Care in Alaska: 2009 report/2010–2014 Strategic Plan. Anchorage, Alaska: 2010. [Google Scholar]
- Sullivan G. Rehospitalization of the Seriously Mentally Ill in Mississippi: Conceptual Models, Study Design, and Implementation. The RAND Corporation; Santa Monica, CA: 1989. p. 83. [Google Scholar]
- Tomasson K, Vaglum P. The role of psychiatric comorbidity in the prediction of readmission for detoxification. Compr Psychiat. 1998;39:129–136. doi: 10.1016/s0010-440x(98)90071-2. [DOI] [PubMed] [Google Scholar]
- Tungström S, Söderberg P, Armelius BA. Relationship between the global assessment of functioning and other DSM axes in routine clinical work. Psychiat Serv. 2005;56:439–443. doi: 10.1176/appi.ps.56.4.439. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Indian Health Services. Alaska Area Profile. Division of Planning; 2007. [Google Scholar]
- US Census Bureau. American FactFinder. 2014 Retrieved 1/3/2014, from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_1YR_DP05&prodType=table.
- Vatnaland T, Vatnaland J, Friis S, Opjordsmoen S. Are GAF scores reliable in routine clinical use? Acta Psychiat Scand. 2007;115:326–330. doi: 10.1111/j.1600-0447.2006.00925.x. [DOI] [PubMed] [Google Scholar]
- Worner TM. Relative kindling effect of readmissions in alcoholics. Alcohol Alcoholism. 1996;31:375–380. doi: 10.1093/oxfordjournals.alcalc.a008164. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


