Abstract
Context
Unrecognized myocardial infarction (MI) is prognostically important but electrocardiography (ECG), the main epidemiology tool for detection, is insensitive to MI.
Objective
Determine prevalence and mortality risk for unrecognized MI (UMI) detected by cardiac magnetic resonance (CMR) or ECG.
Design
ICELAND MI is a cohort substudy of the Age, Gene/Environment Susceptibility-Reykjavik Study (enrollment January 2004–January 2007) using ECG or CMR to detect UMI.
Setting
Community dwelling participants in Iceland over age 67.
Participants
936 participants (ages 67–93 years) including 670 who were randomly selected and 266 with diabetes.
Main Outcome Measures
MI prevalence and mortality through September 1, 2011. Results reported with 95% confidence limits and net reclassification improvement (NRI).
Results
Of 936 participants, 91 had recognized MI (RMI; 9.7% CI 8–12%), and 157 had UMI by CMR (17%; CI 14–19%) which was more prevalent than the 46 UMI by ECG (5%; CI 4–6%, p<0.001). Diabetic participants had more UMI by CMR than UMI by ECG (n=72; 21%; CI 17–26% vs. n=15; 4%; CI 2–7%, p<0.001). UMI by CMR was associated with atherosclerosis risk factors, coronary calcium, coronary revascularization, and peripheral vascular disease. Over a median of 6.4 years, 33% (CI 23–43%) of individuals with RMI died (30 of 91) and 28% (CI 21–35%) with UMI died (44 of 157), both higher rates than the 17% (CI 15–20%) with no MI that died (119 of 688). UMI by CMR improved risk stratification for mortality over RMI (NRI: 0.34; CI 0.16–0.53). Adjusting for age, sex, diabetes, and RMI, UMI by CMR remained associated with mortality (HR 1.45 CI 1.02–2.06, absolute risk increase (ARI) 8%) and significantly improved risk stratification for mortality, NRI 0.16 (CI 0.01–0.31)) but UMI by ECG did not (HR 0.88, CI 0.45–1.73 ARI −2%; NRI: −0.05; CI −0.17–0.05). Compared to those with RMI, participants with UMI by CMR used cardiac medications such as statins less often (36%; CI, 28–43% or 56/157 vs.73%; CI 63–82% or 66/91; p<0.001).
Conclusions
In a community-based cohort, the prevalence of UMI by CMR was higher than the prevalence of recognized MI or UMI by ECG, and was associated with increased mortality risk.
Introduction
The prevalence and prognosis of unrecognized myocardial infarction (MI) in older people with and without diabetes may be higher than previously suspected in population studies.1–4 Advances in MI detection, such as cardiac magnetic resonance (CMR) with late gadolinium enhancement (LGE), are more sensitive than prior methods.5 Ascertaining the prevalence of unrecognized MI (UMI) in these groups is relevant since age and diabetes increase the risks of coronary heart disease (CHD).6 Pathologic studies7 indicate that subclinical coronary plaque rupture occurs frequently, particularly in diabetic individuals, which may culminate in a high prevalence of UMI. Several population studies1–4 have described the prevalence of UMI based on electrocardiography (ECG), but ECG has significant limitations such as limited sensitivity that varies with infarct location8 and Q waves may resolve over time.9 Thus, the true prevalence of UMI may be significantly higher than appreciated in prior epidemiology studies. CMR with late gadolinium enhancement (LGE) has been extensively validated for the detection of MI,10 is more sensitive than SPECT11 or PET12 and therefore is probably more sensitive than ECG. However, increased sensitivity is clinically important when the new test better identifies those at risk for adverse events.
The specific aim of this study was to compare the prevalence and prognosis of recognized and unrecognized MI diagnosed with CMR versus ECG in older diabetic and nondiabetic participants participating in ICELAND MI, a substudy of the Age, Gene/Environment Susceptibility-Reykjavik Study (AGES- Reykjavik). We hypothesized that UMI by CMR: 1) would be more prevalent than UMI by ECG, in both diabetic and nondiabetic individuals 2) would be associated with measures of atherosclerosis, and 3) would be significantly associated with increased mortality risk.
Methods
Patient Sample
ICELAND MI is an epidemiologic cohort study of diabetic and nondiabetic individuals. Participants were enrolled from January 2004 to January 2007, recruited from the AGES-Reykjavik Study (n=5,764),13 a randomly selected population-based cohort of men and women born between 1907 and 1935 who have been followed in Iceland since 1967 by the Icelandic Heart Association. AGES–Reykjavik was approved by the National Bioethics Committee in Iceland that acts as the institutional review board for the Icelandic Heart Association (approval number VSN-00-063) and by the National Institute on Aging Intramural Institutional Review Board. Participants were eligible to participate in ICELAND MI if they provided written informed consent and were ineligible if they could not safely receive CMR scans (e.g., implanted devices) or gadolinium contrast (e.g., severe kidney disease). Participants were recruited from AGES-Reykjavik in two phases. The first phase involved random recruitment, and a second phase recruited all eligible and willing participants with diabetes.
Data Elements
Participants were characterized during three clinic visits.13 CMR studies occurred during a separate exam that included ECG. Participant surveillance has been ongoing since 1967 through the Icelandic Heart Association13 and provided ascertainment of recognized MI.
Participants were defined as having a recognized MI when a history of MI was supported by hospital records or surveillance records.13 Participants were defined as having an UMI by ECG when there was evidence of MI by ECG criteria (Minnesota codes 1.1.1–1.2.8). 1 UMI by CMR meant there was no prior MI by hospital records or by surveillance records, and LGE involved the subendocardium in a coronary distribution. Other “atypical” patterns of LGE were specifically not designated as MI, a strategy that yields sensitivities and specificities >90% for MI detection.14–16 CMR studies were interpreted by cardiologists blinded to clinical information.
Participants were further characterized with demographics, risk factors related to atherosclerosis, other comorbidity, biochemical measurements from blood, coronary calcium (Agatston scores), and ECG. Participants were classified as having diabetes according to standard criteria (fasting glucose ≥7 mmol/L)17 or if they were already receiving treatment for diabetes. All cause mortality was identified by review of hospital records as well as a national mortality index with authentication of all death certificates13 through September 1, 2011.
Cardiovascular Magnetic Resonance Studies
CMR scans were performed on a 1.5T GE scanner (Milwaukee, WI) using a four-element cardiac phased array coil. Typical cine SSFP scan parameters resulted in pixel dimensions of 1.8×2.1 mm, slice thickness 8 mm with 3 mm gap, and 30 images per cycle. Standard long axis and short axis views were obtained to evaluate global and regional function. The presence of MI was evaluated with a prospective, ECG gated, segmented, phase sensitive gradient echo inversion recovery sequence approximately 6–25 minutes after 0.1 mmol/kg intravenous gadolinium (Magnevist, Berlex).18 LGE was designated MI by consensus of cardiologists experienced in CMR.
Statistical analysis
Results are presented with 95% confidence intervals (CI). Categorical variables were compared with the Chi-square or Fisher’s test. Continuous variables were compared with the Wilcoxon rank-sum test. McNemar’s statistic tested whether CMR was more likely to detect UMI than ECG. The log rank test compared survival curve strata. Binary response variables were further analyzed by Cox regression survival analysis, and continuous variables were analyzed by linear regression. Multivariable Cox models adjusted for variation in key baseline characteristics included in prior epidemiologic studies using ECG: age, gender, diabetes, recognized MI, and finally UMI by CMR or UMI by ECG. Proportional hazards assumptions were verified by Schoenfeld residuals and time interaction terms. Absolute risk increases were calculated by measuring the survival rate difference before and after exponentiating the 7 year Kaplan-Meier survival rate in the reference group to the power of the adjusted hazard ratio (HR) in the comparison group. The integrated discrimination index (IDI) and net reclassification index (NRI) evaluated the added predictive ability of survival models with the introduction of the UMI by CMR variable.19,20 Follow-up was enhanced by hospital record information, a national mortality index with authentication of all death certificates, a Minimum Data Set for Nursing Home patients, and Minimum Data Set for Home-Care patients.13 Coronary artery calcium (CAC) was analyzed on the natural logarithm scale, ln(CAC+1). Two sided p values <0.05 were considered significant. SAS software (version 9.2) analyzed the data.
Results
Recruitment
For phase one, 839 individuals were invited and 702 enrolled. In phase two, 421 participants with diabetes were invited and 290 people enrolled (1005 total). Thirty-five participants declined CMR. Of those who underwent CMR (n=970), 34 participants had nondiagnostic CMR scans due to: arrhythmia or inability to breath hold (n=14); claustrophobia (n=7); inability to gate cardiac images (n=3), technical issues with reconstruction and data transfer (n=9); or artifact from spinal implants (n=1). These participants were excluded leaving a final cohort of 936 participants. Survivors were followed for a median of 6.6 years (range 4.6– 7.7 yrs).
Baseline Characteristics
The median age was 76 years (range 68 to 94 years), and 52% (CI 49–55%) were women (484 of 936). Baseline characteristics are summarized in Table 1. ICELAND MI participants randomly selected in phase 1 had characteristics almost identical to the AGES-Reykjavik participants (Supplementary eTable 1).
Table 1.
Baseline characteristics of participants.
| Variable | Number (Percentage) or Median (IQR for continuous variables) N=936 |
|---|---|
| Patient Characteristics | |
| Age, median (IQR), y | 76 (72–81) |
| Women, No. (%, CI) | 484 (52%, 49–55%) |
| BMI, median (IQR) | 27 (25–30) |
| Risk factors for coronary heart disease | |
| Hypertension, No. (%, CI) | 629 (67%, 64–70%) |
| Prior or current smoking, No. (%, CI) | 560 (60%, 57–63%) |
| Family history of MI, No. (%, CI) | 334 (36%, 33–39%) |
| Diabetes, No. (%, CI) | 337 (36%, 33–39%) |
| Hypercholesterolemia, No. (%, CI) | 421 (45%, 42–48%) |
| History of atherosclerosis | |
| Coronary disease (Hospital records) | |
| Prior MI, No. (%, CI) | 91 (10%, 8–12%) |
| Prior coronary revascularization, No. (%, CI) | 139 (15%, 13–17%) |
| Other atherosclerotic disease | |
| Peripheral arterial disease, No. (%, CI) | 18 (2%, 1–3%) |
| Stroke, No. (%, CI) | 52 (6%, 4–7%) |
| Laboratory Results | |
| eGFR, median (IQR) mL/min per 1.73 m2 | 69 (59–82) |
| Total Cholesterol, median (IQR), mg/dL* | 208 (178–240) |
| HDL Cholesterol, median (IQR), mg/dL* | 56 (46–68) |
| LDL Cholesterol, median (IQR), mg/dL* | 128 (99–158) |
| Triglycerides, median (IQR), mg/dL* | 98 (75–135) |
| Coronary calcium score, median (IQR), Agatston† | 361 (74–974) |
To convert to SI units, multiply cholesterol values by 0.0259, and triglyceride values by 0.0113.
The coronary calcium scores ranged from 0–7333. Coronary artery calcification occurs in atherosclerotic arteries and is absent in the normal vessel wall. Higher coronary calcium scores, measured by the Agatston method from CT scans, correlate with higher risks of coronary events.
Prevalence of Myocardial Infarction using Cardiovascular Magnetic Resonance and ECG
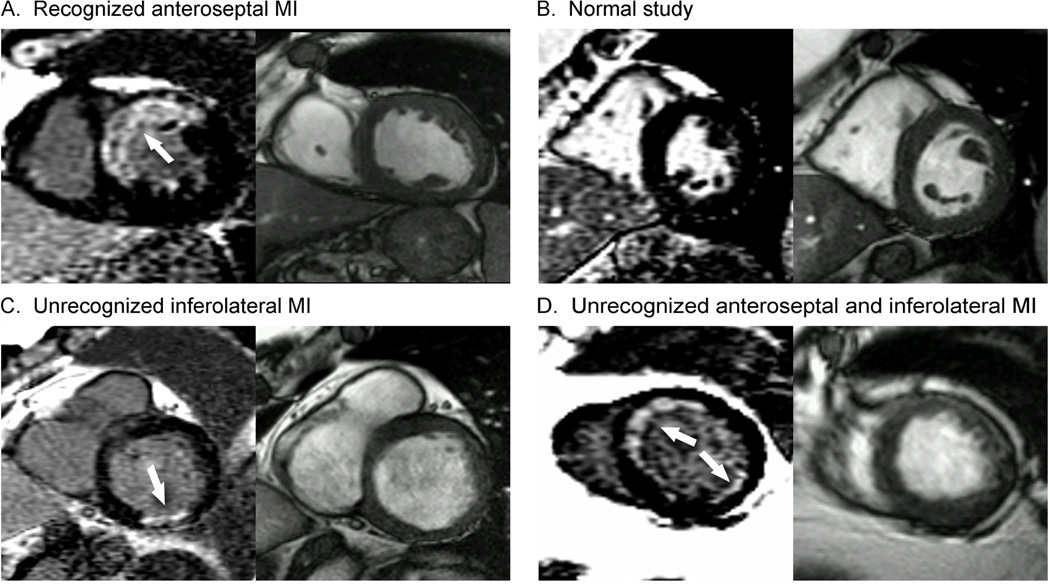
While 91 of 936 participants (9.7% CI, 8–12%) had recognized MI, the prevalence of UMI by CMR was even higher 157 of 936 (17%, CI, 14–19%; p<0.001) as shown in Table 2. Those with diabetes had a higher prevalence of UMI by CMR than those without diabetes (n=72; 21%, CI 17–26% vs. n=85; 14%, CI 11–17%, p<0.001). Examples are shown in Figure 1.
Table 2.
Prevalence of recognized and unrecognized myocardial infarction (MI) by CMR or ECG stratified by diabetes status. UMI by CMR were observed roughly twice as often as recognized MI. The prevalence of MI with the addition of ECG was significantly higher than the prevalence without ECG, but still significantly less than the increased prevalence with the addition of CMR (p<0.01 for both).
| All 936 Participants | Prevalence in 337 Participants with Diabetes, No. (%, CI) |
Prevalence in 599 Participants without Diabetes, No. (%, CI) |
|
|---|---|---|---|
| No MI | 688 (74%, 71–76%) | 228 (68%, 63–73%) | 460 (77%, 73–80%) |
| Clinically Recognized MI | 91 (10%, 8–12%) | 37 (11%, 8–14%) | 54 (9%, 7–11%) |
| Unrecognized MI by ECG | 46 (5%, 4–6%) | 15 (4%, 2–7%) | 31 (5%, 3–7%) |
| Unrecognized MI by CMR | 157 (17%, 14–19%) | 72 (21%, 17–26%) | 85 (14%, 11–17%) |
| Cumulative MI by ECG | 137 (15%, 12–17%) | 52 (15%, 12–19%) | 85 (14%, 11–17%) |
| Cumulative MI by CMR | 248 (27%, 24–29%) | 109 (32%, 27–37%) | 139 (23%, 20–27%) |
Abbreviations: CMR, cardiac magnetic resonance; ECG, electrocardiography; MI, myocardial infarction.
Figure 1. CMR examples of recognized MI (A), no MI (B), and unrecognized MI (C and D).
Panel A demonstrates a recognized myocardial infarction involving the anterior and anteroseptal segments in the typical left anterior descending artery distribution as seen on late gadolinium enhancement imaging (arrow) with the corresponding diastolic cine frame on the right. Panel B demonstrates a participant with no evidence of myocardial infarction on late gadolinium enhancement imaging. The myocardium is uniformly dark (“nulled”) on the late gadolinium enhancement image (left). Panel C demonstrates an unrecognized myocardial infarction in the basal inferolateral wall on late gadolinium enhancement imaging (arrow) with the corresponding end-diastolic cine frame on the right. Panel D demonstrates two unrecognized myocardial infarctions in different coronary territories in the same participant. There is a small myocardial infarction in the inferolateral wall (arrow) corresponding to the left circumflex artery territory and a larger myocardial infarction involving the anterior and anteroseptal segments (arrow) corresponding to left anterior descending artery territory. The corresponding end-diastolic cine frame is shown on the right.
CMR detected 157 UMI which was more than the 46 UMI by ECG (prevalence by CMR 17%, CI 14–19% vs. ECG 5%, CI 4–6%, respectively, p<0.001). There were 27 participants (3%, CI 2–4%) with UMI by ECG that exhibited no MI on CMR, and there were 138 (15%, CI 12– 17%) individuals who had UMI by CMR yet did not meet criteria for UMI by ECG (p<0.001). In the randomly sampled cohort (n=670), 61 (9%, CI 7–11%) had recognized MI and 97 (14%, CI 12–17%) had UMI by CMR whereas only 35 (5%, CI 4–7%) had UMI by ECG, significantly less than UMI by CMR (p<0.001).
Associations of Unrecognized MI by CMR and Recognized MI with Atherosclerosis and Diabetes
Coronary artery disease risk factors were more prevalent in participants with UMI compared with those with no MI. Compared to those without MI, participants with UMI were more frequently male, were slightly older, and had more hypertension and diabetes (Table 3). Similarly, those with UMI had more atherosclerosis with significantly higher coronary calcium scores than those without MI (Table 3). Overall, coronary calcium showed a significant graded relationship to the presence of MI, where participants with UMI had coronary calcium intermediate between those without MI and those with clinically recognized MI (Table 3).
Table 3.
Associations of recognized MI and unrecognized MI detected by CMR with diabetes or atherosclerosis.
| No MI (n=688) |
Unrecognized MI (n=157) |
Recognized MI (n=91) |
P value for trend |
|
|---|---|---|---|---|
| Variable | ||||
| Patient Characteristics | ||||
| Age, median (IQR), y | 76 (72–80) | 77 (74–83) | 78 (74–82) | <0.001 |
| Women, No. (%, CI) | 395 (57%, 54–61%) | 57 (36%, 29–44%)* | 32 (35%, 25–45%) | <0.001 |
| BMI, median (IQR) | 27 (25–30) | 28 (25–30) | 27 (24–31) | 0.80 |
| Risk factors for coronary heart disease | ||||
| Hypertension, No. (%, CI) | 422 (61%, 58–65) | 124 (79%, 73–85%)*† | 83 (91, 85–97%) | <0.001 |
| Prior or current smoking, No. (%, CI) | 391 (58%, 54–61%) | 98 (62%, 55–70%) | 65 (71%, 62–81%) | 0.033 |
| Family history of MI, No. (%, CI) | 237 (34%, 31–38%) | 56 (36%, 28–43%) | 41 (45%, 35–55%) | 0.14 |
| Diabetes, No. (%, CI) | 228 (33%, 30–37%) | 72 (46%, 38–54%)* | 37 (41%, 31–51%) | 0.007 |
| Hypercholesterolemia, No. (%, CI) | 297 (43%, 39–47%) | 72 (46%, 38–54%) | 52 (57%, 47–67%) | 0.041 |
| History of atherosclerosis | ||||
| Prior coronary revascularization, No. (%) | 42 (6%, 4–8%) | 44 (28%, 21–35%)*† | 53 (58%, 48–68%) | <0.001 |
| Peripheral arterial disease, No. (%) | 8 (1%, 0–2%) | 6 (4%, 1–7%)* | 4 (4%, 0–9%) | 0.018 |
| Stroke, No. (%) | 33 (5%, 3–6%) | 11 (7%, 3–11%) | 8 (9%, 3–15%) | 0.20 |
| Laboratory Results | ||||
| eGFR, median (IQR) mL/min per 1.73 m2 | 70 (59–82) | 68 (58–81) | 64 (53–74) | 0.004 |
| Total Cholesterol, median (IQR), mg/dL* | 216 (185–243) | 201 (170–239)*† | 178 (154–205) | <0.001 |
| HDL Cholesterol, median (IQR), mg/dL* | 58 (47–69) | 53 (45–63)* | 51 (42–59) | <0.001 |
| LDL Cholesterol, median (IQR), mg/dL* | 134 (108–162) | 120 (91–157) *† | 98 (77–128) | <0.001 |
| Triglycerides, median (IQR), mg/dL* | 95 (73–132) | 108 (79–148)* | 104 (73–145) | 0.008 |
| Coronary calcium score, median (IQR), Agatston | 227 (50–693) | 792 (263–1713)*† | 1133 (654–2159) | <0.001 |
| Medications | ||||
| Aspirin, No (%, CI) | 215 (31%, 28–35%) | 81 (52%, 44–59%)*† | 74 (81%, 73–89%) | <0.001 |
| Beta blocker, No (%, CI) | 237 (34%, 31–38%) | 70 (45%, 37–52%)*† | 70 (77%, 68–86%) | <0.001 |
| Statins, No (%, CI) | 153 (22%, 20–25%) | 56 (36%, 28–43%)*† | 66 (73%, 63–82%) | <0.001 |
| ACE Inhibitors or Angiotensin receptor blockers, No (%, CI) | 132 (19%, 16–22%) | 42 (27%, 20–34%)* | 26 (29%, 19–38%) | 0.0084 |
| CMR characteristics | ||||
| Ejection fraction (%), median (IQR) | 63 (58–67) | 60 (51–65)*† | 53 (42–61) | <0.001 |
| End diastolic volume index, ml/m2) | 98 (87–111) | 109 (92–124)*† | 113 (96–147) | <.001 |
| Left ventricular mass index, g/m2 | 72 (62–83) | 83 (70–95)* | 83 (69–102) | <.001 |
Significantly different compared to individuals without MI (p<0 .05). For coronary calcium, these differences persisted even after adjusting for age and gender.
Significantly different compared to those with recognized MI (p<0.05). For coronary calcium, these differences persisted even after adjusting for age and gender.
There was also a graded relationship between the likelihood of revascularization and MI status (Table 3). For 26 of 72 diabetic (36%, CI 25–47%) and 18 of 85 nondiabetic (21%, CI 12– 30%) participants with UMI had prior coronary revascularization. Excluding those with prior coronary revascularization (n=139), diabetic and nondiabetic participants still had high rates of UMI (46/273 or 17%, CI 12–21% versus 67/524 or 13%, CI 10–16%, respectively). Thus, UMI was associated with atherosclerosis risk factors, coronary calcium, and treatment for atherosclerosis. Other characteristics of those with UMI by CMR are also provided in Table 3.
Prognosis of Recognized and Unrecognized MI by ECG or CMR
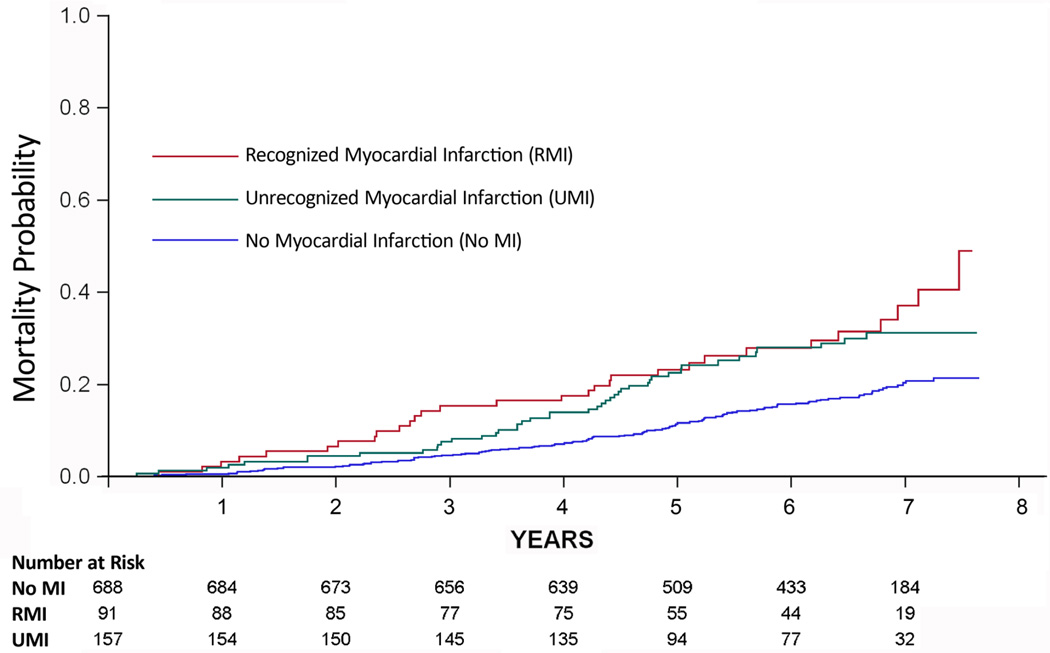
Over a median follow-up of 6.4 years (interquartile range 4.9–7.0 years), 30 of 91 participants with recognized MI died (33%, CI 23–43%) and 44 of 157 with UMI by CMR died (28% CI 21–35%) which were both significantly higher rates than the 17% (CI 15–20%) with no MI that died (119 of 688). Both UMI by CMR and recognized MI had higher mortality compared to those without MI (HR 1.81, CI 1.28–2.56; absolute risk increase 13%, and HR 2.20, CI 1.48–3.29, absolute risk increase 19%, respectively). UMI by CMR improved mortality risk stratification beyond RMI (category free NRI: 0.34; CI 0.16–0.53). UMI detected by ECG was not associated with higher mortality (HR 0.95, CI 0.49–1.87, absolute risk increase; −1%). Unadjusted Kaplan-Meier survival curves for those without MI, those with UMI by CMR, and those with clinically recognized MI are shown in Figure 2. Five years after the CMR scan, the absolute mortality rates were: 12% (CI 9–14%) for those without MI, 23% (CI 16–29%) with unrecognized MI by CMR, and 23% (CI 17–30%) in those with recognized MI. This culminated in approximately a 10% difference in absolute mortality rates between those with and without MI (eTable2).
Figure 2. Mortality curves according to myocardial infarction status.
The mortality was similar (p=0.399) between recognized and unrecognized MI, and the mortality was significantly worse (p<0.001) for those with unrecognized MI versus those without MI based on the log rank test.
After adjusting for age, gender, diabetes, and recognized MI, UMI by CMR remained associated with mortality (HR 1.45 CI 1.02–2.06; absolute risk increase 8%), but UMI by ECG was not associated with mortality (HR 0.88 (CI 0.45–1.73; absolute risk increase −2%). Similarly, UMI by CMR significantly improved the classification of those at risk for mortality (category free NRI 0.16; CI 0.01–0.31, p=0.042) but UMI by ECG did not (NRI: −0.05; CI −0.17– 0.05). Finally, UMI by CMR significantly improved mortality risk stratification (absolute IDI 0.008, CI 0.004–0.013, p<0.001), but UMI by ECG did not improve mortality risk stratification (IDI 0.000 (CI −0.001−0.001; p=0.71).
Treatment Differences
We observed more use of aspirin, beta-blocker, and statin medications in those with UMI by CMR compared to those without MI. Yet, the use of cardiac medications was significantly less in those with UMI compared to those with recognized MI (Table 3). Roughly half of those with UMI were taking aspirin, whereas less than half were taking statins or beta-blockers.
Discussion
Using CMR with a conservative interpretation scheme to detect MI in a cohort of community-dwelling, older people, we found a high overall prevalence of UMI. More participants had UMI (17%) than recognized MI (9.7%) resulting in a much higher fraction of the population being identified as having an MI (26%). Individuals with diabetes had a particularly high prevalence of UMI (21%), underscoring the designation of diabetes as a coronary risk equivalent,6 but the pattern of more UMI than recognized MI was also true in those without diabetes. Participants with UMI by CMR had higher coronary calcium, a higher prevalence of atherosclerotic disease, and a higher prevalence of traditional risk factors compared to those with no MI. CMR was more sensitive than ECG in detecting UMI. UMI detected by CMR was associated with subsequent mortality over 6–7 years, but UMI detected by ECG was not. Compared with those with recognized MI, participants with UMI by CMR received fewer prescriptions for medications used to prevent cardiovascular events. Considering the prevalence of UMI (17%) was higher than the prevalence of RMI (10%), many people might conceivably benefit from more intensive preventive “post-MI” therapy, but this hypothesis remains untested.
Several factors may contribute to the high prevalence of UMI. First, subclinical coronary plaque rupture occurs frequently, particularly in diabetic individuals.21 CMR may detect the myocardial sequelae of coronary plaque rupture or coronary plaque erosion21 that either spontaneously reperfused or were non-occlusive. Second, symptom variation in acute MI 22 may lead patients or their clinicians to attribute MI symptoms to noncardiac causes. Third, given their propensity to be clinically detected, recognized MI may be more severe than UMI and impart greater lethality.23,24 Survivor bias may also have increased the proportion of those with UMI in this study, but survivors are the only people eligible for “post-MI” secondary prevention.
The high prevalence of UMI highlights the advantages of using CMR for detection in epidemiology studies. While the prevalence of UMI by ECG was similar to prior population studies,1–4 ECG was much less sensitive for detecting UMI than CMR. Prior population studies probably underestimate the prevalence of MI and particularly UMI since they relied on ECG for detection. The mortality risk associated with UMI by ECG is less than previous reports;1,3 smaller sample size, survivor bias, and different health care practices may be factors.
The increased mortality risk associated with UMI detected by CMR in a community based cohort of older individuals is an important finding of this study, since we document a high prevalence of UMI. In fact, we found that the majority of all MI were clinically unrecognized, suggesting a significant public health burden. This association between prevalent UMI and mortality is novel, since prior epidemiology studies relying on ECG data indicated that a minority of MI are clinically unrecognized.1–4 Our study is also the first epidemiology study to associate coronary calcium with evident MI on CMR LGE images. While another smaller study employing LGE in 248 individuals also reported that most MI were unrecognized, the study only sampled 75 year old individuals and cannot determine the association with mortality controlling for age.25 UMI appears to represent an intermediate phenotype in the evolution of coronary heart disease, given its graded association with atherosclerosis risk factors, coronary calcium, overt atherosclerosis, and subsequent mortality risk.
Other studies have associated UMI identified by CMR with adverse outcomes, but these studies were not community-based epidemiology studies; instead, they were conducted in referral populations with higher baseline risk and inherent biases.24,26,27 The relative risk of UMI may be higher in these studies due to referral biases not present in our community based population study. Nonetheless, the current study indicates that the adverse outcomes associated with UMI extend to the community. Our study also indicates that CMR is more robust at detecting MI and more strongly associated with mortality compared to ECG – an observation with important implications for future epidemiology studies of UMI.
Several lines of evidence establish that the designation of UMI represents true MI.10,14,16,28,29 First, CMR scans were interpreted conservatively. Specifically, “atypical” patterns of enhancement seen with conditions unrelated to coronary disease were not designated as MI. Second, the prevalence of risk factors for CHD or established atherosclerotic disease documented multiple associations of UMI by CMR with atherosclerosis. Kim et al. have also shown associations between coronary disease and UMI.27 Finally, the association between UMI detected by LGE and mortality also supports the diagnosis of MI.
This investigation also suggests limitations in current prevention strategies. Herein we report a burden of MI in community dwelling older individuals that is higher than previously appreciated. In fact, the burden of UMI was higher than the total burden of recognized MI, and prescription of cardioprotective medications were less than for participants with recognized MI. The high prevalence of MI specifically in diabetic individuals confirms their increased vulnerability. Less than one third of those with UMI by CMR had prior revascularization to establish coronary disease and trigger secondary prevention strategies. Detection of UMI by CMR may provide an opportunity optimize management of these vulnerable individuals. Further study is needed to define optimal treatment strategies for those with UMI.
Limitations
The AGES–Reykjavik cohort provides results that are most applicable to Caucasian participants, and may not extend to other ethnicities. The sensitivity of CMR for detecting chronic MI using a 0.1 mmol/kg gadolinium contrast dose in our study may be lower compared to higher doses.16 However, if our study actually had low sensitivity, then the ‘true’ prevalence of MI would be higher. Mitigating the issue of contrast dose, the phase sensitive LGE18 method used in this study has better signal to noise ratio at low contrast doses than conventional LGE methods. In the minority of participants with both UMI and prior coronary revascularization, we could not ascertain whether UMI occurred independently or as a clinically unappreciated consequence of revascularization. Nonetheless, revascularization complications do not explain the high prevalence of UMI since the prevalence of UMI in diabetic and nondiabetic participants remained high even after excluding prior coronary revascularization. We also did not examine more subtle ECG changes that may be associated with MI. Risk adjustment was limited. This study was designed to demonstrate comparable prognosis between UMI and recognized MI; it was not powered to permit extensive risk adjustment for all baseline differences.
Conclusions
Older individuals in the community had a high prevalence of MI, especially those with diabetes. Most MI were unrecognized, despite associations with atherosclerosis, risk factors, and health care advances. CMR with LGE detected more UMI and was more strongly associated with mortality than ECG. UMI detected by CMR with LGE was associated with mortality similar to recognized MI. Participants with UMI received less cardiac medications than those with recognized MI.
Supplementary Material
Acknowledgements
The study sponsors did not have a role with regard to design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. This study was funded by the National Institute of Heart, Lung and Blood Intramural Research Program (Z01 HL004607-08 CE), the National Institute on Aging Intramural Research Program (contract N01-AG-12100), Hjartavernd (the Icelandic Heart Association), and the Althingi (the Icelandic Parliament). The study was approved by the Icelandic National Bioethics Committee (VSN: 00-063) and the Medstar Research Institute (Project #2003-145). Dr Schelbert is supported by a T. Franklin Williams Scholarship Award; funding provided by: Atlantic Philanthropies, Inc, the John A. Hartford Foundation, the Association of Specialty Professors, and the American Heart Association. Dr. Cao is supported by an American Heart Association Grant-in-Aid 10GRNT4580000. Drs. Schelbert and Arai had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Contributors: Author contributions to this manuscript were as follows: 1) Design - All authors, 2) Acquisition - SS, PK, AHA, GE, AEA, 3) Analysis – EBS, JJC, SS, TA, VG, AEA, 4) Writing - EBS, JJC, LJL,VG, TBH, AEA, 5) Review – all authors, 6) Final Responsibility - EBS, LJL,VG, TBH, AEA
The authors have no conflicts of interest to disclose.
References
- 1.Sigurdsson E, Thorgeirsson G, Sigvaldason H, Sigfusson N. Unrecognized myocardial infarction: epidemiology, clinical characteristics, and the prognostic role of angina pectoris. The Reykjavik Study. Annals of internal medicine. 1995 Jan 15;122(2):96–102. doi: 10.7326/0003-4819-122-2-199501150-00003. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study. N Engl J Med. 1984 Nov 1;311(18):1144–1147. doi: 10.1056/NEJM198411013111802. [DOI] [PubMed] [Google Scholar]
- 3.Sheifer SE, Gersh BJ, Yanez ND, 3rd, Ades PA, Burke GL, Manolio TA. Prevalence, predisposing factors, and prognosis of clinically unrecognized myocardial infarction in the elderly. J Am Coll Cardiol. 2000 Jan;35(1):119–126. doi: 10.1016/s0735-1097(99)00524-0. [DOI] [PubMed] [Google Scholar]
- 4.Boland LL, Folsom AR, Sorlie PD, et al. Occurrence of unrecognized myocardial infarction in subjects aged 45 to 65 years (the ARIC study) Am J Cardiol. 2002 Nov 1;90(9):927–931. doi: 10.1016/s0002-9149(02)02655-3. [DOI] [PubMed] [Google Scholar]
- 5.Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000 Nov 16;343(20):1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 6.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002 Dec 17;106(25):3143–3421. [PubMed] [Google Scholar]
- 7.Burke AP, Kolodgie FD, Farb A, et al. Healed plaque ruptures and sudden coronary death: evidence that subclinical rupture has a role in plaque progression. Circulation. 2001 Feb 20;103(7):934–940. doi: 10.1161/01.cir.103.7.934. [DOI] [PubMed] [Google Scholar]
- 8.Horan LG, Flowers NC, Johnson JC. Significance of the diagnostic Q wave of myocardial infarction. Circulation. 1971 Mar;43(3):428–436. doi: 10.1161/01.cir.43.3.428. [DOI] [PubMed] [Google Scholar]
- 9.Cox CJ. Return to normal of the electrocardiogram 353 after myocardial infarction. Lancet. 1967 Jun 3;1(7501):1194–1197. doi: 10.1016/s0140-6736(67)92843-7. [DOI] [PubMed] [Google Scholar]
- 10.Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999 Nov 9;100(19):1992–2002. doi: 10.1161/01.cir.100.19.1992. [DOI] [PubMed] [Google Scholar]
- 11.Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet. 2003 Feb 1;361(9355):374–379. doi: 10.1016/S0140-6736(03)12389-6. [DOI] [PubMed] [Google Scholar]
- 12.Klein C, Nekolla SG, Bengel FM, et al. Assessment of myocardial viability with contrast-enhanced magnetic resonance imaging: comparison with positron emission tomography. Circulation. 2002 Jan 15;105(2):162–167. doi: 10.1161/hc0202.102123. [DOI] [PubMed] [Google Scholar]
- 13.Harris TB, Launer LJ, Eiriksdottir G, et al. Gene/Environment Susceptibility-Reykjavik Study: multidisciplinary applied phenomics. American journal of epidemiology. 2007 May 1;165(9):1076–1087. doi: 10.1093/aje/kwk115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu E, Judd RM, Vargas JD, Klocke FJ, Bonow RO, Kim RJ. Visualisation of presence, location, and transmural extent of healed Q-wave and non-Q-wave myocardial infarction. Lancet. 2001 Jan 6;357(9249):21–28. doi: 10.1016/S0140-6736(00)03567-4. [DOI] [PubMed] [Google Scholar]
- 15.Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005 Aug;26(15):1461–1474. doi: 10.1093/eurheartj/ehi258. [DOI] [PubMed] [Google Scholar]
- 16.Kim RJ, Albert TS, Wible JH, et al. Performance of delayed-enhancement magnetic resonance imaging with gadoversetamide contrast for the detection and assessment of myocardial infarction: an inter 376 national, multicenter, double-blinded, randomized trial. Circulation. 2008 Feb 5;117(5):629–637. doi: 10.1161/CIRCULATIONAHA.107.723262. [DOI] [PubMed] [Google Scholar]
- 17.Genuth S, Alberti KG, Bennett P, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003 Nov;26(11):3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 18.Kellman P, Arai AE, McVeigh ER, Aletras AH. Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement. Magn Reson Med. 2002 Feb;47(2):372–383. doi: 10.1002/mrm.10051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pencina MJ, D'Agostino RB, Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011 Jan 15;30(1):11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kennedy KF, Pencina MJ. [Accessed June 1, 2011];A SAS® Macro to Compute Added Predictive Ability of New Markers Predicting a Dichotomous Outcome. 2010 http://analytics.ncsu.edu/sesug/2010/SDA07.Kennedy.pdf.
- 21.Burke AP, Virmani R. Pathophysiology of acute myocardial infarction. Med Clin North Am. 2007 Jul;91(4):553–572. doi: 10.1016/j.mcna.2007.03.005. ix. [DOI] [PubMed] [Google Scholar]
- 22.Schelbert EB, Rumsfeld JS, Krumholz HM, et al. Ischaemic symptoms, quality of care and mortality during myocardial infarction. Heart. 2008 Feb;94(2):e2. doi: 10.1136/hrt.2006.111674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burns RJ, Gibbons RJ, Yi Q, et al. The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. J Am Coll Cardiol. 2002 Jan 2;39(1):30–36. doi: 10.1016/s0735-1097(01)01711-9. [DOI] [PubMed] [Google Scholar]
- 24.Kwong RY, Chan AK, Brown KA, et al. Impact of unrecognized myocardial scar detected by cardiac magnetic resonance imaging on event-free survival in patients presenting with signs or symptoms 399 of coronary artery disease. Circulation. 2006 Jun 13;113(23):2733–2743. doi: 10.1161/CIRCULATIONAHA.105.570648. [DOI] [PubMed] [Google Scholar]
- 25.Barbier CE, Nylander R, Themudo R, et al. Prevalence of unrecognized myocardial infarction detected with magnetic resonance imaging and its relationship to cerebral ischemic lesions in both sexes. J Am Coll Cardiol. 2011 Sep 20;58(13):1372–1377. doi: 10.1016/j.jacc.2011.06.028. [DOI] [PubMed] [Google Scholar]
- 26.Kwong RY, Sattar H, Wu H, et al. Incidence and prognostic implication of unrecognized myocardial scar characterized by cardiac magnetic resonance in diabetic patients without clinical evidence of myocardial infarction. Circulation. 2008 Sep 2;118(10):1011–1020. doi: 10.1161/CIRCULATIONAHA.107.727826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim HW, Klem I, Shah DJ, et al. Unrecognized non-Q-wave myocardial infarction: prevalence and prognostic significance in patients with suspected coronary disease. PLoS Med. 2009 Apr 21;6(4):e1000057. doi: 10.1371/journal.pmed.1000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rehwald WG, Fieno DS, Chen EL, Kim RJ, Judd RM. Myocardial magnetic resonance imaging contrast agent concentrations after reversible and irreversible ischemic injury. Circulation. 2002 Jan 15;105(2):224–229. doi: 10.1161/hc0202.102016. [DOI] [PubMed] [Google Scholar]
- 29.Schelbert EB, Hsu LY, Anderson SA, et al. Late gadolinium-enhancement cardiac magnetic resonance identifies postinfarction myocardial fibrosis and the border zone at the near cellular level in ex vivo rat heart. Circ Cardiovasc Imaging. 2010 Nov 1;3(6):743–752. doi: 10.1161/CIRCIMAGING.108.835793. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.