Abstract
Objective
Guided by the Attitude-Social influence-self Efficacy (ASE) theory, this study identified predictors of waterpipe (WP) smoking initiation in a WP naïve cohort of Jordanian schoolchildren.
Methods
A school-based cohort of all 7th grade students (N=1,781) in 19 of 60 schools in Irbid, Jordan, was followed from 2008 to 2011. Generalized linear mixed modeling was used to examine predictors of WP initiation among WP-naïve students (N=1,243).
Results
During the 3-year study, WP initiation was documented in 39% of boys and 28% of girls. Prior cigarette smoking (boys: Odds Ratio 7.41; 95% Confidence Interval 4.05–12.92 and girls: 8.48; 4.34–16.56) and low WP refusal self-efficacy (boys: 26.67; 13.80–51.53 and girls: 11.49; 6.42–20.55) were strongly predictive of initiating WP. Boys were also more likely to initiate WP smoking if they had siblings (2.30; 1.14- 4.64) or teachers (2.07; 1.12–3.84) who smoked and girls if they had friends (2.96; 1.59–5.54) who smoked.
Conclusion
There is a sizeable incidence of WP initiation among students of both sexes. These findings will help in designing culturally responsive prevention interventions against WP smoking. Gender-specific factors, refusal skills, and cigarette smoking need to be important components of such initiatives.
Keywords: cohort, gender, initiation, Jordan, schoolchildren, waterpipe smoking
1. INTRODUCTION
The global spread of waterpipe (WP) smoking among adolescents is widely documented (Centers for Disease Control and Prevention, 2013; Maziak, 2011; Mzayek et al., 2011; Primack et al., 2009; Parna et al., 2008; Maziak et al., 2004b; Maziak, 2013; Warren et al., 2009; Amrock et al., 2014). While the evidence is still preliminary, it suggests that WP smoking is as addictive and detrimental to health as cigarette smoking (Maziak et al., 2011; Rastam et al., 2011; Eissenberg and Shihadeh, 2009; Fromme et al., 2009; Al Rashidi et al., 2008). Prevalence of WP smoking is high among school children in other parts of the world and is increasing among adolescents in the US (Martinasek et al., 2011; Maziak and Mzayek, 2000; Mzayek et al., 2012; Weglicki et al., 2008; Barnett et al., 2013; Warren et al., 2009). A recent review by Akl et al. (2011) reported prevalence for current WP smoking among school students in Estonia and Lebanon to be 21% and 25% respectively; with estimates ranging from 12% −15% for Arab-Americans. In the US, a recent national survey of WP use among adolescents revealed ever-WP smoking prevalence of 7.3% and of large survey involving more than 100,000 students in 152 colleges found the prevalence of waterpipe smoking was 8.4%, second only to cigarettes (16.8%) (Primack et al., 2013). Waterpipe popularity is partly fueled by the widespread misperception that it is safer alternative to cigarettes (Akl et al., 2013; Roskin and Aveyard, 2009; Eissenberg et al., 2008; Maziak et al., 2004). Evidence, however, shows that WP smoking is likely to be associated with many of the health risks of cigarette smoking such as lung cancer, respiratory disease, periodontal disease, and low birth-weight (Akl et al., 2010). Additionally, there are reports of associations between communal WP smoking and increased rates of Helicobacter pylori, hepatitis A, hepatitis C, herpes simplex, and Epstein-Barr virus (Meleigy, 2007). Finally, Torrey et al. (2014) found indoor airborne concentrations of particulate matter and carbon monoxide were higher in WP cafes than in cigarette smoking bars (in Baltimore, MD) and exceeded occupational exposure guidelines; suggesting that both patrons and employees of WP venues are at increased risk from exposure to second hand smoke.
Despite the adverse public health implications of this resurging smoking method, there are no effective prevention or intervention strategies to curb its spread (Maziak et al., 2007, 2005). One of the reasons that such efforts are delayed lies in the lack of knowledge about early stages of WP adoption and important factors influencing initiation. Most of the work about WP initiation has been based on cross-sectional studies and/or lacked guidance of an appropriate theoretical model of behavioral change (Asfar et al., 2005; Fielder et al., 2012, 2013; Islam and Johnson, 2003; Kassim et al., 2013; Knishkowy and Amitai, 2005; Kulwicki and Hill-Rice, 2003; Martinasek et al., 2011; Primack et al., 2009; Ribisl, 2012; Rice et al., 2003, 2006; Weglicki et al., 2008). Recently, two longitudinal studies assessing predictors of WP initiation were conducted among college students in the US (Fielder et al., 2012; Sidani et al., 2013). While both studies reported high rates of initiation; they also reported high prevalence of ever-WP smoking at baseline, which emphasizes the need to study WP initiation dynamics at an earlier age. This evidence is in line with studies worldwide that suggest much of WP initiation occurs at younger ages (Barnett et al., 2013; Akl et al., 2011; Martinasek et al., 2011; Nasim et al., 2012; Prokhorov et al., 2006; Warren 2002; Amrock et al., 2014).
To address this knowledge gap, we employed the Attitude–Social influence–self-Efficacy (ASE) model as a framework for variable selection and interpretation (de Vries et al. 1988, 2003). The ASE model incorporates insights from other tested and validated social cognitive theories, and suggests that behavior is the result of intentions and abilities, whereby motivational factors, such as various attitudes, social influences, and self-efficacy determine intention, while abilities and environmental barriers (e.g., availability, restrictions) determine whether intentions will be realized (Ajzen, 1991; Bandura, 2001). Within this framework, gender is not a central focus; however, gender differences in determinants of adolescent smoking initiation are widely documented and evidence also points to differential effects of smoking prevention and cessation interventions by gender (Amos et al., 2012; Austin and Gortmaker, 2001; Babar et al., 2010; Greaves, 2007; Nichter, 2003; Okoli et al., 2013; Rice et al., 2003; Trudeau et al., 2007; Zhu et al., 1996). Moreover, the defined gender roles found in Jordan are likely to influence smoking uptake differently for boys compared to girls (Maziak et al., 2004; Nichter, 2003). This longitudinal study, guided by the ASE model, examined gender specific predictors of WP initiation among WP naïve school children in Jordan.
2. METHODS
Detailed description of the methodology from this study is published elsewhere (Mzayek et al., 2012, 2011). Briefly, from 2008 to 2011, a school-based cohort of 7th graders (at baseline) was surveyed annually through 10th grade in the city of Irbid, Jordan. The 60 schools in the city of Irbid (Jordan) were stratified by gender (boys, girls, mixed) and type of school attended (public and private). A cluster random sample of 19 schools (8 male, 9 female, 2 mixed and 6 private) was selected with probability proportional to size (PPS). All 7th grade students (age ≈ 13 at baseline) in the selected schools were invited to participate. All selected schools and 95% of the students approached (N=1,781) agreed to participate in the study.
This study was reviewed and approved by the institutional review boards of Jordan University for Science and Technology, University of Memphis, Syrian Society Against Cancer and Florida International University.
2.1 Survey instrument
Development of the study questionnaire was guided by the international guidelines of the World Health Organization (WHO; World Health Organization 1998), other previously used and validated instruments in Arabic and it was subsequently pilot-tested (Maziak et al., 2005; Warren, 2002). The questionnaire included four modules: socio-demographics; cigarette smoking; waterpipe smoking; and media and tobacco control.
2.2 Measures
Initiation of WP was the main outcome. Initiation was defined as the change from never smoker (of WP) at baseline to ever smoker or current smoker (of WP) at any subsequent follow-up survey(s). A student was considered an ever smoker if he/she reported ever experimenting with smoking and a current smoker if he/she reported having smoked in the last 30 days. Assessed theoretical domains and corresponding survey questions are shown in Table 1. Variables were selected by choosing questions on our questionnaire that corresponded to domains in the ASE model as described in previous studies (Kremers et al., 2004; de Vries et al., 1988; Bidstrup et al., 2009; Ma et al., 2008). Density Index (DI) is the number of persons living in a dwelling divided by the number rooms in a home (minus kitchen and bathrooms), which is a proxy for economic status that was used and tested previously in the Middle East (Maziak et al., 2004; Maziak and Asfar, 2003).
Table 1.
Survey questions with corresponding Attitude-Self efficacy-Social influence theoretical model domains and baseline characteristics of school based cohort (N=1,243) of Jordanian school children age ≈13 at baseline, Irbid, Jordan, 2008–2011 (waterpipe initiators versus waterpipe non-initiators)
|
Theoretical Domain |
Survey Questions |
Initiators (n=458) |
Non- initiators (n=785) |
|
|---|---|---|---|---|
| ASE | ||||
| n (%)* | n (%)* | |||
| Predisposing/Demographics | What is your gender? (male) | 256 (53.0) | 305 (40.8) | |
| Have you ever smoked a cigarette, even a puff or two? | 47 (10.4) | 40 (6.0) | ||
| Do you attend public school? | 412 (85.2) | 641 (67.2) | ||
| How old are you? mean (SD) | 12.7 (0.6) | 12.6 (0.6) | ||
| Density Index,b mean (SD) | 1.6 (0.9) | 1.7 (1.1) | ||
| How many years of education does your father have? (>High School) |
145 (33.1) | 273 (40.4) | ||
| How many years of education does your mother have? (>High School) |
104 (25.3) | 190 (27.7) | ||
| How much is your daily allowance? (≥0.50 JOD)c | 73 (18.6) | 120 (19.3) | ||
| Awareness | Do you think smoking WP is harmful for your health? | 421 (92.1) |
710 (90.8) |
|
| Information | Have you seen pro smoking ads in the media in the past month? |
215 (47.0) | 343 (43.6) | |
| Have you seen ads warning about dangers of smoking on health in the media in the past month? |
361 (79.8) | 633 (82.3) | ||
| Have you seen warnings on WP tobacco packaging in the past month? |
196 (42.4) | 302 (35.6) | ||
| Has a family member talked to you about the dangers of WP smoking? |
298 (66.8) | 510 (65.8) | ||
| Motivation | ||||
| Attitude | Do you think students who smoke WP have more friends? |
114 (23.5) | 197 (25.4) | |
| Do you think student who smoke WP are more attractive? |
141 (46.2) | 203 (41.4) | ||
| Do you think smoking WP affects body weight? (lose weight) | 222 (49.0) | 397 (51.1) | ||
| Do you think it is easy to stop smoking WP after smoking for year or two? |
151 (35.1) | 244 (32.7) | ||
|
Social Influence |
Does your family know you smoke cigarettesa? | 10 (23.8) | 10 (29.8) | |
| Do your parent(s) smoke waterpipe? | 116 (28.6) | 164 (20.3) | ||
| Do your sibling(s) smoke waterpipe? | 52 (11.0) | 69 (9.3) | ||
| Do you have close friends who smoke waterpipe? | 108 (22.3) | 133 (18.7) | ||
| Have you seen actors on TV smoking? | 396 (87.8) | 679 (88.0) | ||
| Do your teachers smoke in front of students? | 198 (42.0) | 212 (23.3) | ||
| Self Efficacy | Would you accept WP from friends if offered? | 52 (12.4) | 39 (6.2) | |
| Intention | Do you think that you may start to smoke WP next year? | 42 (9.3) | 61 (8.3) | |
p<0.05 indicated in bold.
Weighted proportions reported to account for complex sampling design.
n=47 for initiators and n=40 for non-initiators for ever smokers of cigarette at baseline
Density Index was calculated by dividing the number of people living in each participant’s home by the number of rooms (minus kitchen and bathroom) in the home.
In Jordanian Dinars (JOD) (1JOD=1.41USD)
2.3 Statistical analysis
All statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, 2011). The cohort for this analysis was derived from WP-naïve participants at baseline (N=1,243). Baseline characteristics were compared between WP initiators and non-WP initiators using chi-square test for categorical variables and t-test for continuous variables. The cohort was then stratified by gender for regression analysis. SAS Proc GLIMMIX was used, which accounted for clustering of schools and the repeated measures during the follow-up in students. Questions with more than two possible response categories were analyzed in two ways: once as they were originally obtained, and the second time as binary. The variables were dichotomized by combining responses such as maybe and sometimes with yes. I don’t know answers were excluded from the analysis. We also combined mother and father into parents and brother and sister into siblings. The results were robust, whether we used multiple categories or binary categories; binary categories were used for clarity of reporting (DeCoster, 2009).
Bivariate correlations for all predictor variables revealed no multicollinearity problems. This was also inspected by checking for extraordinary estimated coefficients and standard errors, which would have suggested the existence of colinearity. A full(er) model as described by Flom and colleagues (2007), that included all potential predictor variables, was then fitted using SAS proc GLIMMIX to find adjusted effects of each variable on initiation.
Odds ratios (OR) and 95% confidence intervals (CI) were reported. P-values of <0.05 were considered significant. Weighted proportions to adjust for complex sampling design were reported throughout.
3. RESULTS
3.1 Characteristics of sample
Baseline characteristics of 1,243 WP initiating and non-WP initiating participants are shown in Table 1. The participants who initiated WP were less likely to have fathers with more than a high school education; to have attended a public school; and to have reported they would accept WP from a friend.
3.2 Smoking initiation incidence
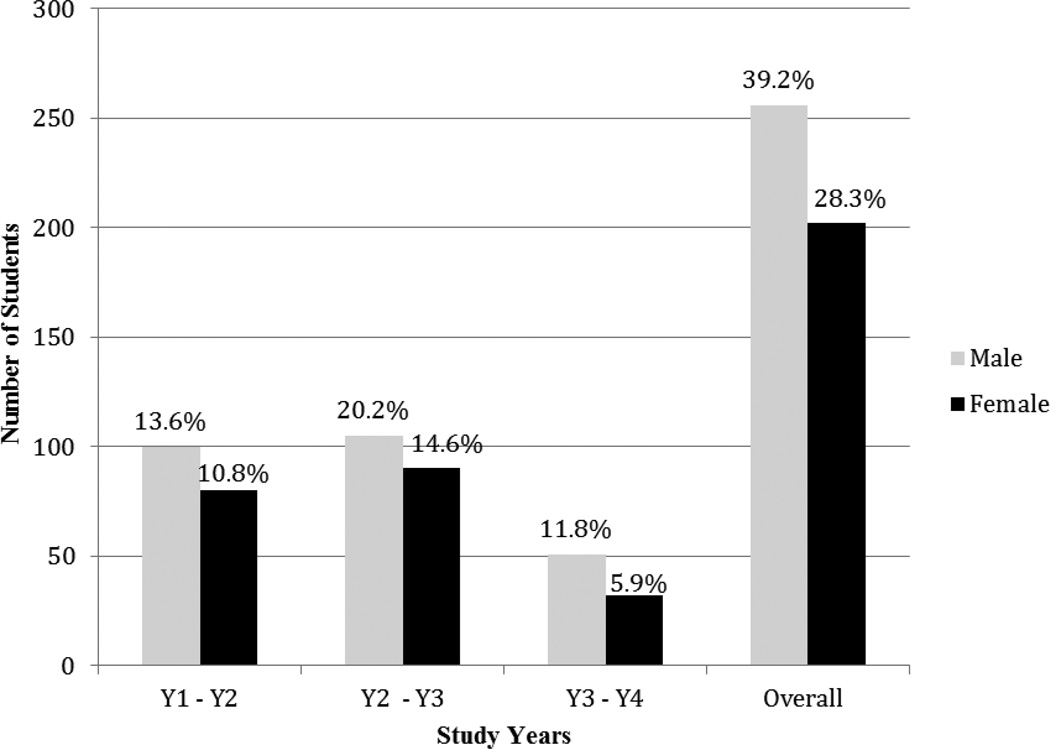
Over the study period of 4 years, 36.8% of participants initiated WP (39.2% of boys and 28.3% of girls). The largest proportion of participants initiated WP smoking at age ≈14, in the 8th grade (Figure 1).
Figure 1.
Number of students initiating waterpipe by gender and year of follow up (2008–2011), Irbid, Jordan
Standardized proportions are reported
3.3 Association of ASE variables and WP smoking initiation by tenth grade
The results of the longitudinal analyses assessing the relationship between WP initiation by 10th grade and potential predictor variables, stratified by gender, are summarized in Table 2. Socio-economic status was not associated with WP smoking initiation in this sample. Previous cigarette smoking and low refusal self-efficacy were strongly associated with WP initiation. Teacher and sibling smoking were associated with initiation among boys while having friends who smoke was associated with initiation among girls. Awareness that WP smoking is harmful for health was protective against initiation (details in Supplementary Table1).
Table 2.
Predictors of Waterpipe Smoking initiation, by gender, among school based cohort of school children aged 13 at baseline, Irbid, Jordan, 2008–2011: longitudinal analysis (N=1,243)
|
Theoretical Domain |
Potential Predictor Variablesa | Boys (n=561) | Girls (n=682) | ||
|---|---|---|---|---|---|
| OR (95%CI) | AOR* (95%CI) | OR (95%CI) | AOR* (95%CI) | ||
| Predisposing | Smoke cigarettes | 7.17 (5.03, 10.20) | 7.41 (4.05, 12.92) | 9.93 (6.55, 15.05) | 8.48 (4.34, 16.56) |
| Density Indexb (continuous)** | 0.89 (0.74, 1.07) | 1.07 (0.80, 1.43) | 0.91 (0.74, 1.11) | 1.02 (0.72, 1.45) | |
| Mother’s education (> High School) | 1.09 (0.76, 1.56) | 1.95 (0.93, 4.07) | 0.69 (0.46, 1.04) | 0.56 (0.24, 1.28) | |
| Father’s education (> High School) | 0.85 (0.59, 1.22) | 0.53 (0.25, 1.12) | 0.61 (0.41, 0.91) | 1.28 (0.58, 2.81) | |
| Daily allowance (≥0 .50 JOD)c | 1.67 (1.21, 2.30) | 1.45 (0.76, 2.78) | 1.06 (0.76, 1.47) | 0.56 (0.24, 1.28) | |
| Age in years (continuous) | 1.19 (1.03, 1.37) | 0.80 (0.60, 1.06) | 1.06 (0.92, 1.24) | 0.84 (0.60, 1.16) | |
| Participation in sports | 3.43 (1.94, 6.07) | 4.28 (1.60, 11.43) | 1.29 (0.82, 2.02) | 0.68 (0.31, 1.49) | |
| Information | Propaganda encouraging smoking | 1.28 (0.92, 1.78) | 1.11 (0.62, 2.00) | 1.20 (0.87, 1.66) | 1.50 (0.84, 2.69) |
| Propaganda warning about smoking | 0.89 (0.62, 1.28) | 0.88 (0.46, 1.67) | 0.72 (0.48, 1.06) | 2.15 (0.96, 4.82) | |
| Warning labels on WP tobacco packages | 1.82 (1.31, 2.52) | 1.46 (0.81, 2.62) | 1.80 (1.30, 2.50) | 1.22 (0.68, 2.22) | |
| Warning of WP dangers from family | 0.89 (0.62, 1.28) | 1.87 (0.92, 3.81) | 0.66 (0.47, 0.93) | 0.82 (0.44, 1.50) | |
| Awareness | Believe WP is bad for health | 0.38 (0.24, 0.59) | 0.39 (0.17,0.88) | 0.34 (0.20, 0.59) | 0.36 (0.13, 0.98) |
| Motivation | Parent(s) smoke WP | 2.10 (1.44, 3.06) | 1.06 (0.56, 2.03) | 3.53 (2.53, 4.94) | 1.79 (0.97, 3.33) |
| Sibling(s) smoke WP | 2.42 (1.55, 3.78) | 2.30 (1.14, 4.64) | 3.14 (2.14, 4.62) | 1.37 (0.71, 2.63) | |
| Friends smoke WP | 3.37 (2.35, 4.84) | 0.68 (0.36, 1.29) | 5.82 (4.09, 8.29) | 2.96 (1.59, 5.54) | |
| Seen TV actors smoke in past 30 days | 1.01 (0.64, 1.58) | 0.47 (0.23, 0.99) | 0.86 (0.50, 1.51) | 0.47 (0.18, 1.23) | |
| Teachers smoke around students | 1.01 (0.64, 1.58) | 2.07 (1.12, 3.84) | 1.53 (1.02, 2.29) | 1.44 (0.73, 2.85) | |
| Accept WP from friendsd | 22.05 (14.78, 32.90) | 26.67 (13.80, 51.53) | 20.52 (13.80, 30.52) | 11.49 (6.42, 20.55) | |
| Believe have more friends if smoke WP | 1.10 (0.75, 1.60) | 0.89 (0.46, 1.75) | 0.84 (0.53, 1.33) | 0.46 (0.19, 1.11) | |
| Believe more attractive if smoke WP | 1.35 (0.93, 1.97) | 1.24 (0.61, 2.54) | 1.79 (1.22, 2.62) | 1.31 (0.61, 2.81) | |
| WP weight belief = lose weight | 0.93 (0.67, 1.30) | 1.05 (0.59, 1.85) | 0.80 (0.58, 1.10) | 0.88 (0.49, 1.58) | |
| Easy to quit after smoking WP year or twod | 2.00 (1.44, 2.78) | 1.35 (0.86, 2.14) | 1.31 (0.92, 1.85) | 0.76 (0.45, 1.27) | |
| Intention | Intend to start smoking WP next yeard | 17.52 (11.87, 25.84) | 8.83 (5.08, 15.35) | 11.05 (7.40, 16.51) | 4.43 (2.39, 8.21) |
OR = Odds Ratio; AOR = Adjusted Odds Ratio; CI = Confidence Interval
AOR for each variable is adjusted for all other variables in the model. Statistically significant adjusted odds ratios (P-value < 0.05) are in bold.
For continuous variables, the OR approximates the risk change for every one-unit increase in the DI or one year increase in age.
No is the referent category
Density Index was calculated by dividing the number of people living in each participant’s home by the number of rooms (minus kitchen and bathroom) in the home.
In Jordanian Dinars (JOD) (1JOD=1.41USD)
Due to suppression effect, AOR for quit belief was not adjusted for intention or self-efficacy. Likewise, intention was not adjusted for quit belief or self-efficacy; nor was self-efficacy was adjusted for quit belief or intention. See text for detailed explanation.
Initial analysis indicated significant effects of quit belief (Is it easy to quit smoking WP after smoking for a year or two?) on WP initiation among girls [OR 0.47; (0.24, 0.94)], these results were not interpretable due to a suppression effect concerning quit belief (Tu et al., 2008). Quit belief was not correlated with the outcome (Spearman’s ρ .078; p < .150). However, quit belief was significantly related to self-efficacy (If a friend offers you a WP would you smoke it?) (Spearman’s ρ = .154; p < .01), and further analyses showed suppression to take place when self-efficacy and/or intention and quit belief enter the model simultaneously. Self-efficacy was strongly related with intention (Do you believe you will start smoking WP in the next year?) (Spearman’s ρ = .546; p < .01) and both self-efficacy (.451; p< .01) and intention (437; p< .01) were associated with the outcome. Therefore, we estimated models with each of these variables adjusted for all predictor variables, except the other two (e.g., self-efficacy was not adjusted for intention or quit belief). When quit belief was entered into the model without self-efficacy and intention, its association with the outcome was no longer significant.
4. DISCUSSION
Results of this study reveal annual incidence rates of WP initiation ranging from 6% - 20% in schoolchildren followed from the 7th to the 10th grade. Over a third of youths initiated WP during the study period. Those who took up WP smoking were more likely to attend a public (vs. private) school and have parents with less than a high school education. More boys than girls initiated WP during this time and most participants initiated around age 14. The young age of initiation may reflect early exposure to the socially accepted practice of WP smoking by family and friends. (McKelvey et al., 2013). Although this study did not seek to test a health behavior theory, the study findings lend some support for use of ASE-based variables in explaining WP smoking behaviors among youth in our study. Among predisposing variables, current cigarette smoking was associated with increased risk of WP initiation for boys and girls, and current involvement with sports was associated with increased risk for boys. Awareness about dangers of smoking was associated with decreased odds of initiation for boys and girls. Social influences to smoke were motivational risk factors for both boys and girls; however, effects differed by gender: for boys, social influences were sibling and teachers smoking and for girls it was friends smoking. Low refusal self-efficacy was another motivational factor and was strongly associated with initiation across genders. Finally the odds of WP initiation were greater among those with an intention to smoke WP within the next year. These findings suggest that interventions should begin early, and target youth who attend public schools, and have not yet smoked. Effective interventions could include skill building to enhance children’s refusal self-efficacy and resistance to social cues to smoke.
Research on the association between SES and adolescent cigarette smoking initiation has been mixed with some studies reporting a null association (Miller et al., 2006; O’Loughlin et al., 2009) and others reporting an increased risk of adolescent smoking initiation associated with lower SES (Morgenstern et al., 2013). Our finding of a null association between adolescent WP smoking initiation and SES is likely due to the widespread availability and commonplace nature of WP smoking in Jordan. WP smoking is a traditional social practice shared among friends and family in cafés, homes, and other natural settings where people gather. (Blank et al., 2014; Roskin and Aveyard, 2009).
Although research on risk factors for WP initiation among adolescents is nonexistent, the temporal precedence of many predictors identified here fit with earlier longitudinal studies on adolescent cigarette smoking initiation (O’Loughlin et al., 2009; Miller et al., 2006; Morgenstern et al., 2013; Bidstrup et al., 2009; Hiemstra et al., 2011; Scal et al., 2003; Ma et al., 2008; Vitória et al., 2011; Skara et al., 2001; Stanton et al., 2005; Chang et al., 2006; Fujimoto et al., 2012; Wood et al., 2013; Tyas and Pederson, 1998). Research has frequently shown that predisposing factors such as use of other tobacco products is predictive of cigarette initiation (O’Loughlin et al., 2009; Mzayek et al., 2012). Some research has also shown that the peer influence common in team sports is associated with smoking behavior and that involvement in certain sports may be related to risk-taking, impulsivity, and consequently tobacco and other substance use (Wood et al., 2013; Fujimoto et al., 2012). It is possible that youth who are attracted to the social nature of team sports may also be attracted to the social nature of WP, an activity usually shared in a group (Blank et al., 2014; Maziak and Mzayek, 2000; Amrock et al., 2014). Although the evidence is cross sectional, an association between participation in organized sports and increased odds of WP smoking has been found among American collegiate athletes as well (Primack et al., 2010). The importance of the social environment - such as siblings’, friends’, and peer smoking behaviors, as well as role-model (e.g., teachers) smoking - on cigarette smoking initiation has been underscored repeatedly in the literature (O’Loughlin et al., 2009; Bidstrup et al., 2009; Hiemstra et al., 2011; Scal et al., 2003; Chang et al., 2006). In line with our findings, other studies report the influence of having friends and siblings who smoke is stronger than the influence of having parents who smoke (Bauman et al., 2001; Distefan et al., 1998; Okoli et al., 2013). Also, certain personal factors we found to predict (low refusal self-efficacy) or protect against (health concerns) WP initiation have also been similarly associated with cigarette smoking initiation (Bidstrup et al., 2009; Hiemstra et al., 2011; O’Loughlin et al., 2009; Piko et al., 2005; Scal et al., 2003; Ma et al., 2008; Chang et al., 2006; Tyas and Pederson, 1998). Finally, in line with our findings, studies measuring smoking intention found this domain to be a strong predictor of cigarette initiation (Vitória et al., 2011; Skara et al., 2001; Stanton et al., 2005).
Previous correlations reported in cigarette initiation research were not confirmed here. For instance, seeing actors smoke has been associated with cigarette initiation (Morgenstern et al., 2013). It is likely our participants saw actors smoking cigarettes and not WP and that these modeled behaviors were interpreted by youth as very distinct. Additionally, longitudinal research of cigarette initiation among youth that employed models similar to ASE identified strengths of some ASE domains to predict smoking that were not supported in our study. For example, motivational factors—such as positive attitudes and beliefs about smoking, like believing adolescents who smoke have more friends—have been shown to influence cigarette-smoking uptake (Miller et al., 2006). Two cohort studies employing ASE (Denmark; Bidstrup et al., 2009) and social cognitive theory (Taiwan; Chang et al., 2006) reported an association between adolescent cigarette smoking initiation and positive attitudes toward smoking. Our divergent findings may be due in part to our having stratified the sample by gender. Also, it is likely that attitudes regarding WP smoking in our sample are less pronounced, as the habit is ubiquitous in Jordan, evoking weak, if any, attitudes compared to those that cigarette smoking produces around the world.
A potential weakness of this study was that all responses were self-reported and there may be a higher level of underreporting of smoking by girls due to the social undesirability of smoking among females in this area of the world. However, research among adolescents has shown strong agreement between self-reported smoking rates and those verified with biochemical measures (Brener et al., 2003). Furthermore, our previous research among adolescents in the Middle East has also shown that youth are willing to share honestly about their smoking experience when confidentiality is assured (Maziak and Mzayek, 2000). Another potential limitation is that the ASE model may not sufficiently translate relevant cultural differences. One study examined the application of the ASE model to predict smoking among youth of different countries (Markham et al., 2009). The study found that the association between country of residence and intention to smoke was only partially mediated by ASE factors and that country also moderated cognitive factors associated with smoking intention. Finally, because of sensitivity around religion in the political context of the study setting, we did not include questions of religiosity as it may have reduced participation in this study. Despite these limitations, our study has several strengths that are important to note. This was the first longitudinal study of tobacco use in the Middle East and while the data were collected in one city, the sample was drawn from the entire population of 7th graders in 2008. Our study also collected smoking information simultaneously for both cigarette and waterpipe. The high response and retention rates across four years also add to the strengths of this study.
Finally, it should be noted that while these findings are not directly generalizable to adolescent populations everywhere, having a comprehensive sample of one of the largest cities in a small country like Jordan allows the findings to be generalized to at least other urban populations of the country. Additionally, many countries in the region share a very similar social, cultural and ethnic background; therefore, our findings provide at a minimum a starting point for further research in the region.
Our study found that adolescents’ efficacy to resist invitations to smoke is an important factor in actual WP smoking initiation. The influence of smoking by siblings, teachers, and friends were also predictive of WP initiation among youth in this study, while parental smoking was not. The influence of prior cigarette smoking on WP initiation, along with the mean initiation age (14 years) of this cohort, suggests that interventions need to begin early and target youth who have not yet smoked. Because social self-efficacy, social influences to smoke, and intention to smoke proved to have strong associations with initiation, self-efficacy beliefs and individual intentions to smoke should be included in the future in smoking prevention programs in Jordan. Furthermore, a distinction between the roles of siblings, peers, and teachers should be emphasized when addressing the social environment of adolescents in health promotion. Going forward, prevention interventions to reduce WP smoking initiation and prevalence among adolescents in the Middle East should be implemented and evaluated. Effective prevention programming would contribute to a sustainable foundation for regional tobacco control.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
REFERENCES
- Ajzen I. The theory of planned behavior. Organ Behav. Hum. Dec. 1991;50:179–211. [Google Scholar]
- Akl E, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int. J. Epidemiol. 2010;39:834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- Akl E, Sameer G, Sohaib A, Rawad O, Philippe J, Roland H, Jihad I. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health. 2011;11:244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akl E, Jawad M, Lam W, Co CN, Obeid R, Irani J. Motives, beliefs and attitudes towards waterpipe tobacco smoking: a systematic review. Harm. Reduct. J. 2013;10:12. doi: 10.1186/1477-7517-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Rashidi M, Shihadeh AL, Saliba NA. Volatile aldehydes in the mainstream smoke of the narghile waterpipe. Food Chem. Toxicol. 2008;46:3546–3549. doi: 10.1016/j.fct.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amos A, Greaves L, Nichter M, Bloch M. Women and tobacco: acall for including gender in tobacco control research, policy and practice. Tob. Control. 2012;21:236–243. doi: 10.1136/tobaccocontrol-2011-050280. [DOI] [PubMed] [Google Scholar]
- Amrock SM, Gordon T, Zelikoff JT, Weitzman M. Hookah use among adolescents in the United States: results of a national survey. Nicotine Tob. Res. 2014;16:231–237. doi: 10.1093/ntr/ntt160. [DOI] [PubMed] [Google Scholar]
- Asfar T, Ward K, Eissenberg T, Maziak W. Comparison of patterns of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health. 2005;5:19. doi: 10.1186/1471-2458-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin SB, Gortmaker SL. Dieting and smoking initiation in early adolescent girls and boys: a prospective study. Am. J. Public Health. 2001;91:446–450. doi: 10.2105/ajph.91.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babar AA, Stigler MH, Perry CL, Arora M, Shrivastav R, Reddy KS. Tobacco-use psychosocial risk profiles of girls and boys in urban India: Implications for gender-specific tobacco intervention development. Nicotine Tob. Res. 2010;12:29–36. doi: 10.1093/ntr/ntp169. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Barnett TE, Forrest JR, Porter L, Curbow BA. A multiyear assessment of hookah use prevalence among Florida high school students. Nicotine Tob. Res. 2013;16:373–377. doi: 10.1093/ntr/ntt188. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Carver K, Gleiter K. Trends in parent and friend influence during adolescence: the case of adolescent cigarette smoking. Addict. Behav. 2001;26:349–361. doi: 10.1016/s0306-4603(00)00110-6. [DOI] [PubMed] [Google Scholar]
- Best JA, Thomson SJ, Santi SM, Smith EA, Brown KS. Preventing cigarette smoking among school children. Annu. Rev. Public Health. 1988;9:161–201. doi: 10.1146/annurev.pu.09.050188.001113. [DOI] [PubMed] [Google Scholar]
- Bidstrup PE, Frederiksen K, Siersma V, Mortensen EL, Ross L, Vinther-Larsen M, Grønbaek M, Johansen C. Social-cognitive and school factors in initiation of smoking among adolescents: a prospective cohort study. Cancer Epidemiol. Biomark. Prev. 2009;18:384–392. doi: 10.1158/1055-9965.EPI-08-0584. [DOI] [PubMed] [Google Scholar]
- Blank MD, Brown KW, Goodman RJ, Eissenberg T. An observational study of group waterpipe use in a natural environment. Nicotine Tob. Res. 2014;16:93–99. doi: 10.1093/ntr/ntt120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Billy J, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J. Adolesc. Health. 2003;33:436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Tobacco product use among middle and high school students — United States, 2011 and 2012. MMWR. 2013;62:893–897. [PMC free article] [PubMed] [Google Scholar]
- Chang FC, Lee CM, Lai HR, Chiang JT, Lee PH, Chen WJ. Social influences and self-efficacy as predictors of youth smoking initiation and cessation: a 3 year longitudinal study of vocational high school students in Taiwan. Addiction. 2006;101:1645–1655. doi: 10.1111/j.1360-0443.2006.01607.x. [DOI] [PubMed] [Google Scholar]
- de Vries H. Socio-economic differences in smoking: Dutch adolescents’ beliefs and behaviour. Soc. Sci. Med. 1995;41:419–424. doi: 10.1016/0277-9536(94)00330-v. [DOI] [PubMed] [Google Scholar]
- de Vries H, Dijkstra M, Kuhlman P. Self-efficacy: The third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health Educ. Res. 1988;3:273–282. [Google Scholar]
- de Vries H, Mudde AN, Kremers SP, Wetzels J, Uiters E, Ariza C, Vitória PD, Anne Fielder A, Holm K, Janssen K, Lehtovuori R, Candel M. The European Smoking Prevention Framework Approach (ESFA): short-term effects. Health Educ. Res. 2003;18:649–663. doi: 10.1093/her/cyg033. [DOI] [PubMed] [Google Scholar]
- Distefan JM, Gilpin EA, Choi WS, Pierce JP. Parental influences predict adolescent smoking in the United States, 1989–1993. J. Adolesc. Health. 1998;22:466–474. doi: 10.1016/s1054-139x(98)00013-5. [DOI] [PubMed] [Google Scholar]
- Eissenberg T, Shihadeh AL. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am. J. Prev. Med. 2009;37:518–523. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eissenberg T, Ward KD, Smith-Simone SY, Maziak W. Waterpipe tobacco smoking on a U.S. college campus: prevalence and correlates. J. Adolesc. Health. 2008;42:526–529. doi: 10.1016/j.jadohealth.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielder RL, Carey KB, Carey MP. Prevalence, frequency, and initiation of hookah tobacco smoking among first-year female college students: a one-year longitudinal study. Addict. Behav. 2012;37:221–224. doi: 10.1016/j.addbeh.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielder RL, Carey KB, Carey MP. Hookah, cigarette, and marijuana use: a prospective study of smoking behaviors among first-year college women. Addict. Behav. 2013;38:2729–2735. doi: 10.1016/j.addbeh.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flom PL, Cassell DL. North East SAS Users Group Inc. 20th Annual Conference: 11–14th November 2007; Baltimore, Maryland: 2007. Stopping Stepwise: Why Stepwise And Similar Selection Methods Are Bad, And What You Should Use. [Google Scholar]
- Fromme H, Silvio D, Heitmann D, Dressel H, Diemer J, Schulz T, Jörres RA, Berlin K, Völkel W. Indoor air contamination during a waterpipe (narghile) smoking session. Food Chem. Toxicol. 2009;47:1636–1641. doi: 10.1016/j.fct.2009.04.017. [DOI] [PubMed] [Google Scholar]
- Fujimoto K, Unger JB, Valente TW. A network method of measuring affiliation-based peer influence: assessing the influences of teammates? Smoking on adolescent smoking. Child Dev. 2012;83:442–451. doi: 10.1111/j.1467-8624.2011.01729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Youth Tobacco Survey Collaborating Group. Differences in worldwide tobacco use by gender: findings from the Global Youth Tobacco Survey. J. School Health. 2003;73:207–215. doi: 10.1111/j.1746-1561.2003.tb06562.x. [DOI] [PubMed] [Google Scholar]
- Greaves L. Gender, equity and tobacco control. Health Soc. Rev. 2007;16:115–129. [Google Scholar]
- Hiemstra M, Otten R, de Leeuw RN, van Schayck OC, Engels R. The changing role of self-efficacy in adolescent smoking initiation. J. Adolesc. Health. 2011;48:597–603. doi: 10.1016/j.jadohealth.2010.09.011. [DOI] [PubMed] [Google Scholar]
- Hoving C, Reubsaet A, de Vries H. Predictors of smoking stage transitions for adolescent boys and girls. Prev. Med. 2007;44:485–489. doi: 10.1016/j.ypmed.2007.02.011. [DOI] [PubMed] [Google Scholar]
- Islam SM, Johnson CA. Correlates of smoking behavior among Muslim Arab-American adolescents. Ethnic Health. 2003;8:319–337. doi: 10.1080/13557850310001631722. [DOI] [PubMed] [Google Scholar]
- Jensen PD, Cortes R, Engholm G, Kremers S, Gislum M. Waterpipe use predicts progression to regular cigarette smoking among Danish youth. Subst. Use Misuse. 2010;45:1245–1261. doi: 10.3109/10826081003682909. [DOI] [PubMed] [Google Scholar]
- Kassim S, Al-Bakri A, al’Absi M, Croucher R. Waterpipe tobacco dependence in U.K. male adult residents: a cross-sectional study. Nicotine Tob. Res. 2013;15:1782–1786. doi: 10.1093/ntr/ntt148. [DOI] [PubMed] [Google Scholar]
- Kleinbaum D, Kupper L, Nizam A, Rosenberg E. Applied Regression Analysis And Other Multivariable Methods. Cengage Learning; Boston: 2013. [Google Scholar]
- Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116:e113–e119. doi: 10.1542/peds.2004-2173. [DOI] [PubMed] [Google Scholar]
- Kremers SP, de Vries H, Mudde AN, Candel M. Motivational stages of adolescent smoking initiation: predictive validity and predictors of transitions. Addict. Behav. 2004;29:781–789. doi: 10.1016/j.addbeh.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Kulwicki A, Hill Rice V. Arab American adolescent perceptions and experiences with smoking. Public Health Nurs. 2003;20:177–183. doi: 10.1046/j.0737-1209.2003.20304.x. [DOI] [PubMed] [Google Scholar]
- Ma H, Unger JB, Chou CP, Sun P, Palmer PH, Zhou Y, Yao J, Xie B, Gallaher PE, Guo Q. Risk factors for adolescent smoking in urban and rural China: findings from the China seven cities study. Addict. Behav. 2008;33:1081–1085. doi: 10.1016/j.addbeh.2008.04.004. [DOI] [PubMed] [Google Scholar]
- Markham WA, Lopez ML, Aveyard P, Herrero P, Bridle C, Comas A, Charlton A, Thomas H. Mediated, moderated and direct effects of country of residence, age, and gender on the cognitive and social determinants of adolescent smoking in Spain and the UK: a cross-sectional study. BMC Public Health. 2009;9:173. doi: 10.1186/1471-2458-9-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinasek MP, McDermott RJ, Martini L. Waterpipe (hookah) tobacco smoking among youth. Curr. Probl. Pediatr. Adolesc. Health Care. 2011;41:34–57. doi: 10.1016/j.cppeds.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Maziak W. The global epidemic of waterpipe smoking. Addict. Behav. 2011;36:1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W. The waterpipe: a new way of hooking youth on tobacco. Am. J. Addict. 2014;23:103–107. doi: 10.1111/j.1521-0391.2013.12073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Asfar T. Physical abuse in low-income women in Aleppo, Syria. Health Care Women Int. 2003;24:313–326. doi: 10.1080/07399330390191689. [DOI] [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Klesges RC, Keil U, Ward KD. Adapting smoking cessation interventions for developing countries: a model for the Middle East. Int. J. Tuberc. Lung Dis. 2004;8:403–413. [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Rastam S, Hammal F, Asfar T, Bachir ME, Fouad MF, Ward KD. Beliefs and attitudes related to narghile (waterpipe) smoking among university students in Syria. Ann. Epidemiol. 2004;14:646–654. doi: 10.1016/j.annepidem.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Ward KD. Patterns of waterpipe use and dependence: implications for intervention development. Pharmacol. Biochem. Behav. 2005;80:173–179. doi: 10.1016/j.pbb.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Maziak W, Mzayek F. Characterization of the smoking habit among high school students in Syria. Eur. J. Epidemiol. 2000;16:1169–1176. doi: 10.1023/a:1010907724688. [DOI] [PubMed] [Google Scholar]
- Maziak W, Rastam S, Eissenberg T, Asfar T, Hammal F, Bachir ME, Fouad MF, Ward KD. Gender and smoking status-based analysis of views regarding waterpipe and cigarette smoking in Aleppo, Syria. Prev. Med. 2004;38:479–484. doi: 10.1016/j.ypmed.2003.11.021. [DOI] [PubMed] [Google Scholar]
- Maziak W, Rastam S, Shihadeh AL, Bazzi A, Ibrahim I, Zaatari GS, Ward KD, Eissenberg T. Nicotine exposure in daily waterpipe smokers and its relation to puff topography. Addict. Behav. 2011;36:397–399. doi: 10.1016/j.addbeh.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Standardizing questionnaire items for the assessment of waterpipe tobacco use in epidemiological studies. Public Health. 2005;119:400–404. doi: 10.1016/j.puhe.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain of a global epidemic. Tob. Control. 2004;13:327–333. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Eissenberg T. Factors related to frequency of narghile (waterpipe) use: the first insights on tobacco dependence in narghile users. Drug Alcohol Depend. 2004;76:101–106. doi: 10.1016/j.drugalcdep.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Eissenberg T. Interventions for waterpipe smoking cessation. Cochrane Database Syst. Rev. 2007;4 doi: 10.1002/14651858.CD005549.pub2. [DOI] [PubMed] [Google Scholar]
- McKelvey KL, Wilcox ML, Madhivanan P, Mzayek F, Khader Y, Maziak W. Time trends of cigarette and waterpipe smoking among a cohort of school children in Irbid, Jordan, 2008–11. Eur. J. Public Health. 2013;23:862–867. doi: 10.1093/eurpub/ckt140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meleigy M. Waterpipe and communicable diseases link, says WHO. Lancet Infect. Dis. 2007;7:448. [Google Scholar]
- Miller CH, Burgoon M, Grandpre JR, Alvaro EM. Identifying principal risk factors for the initiation of adolescent smoking behaviors: the significance of psychological reactance. Health Commun. 2006;19:241–252. doi: 10.1207/s15327027hc1903_6. [DOI] [PubMed] [Google Scholar]
- Morgenstern M, Sargent JD, Engels R, Scholte RH, Florek E, Hunt K, Sweeting H, Mathis F, Faggiano F, Hanewinkel R. Smoking in movies and adolescent smoking initiation: longitudinal study in six European countries. Am. J. Prev. Med. 2013;44:339–344. doi: 10.1016/j.amepre.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mzayek F, Khader Y, Eissenberg T, Al Ali R, Ward KD, Maziak W. Patterns of water-pipe and cigarette smoking initiation in schoolchildren: Irbid longitudinal smoking study. Nicotine Tob Res. 2012;14:448–454. doi: 10.1093/ntr/ntr234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mzayek F, Khader Y, Eissenberg T, Ward KD, Maziak W. Design, baseline results of Irbid longitudinal, school-based smoking study. Am. J. Health Behav. 2011;35:746–755. [PMC free article] [PubMed] [Google Scholar]
- Nasim A, Khader Y, Blank MD, Cobb CO, Eissenberg T. Trends in alternative tobacco use among light, moderate, and heavy smokers in adolescence, 1999–2009. Addict. Behav. 2012;37:866–870. doi: 10.1016/j.addbeh.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichter M. Smoking: what does culture have to do with it? Addiction. 2003;98:139–145. doi: 10.1046/j.1360-0443.98.s1.9.x. [DOI] [PubMed] [Google Scholar]
- Okoli C, Greaves L, Fagyas V. Sex differences in smoking initiation among children and adolescents. Public Health. 2013;127:3–10. doi: 10.1016/j.puhe.2012.09.015. [DOI] [PubMed] [Google Scholar]
- O'Loughlin JL, Karp I, Koulis T, Paradis G, DiFranza J. Determinants of first puff and daily cigarette smoking in adolescents. Am. J. Epidemiol. 2009;170:585–597. doi: 10.1093/aje/kwp179. [DOI] [PubMed] [Google Scholar]
- Parna K, Usin J, Ringmets I. Cigarette and waterpipe smoking among adolescents in Estonia: HBSC Survey Results, 1994–2006. BMC Public Health. 2008;8:392. doi: 10.1186/1471-2458-8-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piko BF, Luszczynska A, Gibbons FX, Teközel M. A culture-based study of personal and social influences of adolescent smoking. Eur. J. Public Health. 2005;15:393–398. doi: 10.1093/eurpub/cki008. [DOI] [PubMed] [Google Scholar]
- Primack BA, Fertman CI, Rice KR, Adachi-Mejia AM, Fine MJ. Waterpipe and cigarette smoking among college athletes in the United States. J. Adolesc. Health. 2010;46:45–51. doi: 10.1016/j.jadohealth.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Mah J, Shensa A, Rosen D, Yonas MA, Fine MJ. Associations between race, ethnicity, religion, and waterpipe tobacco smoking. J. Ethn. Subst. Abuse. 2014;13:58–71. doi: 10.1080/15332640.2013.850462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Shensa A, Kim KH, Carroll MV, Hoban MT, Leino EV, Eissenberg T, Dachille KH, Fine MJ. Waterpipe smoking among U.S. university students. Nicotine Tob. Res. 2013;15:29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Walsh M, Bryce C, Eissenberg T. Water-pipe tobacco smoking among middle and high school students in Arizona. Pediatrics. 2009;123:e282–e288. doi: 10.1542/peds.2008-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prokhorov AV, Winickoff JP, Ahluwalia JS, Ossip-Klein D, Tanski S, Lando HA, Moolchan ET, et al. Youth tobacco use: global perspective for child health care clinicians. Pediatrics. 2006;118:e890–e903. doi: 10.1542/peds.2005-0810. [DOI] [PubMed] [Google Scholar]
- Rastam S, Eissenberg T, Ibrahim I, Ward KD, Khalil R, Maziak W. Comparative analysis of waterpipe and cigarette suppression of abstinence and craving symptoms. Addict. Behav. 2011;36:555–559. doi: 10.1016/j.addbeh.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribisl KM. Research gaps related to tobacco product marketing and sales in the family smoking prevention and tobacco control act. Nicotine Tob. Res. 2012;14:43–53. doi: 10.1093/ntr/ntr098. [DOI] [PubMed] [Google Scholar]
- Rice VH, Templin T, Kulwicki A. Arab-American adolescent tobacco use: four pilot studies. Prev. Med. 2003;37:492–498. doi: 10.1016/s0091-7435(03)00175-0. [DOI] [PubMed] [Google Scholar]
- Rice VH, Weglicki LS, Templin T, Hammad A, Jamil H, Kulwicki A. Predictors of Arab American adolescent tobacco use. Merrill-Palmer Q. 2006;52:327–342. doi: 10.1353/mpq.2006.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice VH, Weglicki LS, Templin TN, Jamil H, Hammad A. Intervention effects on tobacco use in Arab and Non-Arab American adolescents. Addict. Behav. 2010;35:46–48. doi: 10.1016/j.addbeh.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roskin J, Aveyard P. Canadian and English students' beliefs about waterpipe smoking: a qualitative study. BMC Public Health. 2009;9:10. doi: 10.1186/1471-2458-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scal P, Ireland M, Borowsky IW. Smoking among American adolescents: a risk and protective factor analysis. J. Community Health. 2003;28:79–97. doi: 10.1023/a:1022691212793. [DOI] [PubMed] [Google Scholar]
- Sidani JE, Shensa A, Barnett TE, Cook RL, Primack BA. Knowledge, attitudes, and normative beliefs as predictors of hookah smoking initiation: a longitudinal study of university students. Nicotine Tob. Res. 2013;16:647–654. doi: 10.1093/ntr/ntt201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skara S, Sussman S, Dent CW. Predicting regular cigarette use among continuation high school students. Am. J. Health Behav. 2001;25:147–156. doi: 10.5993/ajhb.25.2.7. [DOI] [PubMed] [Google Scholar]
- Stanton WR, Barnett AG, Silva PA. Adolescents’ intentions to smoke as a predictor of smoking. Prev. Med. 2005;40:221–226. doi: 10.1016/j.ypmed.2004.05.026. [DOI] [PubMed] [Google Scholar]
- Steentoft JWJ, Andersen JR. Tuberculosis and water pipes as source of infection. Ugeskr Laeger. 2006;168:904–907. [PubMed] [Google Scholar]
- Thun M, Peto R, Boreham J, Lopez AD. Stages of the cigarette epidemic on entering its second century. Tob. Control. 2012;21:96–101. doi: 10.1136/tobaccocontrol-2011-050294. [DOI] [PubMed] [Google Scholar]
- Torrey CM, Moon KA, D'Ann LW, Green T, Cohen JE, Navas-Acien A, Breysse PN. Waterpipe cafes in Baltimore, Maryland: carbon monoxide, particulate matter, and nicotine exposure. J. Expo. Sci. Environ. Epidemiol. 2014 doi: 10.1038/jes.2014.19. Avail online 16 April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall GK, Azevedo K. Longitudinal effects of a universal family-focused intervention on growth patterns of adolescent internalizing symptoms and polysubstance use: gender comparisons. J. Youth Adolesc. 2007;36:725–740. [Google Scholar]
- Tu Y, Gunnell D, Gilthorpe M. Simpson's paradox, Lord's paradox, and suppression effects are the same phenomenon - the Reversal paradox. Emerg. Themes Epidemiol. 2008;5:2. doi: 10.1186/1742-7622-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob. Control. 1998;7:409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitória PD, Fá Salgueiro M, Silva SA, de Vries H. Social influence, intention to smoke, and adolescent smoking behaviour longitudinal relations. Br. J. Health Psychol. 2011;16:779–798. doi: 10.1111/j.2044-8287.2010.02014.x. [DOI] [PubMed] [Google Scholar]
- Warren CW The Global Youth Tobacco Survey Collaborative Group. Tobacco use among youth: a cross country comparison. Tob. Control. 2002;11:52–70. [Google Scholar]
- Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13—15 year olds between 1999 and 2008: findings from the Global Youth Tobacco Survey. Glob Health Promot. 2009;16:38–90. doi: 10.1177/1757975909342192. [DOI] [PubMed] [Google Scholar]
- Weglicki LS, Templin TN, Rice VH, Jamil H, Hammad A. Comparison of cigarette and water-pipe smoking by Arab and non–Arab-American youth. Am. J. Prev. Med. 2008;35:334–339. doi: 10.1016/j.amepre.2008.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox P. An ecological approach to understanding youth smoking trajectories: problems and prospects. Addiction. 2003;98:57–77. doi: 10.1046/j.1360-0443.98.s1.5.x. [DOI] [PubMed] [Google Scholar]
- Wood AP, Dawe S, Gullo MJ. The role of personality, family influences, and prosocial risk-taking behavior on substance use in early adolescence. J. Adolesc. 2013;36:871–881. doi: 10.1016/j.adolescence.2013.07.003. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Guidelines For Controlling And Monitoring The Tobacco Epidemic. WHO; Geneva: 1998. [Google Scholar]
- Zhu BP, Liu M, Shelton D, Liu S, Giovino GA. Cigarette smoking and its risk factors among elementary school students in Beijing. Am. J. Public Health. 1996;86:368–375. doi: 10.2105/ajph.86.3.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.