Abstract
Neuroendocrine tumors (NETs) are rare group of neoplasms arising from nervous and endocrine systems. Somatostatin analogue imaging is a functional imaging modality of choice for evaluating the NETs. Recent availability of positron emitting radioisotope labeled somatostatin analogues to image neuroendocrine cancers, has raised the interests to use this new imaging modality in management of patients with NETs. 68Ga-DOTATATE PET/CT has demonstrated superiority in lesion detection compared to Octreoscan, MIBG scintigraphy and MRI. In this article, we reviewed the published studies evaluating the role of 68Ga-DOTATATE PET in diagnosis and management of patients with neuroendocrine tumors and comparing it to current FDA approved imaging modalities including Octreoscan, MIBG scintigraphy, 18F FDG PET/CT, CT and MRI.
Keywords: Gallium 68, neuroendocrine tumors, DOTATATE, positron emission tomography, hybrid imaging
Introduction
Neuroendocrine tumors (NETs) are a rare group of neoplasms with an incidence of about 35 cases per 100,000 people in the United States. The defined characteristic of NETs is the expression of somatostatin receptors (SST) [1]. This unique feature has enabled the field of nuclear medicine and molecular imaging to image these tumors with radiolabelled somatostatin analogues agent [2]. Octreotide, a long-acting somatostatin analogue, was initially used in 1989 and since then it evolved as an important agent in the initial evaluation and management of NETs using molecular imaging techniques [3]. However, gamma imaging using 111In-octreotide has several limiting factors which decreased the image quality and overall efficiency of the test. These include low image quality of indium 111 isotope, increased physiological uptake which restricts detection of small lesions, prolonged imaging protocol and relatively high radiation dose to the patients [4,5].
Radiolabelled meta-iodobenzylguanidine (MIBG) with Iiodide 123 or 131 has been used in a subgroup of neuroendocrine cancers including pheochromocytoma and paraganglioma [6]. MIBG imaging has been used as a standard functional imaging for initial evaluation and management of these types of tumors. However, the spatial resolution of MIBG imaging is low and has limitations similar to Octreoscan®. Contrast-enhanced MRI is also used to evaluate neuroendocrine tumors due to its ability to provide high quality images of the abdomen [7] but their specificity is poor, especially for phaeochromocytomas [8].
With recent availability of the PET imaging technique, somatostatin analogues have been labeled with positron emitting isotopes, including Gallium-68, to image somatostatin receptor expressing tumors [9]. It has been demonstrated that 68Ga-DOTATATE PET scan can dramatically improve the spatial resolution and lesion detectability compared to Octreoscan® or MIBG scintigraphy [9,10]. In terms of convenience 68Ga-DOTATATE represents a major advantage for patients as it can be completed in less than 2 hours versus 2 days for Octreoscan or MIBG imaging. 68Ga-DOTATATE also involves lower radiation exposure [11]. However, the superiority of 68Ga-DOTATATE PET imaging is due to the added diagnostic information and also quantification capability in comparison with Octreoscan® or MIBG imaging. 68Ga-DOTATATE has also been proven to have high impact on management of the neuroendocrine cancer patients indicating an important role in clinical practice of somatostatin-avid malignancies [12].
The purpose of this article is to systematically review all published data on the role of 68Ga-DOTATATE PET in diagnostic and management of patients with neuroendocrine cancer and compare it to current FDA approved imaging modalities including Octreoscan®, MIBG scintigraphy, 18F FDG PET/CT, CT and MRI.
Literature review methodology
A comprehensive electronic literature search of the Pubmed and ovid medline databases was performed to find published articles on the diagnostic and management value of 68Ga-DOTATATE PET/CT in NETs patients. We searched using words “Ga 68 or gallium 68” and DOTATATE or DOTA TATE or DOTA-TATE or DOTA octreotide. We defined our search time with no beginning date but ending 15 February 2014. Only English language journals were searched in the database. We included all the articles investigating the diagnostic and management role of 68Ga-DOTATATE PET in patients with NETs comparing to Octreoscan, MIBG scintigraphy or MRI. We excluded the articles that were: review articles, case reports, editorial, letters, author reply, comments, duplicate data, using other radiopharmaceuticals such as 68Ga-DOTATOC studies and articles that were not related to neuroendocrine tumors. The search was performed by three researchers (AM, ST and ED) and all the retrieved abstracts were reviewed carefully and eventually selected according to the inclusion and exclusion criteria described above. All the researchers then reviewed the full papers and their eligibility for inclusion was determined in the consensus meeting.
Basic information from these studies were extracted including authors, type of NETs, country, patient information, study design, reference standard. The value of sensitivity and specificity 68Ga-DOTATATE PET in the diagnosis of NETs were recorded.
As only few studies, following the above mentioned criteria, were found ineach category comparing the 68Ga-DOTATATE PET/CT to Octreoscan, MIBG scintigraphy or MRI, no statistical analysis was performed. The sensitivity and specificity of 68Ga-DOTATATE PET/CT were obtained from individual studies and compared to Octreoscan, MIBG scintigraphy and CT or MRI.
Results
Literature search
The comprehensive literature search showed 73 published papers. Upon review, 59 papers were excluded as they were reviews, letters, or editorials, or because they were not within the field of interest of this review. Finally 14 papers were selected and retrieved in full text version. A total of 570 patients with NETs [17-26], satisfying inclusion and exclusion criteria were included in this review. The characteristics of the included studies are presented in Table 1.
Table 1.
Demographic data
| Author | Journal | Year | No Patients | Tumor | Lesions | Reference |
|---|---|---|---|---|---|---|
| Goel et al | IJNM | 2014 | 30 | All NET | Mets | [26] |
| Armbruster et al | JIR | 2014 | 42 | All NET | Liver Mets | [27] |
| Haug et al | Radiology | 2013 | 63 | All NET (Excluded MTC) | Mets | [19] |
| Schmid et al | EJNMMI | 2013 | 18 | Pancreatic NET | Panc lesions+mets | [25] |
| Haug et al | JNM | 2012 | 104 | All NET | Primary lesions+mets | [18] |
| Maurice et al | EJNMMI | 2012 | 15 | PCC, PGL | Primary lesions+mets | [23] |
| Hofman et al | JMIRO | 2012 | 59 | NET (GEP, Bronc, PCC, PGL) | Primary lesions+mets | [12] |
| Łapińska et al | NMRCEE | 2011 | 97 | NET (GEP, MCT) | Primary lesions+mets | [21] |
| Naji et al | MIAB Aug | 2010 | 12 | PCC, PGL | Primary lesions+mets | [24] |
| Srirajaskanthan et al | JNM June | 2010 | 51 | All NET | Primary lesions+mets | [20] |
| Conry et al | EJNMMI | 2010 | 18 | MTC | Primary lesions+mets | [28] |
| Kayani et al | JNM | 2009 | 18 | All NET | Primary lesions+mets | [30] |
| Kayani et al | Cancer | 2008 | 38 | All NET | Primary lesions+mets | [28] |
| Win et al | NMC | 2007 | 5 | PCC | Mets | [22] |
NET: Neuroendocrine Tumor, MTC: Medullary Thyroid Cancer, PCC: Pheochromocytoma, PGL: Paraganglioma, GEP: Gastroenteropancreatic, Bronc: Bronchial.
Diagnostic performance
The summary data of 68Ga-DOTATATE PET/CT is presented in Table 1. The sensitivity of the 68Ga-DOTATATE PET/CT in the diagnosis of primary or metastatic lesions in NETs is specified in (Tables 2, 3 and 4) ranging 80%-100%. The specificity of the 68Ga-DOTATATE PET/CT in the diagnosis of primary or metastatic lesions in NETs compared to gold standard pathology is demonstrated in Table 2 ranging 82%-90%.
Table 2.
68Ga-DOTATATE sensitivity and specificity compared to pathology as a gold standard
Table 3.
Comparing the 68Ga-DOTATATE to Octreoscan
| Author | 68Ga-DOTATATE | Octreoscan | Pathology confirmed | Reference |
|---|---|---|---|---|
| Hofman et al | Sensitivity 88% | Sensitivity n/a | 41/59 patients (11 suspicious, 4 confirmed with imaging) | [12] |
| Specificity 80% | Specificity n/a | |||
| Srirajaskanthan et al | Sensitivity 87.2% | Sensitivity n/a | Yes all 51 patients | [19] |
| Specificity 100% | Specificity 98% | |||
| Łapińska et al | Sensitivity n/a | Sensitivity n/a | 88/97 patients (9 Suspicious) | [20] |
| Specificity n/a | Specificity n/a |
Table 4.
Comparing the 68Ga-DOTATATE to MIBG scintigraphy
| Author | 68Ga-DOTATATE | MIBG | Pathology confirmed | Reference |
|---|---|---|---|---|
| Win et al | Sensitivity 100% | Sensitivity 60% | No | [21] |
| Specificity 100% | Specificity n/a | |||
| Maurice et al | Sensitivity 80% | n/a (used as a gold standard) | Yes all 15 patients | [22] |
| Specificity n/a | ||||
| Naji et al | Sensitivity 83% | Sensitivity 41.6% | 8/12 patients (4 confirmed with imaging) | [23] |
| Specificity n/a | Specificity n/a |
68Ga-DOTATATE PET/CT versus Octreoscan
3 studies compared the 68Ga-DOTATATE PET/CT to Octreoscan (Table 3). The total number of patients in these studies was 207. The sensitivity of the 68Ga-DOTATATE PET/CT ranged from 83%-88% and its specificity ranged from 80%-100%. The specificity of the Octreoscan mentioned only in one study which was 98%. No sensitivity of Octreoscan was reported in these 3 studies.
68Ga-DOTATATE PET/CT versus Octreoscan: change in clinical management
Two of 3 studies mentioned above reported that the additional information provided by 68Ga-DOTATATE PET resulted in change in clinical management in 70.6%-81% of patients with neuroendocrine cancers.
68Ga-DOTATATE PET/CT versus MIBG scintigraphy
There were 3 studies comparing the 68Ga-DOTATATE PET/CT to MIBG scintigraphy (Table 4). The total number of patients in these studies was 32. The sensitivity of the 68Ga-DOTATATE PET/CT ranged from 80%-100% and its specificity only reported in one study which was 100%.
The sensitivity of the MIBG scintigraphy ranged from 41.6%-60% and its specificity only reported in 2 studies which was 100%.
68Ga-DOTATATE PET/CT versus CT or MRI
There were 2 studies comparing the 68Ga-DOTATATE PET/CT to MRI and 1 study comparing the 68Ga-DOTATATE PET/CT to contrast enhanced CT (Table 5). The total number of patients in these studies were 56. In one of the studies the sensitivity and specificity of the 68Ga-DOTATATE PET/CT was reported to be 93.8-100% whereas it was 92.6-100% respectively for MRI. In another study, sensitivity of MRI was reported to be 63.1%. No specificity of MRI was reported. No sensitivity or specificity in the CT study was calculated.
Table 5.
Comparing the 68Ga-DOTATATE to MRI or CT
| Author | 68Ga-DOTATATE | MRI or CT | Pathology confirmed | Reference |
|---|---|---|---|---|
| Schmid et al | Sensitivity 100% | Sensitivity 63.1% | Yes all 18 patients | [24] |
| Specificity 100% | Specificity n/a | |||
| Goel et al | Sensitivity n/a | Sensitivity n/a | No | [25] |
| Specificity n/a | Specificity n/a | |||
| Armbruster et al | Sensitivity 92.6% | Sensitivity n/a | No | [26] |
| Specificity 93.8% | Specificity n/a |
68Ga-DOTATATE PET/CT versus 18F-FDG PET/CT
There were 3 studies comparing the 68Ga-DOTATATE PET/CT to 18F-FDG PET/CT (Table 6). The total number of patients in these studies was 74. The sensitivity of the 68Ga-DOTATATE PET/CT reported to be 72.2-100%. The sensitivity of the 18F-FDG PET/CT reported to be 66-77.8%. No specificity of the 68Ga-DOTATATE PET/CT or 18F-FDG PET/CT was reported in these 2 studies.
Table 6.
Comparing the 68Ga-DOTATATE to 18F-FDG PET/CT
| Author | 68Ga-DOTATATE | 18F-FDG PET/CT | Pathology confirmed | Reference |
|---|---|---|---|---|
| Kayani et al | Sensitivity 82% | Sensitivity 66% | Not all patients | [27] |
| Specificity n/a | Specificity n/a | |||
| Kayani et al | Sensitivity 100% | Sensitivity 54.4% | Not all patients | [28] |
| Specificity n/a | Specificity n/a | |||
| Conry et al | Sensitivity 72.2% | Sensitivity 77.8% | Not all patients | [29] |
| Specificity n/a | Specificity n/a |
Discussion
Somatostatin receptor-based imaging is the functional imaging of choice in diagnosis and management of NETs. The mechanism of somatostatin receptor-based radionuclide imaging is the binding of a radiolabeled ligand to the somatostatin receptor. The first investigation was published in 1984 by Reubi et al discussed the over expression of somatostatin receptors on tumor tissue [13]. Krenning et al in 1993 was the first to report the scintigraphy of NETs expressing somatostatin receptors using 123I-Tyr-octreotide [14].
With availability of positron emitting tomography in recent years, PET tracers labeled somatostatin analogues have been developed rapidly. With the help of 68Ge/68Ga generators, now the PET radiolabelled tracers can be made on site independent of cyclotron and therefore less expensive for clinical practice. 68Ga is eluted from the 68Ge/68Ga generator which immobilizes the parent radioisotope Germanium. There are several generators available in market including itm (Isotopen Technologien Muenchen AG), EZ (Eckert & Ziegler Strahlen- und Medizintechnik AG) and iThemba labs which differ in their construction and method of germanium immobilization. The Ga-68 can be eluted using various concentrations of HCl. Several different methods have been used for radiolabeling of DOTATATE with Ga-68, including pre-concentration and purification (cationic or anion exchange) method or fractionation method based on the feasibility and type of generator. In few methods post-processing purification by using C-18 Sep Pak purification to ensure removal of free Ga-68. The quality control (including the endotoxin test, 68Ge breakthrough, radionuclide identity test, osmolality test, pH test) of the 68Ga-DOTATATE completes preparation of clinical dose of radiotracer. Nevertheless, the methodology of preparation of 68Ga-DOTATATE is well characterized and standardized for clinical practice upon stringent quality control testing [15]. Reubi et al. reported that the affinity of DOTATATE in binding SST2 to be approximately 10-fold higher than that of octreotide [16]. Souvatzoglou et al. showed that the additional accurate anatomical information provided by the CT component of PET/CT, can add significant value in the diagnosis and evaluation of therapy response due to functional and morphological information of the disease [17].
Haug et al was the first study that evaluated the role of 68Ga-DOTATATE PET/CT in suspected neuroendocrine tumors and correlated it with gold standard pathology [18]. 68Ga-DOTATATE PET/CT identified NET in 29 of the 36 cases and excluded the presence of a NET in 61 of the 68 non-NET patients, indicating a sensitivity of 81% and specificity of 90%. In another study Haug et al investigated the role of 68Ga-DOTATATE PET/CT in detection of metastatic lesions in patients with neuroendocrine cancer and compared it to gold standard pathology [19]. 68Ga-DOTATATE PET/CT helped to identify NET recurrence in 26 of 29 patients (sensitivity, 90%) and excluded the presence of recurrent NET in 28 of 34 patients (specificity, 82%). The accuracy calculated to be 86% (54 of 63). In gastroenteropancreatic NET (n = 45), the 68Ga-DOTATATE PET/CT showed to be more sensitive, specific and accurate. In this subgroup, sensitivity was 94%; specificity was 89%; and accuracy was 91%.
Srirajaskanthan et al were the first group that compared the 68Ga-DOTATATE to Octreoscan [20]. They evaluated the diagnostic and management role of 68Ga-DOTATATE PET imaging in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. They showed that 68Ga-DOTATATE PET was positive in 41 of these 47 patients (87.2%). No false-positive lesions were identified. 68Ga-DOTATATE PET identified significantly more lesions than 111In-DTPA-octreotide scintigraphy (168 versus 27 respectively, P < 0.001). Hofman et al [12] studied the impact of 68Ga-DOTATATE PET/CT for imaging neuroendocrine and other somatostatin expressing tumors and compared it to Octreoscan and conventional imaging. They demonstrated that 88% of 68Ga-DOTATATE PET/CT studies were abnormal. Compared with conventional and In-111 octreotide imaging, additional information was provided by 68Ga-DOTATATE PET/CT in 68 and 83% of patients, respectively. Figure 1 demonstrates side by side comparison of 68Ga-DOTATATE to Octreoscan.
Figure 1.
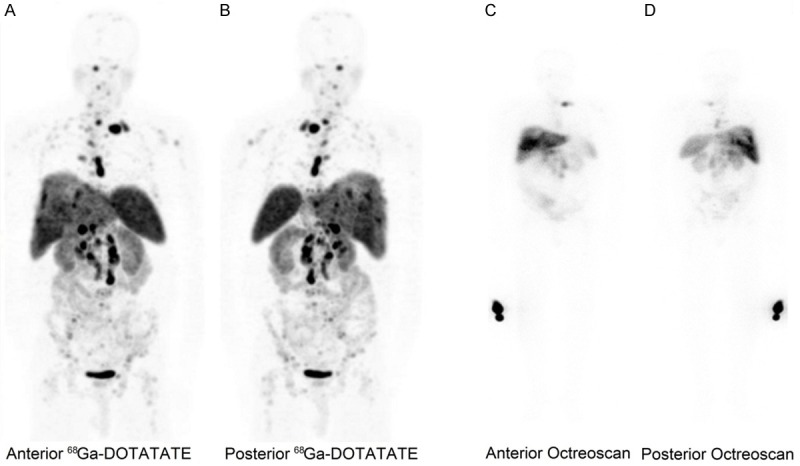
Side by side comparison of 68Ga-DOTATATE to Octreoscan from one of our patients with neuroendocrine tumor. Anterior (A) and posterior (B) 68Ga-DOTATATE pet images demonstrate extensive metastatic disease. Octreoscan anterior (C) and posterior (D) images from same patient demonstrate much fewer lesions indicating superior quality of PET/CT imaging
. To investigate the change in clinical management, Srirajaskanthan et al and Hofman et al further analyzed their data to understand whether the additional information provided by 68Ga-DOTATATE PET/CT resulted in change in clinical management of the patients. Srirajaskanthan et al demonstrated that 68Ga-DOTATATE imaging changed the management in 70.6% of patients, who were subsequently suitable for peptide receptor-targeted therapy. Hofman et al also found that 68Ga-DOTATATE PET/CT resulted in change in clinical management of 81% patients. Management impact was high (inter-modality change) in 47%, moderate (intra-modality change) in 10% and low in 41% (not assessable in 2%) of the patients. High management impact included directing patients to curative surgery by identifying a primary site and directing patients with multiple metastases to systemic therapy. Change in management impact included directing patients to curative surgery by identifying a primary site and directing patients with multiple metastases to systemic therapy.
Łapińska et al studied the somatostatin receptor expression in neuroendocrine cancers using 68Ga-DOTATATE PET/CT [21]. 68Ga-DOTATATE PET/CT detected the presence of the somatostatin receptor affinity in 50 of the 97 patients (51.5%). They concluded that 68Ga-DOTATATE PET provides information on tumor cell receptors status, which has a significant bearing on planning targeted radionuclide therapy.
Win et al were the first that investigated the diagnostic value of 68Ga-DOTATATE in neuroectodermal tumors [22]. They compared 68Ga-DOTATATE to MIBG imaging in small group of patients with neuroectodermal tumors. They showed that 68Ga-DOTATATE identified more lesions with higher uptake and better resolution compared to 123I-MIBG. Out of 5 patients, two patients had negative 123I-MIBG and positive 68Ga-DOTATATE scans. One had a weakly positive 123I-MIBG and a strongly positive 68Ga-DOTATATE scan. One had a positive 123I-MIBG and positive 68Ga-DOTATATE scans. Maurice et al compared the performance of 68Ga-DOTATATE PET/CT and 123I-MIBG SPECT [23]. They noticed that in head and neck lesions, with the lesions in 4 patients being picked up by 68Ga-DOTATATE and missed by 123I-MIBG. On a per-lesion analysis, 68Ga-DOTATATE was able to detect 167 lesions versus 128 lesions detected by CT/MRI and 111 by MIBG imaging. This demonstrated the superiority 68Ga-DOTATATE in detecting lesions in all anatomical locations, and particularly bony lesions. They concluded that 68Ga-DOTATATE should be considered as a first-line investigation in patients at high risk of PGL and metastatic disease, such as in the screening of carriers for mutations associated with familial PGL syndromes. Also they mentioned that, 68Ga-DOTATATE should be preferred over 123I-MIBG in patients with metastatic spread, particularly if the bone involvement, is suspected. In the study by Naji et al similar finding was observed and 68Ga-DOTATATE PET was superior to Octreoscan [24]. They found that 68Ga-DOTATATE PET showed tumor lesions in ten out of 12 patients with confirmed disease, while 123I-MIBG showed lesions in five out of 12 patients. 68Ga-DOTATATE and 123I-MIBG detected a total of 30 lesions, of which 29/30 was positive with 68Ga-DOTATATE and 7/30 with 123I-MIBG. We also found higher incidence of SDHB positive results in patients with positive 68Ga-DOTATATE.
Schmid-Tannwald et al compared the abdominal MRI with diffusion-weighted imaging to 68Ga-DOTATATE PET/CT in detection of neuroendocrine tumors of the pancreas and correlated with gold standard pathology [25]. They found that of the NETs were detected in 8/23 (34.8%) and 9/23 (39.1%) on T2w images by observers 1 and 2, respectively. Detection rates of pancreatic NET with PET/CT (both observers: 23/23 = 100%) were significantly higher than with MRI (p < 0.05). Goel et al evaluated the role of 68Ga-DOTATATE PET/CT for the detection of bone metastases in pediatric neuroendocrine tumors (NETs) and to compare it with contrast enhanced CT scan [26]. Compared with CT scan, 68Ga-DOTATATE PET detected bone metastases at a significantly higher rate (P = 0.0039). On a per lesion analysis, out of a total of 225 lesions detected by 68Ga-DOTATATE PET, only 84 lesions could be detected by CT scan. They concluded that 68Ga-DOTATATE PET/CT is more useful than CECT scan for the early detection of bone metastases in pediatric NETs. Armbruster et al, compared dynamic contrast enhanced magnetic to 68Ga-DOTATATE PET/CT and 18F FDG PET/CT in patients with liver metastases from neuroendocrine tumors [27]. They observed that the lesion-to-background ratios of arterial plasma flow and arterial flow fraction of liver metastases correlated negatively with the lesion-to-background ratios of SUVmean derived from 68Ga-DOTATATE PET/CT (r = j0.54, P G 0.001; r = j0.39, P G 0.001, respectively). However they correlated positively with the lesion-to-background ratios of SUVmean derived from 18F-FDG-PET/CT (r = 0.51, P G 0.05; r = 0.68, P G 0.01, respectively). The lesion-to-background ratios of the DCE-MRI parameters extracellular mean transit time and extracellular volume correlated very weakly with the lesion-to-background ratios of SUVmean from 68Ga-DOTATATE PET/CT, whereas venous plasma flow, total plasma flow, hepatic uptake fraction, and intracellular uptake rate showed no correlation between DCE-MRI and PET/CT. They concluded that, they were able to show some DCE-MRI parameters, especially the flow-related parameters, are correlated with SUV from PET/CT, whereas other parameters correlate poorly or not at all, suggesting that the combination of MR and PET may improve the diagnostic power compared with each technique individually and has the potential to provide additional functional information of the liver.
Neuroendocrine cancers are slow growing tumor and 18F-FDG PET/CT is not commonly used for initial evaluation of the neuroendocrine cancers. Due to slow metabolic activity of the NETs in initial stages, they are not extremely avid on 18F-FDG PET/CT. Opposite to this, they are avid for 68Ga-DOTATATE which demonstrate high uptake because neuroendocrine tumors express significant SSR2. However in the late state of disease when the tumor characteristics changes from being well differentiated to poorly differentiated the uptake pattern will change. In this case the tumor and metastatic sites demonstrate low 68Ga-DOTATATE uptake due to less expression of SSR2 and high 18F-FDG PET/CT uptake. Kayani et al were the first to compare 68Ga-DOTATATE PET/CT to 18F FDG PET/CT [28]. They retrospectively reviewed the findings with 68Ga-DOTATATE and 18F-FDG imaging in 38 patients with primary or recurrent NET. The reported a sensitivity of 82% for 68Ga-DOTATATE PET/CT and 66% for 18F-FDG PET/. The sensitivity of combined 68Ga-DOTATATE and 18F-FDG PET/CT was 92% (35 of 38). There was greater uptake of 68Ga-DOTATATE than 18F-FDG in low-grade NET (median SUV 29 vs 2.9, P < .001). In high-grade NET there was higher uptake of 18F-FDG over 68Ga-DOTATATE (median SUV 11.7 vs 4.4, P 5.03). There was a significant correlation with predominant tumor uptake of 68Ga-DOTATATE or 18F-FDG and tumor grade on histology (P < .0001). Kayani et al published their second article comparing the 68Ga-DOTATATE to 18F-FDG PET/CT in Pulmonary Neuroendocrine Tumors [29]. They retrospectively reviewed 18 patients with primary and recurrent bronchial carcinoid tumors. They found that all typical carcinoids showed high uptake of 68Ga-DOTATATE (SUVmax ≥ 8.2), but 4 of 11 showed negative or minimal 18F-FDG uptake (SUVmax 1.7-2.9). All tumors of higher grade showed high uptake of 18F-FDG (SUVmax ≥ 11.7), but 3 of 5 showed only minimal accumulation of 68Ga-DOTATATE (SUVmax = 2.2-2.8). Neither case of diffuse idiopathic pulmonary neuroendocrine cell hyperplasia showed uptake of 68Ga-DOTATATE or 18F-FDG. Typical carcinoids showed significantly higher uptake of 68Ga-DOTATATE and significantly less uptake of 18F-FDG than did tumors of higher grade (P = 0.002 and 0.005). There was no instance of false-positive uptake of 68Ga-DOTATATE, but there were 3 sites of 18F-FDG uptake secondary to inflammation. 68Ga-DOTATATE was superior to 18F-FDG in discriminating endobronchial tumor from distal collapsed lung (P = 0.02). Conray et al compared the 68Ga-DOTATATE to 18F-FDG PET/CT in medullary thyroid carcinoma [30]. They found that 68Ga-DOTATATE PET/CT detected disease in 13 of 18 patients and 18F-FDG PET/CT in detected disease in 14 of 18 patients. As it was expected, 18F-FDG revealed a total of 28 metastatic MTC regions and 68Ga-DOTATATE 23 regions.
Conclusion
68Ga-DOTATATE PET/CT provides incremental diagnostic information compared to Octreoscan, MIBG scintigraphy and conventional imaging. 68Ga-DOTATATE also has been proved to have significant impact in management of patients with neuroendocrine tumors. Additional benefit of 68Ga-DOTATATE PET/CT include patient convenience with short time acquisition and lower radiation exposure signifying the important role of 68Ga-DOTATATE/CT in clinical practice of neuroendocrine and other somatostatin-avid malignancies.
References
- 1.Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB. One hundred years after carcinoid: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063–72. doi: 10.1200/JCO.2007.15.4377. [DOI] [PubMed] [Google Scholar]
- 2.Lamberts SW, Bakker WH, Reubi JC, Krenning EP. Somatostatin-receptor imaging in the localization of endocrine tumors. N Engl J Med. 1990;323:1246–9. doi: 10.1056/NEJM199011013231805. [DOI] [PubMed] [Google Scholar]
- 3.Krenning EP, Bakker WH, Breeman WA, Koper JW, Kooij PP, Ausema L, Lameris JS, Reubi JC, Lamberts SW. Localisation of endocrine-related tumours with radioiodinated analogue of somatostatin. Lancet. 1989;1:242–4. doi: 10.1016/s0140-6736(89)91258-0. [DOI] [PubMed] [Google Scholar]
- 4.Chopra A. 99mTc-ethylenediamine N,N’-diacetic acid/hydrazinonicotinamide-Tyr3-octreotide. In: Chopra A, editor. Molecular Imaging and Contrast Agent Database (MICAD) Bethesda: NIH; 2007. [Google Scholar]
- 5.Al-Nahhas A, Win Z, Szyszko T, Singh A, Khan S, Rubello D. What can gallium-68 PET add to receptor and molecular imaging? Eur J Nucl Med Mol Imaging. 2007;34:1897–1901. doi: 10.1007/s00259-007-0568-1. [DOI] [PubMed] [Google Scholar]
- 6.Bomanji J, Levison DA, Flatman WD, Horne T, Bouloux PM, Ross G, Britton KE, Besser GM. Uptake of iodine-123 MIBG by pheochromocytomas, paragangliomas, and neuroblastomas: a histopathological comparison. J Nucl Med. 1987;28:973–978. [PubMed] [Google Scholar]
- 7.Maurea S, Cuocolo A, Reynolds JC, Tumeh SS, Begley MG, Linehan WM, Norton JA, Walther MM, Keiser HR, Neumann RD. Iodine-131-metaiodobenzylguanidine scintigraphy in preoperative and postoperative evaluation of paragangliomas: comparison with CT and MRI. J Nucl Med. 1993;34:173–179. [PubMed] [Google Scholar]
- 8.Sankowski AJ, Ćwikla JB, Nowicki ML, Chaberek S, Pech M, Lewczuk A, Walecki J. The clinical value of MRI using single-shot echoplanar DWI to identify liver involvement in patients with advanced gastroenteropancreatic-neuroendocrine tumors (GEP-NETs), compared to FSE T2 and FFE T1 weighted image after i. v. Gd-EOB-DTPA contrast enhancement. Med Sci Monit. 2012;18:33–40. doi: 10.12659/MSM.882719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antunes P, Ginj M, Zhang H, Waser B, Baum RP, Reubi JC, Maecke H. Are radiogalliumlabelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur J Nucl Med Mol Imaging. 2007;34:982–993. doi: 10.1007/s00259-006-0317-x. [DOI] [PubMed] [Google Scholar]
- 10.Poeppel TD, Binse I, Petersenn S, Lahner H, Schott M, Antoch G, Brandau W, Bockisch A, Boy C. 68Ga-DOTATOC versus 68Ga-DOTATATE PET/CT in functional imaging of neuroendocrine tumors. J Nucl Med. 2011;52:1864–1870. doi: 10.2967/jnumed.111.091165. [DOI] [PubMed] [Google Scholar]
- 11.Walker RC, Smith GT, Liu E, Moore B, Clanton J, Stabin M. Measured human dosimetry of 68Ga-DOTATATE. J Nucl Med. 2013;54:855–60. doi: 10.2967/jnumed.112.114165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hofman MS, Kong G, Neels OC, Eu P, Hong E, Hicks RJ. High management impact of Ga-68 DOTATATE (GaTate) PET/CT for imaging neuroendocrine and other somatostatin expressing tumours. J Med Imaging Radiat Oncol. 2012;56:40–7. doi: 10.1111/j.1754-9485.2011.02327.x. [DOI] [PubMed] [Google Scholar]
- 13.Reubi JC, Landolt AM. High density of somatostatin receptors in pituitary tumors from acromegalic patients. J Clin Endocrinol Metab. 1984;59:1148–51. doi: 10.1210/jcem-59-6-1148. [DOI] [PubMed] [Google Scholar]
- 14.Krenning EP, Kwekkeboom DJ, Bakker WH, Breeman WA, Kooij PP, Oei HY, van Hagen M, Postema PT, de Jong M, Reubi JC. Somatostatin receptor scintigraphy with [111In-DTPAD-Phe1] - and [123I-Tyr3] -octreotide: the Rotterdam experience with more than 1000 patients. Eur J Nucl Med. 1993;20:716–731. doi: 10.1007/BF00181765. [DOI] [PubMed] [Google Scholar]
- 15.Zhernosekov KP, Filosofov DV, Baum RP, Aschoff P, Bihl H, Razbash AA, Jahn M, Jennewein M, Rösch F. Processing of Generator-Produced 68Ga for Medical Application. J Nucl Med. 2007;48:1741–1748. doi: 10.2967/jnumed.107.040378. [DOI] [PubMed] [Google Scholar]
- 16.Reubi JC, Schär JC, Waser B, Wenger S, Heppeler A, Schmitt JS, Mäcke HR. Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med. 2000;27:273–282. doi: 10.1007/s002590050034. [DOI] [PubMed] [Google Scholar]
- 17.Souvatzoglou M, Ziegler SI, Martinez MJ, Busch R, Dzewas G, Schwaiger M, Bengel F. Standardised uptake values from PET/CT images: comparison with conventional attenuation- corrected PET. Eur J Nucl Med Mol Imaging. 2007;34:405–412. doi: 10.1007/s00259-006-0196-1. [DOI] [PubMed] [Google Scholar]
- 18.Haug AR, Cindea-Drimus R, Auernhammer CJ, Reincke M, Wängler B, Uebleis C, Schmidt GP, Göke B, Bartenstein P, Hacker M. The role of 68Ga-DOTATATE PET/CT in suspected neuroendocrine tumors. J Nucl Med. 2012;53:1686–92. doi: 10.2967/jnumed.111.101675. [DOI] [PubMed] [Google Scholar]
- 19.Haug AR, Cindea-Drimus R, Auernhammer CJ, Reincke M, Beuschlein F, Wängler B, Uebleis C, Schmidt GP, Spitzweg C, Bartenstein P, Hacker M. Neuroendocrine tumor recurrence: diagnosis with 68Ga-DOTATATE PET/CT. Radiology. 2014;270:517–25. doi: 10.1148/radiol.13122501. [DOI] [PubMed] [Google Scholar]
- 20.Srirajaskanthan R, Kayani I, Quigley AM, Soh J, Caplin ME, Bomanji J. The role of 68Ga-DOTATATE PET in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. J Nucl Med. 2010;51:875–82. doi: 10.2967/jnumed.109.066134. [DOI] [PubMed] [Google Scholar]
- 21.Łapińska G, Bryszewska M, Fijołek-Warszewska A, Kozłowicz-Gudzińska I, Ochman P, Sackiewicz-Słaby A. The diagnostic role of 68Ga-DOTATATE PET/CT in the detection of neuroendocrine tumours. Nucl Med Rev Cent East Eur. 2011;14:16–20. doi: 10.5603/nmr.2011.0004. [DOI] [PubMed] [Google Scholar]
- 22.Win Z, Al-Nahhas A, Towey D, Todd JF, Rubello D, Lewington V, Gishen P. 68Ga-DOTATATE PET in neuroectodermal tumours: first experience. Nucl Med Commun. 2007;28:359–63. doi: 10.1097/MNM.0b013e32808ea0b0. [DOI] [PubMed] [Google Scholar]
- 23.Maurice JB, Troke R, Win Z, Ramachandran R, Al-Nahhas A, Naji M, Dhillo W, Meeran K, Goldstone AP, Martin NM, Todd JF, Palazzo F, Tan T. A comparison of the performance of 68Ga-DOTATATE PET/CT and ¹²³I-MIBG SPECT in the diagnosis and follow-up of phaeochromocytoma and paraganglioma. Eur J Nucl Med Mol Imaging. 2012;39:1266–70. doi: 10.1007/s00259-012-2119-7. [DOI] [PubMed] [Google Scholar]
- 24.Naji M, Zhao C, Welsh SJ, Meades R, Win Z, Ferrarese A, Tan T, Rubello D, Al-Nahhas A. 68Ga-DOTA-TATE PET vs. 123I-MIBG in identifying malignant neural crest tumours. Mol Imaging Biol. 2011;13:769–75. doi: 10.1007/s11307-010-0396-8. [DOI] [PubMed] [Google Scholar]
- 25.Schmid-Tannwald C, Schmid-Tannwald CM, Morelli JN, Neumann R, Haug AR, Jansen N, Nikolaou K, Schramm N, Reiser MF, Rist C. Comparison of abdominal MRI with diffusion-weighted imaging to 68Ga-DOTATATE PET/CT in detection of neuroendocrine tumors of the pancreas. Eur J Nucl Med Mol Imaging. 2013;40:897–907. doi: 10.1007/s00259-013-2371-5. [DOI] [PubMed] [Google Scholar]
- 26.Goel R, Shukla J, Bansal D, Sodhi K, Bhattacharya A, Kumar Marwaha R, Rai Mitta B. 68Ga-DOTATATE positron emission tomography/computed tomography scan in the detection of bone metastases in pediatric neuroendocrine tumors. Indian J Nucl Med. 2014;29:13–17. doi: 10.4103/0972-3919.125762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Armbruster M, Sourbron S, Haug A, Zech CJ, Ingrisch M, Auernhammer CJ, Nikolaou K, Paprottka PM, Rist C, Reiser MF, Sommer WH. Evaluation of neuroendocrine liver metastases: a comparison of dynamic contrast-enhanced magnetic resonance imaging and positron emission tomography/computed tomography. Invest Radiol. 2014;49:7–14. doi: 10.1097/RLI.0b013e3182a4eb4a. [DOI] [PubMed] [Google Scholar]
- 28.Kayani I, Bomanji JB, Groves A, Conway G, Gacinovic S, Win T, Dickson J, Caplin M, Ell PJ. Functional imaging of neuroendocrine tumors with combined PET/CT using 68Ga-DOTATATE (DOTA-DPhe1,Tyr3-octreotate) and 18F-FDG. Cancer. 2008;112:2447–55. doi: 10.1002/cncr.23469. [DOI] [PubMed] [Google Scholar]
- 29.Kayani I, Conry BG, Groves AM, Win T, Dickson J, Caplin M, Bomanji JB. A comparison of 68Ga-DOTATATE and 18F-FDG PET/CT in pulmonary neuroendocrine tumors. J Nucl Med. 2009;50:1927–32. doi: 10.2967/jnumed.109.066639. [DOI] [PubMed] [Google Scholar]
- 30.Conry BG, Papathanasiou ND, Prakash V, Kayani I, Caplin M, Mahmood S, Bomanji JB. Comparison of (68)Ga-DOTATATE and (18)F-fluorodeoxyglucose PET/CT in the detection of recurrent medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2010;37:49–57. doi: 10.1007/s00259-009-1204-z. [DOI] [PubMed] [Google Scholar]


