Abstract
Objective
This study evaluated color stability of acrylic denture teeth and base resins after 48 weeks of commercial denture cleanser simulation.
Materials and Methods
Two brands of denture teeth (Trubyte Portrait IPN, TP; SR Vivodent DCL, SR) in shades A1, B1, and C1 and three acrylic base resins (Lucitone, LU; Paragon, PA; Valplast, VA) prepared to manufacturer’s specifications, were exposed 10 hours daily to four cleansers (Clorox Bleach, CB; Polident 3-minute, PO3; Efferdent, EF; and Kleenite, KL) and distilled water (DW) control, approximating consumer overnight use. Color measurements used the CIE L*a*b* color space (0, 4, 12, 24, 36, and 48 weeks.) Color differences (ΔE*) at 48-weeks were subjected to 4-way analysis-of-variance (ANOVA). Mean values were compared with Fisher’s PLSD intervals (0.05 significance level).
Results
Mean color differences (ΔE*) demonstrated color changes in each material. ANOVA indicated color changes in teeth were significantly affected by both cleansers and teeth brand (p<0.05), but not shade. Color changes in base resins were significantly affected by cleansers (p<0.05), but not brand alone. Overall, KL produced the least color change while CB and PO3 produced the most for all materials.
Conclusions
After 48 weeks of daily simulation, TP teeth were more color-stable than SR in all cleansers except EF (p<0.0001). Base resin VA was less color-stable than LU and PA. Cleanser KL resulted in the lowest color changes.
Clinical Significance
All tested materials yield clinically acceptable color changes (ΔE*<3.5); all cleansing methods tested can be recommended, though Kleenite demonstrated the least change after 48-weeks.
Keywords: Color stability, Denture, Denture cleansers, Denture teeth, Denture base
INTRODUCTION
Several research studied suggested that whiteness and color of teeth are important factors in esthetic consideration of aging population.1,2 The resistance of denture teeth and denture base to color changes plays a significant role for patient and provider in the selection of materials for removable prostheses.3
Routine denture cleaning methods recommended by dental healthcare provider consist of mechanical and chemical methods.4 Mechanical cleaning of dentures includes using of brushes, microwave oven, and ultrasonic cleanser. Chemical cleaning of dentures includes the use of denture cleansing agents, antimicrobial solution, denture cream, dish washing agent, etc.5 Improper brushing technique could potentially cause wear of denture teeth and acrylic resin and adversely affect the esthetic of the denture.6 Chemical cleansing agents are increasing popular and have been routinely used by denture wearers. The advantages are ease of use especially for patients with impaired manual dexterity.7 However, there were reports on the long term whitening of denture teeth and acrylic resin base color that may contribute to visually detectible and/or esthetically unacceptable color changes of the denture.8,9 Replacing any component of denture dues to wear or discoloration is not desirable as it imposes additional cost in addition to the loss of denture wearing time for patients.
Denture cleansers vary in purpose, composition and method of application. They have been used in different capacities to remove deposits, debris, stains and bacteria. Denture cleansers can be alkaline peroxides (most commonly available), alkaline hypochlorites, dilute organic and inorganic acids, disinfectants, and enzymes.10 Ideal denture cleansing agents should be easy for patient to use, be compatible with all denture base materials, have disinfection property, effectively remove organic and inorganic substances, and help maintain color stability of denture teeth and denture base.5 However, there is no currently available product that could fulfill these requirements.7
While studies have considered the effect of denture cleansers on denture base acrylic resins.7–9,11–15 and soft denture lining materials16–17 well as the discoloration of denture teeth3,18–22 denture base acrylic resins23–24 and soft denture liners25 subjected to staining agents, there have not been recent studies on the simultaneous effects of denture cleansers on the color stability of denture teeth and denture base acrylic resins.
The aim of this study was to evaluate color stability of acrylic denture teeth and acrylic denture base resins after being subjected to commercial denture cleansers for 48 weeks using spectrophotometric analysis. The null hypothesis was that there would be no effect of long term usage of denture cleansers on color stability of denture teeth or denture base materials evaluated.
MATERIALS AND METHODS
Two brands of denture teeth (Trubyte Portrait IPN, TP; and SR Vivadent DCL, SR) each in shades A1, B1, and C1 and three acrylic base resins (Lucitone, LU; Paragon, PA; and Valplast, VA), all prepared according to manufacturer’s specifications, were exposed 10 hours daily to four commercial denture cleansers (Clorox Bleach, CB; Polident 3-minute, PO3; Efferdent, EF; and Kleenite, KL) and a distilled water control (DW), approximating consumer overnight use. The materials used in this study are shown in Table 1.
Table 1.
Variables and Manufacturer Information
| Denture Cleanser | Type | Manufacturer |
|---|---|---|
| Distilled Water (DW) | Control | |
| Clorox Bleach (CB) | Alkaline hypochlorite | The Clorox Co., Oakland, CA |
| Polident 3-minute Anti-Bacterial Denture Cleanser (PO3) | Alkaline Peroxide | GlaxoSmithKline Consumer Healthcare, Parsippany, NJ |
| Efferdent Anti-Bacterial Denture Cleanser (EF) | Alkaline Peroxide | Pfizer, Inc., Morris Plains, NJ |
| Kleenite Dental Cleanser (KL) | Alkaline Peroxide | Regent Labs, Inc., Deerfield Beach, FL |
| Denture Teeth | Manufacturer |
|---|---|
| Dentsply Trubyte Portrait IPN (TP) | Dentsply International, York, PA |
| Ivoclar Vivadent SR Vivodent DCL (SR) | Ivoclar Vivadent, Amherst, NY |
| Denture Base Acrylic Resin | Manufacturer |
|---|---|
| Dentsply Lucitone 199 (LU) | Dentsply International, York, PA |
| Paragon Denture Resin (PA) | Coltene/Whaledent, Mahwah, NJ |
| Valplast Flexible Resin (VA) | Glidewell Laboratories, Newport Beach, CA |
One denture tooth specimen consisted of one denture tooth of one brand in one shade and one acrylic base resin specimen consisted of one disc of base resin measuring 35 mm in diameter and 3 mm in thickness. Five specimens of each denture teeth and denture base resins were tested, for a total of 225 specimens (150 denture teeth and 75 denture base specimens). The cleansers and denture materials were prepared according to manufacturer specifications. Solutions were prepared using 110 mL (±5 mL) tap water at 140°F (± 2°) and one tablet of PO3 or EF, or ¾ capful of KL. In the case of the CB disinfection method, a 1% sodium hypochlorite solution was prepared from household bleach (6% NaOCl).26 After the specimen were prepared, they were stored in distilled water for 24 hours at 37°C.5 They were subsequently polished, rinsed and air-dried.
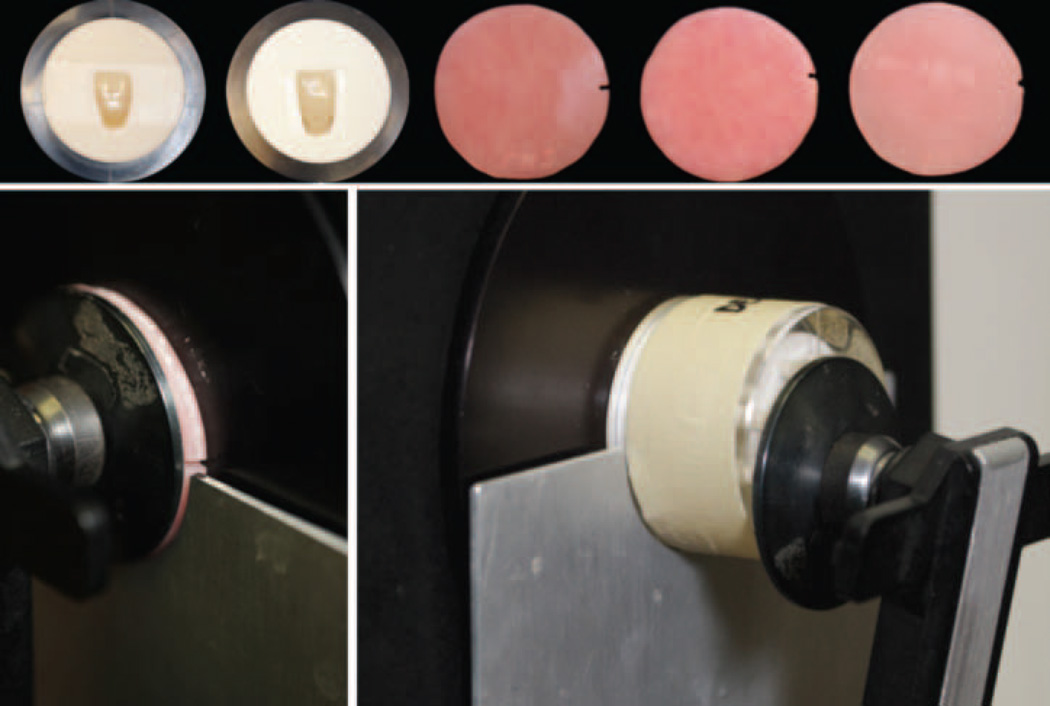
Five specimens of each variable were immersed daily in cleanser for 10 hours to approximate actual consumer overnight use. (Figure 1) KL, PO3, and EF while CB solution achieves disinfection after 1 minute of immersion.27 Between cleansings, the specimen were rinsed in tap water, and then stored in distilled water for 14 hours to prevent drying and distortion. Single operator performed this method for all materials used and repeated daily for 48 weeks (336 days or 3,360 hours) and color measurements were taken at baseline, 4, 12, 24, 36 and 48 weeks which were counted for 280, 840, 1,680, 2,520, and 3,360 hours of denture cleanser soaking times.
Figure 1.
After equipment calibration, color stability measurements were taken using a Color Eye 7000 spectrophotometer (Figure 2) and recorded using the CIE L*a*b color space and D65 lighting source. To ensure that the measurements were taken at the same area of each specimen, clear acrylic and white condensation silicone jigs were fabricated for the teeth and the denture resin discs were marked for positioning. (Figure 2) Denture teeth in jigs were measured using a rectangular 2mm × 6mm spectrophotometer aperture and 2° observer setting while resin discs used a 10 mm diameter circular aperture and 10° observer setting.
Figure 2.
Statistical analysis yielded mean values, standard deviations and variance data for comparison among the combinations of teeth, base, and cleanser. (Table 2) The color differences (ΔE*) at specified time periods were subjected to 3-way analysis of variance (ANOVA) (Table 3a–c). Mean values were compared with Fisher’s PLSD intervals calculated at the 0.05 significance level. In addition, the clinical relevance of the results have been interpreted through the literature findings for visual thresholds: 50:50% perceptibility threshold (ΔE*=1.8) and 50:50% acceptability threshold (ΔE*=3.5).27
Table 2.
Statistical Analysis
| ANOVA Table for ΔE at 48 weeks, Denture Teeth | |||||||
|---|---|---|---|---|---|---|---|
| DF | Sum of Squares |
Mean Square |
F- Value |
P- Value |
Lambda | Power | |
| Cleanser | 4 | 9.792 | 2.448 | 7.111 | <.0001 | 28.442 | 0.997 |
| Company | 1 | 2.042 | 2.042 | 5.931 | 0.0163 | 5.931 | 0.676 |
| Shade | 2 | 1.198 | 0.599 | 1.740 | 0.1800 | 3.479 | 0.346 |
| Cleanser*Company | 4 | 2.852 | 0.713 | 2.071 | 0.0888 | 8.284 | 0.597 |
| Cleanser*Shade | 8 | 1.131 | 0.141 | 0.411 | 0.9125 | 3.286 | 0.185 |
| Company*Shade | 2 | 1.736 | 0.868 | 2.522 | 0.0846 | 5.043 | 0.485 |
| Cleanser*Company*Shade | 8 | 3.919 | 0.490 | 1.423 | 0.1937 | 11.384 | 0.619 |
| Residual | 120 | 41.314 | 0.344 | ||||
| ANOVA Table for ΔE at 48 weeks, Denture Resin | |||||||
|---|---|---|---|---|---|---|---|
| DF | Sum of Squares |
Mean Square |
F-Value | P-Value | Lambda | Power | |
| Cleanser | 4 | 18.945 | 4.736 | 23.413 | <.0001 | 93.65 | 1.000 |
| Denture | 2 | 0.828 | 0.414 | 2.046 | 0.1382 | 4.091 | 0.393 |
| Ceanser*Denture | 8 | 11.635 | 1.454 | 7.189 | <.0001 | 57.515 | 1.000 |
| Residual | 60 | 12.137 | 0.202 | ||||
Table 3.
| a. Mean Color Change (ΔE) – Dentsply Teeth | |||||
|---|---|---|---|---|---|
| DW (control) | CB | PO3 | EF | KL | |
| ΔE (SD) | ΔE (SD) | ΔE (SD) | ΔE (SD) | ΔE (SD) | |
| TP shade A1 | |||||
| 4 weeks | 0.5 (0.4) | 1.1 (0.5) | 0.6 (0.3) | 1.1 (0.4) | 1.2 (0.4) |
| 12 weeks | 0.9 (0.6) | 1.1 (0.5) | 1 (0.4) | 1.0 (0.2) | 0.7 (0.4) |
| 24 weeks | 0.8 (0.4) | 0.9 (0.2) | 1.4 (0.5) | 1.6 (0.5) | 1.9 (0.5) |
| 36 weeks | 0.3 (0.3) | 0.5 (0.4) | 1.1 (0.3) | 1.0 (0.3) | 1.4 (0.8) |
| 48 weeks | 0.6 (0.5) | 1.5+ (0.5) | 1.3+ (0.4) | 1.2+ (0.5) | 0.5 (0.3) |
| TP shade B1 | |||||
| 4 weeks | 0.5 (0.2) | 0.6 (0.3) | 1.0 (0.6) | 0.9 (0.2) | 1.2 (0.7) |
| 12 weeks | 0.4 (0.3) | 0.7 (0.3) | 1.5 (0.5) | 1.0 (0.5) | 1.4 (0.4) |
| 24 weeks | 1.0 (0.7) | 1.1 (0.5) | 1.8 (0.7) | 1.4 (0.5) | 2.2 (0.5) |
| 36 weeks | 0.7 (0.3) | 0.7 (0.6) | 1.5 (0.5) | 0.9 (0.3) | 1.5 (0.5) |
| 48 weeks | 0.7 (0.4) | 0.7 (0.6) | 0.8 (0.5) | 1.1+ (0.5) | 0.5 (0.2) |
| TP shade C1 | |||||
| 4 weeks | 0.4 (0.2) | 0.5 (0.3) | 0.7 (0.4) | 1 (0.2) | 1.6 (0.9) |
| 12 weeks | 0.6 (0.3) | 1.0 (0.4) | 1.1 (0.3) | 1.3 (0.3) | 1.1 (0.4) |
| 24 weeks | 0.5 (0.3) | 1.3 (0.6) | 1.3 (0.4) | 1.7 (0.4) | 2.0 (0.6) |
| 36 weeks | 0.4 (0.1) | 0.9 (0.3) | 0.9 (0.2) | 1.0 (0.2) | 1.6 (0.9) |
| 48 weeks | 0.4 (0.2) | 0.5 (0.3) | 0.8+ (0.3) | 1.0+ (0.4) | 0.4 (0.3) |
| b. Mean Color Change (ΔE) – Ivoclar Teeth | |||||
|---|---|---|---|---|---|
| DW (control) | CB | PO3 | EF | KL | |
| ΔE (SD) | ΔE (SD) | ΔE (SD) | ΔE (SD) | ΔE (SD) | |
| SR shade A1 | |||||
| 4 weeks | 0.4 (0.4) | 0.6 (0.4) | 1.0 (0.6) | 0.9 (0.2) | 1.0 (0.5) |
| 12 weeks | 0.4 (0.3) | 1.0 (0.6) | 1.3 (0.5) | 1.4 (0.6) | 1.1 (0.6) |
| 24 weeks | 0.6 (0.3) | 0.5 (0.3) | 1.1 (0.5) | 1.4 (0.6) | 1.6 (1.0) |
| 36 weeks | 0.9 (0.4) | 0.5 (0.4) | 1.1 (0.4) | 0.9 (0.3) | 0.8 (0.5) |
| 48 weeks | 0.8 (0.3) | 1.1 (0.9) | 1.6+ (1.2) | 1.0 (0.3) | 0.8 (0.5) |
| SR shade B1 | |||||
| 4 weeks | 0.5 (0.3) | 1.2 (0.9) | 0.8 (0.6) | 0.9 (0.4) | 0.9 (0.4) |
| 12 weeks | 0.3 (0.0) | 1.5 (1.1) | 0.6 (0.3) | 0.9 (0.2) | 1.3 (0.8) |
| 24 weeks | 0.7 (0.3) | 0.9 (1.0) | 0.6 (0.3) | 1.1 (0.7) | 1.4 (0.8) |
| 36 weeks | 1.1 (0.2) | 0.9 (0.6) | 0.7 (0.4) | 0.7 (0.3) | 0.9 (0.8) |
| 48 weeks | 0.5 (0.4) | 1.7+ (1.4) | 1.1+ (0.8) | 0.7 (0.3) | 0.5 (0.3) |
| SR shade C1 | |||||
| 4 weeks | 1.0 (0.5) | 1.2 (0.6) | 1.0 (0.3) | 1.0 (0.5) | 0.7 (0.2) |
| 12 weeks | 1.1 (0.5) | 1.3 (0.7) | 1.0 (0.4) | 1.3 (0.4) | 0.6 (0.4) |
| 24 weeks | 1.4 (0.7) | 0.6 (0.6) | 0.6 (0.2) | 1.9 (1.0) | 1.9 (0.7) |
| 36 weeks | 1.0 (0.7) | 1.0 (0.3) | 1.0 (0.4) | 1.0 (0.6) | 1.0 (0.9) |
| 48 weeks | 1.2 (0.7) | 1.5 (0.7) | 1.6+ (0.9) | 0.7* (0.6) | 0.7* (0.5) |
| c. Mean Color Change (ΔE) – Acrylic Base Resin | |||||
|---|---|---|---|---|---|
| DW (control) | CB | PO3 | EF | KL | |
| ΔE (SD) | ΔE (SD) | ΔE (SD) | ΔE (SD) | ΔE (SD) | |
| LU | |||||
| 4 weeks | 1.8 (0.4) | 1.8 (0.7) | 1.3 (0.1) | 1.8 (0.2) | 1.9 (0.3) |
| 12 weeks | 2.4 (0.4) | 2.5 (1.0) | 1.9 (0.1) | 1.7 (0.2) | 1.4 (0.3) |
| 24 weeks | 2.4 (0.4) | 2.7 (0.9) | 2.0 (0.1) | 1.8 (0.2) | 1.7 (0.3) |
| 36 weeks | 2.4 (0.3) | 2.6 (1.0) | 1.9 (0.2) | 1.6 (0.2) | 1.3 (0.2) |
| 48 weeks | 1.4 (0.1) | 1.9+ (1.0) | 1.7 (0.2) | 1.3 (0.1) | 1.6 (0.2) |
| PA | |||||
| 4 weeks | 1.9 (0.2) | 2.0 (0.2) | 1.2 (0.2) | 2.1 (0.1) | 2.8 (0.1) |
| 12 weeks | 2.8 (0.2) | 2.8 (0.2) | 2.0 (0.1) | 2.1 (0.2) | 1.3 (0.2) |
| 24 weeks | 2.9 (0.2) | 3.1 (0.2) | 2.1 (0.1) | 2.3 (0.2) | 1.7 (0.2) |
| 36 weeks | 2.8 (0.2) | 2.9 (0.2) | 2.0 (0.1) | 2.1 (0.1) | 1.3 (0.2) |
| 48 weeks | 1.6 (0.1) | 1.9 (0.2) | 1.7 (0.1) | 2.0+ (0.1) | 0.4* (0.1) |
| VA | |||||
| 4 weeks | 0.5 (0.2) | 0.6 (0.3) | 0.7 (0.2) | 2.6 (1.2) | 1.7 (0.1) |
| 12 weeks | 1.4 (0.1) | 1.6 (0.1) | 1.4 (0.2) | 2.6 (1.2) | 1.1 (0.4) |
| 24 weeks | 1.6 (0.1) | 2.4 (0.1) | 1.7 (0.2) | 2.8 (1.1) | 1.6 (0.3) |
| 36 weeks | 1.7 (0.1) | 2.6 (0.1) | 1.6 (0.2) | 2.7 (1.1) | 1.3 (0.3) |
| 48 weeks | 1.7 (0.1) | 3.1+ (0.1) | 1.4 (0.1) | 2.3+ (1.3) | 0.3* (0.2) |
indicates significantly lower ΔE than control
indicates significantly higher ΔE than control
RESULTS
The null hypothesis was that long term usage of denture cleansers did not affect the color stability of denture teeth nor denture base materials evaluated was rejected. Mean ΔE values comparing baseline values to color measurements at 4, 12, 24, 36, and 48 weeks demonstrate color change in each material over time. (Table 3a–c) ANOVA statistical analysis (Table 2) indicates color change in denture teeth is significantly (P<0.05) affected by cleanser manufacturer and denture teeth manufacturer, but not by shade or specific combinations of variables. Color change in denture acrylic base resin is significantly (P<0.05) affected by cleanser manufacturer as well as the combination of cleanser and acrylic resin manufacturer, but not by acrylic resin manufacturer alone.
SR shades generally experienced more color change than TP shades in all solutions except EF. In EF group, TP experienced more color change than SR (P<0.05). Among denture acrylic base resins, VA shows more color change in CB and EF cleansers, LU shows more change in KN cleanser (P<0.05).
Table 3a: after 48 weeks, TP A1 that were immersed in CB, PO3 and EF solutions demonstrated significant color change compared to the DW (control) group (P<0.05). TP A1 in KL solution showed less color change than the control group. TP B1 had significant color change in EF solution compared to the control (P<0.05). In KL and CB, teeth experienced less color change than the control. TP C1 in KN showed less color change than the control group, while in PO3 and EF had significant color change (P<0.05).
Table 3b: SR A1 in KL showed less color change at 48 weeks than the control while PO3 showed significantly more color change (P<0.05). In shade B1, SR showed significantly more color change in CB and PO3 (P<0.05) but similar change in EF and KL when compared to the control. SR C1 showed significantly more color change when immersed in PO3 but significantly less color change in both EF and KL as compared with the control group (P<0.05).
Table 3c: LU specimen immersed in CB showed significantly more color change after 48 weeks than the control group (P<0.05). In EF solution, LU showed less color change than the control group. PA denture resin showed significantly more color change when immersed in EF solution and significantly less color change while immersed in KL solution as compared to the control (P<0.05). VA showed significantly more color change in CB and EF than the control group. Immersed in PO3 solution, VA showed less color change and in KL showed significantly less color change than the control group (P<0.05).
DISCUSSION
Color stability is a significant factor affecting longevity of dental prostheses. In addition to the reference used for interpretation of visual thresholds,27 ΔE* of 1.029 and 2.632 were reported as 50:50% perceptibility thresholds for direct restorative dental materials and denture teeth, respectively. Some of reported 50:50% acceptability thresholds include ΔE values of 2.7 (resin composite disks),30 3.3 direct restorative dental materials,31 and 5.5 (denture teeth).32
The esthetic, color stability, and visual threshold in restorative dentistry have been evaluated in numbers of studies.33–37 In this study, color changes of denture teeth were ranged from 0.3–2.2 in TP group and 0.3–1.9 in SR group. Color changes of acrylic resin denture bases were ranged from 1.3–2.7 in LU group. 0.4–2.9 in PA group, and 0.3–3.1 in VA group. There were none of any group that had ΔE ≥ 3.5, therefore, all color changes after 48-week were considered clinically acceptable.
Dentsply Trubyte reported the introduction of their denture teeth with decrease the potential for discoloration while Ivoclar Vivadent introduced denture teeth with solvent resistant (SR) and provides stability of the shade.3 The results from this study showed that color changes of all denture teeth were considered clinically acceptable (ΔE < 3.5) after subjected to 48-week of exposure to 4 cleansers. However, Dentsply Trubyte denture teeth were more color stable than Ivoclar Vivadent SR teeth in all denture cleansers except Efferdent (p<0.0001).
While color change over the test period have been determined to be clinically acceptable by current standards, the results demonstrated that denture base resins showed more color changes when compared to the denture teeth in this study. Among all 3 resin denture bases, Valplast soaked in Clorox after 48-week showed the highest color changes (ΔE = 3.1).
Overall after 48-week, Kleenite denture cleanser, a liquid denture cleanser, demonstrated the least effect on the color stability of all materials tested. Efferdent and Polident, tablet denture cleanser, had more whitening effect on the color stability of all materials especially with Polident 3 minutes. This may be due to the higher peroxide content and level of oxygenation.4,16 Efferdent used in this study was designed to use overnight but Polident 3 minutes was not. Three minutes formula contained TAED which is an organic compound which activates the oxidizers (oxygene booster) in Polident MicroClean Formula to form peracetic acid. Paracetic acid provides antifungal and antibacterial action and has stronger antimicrobial action than active oxygen products alone as in traditional tablets. Therefore, it is recommended for use during short period of cleaning not overnight. To follow the product instructions on the package is imperative especially when soaking complete dentures. In contrast, 3 minutes formula may be used for other appliances that have no esthetic component such as clear acrylic occlusal guard. The stronger whitening effect would add a positive value to this type of appliance.
Because there have not been recent studies on the effects of denture cleansers on the color stability of denture teeth. There was only one study that comparable to our study related to the color stability of acrylic resin denture base immersed in denture cleansers over long period of time. The results from Paranhos HdeFl et al (2013),15 showed color changes (ΔE = 2.3) of Lucitone 550 after immerse in Alkaline Peroxide (Corega tablet: product of GlaxoSmithKline, UK similar to Polident in our study) after 4,384 hours (1.5 years, 548 days, 8 hours/day). Our study showed color changes (ΔE = 1.6) of Lucitone 199 after immerse in similar Alkaline Peroxide (Polident tablet: product of GlaxoSmithKline, UK) after 3,360 hours (48 weeks, 336 days, 10 hours/day). With 1,024 hours longer immersion in Alkaline Peroxide cleansing tablet, the color changes increases 0.69 point. Still, the value does not exceed clinical acceptable changes after 1.5 years. Further study of these materials using longer aging term would be fruitful due to majority of denture wearers retains their dentures longer than 1.5 years. Future studies may also include new formulas of denture cleansers such as ones designed for metal partial and overnight whitening for occlusal guard.
CONCLUSION
After 48 weeks of simulated daily use of denture cleansers, Dentsply Trubyte denture teeth were more color stable than Ivoclar Vivadent SR teeth in all denture cleansers except Efferdent (p<0.0001). Valplast acrylic base resin was less color stable than Lucitone and Paragon. Kleenite denture cleanser demonstrated the least effect on the color stability of all materials tested. All tested materials yield clinically acceptable color change after subjected to 48-week of exposure.
ACKNOWLEDGMENT
The study was supported by NIH T32DE015355 grant. DENTSPLY Prosthodontics and Ivoclar Vivadent supplied denture teeth. The University of Texas Health Science Center School of Dentistry and Miracle Dental Labs provided denture resins and processing.
Footnotes
Disclosure Statement
The authors do not have any financial interest in any of the companies whose products are included in this article.
REFERENCES
- 1.Goldstein RE, Lancaster JS. Survey of patient attitudes toward current esthetic procedures. J Prosthet Dent. 1984;52:775–780. doi: 10.1016/s0022-3913(84)80001-3. [DOI] [PubMed] [Google Scholar]
- 2.Neumann LM, Christensen C, Cavanaugh C. Dental esthetic satisfaction in adults. J Am Dent Assoc. 1989;118:565–570. doi: 10.14219/jada.archive.1989.0077. [DOI] [PubMed] [Google Scholar]
- 3.Gregorius WC1, Kattadiyil MT, Goodacre CJ, et al. Effects of ageing and staining on color of acrylic resin denture teeth. J Dent. 2012;40(Suppl 2):e47–e54. doi: 10.1016/j.jdent.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Nikawa H, Hamada T, Yamashiro H, et al. A review of in vitro and in vivo methods to evaluate the efficacy of denture cleansers. Int J Prosthodont. 1999;12:153–159. [PubMed] [Google Scholar]
- 5.Jagger DC, Harrison A. Denture cleansing – The best approach. Br Dent J. 1995;178:413–417. doi: 10.1038/sj.bdj.4808788. [DOI] [PubMed] [Google Scholar]
- 6.Freitas-Pontes KM, Silva-Lovato CH, Paranhos HF. Mass loss of four commercially available heat-polymerized acrylic resins after toothbrushing with three different dentifrices. J Appl Oral Sci. 2009;17:116–121. doi: 10.1590/s1678-77572009000200009. [DOI] [PubMed] [Google Scholar]
- 7.Sato S, Cavalcante MR, Orsi IA, et al. Assessment of flexural strength and color alteration of heat-polymerized acrylic resins after simulated use of denture cleansers. Braz Dent J. 2005;16:124–128. doi: 10.1590/s0103-64402005000200007. [DOI] [PubMed] [Google Scholar]
- 8.Unlü A, Altay OT, Sahmali S. The role of denture cleansers on the whitening of acrylic resins. Int J Prosthodont. 1996;9:266–270. [PubMed] [Google Scholar]
- 9.Buyukyilmaz S, Ruyter IE. Color stability of denture base polymers. Int J Prosthodont. 1994;7:372–382. [PubMed] [Google Scholar]
- 10.Moore TC, Smith DE, Kenny GE. Sanitization of dentures by several denture hygiene methods. J Prostet Dent. 1984;52:158–163. doi: 10.1016/0022-3913(84)90087-8. [DOI] [PubMed] [Google Scholar]
- 11.Hong G, Murata H, Li Y, et al. Influence of denture cleansers on the color stability of three types of denture base acrylic resin. J Prosthet Dent. 2009;101:205–213. doi: 10.1016/S0022-3913(09)60032-9. [DOI] [PubMed] [Google Scholar]
- 12.McNeme SJ, von Gonten AS, Woolsey GD. Effects of laboratory disinfecting agents on color stability of denture acrylic resins. J Prosthet Dent. 1991;66:132–136. doi: 10.1016/0022-3913(91)90359-5. [DOI] [PubMed] [Google Scholar]
- 13.May KB, Razzoog ME, Koran A, et al. Denture base resin: Comparison study of color stability. J Prosthet Dent. 1992;68:78–82. doi: 10.1016/0022-3913(92)90290-q. [DOI] [PubMed] [Google Scholar]
- 14.Garcia RCMR, Junior JAdS, Rached RN, et al. Effect of denture cleansers on the surface roughness and hardness of a microwave-cured acrylic resin and dental alloys. J Prosthodont. 2004;13:173–178. doi: 10.1111/j.1532-849X.2004.04028.x. [DOI] [PubMed] [Google Scholar]
- 15.Paranhos Hde F1, Peracini A, Pisani MX, Oliveira Vde C, de Souza RF, Silva-Lovato CH. Color stability, surface roughness and flexural strength of an acrylic resin submitted to simulated overnight immersion in denture cleansers. Braz Dent J. 2013;24:152–156. doi: 10.1590/0103-6440201302151. [DOI] [PubMed] [Google Scholar]
- 16.Nikawa H, Iwanaga H, Hamada T, et al. Effects of denture cleansers on direct soft denture lining materials. J Prosthet Dent. 1994;72:657–662. doi: 10.1016/0022-3913(94)90300-x. [DOI] [PubMed] [Google Scholar]
- 17.Anil N, Hekimoglu C, Sahin S. Color stability of heat-polymerized and autopolymerized soft denture liners. J Prosthet Dent. 1999;81:481–484. doi: 10.1016/s0022-3913(99)80018-3. [DOI] [PubMed] [Google Scholar]
- 18.Koksal T, Dikbas I. Color stability of different denture teeth materials against various staining agents. Dent Mat J. 2008;27:139–144. doi: 10.4012/dmj.27.139. [DOI] [PubMed] [Google Scholar]
- 19.Liberman R, Combe EC, Piddock V, et al. Color changes in acrylic teeth – comparison of an objective and subjective method. J Oral Rehab. 1996;23:464–469. doi: 10.1111/j.1365-2842.1996.tb00880.x. [DOI] [PubMed] [Google Scholar]
- 20.Mutlu-Sagesen L, Ergun G, Ozkan Y, et al. Color stability of different denture teeth materials: an in vitro study. J Oral Sci. 2001;43:193–205. doi: 10.2334/josnusd.43.193. [DOI] [PubMed] [Google Scholar]
- 21.Rosentritt M, Esch J, Behr M, et al. In vivo color stability of resin composite veneers and acrylic resin teeth in removable partial dentures. Quintessence International. 1998;29:517–522. [PubMed] [Google Scholar]
- 22.Silva PM, Acosta EJ, Jacobina M, et al. Effect of repeated immersion solution cycles on the color stability of denture tooth acrylic resins. J Appl Oral Sci. 2011;19:623–627. doi: 10.1590/S1678-77572011000600013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hersek N, Canay S, Uzun G, et al. Color stability of denture base acrylic resins in three food colorants. J Prosthet Dent. 1999;81:375–379. doi: 10.1016/s0022-3913(99)80001-8. [DOI] [PubMed] [Google Scholar]
- 24.Polyzois GL, Yannikakis SA, Zissis AJ. Color stability of visile-light-cured, hard direct denture reliners: an in vitro investigation. Int J Prosthodont. 1999;12:140–146. [PubMed] [Google Scholar]
- 25.Saraç D1, Saraç YS, Kurt M, et al. The effectiveness of denture cleansers on soft denture liners colored by food colorant solutions. J Prosthodont. 2007;16:185–191. doi: 10.1111/j.1532-849X.2006.00170.x. [DOI] [PubMed] [Google Scholar]
- 26.Azevedo A, Machado AL, Vergani CE, et al. Effect of Disinfectants on the Hardness and Roughness of Reline Acrylic Resins. J Prosthodont. 2006;15:235–242. doi: 10.1111/j.1532-849X.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 27.Ghinea R, Pérez M, Herrera L, et al. Color difference thresholds in dental ceramics. J Dent. 2010;38(Suppl 2):e57–e64. doi: 10.1016/j.jdent.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Lee D, Howlett J, Pratten J, et al. Susceptibility of MRSA biofilms to denture-cleansing agents. FEMS Microbiology Letter. 2009;291:241–246. doi: 10.1111/j.1574-6968.2008.01463.x. [DOI] [PubMed] [Google Scholar]
- 29.Kuehni FG, Marcus RT. An experiment in visual scaling of small color differences. Color Research and Application. 1979;4:83–91. [Google Scholar]
- 30.Regain JC, Johnston WM. Color acceptance of direct dental restorative materials by human observers. Color Research and Application. 2000;25:278–285. [Google Scholar]
- 31.Ruyter IE, Nilner K, Moller B. Color stability of dental composite resin materials for crown and bridge veneers. Dent Mat. 1987;3:246–251. doi: 10.1016/S0109-5641(87)80081-7. [DOI] [PubMed] [Google Scholar]
- 32.Douglas RD, Steinhauer TJ, Wee AG. Intraoral determination of the tolerance of dentists for perceptibility and acceptability of shade mismatch. J Prosthet Dent. 2007;97:200–208. doi: 10.1016/j.prosdent.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Sabatini C, Campillo M, Aref J. Color Stability of Ten Resin-Based Restorative Materials. J Esthet Rest Dent. 2012;24:185–199. doi: 10.1111/j.1708-8240.2011.00442.x. [DOI] [PubMed] [Google Scholar]
- 34.Tuncer S, Demirci M, Tiryaki M, et al. The Effect of a Modeling Resin and Thermocycling on the Surface Hardness, Roughness, and Color of Different Resin Composites. J Esthet Rest Dent. 2013;25:404–419. doi: 10.1111/jerd.12063. [DOI] [PubMed] [Google Scholar]
- 35.Aguiar FHB, Georgetto MH, Soares GP, et al. Effect of Different Light-Curing Modes on Degree of Conversion, Staining Susceptibility and Stain's Retention Using Different Beverages in a Nanofilled Composite Resin. 2011;23:106–144. doi: 10.1111/j.1708-8240.2011.00406.x. [DOI] [PubMed] [Google Scholar]
- 36.Patras M, Kourtis S, Sykaras N. Creating Natural-Looking Removable Prostheses: Combining Art and Science to Imitate Nature. 2012;24:160–168. doi: 10.1111/j.1708-8240.2011.00493.x. [DOI] [PubMed] [Google Scholar]
- 37.Paravina RD, Swift EJ. Color in Dentistry: Match me, Match me not. 2009;21:133–139. doi: 10.1111/j.1708-8240.2009.00246.x. [DOI] [PubMed] [Google Scholar]