Abstract
Purpose/Objective
People with Multiple Sclerosis (MS) experience higher levels of depression and anxiety than the general population. This is the first study to examine the relationship of worry about affording health care and symptoms in MS.
Methods
People with MS (n=405) were recruited for a needs assessment study. Participants completed a structured telephone interview measuring depression, anxiety, fatigue, sleep disturbance, pain interference, social function and perceived cognitive functioning and rated their worry about the following: premiums increasing, income decreasing, affording health care services, insurance dropping coverage, and affording prescriptions. Multiple regression analyses controlled for age, gender, disability status, education, income and health insurance coverage.
Results
The highest rated worry was inability to afford health care services. Higher health care worry was reported by women, younger participants, participants with lower incomes and those with only private (vs. public) insurance. Total level of health care worry was significantly related to depression, anxiety, fatigue, sleep disturbance, pain interference, social function and perceived cognitive functioning.
Conclusion
Health care worry was significantly related to psychological, physical and cognitive symptoms. Future research should compare health care worry in MS to other populations (i.e. healthy adults) and should examine changes in health care worry over time.
Keywords: Worry, health insurance, health care, depression, anxiety
People with Multiple Sclerosis (MS) experience increased stress, anxiety and depression and those with increased perceived stress have worse adjustment (Dennison, Moss-Morris, & Chalder, 2009). Worry in MS has been less well studied even though worry is often the cause of elevated anxiety and distress. Worry is a form of perseverative cognition, characterized by recurrent thoughts about potential negative events and attempts to mentally solve these future problems (Andrews et al., 2010). Worry is hypothesized as one way through which stress leads to worse health by prolonging the effects of stressful events on immune and endocrine function (Brosschot, Gerin, & Thayer, 2006). While a small amount of worry is normal and useful for problem solving especially for people with an unpredictable disease such as MS, research suggests heightened worry may be particularly problematic for people with MS (Bruce & Arnett, 2009).
Studies suggest general and MS-specific worry (obtaining medication, financial problems due to MS, being a burden to family) are elevated and common in people living with MS (Bruce & Arnett, 2009; Iezzoni & Ngo, 2007; Iezzoni, Ngo, & Kinkel, 2008; Mackereth, Booth, Hillier, & Caress, 2009). People with MS often report more worries than people without MS and this difference appears stronger for women with MS and for health-related worries instead of general worry (Buchanan et al., 2010; Buchanan et al., 2011; Pfaffenberger et al., 2011; Thornton, Tedman, Rigby, Bashforth, & Young, 2006). People with MS also have higher levels of worry than those with spinal cord injury, comparable levels of worry to those with rheumatoid arthritis and lower levels of worry than those with chronic fatigue syndrome (Lankhorst et al., 1996; Taillefer, Kirmayer, Robbins, & Lasry, 2002, 2003). One study found that higher general worry was related to worse outcomes such as increased disability, sleep disturbance, social fatigue, pain interference and worse problem solving on an objective neuropsychological measure and these relationships remained after controlling for anxiety (Bruce & Arnett, 2009).
The majority of past research has examined levels of general and illness-specific worry in people with MS. Given the recent increases in costs of MS treatments (Hauser & Johnston, 2012; Stavnitser, Patel, Miller, & Matlin, 2013), examining worry about affording health care is particularly timely. However, no study has examined whether worry about affording health care, such as affording medication and maintaining health insurance coverage, are also related to worse psychological and physical outcomes. While any effect of insurance coverage on objective health measures is debatable (Levy & Meltzer, 2008; Medicine, 2009), recent studies have suggested that health insurance coverage may improve patient-reported outcomes. Research from the Oregon Experiment, which examined the effects of Medicaid coverage assigned through a lottery, found that health insurance coverage improved financial stability, feelings of happiness and perceived health and reduced depressive symptoms (Baicker & Finkelstein, 2011; Baicker et al., 2013). These results suggest worry about affording healthcare coverage (hereafter referred to as health care worry) could be a factor in psychological and physical outcomes. The current study examined the association of health care worry and depression, anxiety, pain interference, fatigue, sleep disturbance, social function and self-reported cognitive problems. Due to the lack of previous research, an exploratory approach was used.
Methods
Participants and Procedures
This study was conducted following approval from the Institutional Review Board. To be eligible, participants had to self-report being diagnosed with MS by a physician, be at least 18 years of age and able to read and write English. Participants were recruited from the local Chapter of the National MS Society (MS Society Chapter) member list. A sample of 3,000 members of the MS Society Chapter was contacted and a total of 405 people with MS completed the survey, including the section on health care worry, between April and June 2011. Participants from rural areas, on Medicaid and recently diagnosed with MS were oversampled. See Figure 1 for flow of participant recruitment, response rates and reasons for not completing the survey. The response rate was 22% for all people the researchers attempted to contact; however, of those who spoke to the research team, 60% consented to participate and 70% of people who spoke to the research team and were eligible consented to participate.
Figure 1.
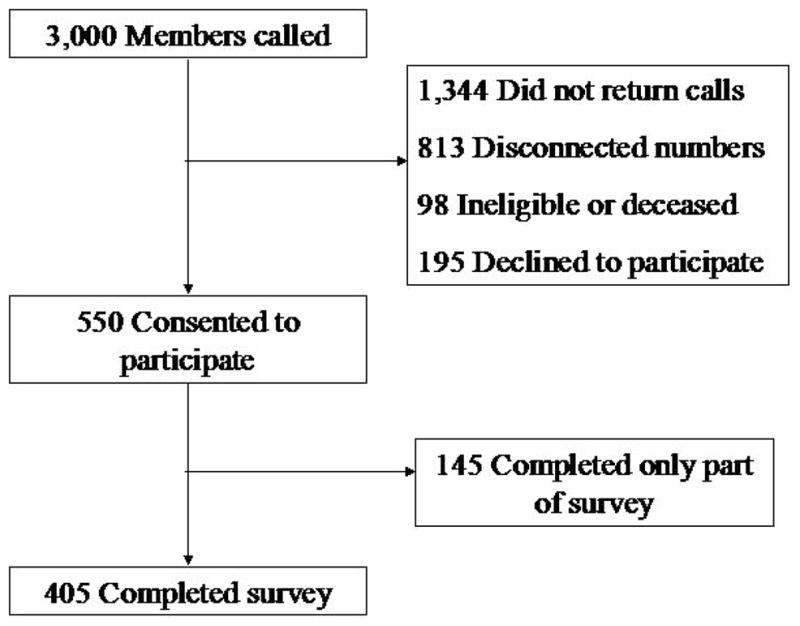
Participant flow diagram. Of the 3,000 members of the Greater Northwest Chapter of the National MS Society who we attempted to contact, 405 completed the survey.
Measures
Health Care Worry
Questions on worry about affording health care were developed using input from the local chapter of the Multiple Sclerosis Society, and focus groups of people with MS. Eight moderated focus groups were conducted with 35 people with MS (seven of the focus groups) and 10 caregivers (one of the focus groups) identified through the Multiple Sclerosis Society and a local adult day home. Groups were conducted in Alaska, Montana and Washington state. Five questions were developed and asked participants to rate how much they worried about various aspects of health care coverage on a 4-point scale (0=“not at all worried”, 1=“not too worried”, 2=“somewhat worried”, and 3=“very worried”). The item content of the five worry questions was as follows: “your insurance company will raise your premiums so much you will no longer be able to afford your health insurance” (premiums increase); “your income will go down and you won’t be able to afford the cost of your current health insurance coverage” (income decrease); “you won’t be able to afford the health care services you need” (healthcare services); “your insurance company will drop your coverage” (insurance dropped); and “you won’t be able to afford the prescription drugs you need” (medications).
Psychological and Physical Outcomes
Depressive symptoms, anxiety, fatigue, sleep disturbance, pain interference and social functioning were measured using the Patient Reported Outcomes Measurement Information System (PROMIS, (Cella et al., 2010)) Profile 29 version 1. PROMIS profile 29 consists of four to five items per construct and the instruments were developed with a sample that included people with MS. Each item is rated on a 1 to 5 scale, except for the level of pain intensity that uses a 0 to 10 rating scale. The depression and anxiety scales do not contain any items measuring physical symptoms (Pilkonis et al., 2011). The PROMIS instruments were developed using Item Response Theory (IRT)-based scores, which are transformed into t-scores with a mean of 50 (standard deviation of 10) representing the mean of the United States general population based on a large community sample matched to Census 2000 on age, gender and race/ethnicity (Liu et al., 2010; Reeve et al., 2007). Higher scores indicate better social function, more depressive symptoms, anxiety, fatigue, sleep disturbance, and pain interference. The PROMIS instruments have been used to measure symptoms and quality of life indicators in people with MS (Amtmann, Cook, Johnson, & Cella, 2011).
Neuro-QOL Executive Functioning and General Cognition Subscales
Perceived cognitive functioning was measured using the Executive Functioning and General Cognition subscales from the Neuro-QOL (Gershon et al., 2012). These instruments were created specifically to measure perceived cognitive function in those with neurological illness and people with MS were well represented in the development samples. Each short form consists of eight items rated on a 5-point scale. IRT-based scores are transformed into t-scores similar to the PROMIS measures (mean of 50 representing the US general population, standard deviation of 10) with higher scores indicating more perceived cognitive dysfunction.
Disability status
The mobility subscale of the self-reported Expanded Disability Status Scale (EDSS) was used to measure disability level (Bamer, Cetin, Amtmann, Bowen, & Johnson, 2007). The EDSS asks about participants’ mobility and use of assistive devices for mobility. Total scores range for 0 (normal) to 10 (death due to MS). However, as all participants were livings in this study, scores ranged from 1 to 9 with a mean of 4.70 (SD=3.02).
Analyses
Two sets of analyses were conducted. The first set examined the properties of the five health care worry items to determine if a total score could be used. Reliability (Cronbach’s alpha), inter-item correlations and item-total correlations were examined. The total score was also examined for floor and ceiling effects. A one-factor model was also fit to the five items using a polychoric correlation matrix and diagonally-weighted least squares in Lisrel 8.8. The following fit indices were used to evaluate fit: tests of perfect and close fit are not significant; root mean square error of approximation (RMSEA) less than .08; root mean square residual (RMSR) below .08; and comparative fit index (CFI) above .95. The second set of analyses examined the relationship of health care worry to various demographics using t-tests and correlations. The relationship of health care worry to the outcomes was examined using hierarchical multiple regression. Depressive symptoms, anxiety, sleep disturbance, fatigue, pain interference, social function and perceived cognitive functioning were the dependent variables. Covariates were entered in the first step to control for age, gender, education, income, EDSS and whether participants had health insurance. On the second step in the regressions, health care worry was entered. For the regression analyses, the total score for health care worry was entered, calculated by summing the values on the five items. A Bonferroni error correction was used across the eight analyses of each dependent variable as it is a very conservative correction. Because of this correction, alpha was set at .006 instead of .05 for the regressions.
Results
Participants reported a moderate amount of worry about health care. See Table 1 for demographics and disease information and frequencies of responses to the worry items. The majority of participants had health insurance (96.3%) consistent with previous samples (Minden, Frankel, Hadden, & Hoaglin, 2007). The highest rated worry was inability to afford healthcare services (mean=1.45, SD=1.11). The least amount of worry was for insurance being dropped (mean=.91, SD=1.04). Means and standard deviations for the remaining worries were as follows: premiums increase 1.34 (SD=1.11); income decrease 1.29 (SD=1.14); and medications 1.33 (SD=1.14). The mean score for the total healthcare worry scale was 6.32 (SD=4.62).
Table 1.
Demographics and Disease Information, n=405. PROMIS Profile 29, v. 1 and the Neuro-QOL scales were used to measure depressive symptoms, anxiety, fatigue, sleep disturbance, pain interference, social function and perceived cognition.
| Variable | Mean (SD) or % (n) |
|---|---|
| Age | 52.68 (12.91) |
| Sex, % female | 69.1% (280) |
| Education, Bachelor’s or higher | 38.0% (154) |
| Income >$40,000 | 51.8% (210) |
| Relationship Status | |
| Married/Civil Union | 60.2% (244) |
| Long-term relationship | 9.9% (40) |
| Divorced/Single/Separated/Widowed | 28.4% (115) |
| Race/Ethnicity | |
| Caucasian | 92.6% (375) |
| African American | 2.0% (8) |
| Hispanic | 2.0% (8) |
| Asian or Pacific Islander | 0.7% (3) |
| Native American | 0.7% (3) |
| Other/did not answer | 2.9% (12) |
| Currently employed | 29.4% (119) |
| Has health insurance coverage | 96.3% (390) |
| Medicaid | 16.3% (66) |
| Medicare | 44.2% (179) |
| Private Insurance | 64.4% (261) |
| MS Type | |
| Relapsing/Remitting | 58.8% (238) |
| Primary Progressive | 11.1% (45) |
| Secondary Progressive | 20.0% (81) |
| Progressive Relapsing | 1.0% (4) |
| Time since MS diagnosis, years | 14.72 (9.70) |
| Depressive Symptoms | 52.69 (9.77) |
| Anxiety | 52.82 (9.26) |
| Fatigue | 59.09 (9.34) |
| Sleep Disturbance | 52.47 (9.46) |
| Pain Interference | 56.25 (10.05) |
| Social Function | 44.24 (8.57) |
| Perceived Cognition, Executive Function | 42.38 (9.03) |
| Perceived Cognition, General | 39.67 (9.49) |
Analyses of the five healthcare worry items suggested that a total score was reasonable to use in the multiple regressions. Cronbach’s alpha for the total scale was .96. Inter-item correlations ranged from .728 to .906, indicating that items were sufficiently related. Item-total correlations were: premiums increase .881; income decrease .917; healthcare services .930; coverage dropped .807; and medications .903. A slight floor effect was present as 19% of the sample reported the lowest level of healthcare worry (score of 0) but a minimal ceiling effect was shown as only 6.4% of the sample reported the highest level of healthcare worry (score of 15). Results of the factor analysis showed sufficient factor loadings for all items: premiums increase .81; income decrease .92; healthcare services .92; coverage dropped .75; and medications .86. The model fit the data well as indicated by the fit indices: RMSEA=.078, RMSR=.027, and CFI=.99. The test of close fit was not significant (p=.10) but the test of perfect fit was significant (p<.001).
Analyses found statistically significant associations between health care worry and demographic characteristics. Women reported more health care worry than men (t(403)=−2.564, p=.011, Cohen’s d=−.276) and age was negatively related to health care worry (r=−.121, p=.015). People with incomes below $40,000 per year reported more health care worry than those with incomes above $40,000 (t(354)=3.352, p=.001, Cohen’s d=.355). Education was unrelated to health care worry (t(401)=.880, p=.379). People with only private insurance reported more health care worry than people with any public insurance such as Medicare (t(403)=2.239, p=.026, Cohen’s d=.225).
The results of the multiple regressions suggested that health care worry was statistically significantly related to several health outcomes. See Table 2 for results. The total healthcare worry score was significantly related (all ps<.001) to depression, anxiety, fatigue, sleep disturbance, pain interference, social function, perceived executive function and perceived general cognition such that more worry was associated with worse outcomes. Additional variance accounted by health care worry ranged from 5.8% (fatigue) to 12.3% (anxiety). To determine which outcomes were uniquely related to worry, we conducted another multiple regression in which health care worry was the dependent variable. Covariates (age, gender, education, income, EDSS, health insurance) were entered on the first step. On the second step, the eight outcomes were entered. Anxiety (β=.198, t(311)=2.548, p=.011) and sleep disturbance (β=.164, t(311)=2.878, p=.004) were significantly related to health care worry. Social role function (β=−.128, t(311)=−1.897, p=.059) and perceived executive function (β=−.145, t(311)=−1.840, p=.067) were nearly significantly related to health care worry. Depression, fatigue, pain interference and perceived general cognition were unrelated (all ps>.180).
Table 2.
Relationship of health care worry to psychological and physical outcomes. Health care worry was entered on the second step and the R2 change represents the additional variance accounted by worry beyond the covariates. R2 controls represents step 1 in the regression. Covariates (gender, age, EDSS/Disability score, education, income, health insurance/no insurance) not shown for clarity. N’s ranged from 335 (executive function) – 346 (anxiety).
| Outcome: Predictor |
Std. β | Unstandardized Coefficient | Standard Error | T-test | R2 Δ | R2 total |
|---|---|---|---|---|---|---|
| Depressive symptoms: | ||||||
| Total Health care worry | .317 | .671* | .107 | 6.249 | .094* | .178 |
| Anxiety: | ||||||
| Total Health care worry | .363 | .730* | .101 | 7.202 | .123* | .184 |
| Fatigue: | ||||||
| Total Health care worry | .250 | .505* | .106 | 4.751 | .058* | .119 |
| Sleep Disturbance: | ||||||
| Total Health care worry | .302 | .620* | .107 | 5.766 | .085* | .122 |
| Pain Interference: | ||||||
| Total Health care worry | .257 | .561* | .113 | 4.975 | .061* | .157 |
| Social Function: | ||||||
| Total Health care worry | −.262 | −.491* | .093 | −5.301 | .064* | .224 |
| Perceived Cognition, Executive Function: | ||||||
| Total Health care worry | −.276 | −.541* | .106 | −5.110 | .070* | .099 |
| Perceived General Cognition: | ||||||
| Total Health care worry | −.255 | −.527* | .110 | −4.778 | .061* | .094 |
EDSS= Expanded Disability Status Scale, Std=Standardized,
p<.001
Discussion
The results of this study suggest an association of health care worry with symptoms or health outcomes in people with Multiple Sclerosis. The study also found women, younger participants, those with less income and those with private insurance reported more health care worry. Health care worry accounted for a statistically significant amount of the variance in depressive symptoms, anxiety, fatigue, sleep disturbance, pain interference, social function, perceived executive function and perceived general cognition. More health care worry was related to more depressive symptoms, anxiety, fatigue, sleep disturbance and pain interference as well as worse social function and perceived cognition. Anxiety and sleep disturbance showed a particularly strong relationship to health care worry. This is understandable in the context of increasing prices of the disease modifying therapies used to slow progression of MS. The introduction of disease-modifying therapies has caused the cost of MS treatment to increase drastically (Hauser & Johnston, 2012; Stavnitser et al., 2013). The results of this study suggest that in addition to having financial implications, the rising cost of treatment for MS may also be related to worse psychological, physical and perceived cognitive functioning of people with MS.
The results of this study support the hypothesis that excessive perseverative cognition such as health care worry is related to worse health (Brosschot et al., 2006) and extends that research to people with MS. This also supports work on general worry in MS (Bruce & Arnett, 2009) that showed general worry was related to fatigue, sleep disturbance and pain. However, the relationship between health care worry and symptoms is likely bi-directional. More symptoms may lead to a person with MS worrying about maintaining health coverage as increased symptoms would indicate a need for more treatment.
Due to the potential detrimental correlates of worry in MS, this study has implications for clinical practice. People with MS reporting perceived cognitive dysfunction as well as other symptoms may also be experiencing additional distress from healthcare worry and clinicians may need to refer patients for treatment or to additional resources if needed. Additionally, providing treatments for the symptoms that are exacerbating the worry may also help provide relief. However, given recent changes in health care such as the Affordable Care Act, worry about affording health care may change and future research could examine the effects of these changes.
The study has several limitations that also indicate future areas for research. First, this was a cross-sectional study and longitudinal and treatment studies would be required to examine causation and directionality of the relationship between health care worry and outcomes. Second, this study oversampled several groups typically underrepresented in MS research (rural, progressive MS, men) and as a result their points of view are represented in these data, however this means the sample is not representative of the larger MS population. Information on disease modifying treatments was not collected on this sample and the potential moderating effects of these treatments on health care worry could not be tested. Additionally, we were unable to compare the MS sample to the general population or another medical population and were unable to compare health care worry to generalized worry. As is common for mail or phone surveys, the overall response rate was low but over 70% of people who spoke to the research team did consent to participate. Also, MS diagnosis and disease course were not confirmed with a physician. The health care worry scale only examined affording care and not worries about other aspects of care such as communicating with providers and was not compared to actual behavior such as utilization of health care. The scale was also new and had not been previously validated. Future research, in addition to examining causality, could also compare general worry and health care worry in predicting psychological and physical outcomes as well as examine health care worry in different groups (MS, healthy individuals, other chronic illnesses) to determine for whom this worry is elevated.
Impact Statement.
This study was the first to examine worry about affording health care in people with Multiple Sclerosis and found that worry about affording health care was related to worse symptoms.
Future research should examine the causal relationship between worry about affording health care and symptoms as well as what effects this worry.
Acknowledgments
The contents of this article were developed under a grant from the Department of Education, NIDRR grant number H133B080025. However, those contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the Federal Government. The authors would also like to thank the study participants as well as the research staff who contributed to this project. Dr. Wu is supported by a fellowship from the National Institute of Aging (T32 AG027677).
Contributor Information
Salene M. Jones, Email: wu.582@osu.edu, Group Health Research Institute, 1730 Minor Ave, Seattle, WA 98103, Telephone: (206) 287-2108
Dagmar Amtmann, University of Washington, Department of Rehabilitation Medicine, Seattle, WA, United States of America
References
- Amtmann D, Cook KF, Johnson KL, Cella D. The PROMIS initiative: involvement of rehabilitation stakeholders in development and examples of applications in rehabilitation research. Arch Phys Med Rehabil. 2011;92(10 Suppl):S12–19. doi: 10.1016/j.apmr.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G, Hobbs MJ, Borkovec TD, Beesdo K, Craske MG, Heimberg RG, Stanley MA. Generalized Worry Disorder: A Review of Dsm-Iv Generalized Anxiety Disorder and Options for Dsm-V. Depression and Anxiety. 2010;27(2):134–147. doi: 10.1002/Da.20658. [DOI] [PubMed] [Google Scholar]
- Baicker K, Finkelstein A. The effects of Medicaid coverage--learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–685. doi: 10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, Group OHS. The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamer AM, Cetin K, Amtmann D, Bowen JD, Johnson KL. Comparing a self report questionnaire with physician assessment for determining multiple sclerosis clinical disease course: a validation study. Mult Scler. 2007;13(8):1033–1037. doi: 10.1177/1352458507077624. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research. 2006;60(2):113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Bruce JM, Arnett P. Clinical correlates of generalized worry in multiple sclerosis. J Clin Exp Neuropsychol. 2009;31(6):698–705. doi: 10.1080/13803390802484789. [DOI] [PubMed] [Google Scholar]
- Buchanan RJ, Minden SL, Chakravorty BJ, Hatcher W, Tyry T, Vollmer T. A pilot study of young adults with multiple sclerosis: demographic, disease, treatment, and psychosocial characteristics. Disabil Health J. 2010;3(4):262–270. doi: 10.1016/j.dhjo.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Buchanan RJ, Zuniga MA, Carrillo-Zuniga G, Chakravorty BJ, Tyry T, Moreau RL, Vollmer T. A pilot study of Latinos with multiple sclerosis: demographic, disease, mental health, and psychosocial characteristics. J Soc Work Disabil Rehabil. 2011;10(4):211–231. doi: 10.1080/1536710X.2011.622959. [DOI] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Group PC. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennison L, Moss-Morris R, Chalder T. A review of psychological correlates of adjustment in patients with multiple sclerosis. Clin Psychol Rev. 2009;29(2):141–153. doi: 10.1016/j.cpr.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Gershon RC, Lai JS, Bode R, Choi S, Moy C, Bleck T, Cella D. Neuro-QOL: quality of life item banks for adults with neurological disorders: item development and calibrations based upon clinical and general population testing. Qual Life Res. 2012;21(3):475–486. doi: 10.1007/s11136-011-9958-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser SL, Johnston SC. Multiple sclerosis drugs: sticker shock. Ann Neurol. 2012;71(5):A5–6. doi: 10.1002/ana.23608. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Ngo L. Health, disability, and life insurance experiences of working-age persons with multiple sclerosis. Mult Scler. 2007;13(4):534–546. doi: 10.1177/1352458506071356. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Ngo LH, Kinkel RP. Working-age persons with multiple sclerosis and access to disease-modifying medications. Mult Scler. 2008;14(1):112–122. doi: 10.1177/1352458507080466. [DOI] [PubMed] [Google Scholar]
- Lankhorst GJ, Jelles F, Smits RC, Polman CH, Kuik DJ, Pfennings LE, Vleugels L. Quality of life in multiple sclerosis: the disability and impact profile (DIP) J Neurol. 1996;243(6):469–474. doi: 10.1007/BF00900502. [DOI] [PubMed] [Google Scholar]
- Levy H, Meltzer D. The impact of health insurance on health. Annu Rev Public Health. 2008;29:399–409. doi: 10.1146/annurev.publhealth.28.021406.144042. [DOI] [PubMed] [Google Scholar]
- Liu H, Cella D, Gershon R, Shen J, Morales LS, Riley W, Hays RD. Representativeness of the Patient-Reported Outcomes Measurement Information System Internet panel. J Clin Epidemiol. 2010;63(11):1169–1178. doi: 10.1016/j.jclinepi.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackereth PA, Booth K, Hillier VF, Caress AL. What do people talk about during reflexology? Analysis of worries and concerns expressed during sessions for patients with multiple sclerosis. Complement Ther Clin Pract. 2009;15(2):85–90. doi: 10.1016/j.ctcp.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Medicine, I. o. America’s Uninsured Crisis: Consequences for Health and Health Care. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Minden SL, Frankel D, Hadden L, Hoaglin DC. Access to health care for people with multiple sclerosis. Mult Scler. 2007;13(4):547–558. doi: 10.1177/1352458506071306. [DOI] [PubMed] [Google Scholar]
- Pfaffenberger N, Gutweniger S, Kopp M, Seeber B, Stürz K, Berger T, Günther V. Impaired body image in patients with multiple sclerosis. Acta Neurol Scand. 2011;124(3):165–170. doi: 10.1111/j.1600-0404.2010.01460.x. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, Group PC. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS) Med Care. 2007;45(5 Suppl 1):S22–31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- Stavnitser A, Patel NV, Miller AR, Matlin OS. Impact of New Oral Therapies on Multiple Sclerosis Cost and Utilization Trends. American Journal of Pharmacy Benefits. 2013;5:36–39. [Google Scholar]
- Taillefer SS, Kirmayer LJ, Robbins JM, Lasry JC. Psychological correlates of functional status in chronic fatigue syndrome. J Psychosom Res. 2002;53(6):1097–1106. doi: 10.1016/s0022-3999(02)00566-4. [DOI] [PubMed] [Google Scholar]
- Taillefer SS, Kirmayer LJ, Robbins JM, Lasry JC. Correlates of illness worry in chronic fatigue syndrome. J Psychosom Res. 2003;54(4):331–337. doi: 10.1016/s0022-3999(02)00332-x. [DOI] [PubMed] [Google Scholar]
- Thornton EW, Tedman S, Rigby S, Bashforth H, Young C. Worries and concerns of patients with multiple sclerosis: development of an assessment scale. Mult Scler. 2006;12(2):196–203. doi: 10.1191/135248506ms1273oa. [DOI] [PubMed] [Google Scholar]


