Abstract
Previous exploratory analyses suggest that the Oral Health Impact Profile (OHIP) consists of four correlated dimensions and that individual differences in OHIP total scores reflect an underlying higher-order factor. The aim of this report is to corroborate these findings in the Dimensions of Oral Health-Related Quality of Life (DOQ) Project, an international study of general population subjects and prosthodontics patients. Using the project's Validation Sample (N=5,022), we conducted confirmatory factor analyses in a sample of 4,993 subjects with sufficiently complete data. In particular, we compared the psychometric performance of three models: a unidimensional model, a four-factor model, and a bifactor model that included one general factor and four group factors. Using model fit criteria and factor interpretability as guides, the four-factor model was deemed best in terms of strong item loadings, model fit (RMSEA=0.05, CFI=0.99), and interpretability. These results corroborate our previous findings that four highly correlated factors—which we have named Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact —can be reliably extracted from the OHIP item pool. However, the good fit of the unidimensional model and the high inter-factor correlations in the four-factor solution suggest that OHRQoL can also be sufficiently described with one score.
Keywords: Oral health-related quality of life, Oral Health Impact Profile, dimensions, factor structure, confirmatory factor analysis
Introduction
The Oral Health Impact Profile, OHIP (1) is used by researchers and clinicians to assess the patient-perceived impact of oral conditions and dental interventions. As a measure of oral health-related quality of life (OHRQoL), the OHIP ought to accurately reflect the theoretical structure of patient-perceived oral health. In turn, the theoretical structure of OHRQoL may need revision in light of empirical analyses. A necessary condition for the OHIP to be a valid measure of OHRQoL is that OHIP items must represent the theoretical components of patient-perceived oral health. In other words, the OHIP should demonstrate structural validity.
Establishing structural validity is a multistep process. The results of an exploratory, hypothesis-generating analysis should be investigated with a confirmatory, hypothesis-testing analysis conducted on independent data. Our exploratory factor analysis (EFA) conducted as part of the Dimensions of Oral Health-Related Quality of Life (DOQ) Project (2) found four dimensions and a strong general factor for the 49-item OHIP (3). Specifically, we found one factor representing general OHRQoL and four factors representing more detailed aspects of oral health named Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact. As part of the DOQ Project, data were randomly split into two independent sets, a Learning Sample and a Validation Sample. The Learning Sample was used for the previously mentioned exploratory analyses, holding back the Validation Sample for confirmatory analyses.
In this report, confirmatory factor analysis (CFA) was applied to test the structures suggested by our exploratory factor analysis. Specifically, we tested the two major hypotheses (i) that the OHIP scores have a strong general factor and (ii) that the OHIP consists of the four dimensions found by the EFA.
Materials and methods
Study design, subjects and OHIP data
The study was a secondary data analysis. Data came from the Dimensions of Oral Health-Related Quality of Life (DOQ) Project (2). The project contains 49-item OHIP (1) data from general population subjects and prosthodontics patients of six countries with validated OHIP instruments (4-9). As part of the DOQ Project, we assigned OHIP responses to one of three data sets (2). The present study uses the Validation Sample, containing 5,022 subjects (3,172 general population subjects and 1,850 prosthodontic patients.) We studied the 46 OHIP items that did not refer to dentures specifically. Some subjects had a large number of missing responses such that an accurate characterization of an individual's OHRQoL status was compromised. Therefore, as in previous studies (10), subjects with five or more missing OHIP responses were omitted from the analysis. In the 4,993 remaining subjects, missing responses were imputed with the person's median response.
Each OHIP item describes a situation that impacts OHRQoL and asks subjects to rate how often they experienced that impact within a certain recall period, most often the last month (response categories ‘never’, ‘hardly ever’, ‘occasionally’, ‘fairly often’, and ‘very often’).
Data analysis
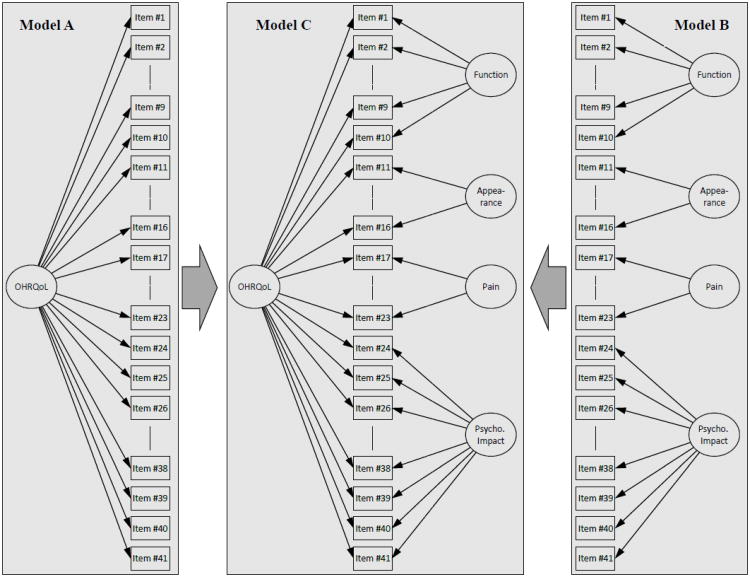
In our previous article (3), an EFA found both a dominant first factor and an interpretable four-factor solution with factors representing Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact. These results suggested both a unidimensional model (Figure 1, Model A) and a four-factor model (Figure 1, Model B) as plausible structures for the OHIP. Thus, we tested two primary hypotheses in the current study:
Figure 1. Graphical display of the unidimensional (A), four-factor (B), and bifactor (C) models.
Ovals represent latent factors, rectangles represent measured indicators for a latent factor. Lines connecting a latent factor to a measured indicator represent non-zero factor loadings.
Hypothesis 1: OHIP scores are unidimensional
Hypothesis 2: OHIP items have four dimensions, representing Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact.
Combining elements of both primary hypotheses in a bifactor model (11, 12), we also investigated a third hypothesis (Figure 1, Model C): OHIP items reflect both a general factor and four group (domain) factors representing Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact in a bifactor model.
The unidimensional (Figure 1, Model A) and the bifactor model (Figure 1, Model C) allow all OHIP items to load on a common (general) factor, representing perceived oral health. The four-factor (Figure 1, Model B) and bifactor (Figure 1, Model C) models assign items to factors (dimensions), under the classifications suggested by the EFA. These dimensions represent important areas within the overall OHRQoL framework where individuals perceive the impact from oral disorders and dental interventions.
The four-factor classification of items was found by considering items with factor pattern loadings of 0.45 or higher on at least one factor in the oblimin-rotated EFA (3). Of the 46 items not specifically referring to dentures, 41 items met our criterion for saliency. One item (headaches) loaded highly on both the Orofacial Pain and Psychosocial Impact factors, challenging its assignment to a dimension. For conceptual reasons we considered headaches an indicator of the Orofacial Pain dimension.
In the unidimensional model, all items loaded on the same (general) factor. In the four-factor model, all items loaded on exactly one domain factor, as suggested by the EFA. In the bifactor model, all items loaded on a general factor and exactly one domain factor. Whereas in the four-factor solution all factors were free to correlate, in the bifactor model all factors were constrained to be mutually orthogonal, i.e., not correlated.
To evaluate model fit for these three models, we used a set of indices to address various aspects of model fit. We included the log-likelihood chi-square test, the root mean square error of approximation (RMSEA), the comparative fit index (CFI) and the Tucker–Lewis index (TLI). Commonly applied guidelines for adequate model fit suggest (13): RMSEA: ≤0.06; and CFI, TLI: ≥0.95. Eigenvalues were calculated to provide further insight into dimensionality and Cronbach's alphas were calculated to provide estimates for factor reliability.
Responses to the OHIP occurred on a 5-point Likert scale and were positively skewed in the DOQ Project data set. Thus, each model was estimated by fitting the polychoric correlation matrix with diagonally weighted least squares (DWLS; (14)) estimation. This estimation procedure minimizes the squared distance between the observed and estimated polychoric correlations, weighted by the inverse asymptotic variances of these statistics. For each model, the latent factor(s) were constrained to have a mean of 0 and a variance of 1. All computations were performed with the statistical software R (15) using version 0.5-15 of the lavaan package (16).
Results
Primary hypothesis 1: OHIP scores are unidimensional
The unidimensional model fit the data well. The chi-square test (χ2(779) = 27142, p < 0.001) rejected the model, as we expected with our large sample size. Although the RMSEA for the unidimensional model came with 0.08 only close to the 0.06 guideline criterion, both comparative fit indices were much greater than 0.95. These fit statistics indicate acceptable model fit, suggesting that the OHIP covariance structure can be well-modeled by a latent, one-factor model. Standardized parameter estimates indicated that all items were strong indicators of a general factor (median loading of 0.81), with loadings ranging from 0.51 (sensitive teeth) to 0.88 (depressed). All loadings had small standard errors (0.006 to 0.012). The scree plot of the item polychoric correlation matrix also supported a strong general factor. Namely, the largest eigenvalue of the matrix was 24.8 and the second largest eigenvalue was 2.4, yielding a ratio of the first-to-the second eigenvalue of over 10. The third and the fourth eigenvalues were small with 1.6 and 1.3. In the aggregate, these findings support the hypothesis that OHIP data are well-characterized by a unidimensional model.
Primary hypothesis 2: OHIP items have four dimensions
The chi-square test rejected the four-dimensional model (χ2 (773) = 12123, p < 0.001). However, the four-dimensional model fit significantly better than the unidimensional model, as evidenced by a likelihood ratio test: χ2(6) =184.2. Model fit indices also improved over the unidimensional model (RMSEA: 0.05, comparative fit indices were >0.99). As expected, standardized loadings increased over the one-factor model, ranging from 0.60 (sensitive teeth) to 0.91 (uncomfortable about appearance) with small standard errors (0.005 to 0.013). The four dimensions were highly correlated with estimated correlations between 0.75 and 0.85 (Table 2) and Cronbach's alphas ranged from .85 to .95 (Table 1). Thus, based on the significant improvement in model fit and high factor loadings, we accepted the hypothesis that OHIP data have four dimensions.
Table 2. Fit Statistics for the unidimensional, four-factor, and bifactor models.
| Unidimensional Model | Four-Factor Model | Bifactor Model | |
|---|---|---|---|
| Model χ2 | 27142 | 12123 | 8458 |
| Model df | 779 | 773 | 738 |
| RMSEA | .082 | .054 | .046 |
| CFI | .986 | .994 | .996 |
| TLI | .986 | .994 | .996 |
Table 1. Standardized factor loadings and fit statistics for a unidimensional, four-factor, and bifactor model for OHIP data.
‘G’ denotes a general factor, ‘D1’ denotes Oral Function, ‘D2’ denotes Orofacial Appearance, ‘D3’ denotes Orofacial Pain, and ‘D4’ denotes Psychosocial Impact.
| Item | Unidimensional model | Four-factor model | Bifactor model | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| # | Content | G | D1 | D2 | D3 | D4 | G | D1 | D2 | D3 | D4 |
| 1. | Difficulty chewing | .78 | .82 | .80 | .03 | ||||||
| 2. | Trouble pronouncing words | .79 | .83 | .76 | .46 | ||||||
| 6. | Taste worse | .75 | .80 | .73 | .44 | ||||||
| 16. | Uncomfortable to eat | .82 | .87 | .85 | -.06 | ||||||
| 24. | Speech unclear | .83 | .87 | .79 | .48 | ||||||
| 25. | Others misunderstood | .78 | .83 | .76 | .41 | ||||||
| 26. | Less flavor in food | .79 | .84 | .78 | .39 | ||||||
| 28. | Avoid eating | .80 | .85 | .83 | .00 | ||||||
| 29. | Diet unsatisfactory | .83 | .89 | .86 | .01 | ||||||
| 32. | Interrupt meals | .82 | .88 | .86 | -.03 | ||||||
|
|
|||||||||||
| 3. | Noticed tooth which doesn't look right | .62 | .67 | .59 | .49 | ||||||
| 4. | Appearance affected | .73 | .79 | .71 | .40 | ||||||
| 19. | Worried | .76 | .83 | .75 | .38 | ||||||
| 20. | Self-conscious | .82 | .89 | .81 | .31 | ||||||
| 22. | Uncomfortable about appearance | .84 | .91 | .83 | .39 | ||||||
| 31. | Avoid smiling | .82 | .90 | .83 | .23 | ||||||
|
|
|||||||||||
| 10. | Painful aching | .73 | .85 | .70 | .48 | ||||||
| 11. | Sore jaw | .68 | .79 | .65 | .47 | ||||||
| 12. | Headaches | .65 | .76 | .65 | .24 | ||||||
| 13. | Sensitive teeth | .51 | .60 | .48 | .44 | ||||||
| 14. | Toothache | .66 | .76 | .62 | .48 | ||||||
| 15. | Painful gums | .71 | .82 | .68 | .45 | ||||||
| 17. | Sore spots | .71 | .82 | .68 | .45 | ||||||
|
|
|||||||||||
| 23. | Tense | .83 | .86 | .83 | .18 | ||||||
| 33. | Sleep interrupted | .78 | .80 | .72 | .36 | ||||||
| 34. | Upset | .82 | .84 | .81 | .15 | ||||||
| 35. | Difficult to relax | .82 | .84 | .76 | .39 | ||||||
| 36. | Depressed | .88 | .90 | .83 | .34 | ||||||
| 37. | Concentration affected | .87 | .89 | .79 | .41 | ||||||
| 38. | Been embarrassed | .85 | .88 | .86 | .15 | ||||||
| 39. | Avoid going out | .86 | .88 | .81 | .33 | ||||||
| 40. | Less tolerant of others | .84 | .86 | .74 | .47 | ||||||
| 41. | Trouble getting on with others | .79 | .81 | .70 | .46 | ||||||
| 42. | Irritable with others | .83 | .84 | .71 | .52 | ||||||
| 43. | Difficulty doing jobs | .87 | .89 | .77 | .48 | ||||||
| 44. | Health worsened | .80 | .82 | .74 | .37 | ||||||
| 45. | Financial loss | .66 | .68 | .62 | .28 | ||||||
| 46. | Unable to enjoy people's company | .86 | .88 | .81 | .34 | ||||||
| 47. | Life unsatisfying | .82 | .84 | .74 | .43 | ||||||
| 48. | Unable to function | .84 | .86 | .76 | .43 | ||||||
| 49. | Unable to work | .85 | .87 | .75 | .49 | ||||||
|
|
|||||||||||
| Factors | Cronbach's alpha | Correlation between factors | |||||||||
| D1 | .92 | 1 | |||||||||
| D2 | .88 | .84 | 1 | ||||||||
| D3 | .85 | .77 | .78 | 1 | |||||||
| D4 | .95 | .85 | .84 | .75 | 1 | ||||||
Hypothesis 3: OHIP items reflect both a general factor and four dimensions
Our previous findings suggested that both a unidimensional and a four-factor model were plausible models for the latent structure of the OHIP. The chi-square test (χ2(738) = 8458, p < 0.001) rejected a bifactor model that contained a general factor and four domain specific dimensions, though the bifactor model fit significantly better than the four-factor model (χ2(35) = 334). However, the bifactor fit statistics improved only in the third digit over the four-factor model (RMSEA: 0.05, comparative fit indices were >0.99) and the improvement in model fit was accompanied by a large increase in model complexity. Additionally, the results for the bifactor model were more difficult to interpret. Similar to the unidimensional model, loadings on the general factor were large, ranging from 0.48 (sensitive teeth) to 0.86 (diet unsatisfactory, interrupt meals, and been embarrassed) with standard errors comparable to those found with the unidimensional and four-factor models. The bifactor domain loadings on the Function, Pain, and Appearance factors were generally lower than the corresponding loadings in the four-factor model, but still moderately large. Loadings on the Orofacial Pain, Orofacial Appearance, and Psychosocial Impact factors ranged from 0.15 to 0.52 with a median loading of 0.40. The standard errors of these loadings were higher than in the other models, with errors in the range of 0.013 to 0.017. Finally, the loadings on the Oral Function factor did not show a consistent trend. Items 1, 16, 28, 29, and 32 had loadings close to 0 while items 2, 6, 24, 25, and 26 had larger loadings.
Selection of the best model for OHIP
The bifactor model with four dimensions and one general factor provided the best fit among the models tested. However, the bifactor results were challenging to interpret, suggesting that a bifactor structure is overly complex for these data. The four-factor model appeared as the clearest structure of OHIP scores because of good model fit, consistently high domain loadings, and theoretical plausibility.
Discussion
This secondary analysis of international data from prosthodontics patients and general population subjects in six countries confirmed that the latent structure of the Oral Health Impact Profile is well-characterized by both a four-dimensional and a higher-order, general factor model. We named the four correlated latent factors Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact. These dimensions serve as a parsimonious set of dimensions for OHRQoL measured with OHIP. In addition, the functional, painful, and aesthetical effects of oral disorders and their psychosocial distress are strongly correlated, justifying that OHRQoL status can be described sufficiently with one summary score.
We believe that these four dimensions are a set of core features reflecting how individuals perceive oral health. This does not mean that our model could not be extended. For example, previous findings using the Orofacial Aesthetics Scale, which exclusively measures Orofacial Appearance (17, 18), provided preliminary evidence that appearance may have an intra- and an extra-oral component (19). The dimension Oral Function may also have sub-components. Our bifactor analysis suggested that at least two types of Oral Function may exist. Items with high domain loadings seem to reflect Communication and those items with low domain loadings seem to reflect Eating. Certainly, further differentiation of our Psychosocial Impact dimension is already available, as indicated by the existence of instruments measuring depression, anxiety, and similar constructs (20). While the existing OHIP-49 may provide enough information to assess Psychosocial Impact in some settings, it certainly lacks the potential for detailed insight that more specific instruments provide.
The OHIP authors grouped questionnaire items into seven domains based on expert opinion and a conceptual model of oral health (1). Subsequent qualitative studies provided evidence for the multidimensional nature of OHIP scores, but their findings did not agree on the number of dimensions. On one hand, studies of OHIP-14 responses by UK and Australian general population subjects led authors to accept the original seven-dimensional structure (21). On the other hand, experts found that only four dimensions were needed when assigning OHIP items to each of the original seven domains (22).
Quantitative methods such as factor analysis have been used to investigate the structure of the OHIP. Previous EFA studies provided inconsistent solutions (for details, we refer to an article in this issue (3).) Studies have been heterogeneous regarding the populations studied, the instruments (long or short forms) used, and the methods applied. The results have agreed in the rejection of OHIP's initial seven-dimensional structure. They also agreed, except for one study (23), that OHIP is a multifactorial instrument. We believe that our previous EFA result of four factors–the structure that served as the basis for the current CFA–synthesized many of these previous findings (3).
Similar to the considerable number of EFA studies, previous CFA analyses reported varied results. One study used OHIP's seven-domain structure as the hypothesis to be tested (24). Three studies generated a hypothesis with EFA first and then tested the derived structure (23, 25, 26). All four studies rejected the original seven-domain structure. In the first study, using OHIP-49 in older Canadian adults, a six-factor structure was proposed for 22 OHIP items with the following dimensions: Functional Limitations, Pain, Psychological Impact, Physical Disability, Social Disability, and Handicap (24). In a second study, with an 18-item OHIP in middle-aged Japanese workers, a four-dimensional structure was confirmed: Functional Limitation, Physical Pain, Psychological Discomfort, and Disability & Handicap (26). A third study, using two OHRQoL instruments together (14-item OHIP (27) and Oral Impact of Daily Performances questionnaire (28)) in healthy Spanish workers, Functional Limitation, Pain-Discomfort, and Psychosocial Impacts were confirmed (25). Finally, using the 14-item OHIP (27) in two Brazilian samples (postpartum women and older adults), this Spanish three-factor model was tested, found to fit the data, but then rejected in favour of the simpler unidimensional (one-factor) model (23). These four studies agreed with our finding that Function and Pain are essential OHRQoL dimensions. Our Psychosocial Impact dimension is somewhat consistent with these previous results. Whereas two studies separated Psychosocial Impact into two or more dimensions (24, 26), the other two studies did not (23, 25). We also did not differentiate Psychosocial Impact. The four studies did not find Orofacial Appearance as a separate dimension. As we previously discussed (3), conceptual and technical reasons might explain this situation. From a technical point of view, abbreviated instruments such as OHIP-14 are not able to identify this dimension because they do not contain enough indicators of this dimension. From a conceptual point of view, previous investigators stayed within the original seven-dimensional framework which does not have an Appearance dimension. We believe that Orofacial Appearance is so important for individuals - on par with Pain and Function - that this component of perceived oral health deserves a place in the theoretical structure of OHRQoL. Our dimensions Oral Function, Orofacial Pain, and Orofacial Appearance were already measured with other stand-alone instruments, providing evidence for the existence of and the interest in these constructs. For example, the Research Diagnostic Criteria for TMD (29) provided a Jaw Disability List to measure Oral Function. Whereas facial aesthetics has been incorporated into a variety of instruments mainly for adolescents to assess the impact of malocclusion and dentofacial deformity such as a condition-specific QOL measure suggested by Cunningham (30), more recently a specific instrument was developed to measure Orofacial Appearance in adults (17, 18). To characterize Orofacial Pain, instruments such as the Symptom Severity Index (31) have been developed to summarize several aspects of TMJ, jaw and temple muscle pain. Numerous instruments measure the specific aspects of the broader Psychosocial Impact such as depression, anxiety and similar constructs (20).
Strengths and limitations
We used the original long OHIP (1) so that the analysis had many indicators for identification of dimensions. In many clinical and population-based settings, this long instrument is not feasible and shorter OHIPs are applied commonly. Because the abbreviated instruments comprise a subset of the larger item pool, our results are also applicable to these instruments. While this is a strength, our study also has some limitations. When using the EFA as basis for our model, we omitted five items from the analysis because these items did not have salient loadings on one of the four dimensions. However, our previous analysis showed that all 46 items, including the three denture-specific items, describe a general OHRQoL factor (3) The 41 items used in the present analysis provided a clearly interpretable pattern compatible with the full item set. In addition, all our statistical models were appropriate according to several indices describing various aspects of model fit. Some findings need more elaborate follow-up analyses. The headaches item had salient loadings on two factors and items in the Oral Function dimension lost their influence on the dimension in the bifactor model. Refinement of OHRQoL measurement with OHIP is possible in light of our results. Adding items to better measure theoretical domains and omitting other items may lead to better correspondence between theory and measurement. Finally, while prosthodontics patients and general population subjects are populations with a substantial potential to generalize to other populations (2), validation of our OHIP structure findings in specific patient and non-patient populations is needed. When we combined patients and general population subjects in one analysis to achieve greater generalizability of results, we found a strong and consistent solution. We consider this promising evidence that findings may also be generalizable to other patient populations.
Conclusions
Our findings are a contribution to the understanding of OHRQoL in particular and perceived oral health in general. Under the assumption that the 49 OHIP items adequately represent perceived oral health, four correlated aspects of patient-perceived OHRQoL – Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact – exist. These dimensions could serve as a framework to understand and measure the impact of oral conditions and the effect of dental interventions.
Our findings inform use of the OHIP in research and patient care. One OHIP summary score is sufficient to characterize oral health-related quality of life. Because of the high correlations between factors and the small number of indicators for some dimensions, we recommend that one score be used in research and patient care under the current forms of the OHIP. Application of the seven original OHIP domain scores is discouraged in long or abbreviated versions. Use of the original seven-dimensional structure leads to diminished statistical power and, more importantly, claims to measure constructs that are not supported by empirical evidence. In the same vein, OHIP has several condition-specific versions such as OHIP-aesthetic (32) and OHIP-Edent (33); and their use with one summary score is supported by OHIP's strong general factor. However, these abbreviated instruments may be less specific to the target condition, for example, to measures aesthetical problems, than envisioned. The use of many different OHIP versions in general limits comparability of OHRQoL results across studies. Based on our findings, the use of the 14-item OHIP (27) as the most widely used abbreviated version is encouraged (without using dimension scores) when 49 items are not feasible. If 14 items are not feasible, an ultrashort 5-item version (34) is available that contains one item for each of the four dimensions confirmed in this study. The 49, 14, and 5-item OHIP versions will allow an assessment of an individual's overall OHRQoL impairment in almost any setting.
Acknowledgments
Research reported in this publication was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health under Award Number R01DE022331.None of the authors reported any conflict of interest.
References
- 1.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 2.John MT, Reiβmann DR, Feuerstahler L, Waller N, Baba K, Larsson P, et al. Dimensions of Oral Health–Related Quality of Life Project - Overview and studied population. J Prosthodont Res. 2014;1:26–34. doi: 10.1016/j.jpor.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.John MT, Reiβmann DR, Feuerstahler L, Waller N, Baba K, Larsson P, et al. Exploratory factor analysis of the Oral Health Impact Profile. J Oral Rehabil. doi: 10.1111/joor.12192. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szentpetery A, Szabo G, Marada G, Szanto I, John MT. The Hungarian version of the Oral Health Impact Profile. Eur J Oral Sci. 2006;114:197–203. doi: 10.1111/j.1600-0722.2006.00349.x. [DOI] [PubMed] [Google Scholar]
- 5.Petricevic N, Celebic A, Papic M, Rener-Sitar K. The Croatian version of the Oral Health Impact Profile Questionnaire. Coll Antropol. 2009;33:841–847. [PubMed] [Google Scholar]
- 6.John MT, Patrick DL, Slade GD. The German version of the Oral Health Impact Profile--translation and psychometric properties. Eur J Oral Sci. 2002;110:425–433. doi: 10.1034/j.1600-0722.2002.21363.x. [DOI] [PubMed] [Google Scholar]
- 7.Rener-Sitar K, Celebic A, Petricevic N, Papic M, Sapundzhiev D, Kansky A, et al. The Slovenian version of the Oral Health Impact Profile Questionnaire (OHIP-SVN): translation and psychometric properties. Coll Antropol. 2009;33:1177–1183. [PubMed] [Google Scholar]
- 8.Larsson P, List T, Lundstrom I, Marcusson A, Ohrbach R. Reliability and validity of a Swedish version of the Oral Health Impact Profile (OHIP-S) Acta Odontol Scand. 2004;62:147–152. doi: 10.1080/00016350410001496. [DOI] [PubMed] [Google Scholar]
- 9.Yamazaki M, Inukai M, Baba K, John MT. Japanese version of the Oral Health Impact Profile (OHIP-J) J Oral Rehabil. 2007;34:159–168. doi: 10.1111/j.1365-2842.2006.01693.x. [DOI] [PubMed] [Google Scholar]
- 10.John MT, LeResche L, Koepsell TD, Hujoel PP, Miglioretti DL, Micheelis W. Oral health-related quality of life in Germany. Eur J Oral Sci. 2003;111:483–491. doi: 10.1111/j.0909-8836.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 11.Holzinger KJ, Swineford F. The bi-factor method. Psychometrika. 1937;2:41–54. [Google Scholar]
- 12.Reise SP. The rediscovery of bifactor measurement model. Multivariate Behav Res. 2012;47:667–696. doi: 10.1080/00273171.2012.715555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 14.Christoffersson A. Two-Step Weighted Least Squares Factor Analysis of Dichotomized Variables. Psychometrika. 1977;3:433–438. [Google Scholar]
- 15.A Core Team. R: A Language and Environment for Statistical Computing. 2013;2013 [Google Scholar]
- 16.lavaan Rosseel Y. An R Package for Structural Equation Modeling. J Stat Softw. 2012;48:1–36. [Google Scholar]
- 17.Larsson P, John MT, Nilner K, List T. Reliability and validity of the Orofacial Esthetic Scale in prosthodontic patients. Int J Prosthodont. 2010;23:257–262. [PubMed] [Google Scholar]
- 18.Larsson P, John MT, Nilner K, Bondemark L, List T. Development of an Orofacial Esthetic Scale in prosthodontic patients. Int J Prosthodont. 2010;23:249–256. [PubMed] [Google Scholar]
- 19.John MT, Larsson P, Nilner K, Bandyopadhyay D, List T. Validation of the Orofacial Esthetic Scale in the general population. Health Qual Life Outcomes. 2012;10:135. doi: 10.1186/1477-7525-10-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.PROMIS. Patient Reported Outcomes Measurement Information System. 2013;2013 [Google Scholar]
- 21.Nuttall NM, Slade GD, Sanders AE, Steele JG, Allen PF, Lahti S. An empirically derived population-response model of the short form of the Oral Health Impact Profile. Community Dent Oral Epidemiol. 2006;34:18–24. doi: 10.1111/j.1600-0528.2006.00262.x. [DOI] [PubMed] [Google Scholar]
- 22.John MT. Exploring dimensions of oral health-related quality of life using experts' opinions. Qual Life Res. 2007;16:697–704. doi: 10.1007/s11136-006-9150-8. [DOI] [PubMed] [Google Scholar]
- 23.dos Santos CM, de Oliveira BH, Nadanovsky P, Hilgert JB, Celeste RK, Hugo FN. The Oral Health Impact Profile-14: a unidimensional scale? Cad Saude Publica. 2013;29:749–757. doi: 10.1590/s0102-311x2013000800012. [DOI] [PubMed] [Google Scholar]
- 24.Baker SR, Gibson B, Locker D. Is the oral health impact profile measuring up? Investigating the scale's construct validity using structural equation modelling. Community Dent Oral Epidemiol. 2008;36:532–541. doi: 10.1111/j.1600-0528.2008.00440.x. [DOI] [PubMed] [Google Scholar]
- 25.Montero J, Bravo M, Vicente MP, Galindo MP, Lopez JF, Albaladejo A. Dimensional structure of the oral health-related quality of life in healthy Spanish workers. Health Qual Life Outcomes. 2010;8:24. doi: 10.1186/1477-7525-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ide R, Mizoue T, Yamamoto R, Tsuneoka M. Development of a shortened Japanese version of the Oral Health Impact Profile (OHIP) for young and middle-aged adults. Community Dent Health. 2008;25:38–43. [PubMed] [Google Scholar]
- 27.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 28.Adulyanon S, Sheiham A. A new socio-dental indicator of oral impacts on daily performances. J Dent Res. 1996;75:231. abstract. [Google Scholar]
- 29.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 30.Cunningham SJ, Garratt AM, Hunt NP. Development of a condition-specific quality of life measure for patients with dentofacial deformity: I. Reliability of the instrument. Community Dent Oral Epidemiol. 2000;28:195–201. doi: 10.1034/j.1600-0528.2000.280305.x. [DOI] [PubMed] [Google Scholar]
- 31.Fricton JR. Musculoskeletal measures of orofacial pain. Anesth Prog. 1990;37:136–143. [PMC free article] [PubMed] [Google Scholar]
- 32.Wong AH, Cheung CS, McGrath C. Developing a short form of Oral Health Impact Profile (OHIP) for dental aesthetics: OHIP-aesthetic. Community Dent Oral Epidemiol. 2007;35:64–72. doi: 10.1111/j.1600-0528.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 33.Allen F, Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont. 2002;15:446–450. [PubMed] [Google Scholar]
- 34.John MT, Miglioretti DL, LeResche L, Koepsell TD, Hujoel P, Micheelis W. German short forms of the Oral Health Impact Profile. Community Dent Oral Epidemiol. 2006;34:277–288. doi: 10.1111/j.1600-0528.2006.00279.x. [DOI] [PubMed] [Google Scholar]