Abstract
OBJECTIVE
To determine if self-reported anxiety levels decreased after tracheostomy placement in a sample of mechanically ventilated intensive care unit patients.
BACKGROUND
There is limited research regarding the impact of a tracheostomy on patients’ anxiety. Elevated anxiety delays healing and contributes to long-term mental health complications.
METHODS
This was a secondary analysis of data from a large clinical trial conducted in urban Minnesota. Fifty-one of 116 patients received a tracheostomy. Anxiety scores were obtained daily using the Visual Analog Scale-Anxiety. Mixed model analysis was used to compare anxiety ratings pre- and post-tracheostomy.
RESULTS
There was no significant decrease in anxiety following tracheostomy after controlling for time and gender (all p>.16). Age was the only variable to impact anxiety levels: anxiety scores increased as age increased (p=.02).
CONCLUSIONS
Prospective studies are needed to more accurately assess the impact of tracheostomy placement on patient anxiety and salient outcomes.
Keywords: Tracheostomy, Anxiety, Mechanical Ventilation, Intensive Care Unit, Adult
INTRODUCTION
Mechanically ventilated adult intensive care unit (ICU) patients frequently undergo tracheostomy placement when they have difficulty weaning from the ventilator or they require long-term ventilator support.1,2 Although disagreement regarding the timing and specific benefits of the procedure continues to dominate research on tracheostomy placement,1–11 commonly accepted advantages include reduced oral, laryngeal, and tracheal damage,3–4 improved work of breathing,12 faster weaning,1,3–5,13 reduced sedation needs,6,14 decreased morbidity and mortality rates,1–4,15 shorter hospital and ICU stays,1,4–5 and lower costs.5
The physical and psychological discomforts of mechanical ventilation (MV) via an endotracheal tube have been well documented.16–26 Tracheostomy placement in mechanically ventilated patients is presumed to mitigate these discomforts by allowing for oral nutrition,6 increased mobility,14 and verbal communication.27 However, patients continue to report physical and psychological distress after tracheostomy placement. In addition to pain,28–29 fatigue,28,30 frequent coughing,28 and thirst,31 patients describe anxiety related to feelings of powerlessness,30 fear,32 uncertainty about the future,28–31 impaired communication,28–29,31,33 and altered body image.28,34
Anxiety is defined by Johnson and Sexton20 as a state marked by prolonged apprehension, increased motor tension or activity, and autonomic arousal. Bay35 further describes anxiety as a “perceived mismatch”35 and the resultant “feeling of dread or impending doom”35 that leads to hyperawareness and physiologic responses. Anxiety is one of the most commonly reported and most distressing symptoms associated with MV,21,23,32,36–40 including those patients who receive MV via a tracheostomy.30 Prolonged anxiety delays healing and predisposes patients to difficult weaning.20,33 Additionally, prolonged anxiety has been shown in multiple studies to contribute to long-term depression and post-traumatic stress disorder (PTSD) in patients who have survived their critical illness.6,18,24,33,41–43
Background
Despite anxiety’s ill effects on healing, there is a noteworthy deficiency of research on patients’ self-reported anxiety levels in the ICU following tracheostomy placement. The OVID Medline, PubMed, PsychInfo, and CINAHL databases were used to conduct the literature review for this analysis, and the located articles were cross-referenced. No identified quantitative studies specifically evaluated anxiety post-tracheostomy as a study aim Several researchers have assessed the broader category of patient comfort;6,13,14 however, comfort includes but is not limited to anxiety.32 Furthermore, measures and conclusions about patient comfort and anxiety rely almost exclusively on proxy indicators, such as decreased sedation needs6,14,27 and nurse or family member assessments,7,14,27 rather than first-person patient reports.
Proxy assessments of patient symptoms are problematic because research in a number of settings has revealed that care providers and family members tend to incorrectly estimate patients’ symptoms.17,32,44–46 Symptoms, in general, are more frequently underestimated than overestimated by proxy assessors.47–49 Anxiety, specifically, is both under-45,50 and overestimated,48,50 making self-reported evaluation of this common symptom in mechanically ventilated patients essential for effective management.
The purpose of this secondary analysis was to begin to fill the knowledge gap about patient anxiety post-tracheostomy placement. The primary aim was to determine if self-reported anxiety levels decreased after tracheostomy placement in a sample of ICU patients receiving mechanical ventilatory support. Secondary aims were to evaluate anxiety in patients with and without a tracheostomy with regard to such potential covariates as age, gender, race, ethnicity, and receipt of sedative medications.
METHODS
Design
This study was a secondary analysis of existing data from a large parent study. The aim of the parent study was to determine the effects of patient-initiated music listening on anxiety levels and sedative exposure in critically ill patients receiving mechanical ventilatory support. Subjects remained on protocol as long as they were receiving mechanical ventilation in the ICU, from 1 to 30 days per protocol. Findings for the parent study are reported elsewhere.51 Subjects who were randomized to the usual care group in the parent clinical trial were used as the sample group for this secondary analysis.
Setting and Sample
This study was conducted in the Minneapolis and St. Paul, Minnesota urban area. Subjects were recruited from 12 ICUs between September 2006 and March 2011. Approval was obtained from the principal investigator’s Institutional Review Board (IRB), as well as the IRBs of all of the participating hospitals. Patients were required to provide their own informed consent due to the patient-directed nature of the intervention in the parent study. Trained research nurses obtained consent from all enrolled patients.
Inclusion criteria for the parent study consisted of mechanically ventilated patients in the participating ICUs who were age 18 or older, alert and participating in their care, able to read and write in English, had adequate corrected hearing and vision as determined by bedside ICU nurses’ assessment, were hemodynamically stable and not requiring active titration of vasopressor medications, and who were receiving ventilatory support for a pulmonary issue. Exclusion criteria included aggressive ventilatory support, hemodynamic instability, unresponsiveness, deafness or blindness without signing ability, or patients with documentation in the medical record that indicated they were not mentally capable of providing their own informed consent (i.e., Alzheimer’s disease).
A total of 125 patients from the participating ICUs were randomized to the usual care group in the parent study. Patients’ diagnoses were primarily respiratory or cardiac (Table 1). Anxiety data were obtained from 116 of these patients; they comprise the sample for the study reported here. A sample of 116 subjects would be able to detect a difference of 13% in the VAS-A scores after tracheostomy placement, with power of 80% and alpha set at .05.
TABLE 1.
Admitting medical diagnoses and primary indication for tracheostomy
| Diagnostic Category (n=116) |
N(Valid %) |
|---|---|
| Pulmonary | 68(59%) |
| Cardiac | 16(14%) |
| Gastrointestinal | 9(8%) |
| Neurological & Neuromuscular | 5(4%) |
| Oncology | 4(3%) |
| Sepsis/Infection | 6(5%) |
| Other1 | 8(7%) |
| Primary Indications for Tracheostomy2 (n=22) | n(%) |
| Respiratory failure | 24(21%) |
| Pneumonia | 3(3%) |
| Respiratory arrest | 2(2%) |
| Respiratory distress/shortness of breath/dyspnea | 27(23%) |
| Airway protection | 5(4%) |
| Tachypnea | 3(3%) |
“Other” includes shock/hypotension, surgery (non-cardiac), trauma, and vascular
Up to three indications given
Demographic and clinical variables are compared between patients who received a tracheostomy and those who did not in Table 2. Indications for tracheostomy placement were available for only 22 patients; all indications were respiratory (Table 1). There were no established standards for time to tracheostomy placement in any of the participating ICUs.
TABLE 2.
Comparison of demographic and clinical characteristics of patients with and without tracheostomy
| Variable | No Tracheostomy (n = 65) |
Tracheostomy (n = 51) |
||
|---|---|---|---|---|
| Mean(SD) | Mean (SD) | p-value | ||
| Age | 58.1(11.9) | 56.0(14.1) | .39 | |
| APACHE III | 64.9(22.7) | 65.6(24.5) | .86 | |
| VAS-A at entry to study | 53.4(29.6) | 51.7(30.1) | .75 | |
| N(%) | N(%) | p-value | ||
| Male | 27(42) | 25(49) | .42 | |
| Hispanic1 | 1(2) | 2(4) | .58 | |
| Race: | .64 | |||
| White | 58(89) | 43(84) | ||
| American Indian | 1(2) | 2(4) | ||
| Black | 6(9) | 6(12) | ||
| Median(range) | Median(range) | p-value | ||
| ICU days at admission to study | 4.5(.3–18.5) | 13.4(1.5–34) | <.001 | |
| Total days in ICU | 10.0(2–52) | 26(4–62) | <.001 | |
| Days in study | 2.0(.01–24) | 8.1(1.2–30) | <.001 | |
| Days on ventilator at admission to study | 3.5(.3–38) | 11.8(1.6–33) | <.001 | |
| Total hours on ventilator | 154.4(29–939) | 457.8(205–1105) | <.001 | |
Fisher’s exact test
Variables and Their Measurement
Anxiety
Anxiety can be defined as a state marked by apprehension, agitation, increased motor activity, arousal, and fearful withdrawal.21 The VAS-A was used in this study to measure patients’ anxiety each day. Each day during study enrollment, at around the same assessment time each day, patients were asked to mark their current level of anxiety on the VAS-A using a large, black, felt-tipped marker. They were instructed to rate their level of anxiety in response to the question, “How are you feeling right now?” Patients were assisted by research nurses as needed to mark their current level of anxiety. The VAS-A was anchored on each end by the statements “not anxious at all” (0 mm) and “the most anxious I have ever been” (100 mm). A VAS-A score of 50 mm was considered to represent a moderate anxiety level.52 Scores were derived by measuring the distance in millimeters from the bottom edge of the line anchor to the mark placed by the participant. The same ruler was used to score all completed VAS-A measures.
The VAS-A had a vertical orientation, which is thought to be more sensitive and easier for subjects to use. It is considered to be particularly useful for those patients with a narrowed visual field or patients who are under stress.53–54 Visual Analog Scales (VAS) are appropriate for tracking a subject's clinical course, are easily administered, are easy for subjects to see, and use few words to minimize the possibility of different interpretations.54–55 Careful instruction and repeated use of a VAS can eliminate problems with conceptual understanding of the method.55 Mechanically ventilated subjects have not reported difficulty completing the VAS-A in other studies38 or in the parent study.51 The VAS-A has been used by investigators to measure anxiety in patients receiving MV,53 and to measure changes in anxiety in ventilated patients undergoing weaning trials.56
The VAS-A and the Spielberger State Anxiety Inventory (SAI) have been found to be correlated r = 0.4938 to .82,57 demonstrating concurrent validity. Measures of reliability, such as test-retest, are usually not addressed with VAS scales due to the dynamic nature of the phenomenon being measured.55,58 The VAS-A has been found to be an accurate and sensitive measure of state anxiety, capable of producing reliable measures of anxiety in ventilated patients undergoing weaning trials56 and ambulatory surgical procedures.57
Time to Tracheostomy
Time to tracheostomy was defined as the amount of time in days that had elapsed between a patient’s initial intubation in the ICU and the day that the tracheostomy tube was placed. Attending physicians in each ICU determined patients’ need for and the timing of tracheostomy. Time to tracheostomy was not standardized in this study because it was not an aim of the parent study.
Sedation
Given the potential influence of sedative medications on anxiety, receipt of these medications was recorded from each patient’s medical record. Sedation was operationalized for this study as any receipt of commonly administered medications to ICU patients pre-and post-tracheostomy placement, coded “Yes/No” for data analysis. Sedative medications included the following drugs: propofol, dexmedetomidine, diazepam, lorazepam, midazolam, haloperidol, fentanyl, morphine and hydromorphone. For example, “pre-tracheostomy sedation” meant that a patient received any sedative medication on any day prior to tracheostomy; “post-tracheostomy sedation” meant that a patient received any sedative medication after tracheostomy placement.
Data Analysis
Descriptive statistics were generated using frequencies and percentages for categorical data. Interval data were described using means and standard deviations for normally distributed data; medians and ranges were used for non-normally distributed data. Preliminary assessments of differences in interval data, such as pre-tracheostomy VAS-A scores and other covariates of interest, were generated using a t-test for 2 groups. The screening of categorical variables as possible covariates used a chi-square test of association between the tracheostomy and non-tracheostomy groups. Percentages of subjects in the tracheostomy group who received sedation pre- and post-procedure were compared bivariately using a McNemar’s test for related samples.
Available daily VAS-A scores from the patients who did and did not receive a tracheostomy were compared pre- and post-tracheostomy placement using a mixed model analysis with Statistical Analysis Software (SAS), version 9.2, proc mixed. Mixed models were chosen because they handle missing data well. Using the unaltered data within a mixed model analysis has a lower type I error and a higher power than any type of imputation method used for missing data. In addition, imputation may result in biased estimates of effects and standard errors. In this study, missing data was due to differing lengths of follow-up time, patient illness, and activity or procedure time conflict at the time VAS-A scores were collected on a particular day. In the mixed model, tracheostomy placement was treated as a time dependent covariate, which controlled for the differing times of tracheostomy placement after study enrollment. Baseline anxiety was also included as a covariate, in order to control for the range of initial anxiety levels. The covariance structure chosen was auto-regressive, based on the correlation matrix of VAS-A values day to day. All results were considered significant at p < .05.
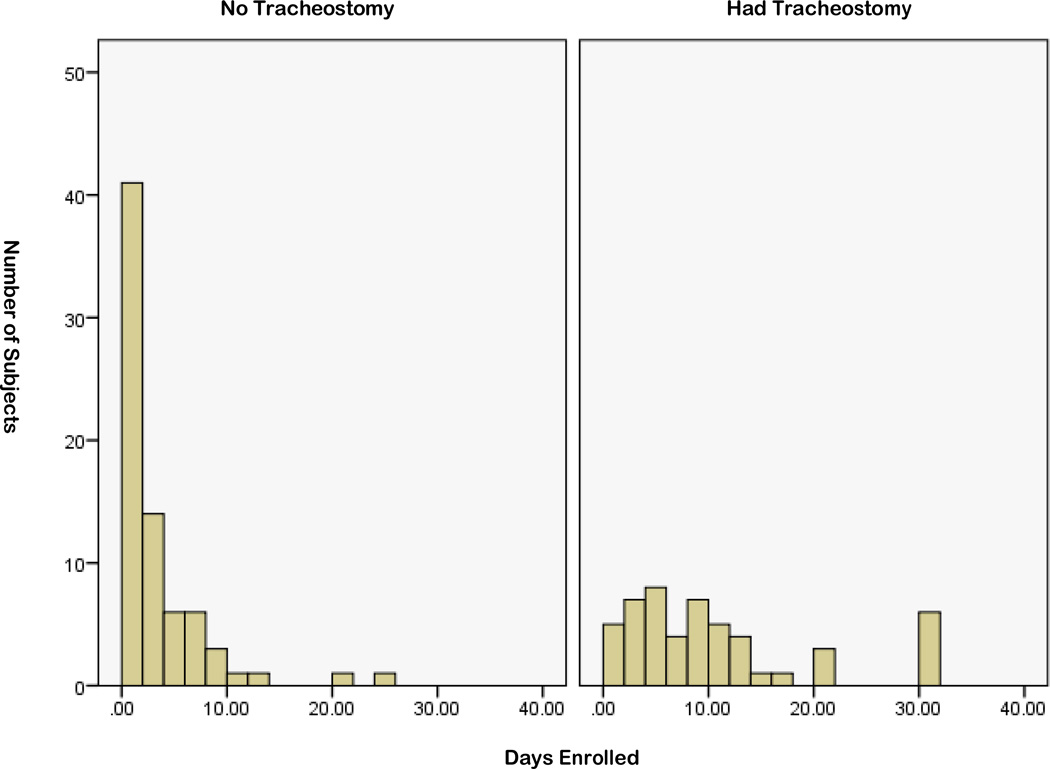
RESULTS
Of the patients randomized to the parent study’s usual care group and used in this study (n = 116), 6 remained in the study until the 30 day limit. Of the overall 116 patients, 77 were extubated. Of the 110 patients who were enrolled in the study for fewer than 30 days, 12 died and 4 withdrew from the study. For these reasons, the amount of VAS-A data collected decreased over time (Figure 1).
FIGURE 1.
Number of enrolled subjects by study day (non-cumulative)
Fifty-one of the 116 patients in this sample underwent tracheostomy placement at some point during their enrollment in the parent study. There were no significant differences in age, gender, race, ethnicity, or Acute Physiology, Age, Chronic Health Evaluation (APACHE) III scores between patients who underwent tracheostomy placement and those who did not (Table 2). At the time of study entry, mean VAS-A scores did not significantly differ between patients who eventually received a tracheostomy and those who did not (Table 2). However, mean VAS-A scores for the total time spent in the study were significantly higher for male patients who did not receive a tracheostomy as compared to those who did (p = .03) (Table 3).
TABLE 3.
Mean1 Visual Analog Scale-Anxiety (VAS-A) Scores by Sex, Ethnicity, and Race
| Variable | No Tracheostomy (n=65) Mean (95% CI) |
Tracheostomy (n=51) Mean (95% CI) |
p-value | |
|---|---|---|---|---|
| Sex | ||||
| Male | 60.0(49.4, 70.6) | 45.7(35.9, 55.5) | .047 | |
| Female | 46.3(38.8, 53.8) | 55.4(48.1, 62.8) | .10 | |
| Ethnicity | ||||
| Non-Hispanic | 51.8(45.4, 58.2) | 50.4(44.1, 56.6) | .76 | |
| Hispanic | 66.0 (only 1) | 57.5(29.2, 91.5) | .75 | |
| Race | ||||
| White | 53.1(46.3, 60.0) | 50.1(43.9, 56.4) | .53 | |
| American Indian | 72(only 1) | 41.6(−25.4, 128.8) | .62 | |
| African American | 38.1(21.9, 54.3) | 57.6(27.4, 87.8) | .18 | |
VAS-A scores were meaned for each subject over the total time he or she participated in the study
Results of the mixed model analysis show that, following tracheostomy placement, patients’ anxiety levels did not significantly decrease due to tracheostomy placement, gender of the patient, time in study, or time by tracheostomy interaction (all p > .16). Age was the only variable to impact VAS-A levels over time, independent of whether or not a patient had a tracheostomy placed (p = .02) (Table 4); for every year older a subject was, his or her VAS-A scores increased by one half of a point.
TABLE 4.
Mixed model analysis of the impact of tracheostomy placement on anxiety*
| β(se(β)) | p-value | |
|---|---|---|
| Day in study | .11(1.7) | .95 |
| Age | .50(.21) | .02 |
| Male | 9.1(6.4) | .16 |
| Has tracheostomy | −4.8(5.1) | .36 |
| Tracheostomy by day interaction | −.82(1.6) | .62 |
There is no significant effect of time (day) or having a tracheotomy on the VAS-A
Twenty-nine (97%) of the 30 patients who received sedative medication prior to tracheostomy placement continued to receive sedative medication post tracheostomy. Sixteen (76%) of the 21 patients who did not receive any sedative medication prior to tracheostomy placement received a sedative medication post-tracheostomy, which was significant (p = <.001).
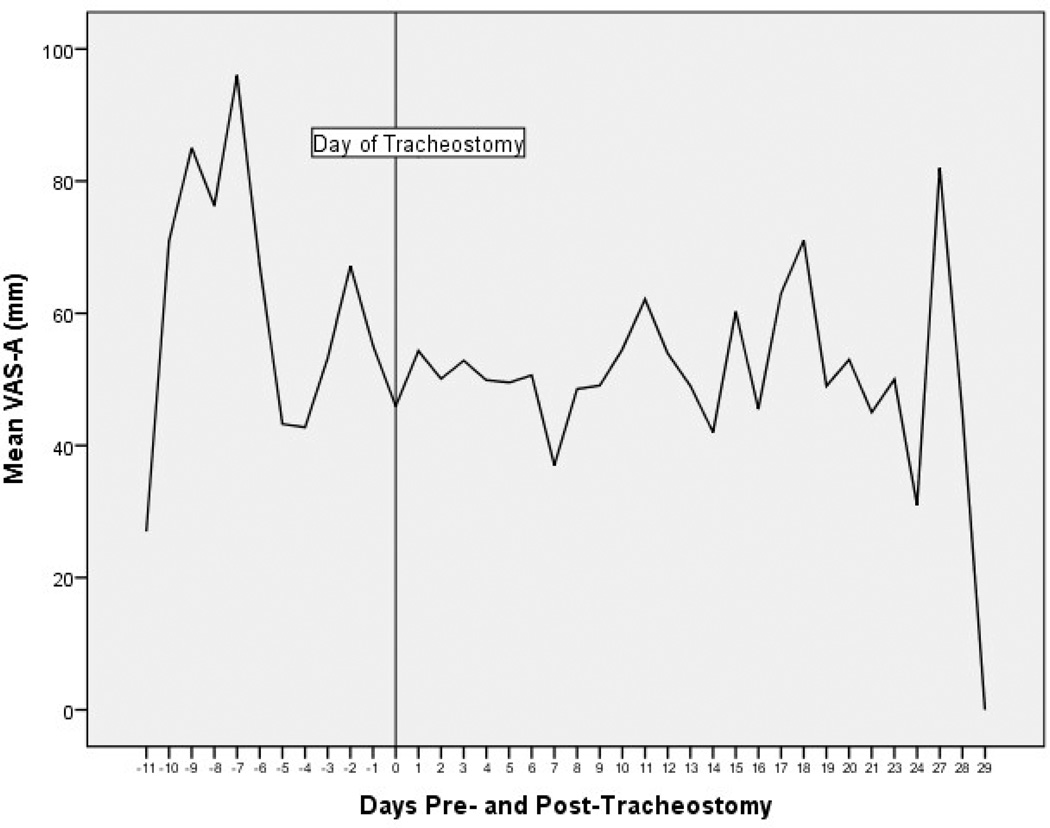
In this study, anxiety did not significantly decline for the sample group following tracheostomy placement. However, daily mean anxiety scores were noted to be quite variable in patients who received a tracheostomy (Figure 2). In Figure 2, Day 0 signifies the day of tracheostomy placement; time is adjusted in reference to Day 0. Negative numbers represent the days leading up to tracheostomy placement, and positive numbers indicate the days following the procedure. Centering time around tracheostomy placement was done to accommodate patients’ varying times of study enrollment and tracheostomy placement.
FIGURE 2.
Mean anxiety trends before and after tracheostomy placement (n=51)
DISCUSSION
The main finding from this secondary analysis was that patients’ self-reported anxiety ratings, as measured by the VAS-A, did not decline after tracheostomy placement. This result contrasts with the conclusion of Blot et al,13 who tentatively reported that patient comfort increased following the procedure. However, comfort is a broad term that may include, but differs from, anxiety.32,35
A related finding to the main finding was that receipt of a sedative medication increased after tracheostomy placement. This result is corroborated by the research of Blot et al,13 as well as Veelo et al,59 but it contradicts the findings of Trouillet et al6 and Nieszkowska et al.14 The basis for the finding of increased sedation after tracheostomy is not known; further study is required to determine the clinical reasoning behind this change.
The finding that anxiety did not significantly decrease following tracheostomy placement is particularly relevant in light of several recent studies that reported limited or no improvement in patients’ physiological parameters after the procedure, including morbidity, mortality, weaning, and length of ICU or hospital stay.1,8,13 Furthermore, the lack of a significant decrease in patient anxiety following tracheostomy placement, compounded with the finding of an increased number of patients receiving a sedative medication post-tracheostomy, contradicts the general supposition by clinicians of improved patient comfort after the procedure. These findings support the conclusion reached by Sherlock et al: “Tracheostomy is potentially much more psychologically and physically traumatic for patients than clinicians may be aware of.”31
Although overall anxiety did not decline in this sample following tracheostomy placement, a secondary finding in this study was that VAS-A scores fluctuated widely day to day before and after the procedure (Figure 2). The daily variability noted in patient anxiety is consistent with similar fluctuation, a wide range in VAS-A scores, and no discernable patterns in anxiety ratings noted in previous studies.37,52 Tate et al32 attributed patients’ differing psychological responses to being mechanically ventilated to multifactorial influences, such as individual personality characteristics and health history. Continued fluctuations in the level of anxiety post-tracheostomy placement may also be related to patients’ clinical conditions and their on-going need to receive MV in the ICU.22 In previous studies, patients reported higher anxiety with longer periods of MV (4–7 days versus >7 days33; 6–21 days versus >22 days37). Tate et al32 proposed that patient anxiety may increase with time because patients “anticipated discomfort based on memories of prior encounters.”32
Furthermore, chronically elevated anxiety may be related to inadequate management of this common symptom.23 Researchers in previous studies have indicated that clinicians can and should do more to alleviate patients’ anxiety. For example, several studies have noted that patients felt that they received less assistance, attention, explanation about procedures, or support from nurses than they desired.17–19, 26,30 Inability to communicate continues to be cited as one of the most aggravating effects of MV,16,18,22–23,28,30 in spite of a great deal of research on how nurses and other care providers can facilitate communication and empower patients.
Study Limitations
This study was limited in a number of ways. It was a secondary data analysis, so a number of variables were affected by the parameters and the available data of the parent study. Enrolled patients had conditions that were expected to improve, a quality influenced by the parent study’s requirement for patients’ consent to participate. In some cases, patients were stable enough to transfer from the ICU to long-term acute care units (LTAC), but they were not transferred because of the limited number of LTAC beds in the urban area in which the study occurred. Results may differ in patients with higher APACHE III scores.
Indications for and time to tracheostomy placement were not standardized for any of the participating ICUs, since tracheostomy placement was not part of the parent study’s aims. Neither were the timings and dosages of sedative medications specifically controlled, since they were administered per usual care in each of the participating ICUs.
The number of VAS-A scores obtained per day varied. Some VAS-A scores are missing because patients were not always able, due to illness, activity, or procedure time conflict, to report their anxiety level at the designated time. Furthermore, the amount of data collected each day varied since many patients withdrew or were discharged from the study prior to the 30 day limit. Data were collected in this manner in order to reflect the normal follow-up of mechanically ventilated ICU patients, per the parameters of the parent study. These factors were controlled for in the data analysis, but a complete data set is always ideal.
Recommendations for Further Research
Further study is needed to more accurately assess the impact of tracheostomy placement on patients’ anxiety, salient outcomes, and quality of life from the patient’s perspective. Tracheostomy placement’s impact on anxiety should be the primary aim of future study. Researchers should utilize first-person patient symptom assessments, and data should be collected while patients are still in the ICU. In addition, locating future studies in geographically disparate ICUs will result in more generalizable results.
Recommendations for Clinical Practice
Sustained anxiety requires continual nursing management to promote patients’ physical and psychological health. The new ICU pain, agitation, and delirium (ICU PAD) guidelines address the importance of regular symptom assessment and emphasize evaluating patients’ self-reported symptom experiences rather than using secondary indicators.60 Many of the ICU PAD recommendations can be applied to anxiety assessment and management as well. Namely, patients’ self-reported anxiety should be regularly assessed whenever possible, utilizing valid and reliable instruments that are not burdensome for patients. Clinicians cannot assume they are the best judges of the presence and intensity of unpleasant symptoms such as anxiety. They also should not assume that distressing symptoms such as anxiety are diminished after tracheostomy placement. Clinicians are encouraged to utilize evidence-based interventions, such as communication techniques, supportive measures, anticipatory care, and complementary therapies, in order to help alleviate patients’ anxiety before and after tracheostomy placement.
ACKNOWLEDGMENTS
The parent study was supported by grant #R01-NR009295, L. Chlan, Principal Investigator. We would like to thank the healthcare providers and patients for their participation.
ABBREVIATIONS LIST
- ANOVA
Analysis of Variance
- APACHE III
Acute Physiology, Age, Chronic Health Evaluation; range 0–299
- ICU
Intensive Care Unit
- ICU PAD
Intensive Care Unit Pain, Agitation, and Delirium
- IRB
Institutional Review Board
- LTAC
Long-term Acute Care
- MV
Mechanical Ventilation
- PTSD
Post-traumatic Stress Disorder
- SAI
Spielberger State Anxiety Inventory
- SAS
Statistical Analysis Software
- SD
Standard Deviation
- VAS
Visual Analog Scale
- VAS-A
Visual Analog Scale-Anxiety
Footnotes
CONFLICT OF INTEREST
The authors report no conflicts of interest.
Contributor Information
Stephanie J. Breckenridge, Allina Health Staff RN, University of Minnesota Research Assistant, 1180 California Drive Apt 101, St. Paul, MN 55108, burg0417@umn.edu, 406-249-7056.
Linda Chlan, Distinguished Professor of Symptom Management Research, College of Nursing, Ohio State University, 398 Newton Hall, 1585 Neil Avenue, Columbus, OH 43210, chlan.1@osu.edu, 614-6292-8341.
Kay Savik, Statistician School of Nursing University of Minnesota, 5-140 Weaver-Densford Hall, 308 Harvard Street SE, Minneapolis, MN 55455, savik001@umn.edu, 612-624-2359.
REFERENCES
- 1.Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330(7502):1243. doi: 10.1136/bmj.38467.485671.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frutos-Vivar F, Esteban A, Apezteguia C, et al. Outcome of mechanically ventilated patients who require a tracheostomy. Crit Care Med. 2005;33(2):290–298. doi: 10.1097/01.ccm.0000150026.85210.13. [DOI] [PubMed] [Google Scholar]
- 3.Boynton JH, Hawkins K, Eastridge BJ, O'Keefe GE. Tracheostomy timing and the duration of weaning in patients with acute respiratory failure. Crit Care. 2004;8(4):R261–R267. doi: 10.1186/cc2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rumbak MJ, Newton M, Truncale T, Schwartz S, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004;32(8):1689–1694. doi: 10.1097/01.ccm.0000134835.05161.b6. [DOI] [PubMed] [Google Scholar]
- 5.Arabi YM, Alhashemi JA, Tamim HM, et al. The impact of time to tracheostomy on mechanical ventilation duration, length of stay, and mortality in intensive care unit patients. J Crit Care. 2009;24(3):435–440. doi: 10.1016/j.jcrc.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Trouillet JL, Luyt CE, Guiguet M, et al. Early percutaneous tracheotomy versus prolonged intubation of mechanically ventilated patients after cardiac surgery: A randomized trial. Ann Inter Med. 2011;154(6):373–383. doi: 10.7326/0003-4819-154-6-201103150-00002. [DOI] [PubMed] [Google Scholar]
- 7.Saffle JR, Morris SE, Edelman L. Early tracheostomy does not improve outcome in burn patients. J Burn Care Rehabil. 2002;23(6):431–438. doi: 10.1097/00004630-200211000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Wang F, Wu Y, Bo L, et al. The timing of tracheotomy in critically ill patients undergoing mechanical ventilation: A systematic review and meta-analysis of randomized controlled trials. Chest. 2011;140(6):1456–1465. doi: 10.1378/chest.11-2024. [DOI] [PubMed] [Google Scholar]
- 9.Barquist ES, Amortegui J, Hallal A, et al. Tracheostomy in ventilator dependent trauma patients: a prospective, randomized intention-to-treat study. J Trauma. 2006;60(1):91–97. doi: 10.1097/01.ta.0000196743.37261.3f. [DOI] [PubMed] [Google Scholar]
- 10.Terragni PP, Antonelli M, Fumagalli R, et al. Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA. 2012;303(15):1483–1489. doi: 10.1001/jama.2010.447. [DOI] [PubMed] [Google Scholar]
- 11.Clec’h C, Alberti C, Vincent F, et al. Tracheostomy does not improve the outcome of patients requiring prolonged mechanical ventilation: a propensity analysis. Crit Care Med. 2007;35(1):132–138. doi: 10.1097/01.CCM.0000251134.96055.A6. [DOI] [PubMed] [Google Scholar]
- 12.Diehl JL, El Atrous S, Touchard D, Lemaire F, Brochard L. Changes in the work of breathing induced by tracheotomy in ventilator-dependent patients. Am J Respir Crit Care Med. 1999;159(2):383–388. doi: 10.1164/ajrccm.159.2.9707046. [DOI] [PubMed] [Google Scholar]
- 13.Blot F, Similowski T, Trouillet JL, et al. Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med. 2008;34(10):1779–1787. doi: 10.1007/s00134-008-1195-4. [DOI] [PubMed] [Google Scholar]
- 14.Nieszkowska A, Combes A, Luyt CE, et al. Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med. 2005;33(11):2527–2533. doi: 10.1097/01.ccm.0000186898.58709.aa. [DOI] [PubMed] [Google Scholar]
- 15.Combes A, Luyt CE, Nieszkowska A, Trouillet JL, Gibert C, Chastre J. Is tracheostomy associated with better outcomes for patients requiring long-term mechanical ventilation? Crit Care Med. 2007;35(3):802–807. doi: 10.1097/01.CCM.0000256721.60517.B1. [DOI] [PubMed] [Google Scholar]
- 16.Arslanian-Engoren C, Scott L. The lived experience of survivors of prolonged mechanical ventilation: A phenomenological study. Heart Lung. 2003;32(5):328–334. doi: 10.1016/s0147-9563(03)00043-8. [DOI] [PubMed] [Google Scholar]
- 17.Hall-Lord ML, Larsson G, Steen B. Pain and distress among elderly intensive care unit patients: Comparison of patients’ experiences and nurses’ assessments. Heart Lung. 1998;27(2):123–132. doi: 10.1016/s0147-9563(98)90020-6. [DOI] [PubMed] [Google Scholar]
- 18.Hofhuis JGM, Spronk PE, Van Stel HF, Schrijvers AJP, Rommes JH, Bakker J. Experiences of critically ill patients in the ICU. Intensive Crit Care Nurs. 2008;24:300–313. doi: 10.1016/j.iccn.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Johnson P, St. John W, Moyle W. Long-term mechanical ventilation in a critical care unit: Existing in an uneveryday world. J Adv Nurs. 2006;53(3):551–558. doi: 10.1111/j.1365-2648.2006.03757.x. [DOI] [PubMed] [Google Scholar]
- 20.Johnson MM, Sexton DL. Distress during mechanical ventilation: Patients’ perceptions. Crit Care Nurs. 1990;10(7):48–57. [PubMed] [Google Scholar]
- 21.McCartney JR, Boland RJ. Anxiety and delirium in the intensive care unit. Crit Care Clin. 1994;10(4):937–955. [PubMed] [Google Scholar]
- 22.Menzel LK. Factors related to the emotional responses of intubated patients to being unable to speak. Heart Lung. 1998;27(4):245–252. doi: 10.1016/s0147-9563(98)90036-x. [DOI] [PubMed] [Google Scholar]
- 23.Rotondi AJ, Chelluri L, Sirio C, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):745–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Shaw RJ, Harvey JE, Bernard B, Gunary R, Tiley M, Steiner H. Comparison of short-term psychological outcomes of respiratory failure treated by either invasive or non-invasive ventilation. Psychosomatics. 2009;50(6):586–591. doi: 10.1176/appi.psy.50.6.586. [DOI] [PubMed] [Google Scholar]
- 25.Van de Leur JP, Van der Schans CP, Loef BG, Deelman BG, Geertzen JHB, Zwaveling JH. Discomfort and factual recollection in intensive care unit patients. Crit Care. 2004;8(6):R467–R473. doi: 10.1186/cc2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang K, Zhang B, Li C, Wang C. Qualitative analysis of patients’ intensive care experience during mechanical ventilation. J Clin Nurs. 2008;18:183–190. doi: 10.1111/j.1365-2702.2008.02518.x. [DOI] [PubMed] [Google Scholar]
- 27.Astrachan DI, Kirchner JC, Goodwin WJ. Prolonged intubation vs. tracheotomy: Complications, practical and psychological considerations. Laryngoscope. 1988;98:1165–1169. doi: 10.1288/00005537-198811000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Foster A. More than nothing: The lived experience of tracheostomy while acutely ill. Intensive Crit Care Nurs. 2009;26:33–43. doi: 10.1016/j.iccn.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Oermann MH, McHugh NG, Dietrich J, Boyll R. After a tracheostomy: Patients describe their sensations. Cancer Nurs. 1983;6(5):361–366. [PubMed] [Google Scholar]
- 30.Carroll SM. Silent, slow lifeworld: The communication experience of nonvocal ventilated patients. Qual Health Res. 2007;17(9):1165–1177. doi: 10.1177/1049732307307334. [DOI] [PubMed] [Google Scholar]
- 31.Sherlock ZV, Wilson JA, Exley C. Tracheostomy in the acute setting: Patient experience and information needs. J Crit Care. 2009;24:501–507. doi: 10.1016/j.jcrc.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 32.Tate JA, Devito Dabbs A, Hoffman LA, Milbrandt E, Happ MB. Anxiety and agitation in mechanically ventilated patients. Qual Health Res. 2012;22(2):157–173. doi: 10.1177/1049732311421616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bergbom-Engberg I, Haljamäe H. Assessment of patients’experience of discomforts during respirator therapy. Crit Care Med. 1989;17(10):1068–1072. doi: 10.1097/00003246-198910000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Gilony D, Gilboa D, Blumstein T, et al. Effects of tracheostomy on well-being and body-image perceptions. Otolaryng Head Neck Surg. 2005;133:366–371. doi: 10.1016/j.otohns.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 35.Bay EJ, Algase DL. Fear and anxiety: A simultaneous concept analysis. Nurs Diagn. 1999;10(3):103–111. doi: 10.1111/j.1744-618x.1999.tb00036.x. [DOI] [PubMed] [Google Scholar]
- 36.Chlan LL. A review of the evidence for music intervention to manage anxiety in critically ill patients receiving mechanical ventilatory support. Arch Psychiatr Nurs. 2009;23(2):177–179. doi: 10.1016/j.apnu.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 37.Chlan LL. Description of anxiety levels by individual differences and clinical factors in patients receiving mechanical ventilatory support. Heart Lung. 2003;32(4):275–282. doi: 10.1016/s0147-9563(03)00096-7. [DOI] [PubMed] [Google Scholar]
- 38.Chlan LL. Relationship between two anxiety instruments in patients receiving mechanical ventilatory support. J Adv Nurs. 2004;48(5):493–499. doi: 10.1111/j.1365-2648.2004.03231.x. [DOI] [PubMed] [Google Scholar]
- 39.Chlan LL, Savik K, Weinert C. Development of a shortened state anxiety scale from the Spielberger State-Trait Anxiety Inventory (STAI) for patients receiving mechanical ventilatory support. J Nurs Meas. 2003;11(3):283–293. doi: 10.1891/jnum.11.3.283.61269. [DOI] [PubMed] [Google Scholar]
- 40.Kress JP, Gehlbach B, Lacy M, Pliskin N, Pohlman AS, Hall JB. The long-term psychological effects of daily sedative interruption on critically ill patients. Am J Respir Crit Care Med. 2003;168(12):1457–1461. doi: 10.1164/rccm.200303-455OC. [DOI] [PubMed] [Google Scholar]
- 41.Jones C, Bäckman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. Precipitants of post-traumatic stress disorder following intensive care: A hypothesis generating study of diversity in care. Intensive Care Med. 2007;33(6):978–985. doi: 10.1007/s00134-007-0600-8. [DOI] [PubMed] [Google Scholar]
- 42.Samuelson KA, Lundberg D, Fridlund B. Memory in relation to depth of sedation in adult mechanically ventilated intensive care patients. Intensive Care Med. 2006;32(5):660–667. doi: 10.1007/s00134-006-0105-x. [DOI] [PubMed] [Google Scholar]
- 43.Samuelson KA, Lundberg D, Fridlund B. Stressful experiences in relation to depth of sedation in mechanically ventilated patients. Nurs Crit Care. 2007;12(2):93–104. doi: 10.1111/j.1478-5153.2006.00199.x. [DOI] [PubMed] [Google Scholar]
- 44.Ewing G, Rogers M, Barclay S, et al. Palliative care in primary care: A study to determine whether patients and professionals agree on symptoms. Br J Gen Pract. 2006;56:27–34. [PMC free article] [PubMed] [Google Scholar]
- 45.Nekolaichuk CL, Maguire TO, Suarez-Almazor M, Rogers TW, Bruera E. Assessing the reliability of patient, nurse, and family caregiver symptom ratings in hospitalized advanced cancer patients. J Clin Oncol. 1999;17(11):3621–3630. doi: 10.1200/JCO.1999.17.11.3621. [DOI] [PubMed] [Google Scholar]
- 46.Egerod I. Uncertain terms of sedation in ICU: How nurses and physicians manage and describe sedation for mechanically ventilated patients. J Clin Nurs. 2002;11(6):831–840. doi: 10.1046/j.1365-2702.2002.00725.x. [DOI] [PubMed] [Google Scholar]
- 47.Grande GE, Barclay S, Todd CJ. Difficulty of symptom control and general practitioners’ knowledge of patients’ symptoms. Palliat Med. 1997;11:399–406. doi: 10.1177/026921639701100511. [DOI] [PubMed] [Google Scholar]
- 48.Laugsand EA, Sprangers MA, Bjordal K, Skorpen F, Kaasa S, Kepstad P. Health care providers underestimate symptom intensities of cancer patients: A multicenter European study. Health Qual Life Outcomes. 2012;8:104–117. doi: 10.1186/1477-7525-8-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Broyles LM, Colbert AM, Tate JA, Swigart VA, Happ MB. Clinicians’ evaluation and management of mental health, substance abuse, and chronic pain conditions in the intensive care unit. Crit Care Med. 2008;36(1):87–93. doi: 10.1097/01.CCM.0000292010.11345.24. [DOI] [PubMed] [Google Scholar]
- 50.Nekolaichuk CL, Bruera E, Spachynski K, MacEachern T, Hanson J, Maguire TO. A comparison of patient and proxy symptom assessments in advanced cancer patients. Palliat Med. 1999;13:311–323. doi: 10.1191/026921699675854885. [DOI] [PubMed] [Google Scholar]
- 51.Chlan LL, Weinert CR, Heiderscheit A, et al. Effects of patient-directed music intervention on anxiety and sedative exporsure in critically ill patients receiving mechanical ventilator support: A randomized clinical trial. JAMA. 2013;309(22):2335–2344. doi: 10.1001/jama.2013.5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chlan LL, Savik K. Patterns of anxiety in critically ill patients receiving mechanical ventilatory support. Nurs Res. 2011;60(3 Suppl):S50–S57. doi: 10.1097/NNR.0b013e318216009c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cline ME, Herman J, Shaw ER, Morton RD. Standardization of the visual analogue scale. Nurs Resh. 1992;4(6):378–380. [PubMed] [Google Scholar]
- 54.Gift AG. Visual analogue scales: measurement of subjective phenomena. Nurs Res. 1989;38(5):286–288. [PubMed] [Google Scholar]
- 55.Wewers M, Lowe N. A critical review of visual analog scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13(4):227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 56.Knebel AR, Janson-Bjerklie SL, Malley JD, Wilson AG, Marini JJ. Comparison of breathing comfort during weaning with two ventilatory modes. Am J Respir Crit Care Med. 1994;149(1):14–18. doi: 10.1164/ajrccm.149.1.8111572. [DOI] [PubMed] [Google Scholar]
- 57.Vogelsang J. The Visual Analog Scale: An accurate and sensitive method for self-reporting preoperative anxiety. J Post Anesth Nurs. 1988;3(4):235–239. [PubMed] [Google Scholar]
- 58.Lush MT, Janson-Bjerklie S, Carrieri VK, Lovejoy N. Dyspnea in the ventilator-assisted patient. Heart Lung. 1988;17(5):528–535. [PubMed] [Google Scholar]
- 59.Veelo DP, Dongelmans DA, Binnekade JM, Korevaar JC, Vroom MB, Schultz MJ. Tracheotomy does not affect reducing sedation requirements of patients in intensive care – A retrospective study. Crit Care. 2006;10(4):R99. doi: 10.1186/cc4961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]