Abstract
Purpose of review
Despite widespread marijuana use among adolescents, accurate information on known health effects is poorly disseminated to clinicians and their patients. Amidst rapidly evolving drug policy in the United States and elsewhere, it is imperative that providers understand the short- and long-term consequences of marijuana use.
Recent findings
Research on regular marijuana use highlights a unique susceptibility of the developing adolescent brain to adverse neurocognitive and psychiatric outcomes. Although studies have not firmly established causality, onset of regular marijuana use in adolescence is associated with later decline in cognitive function, as well as with adult onset of psychosis and anxiety. Educational and employment outcomes may be poorer among regular marijuana-using adolescents. A number of other adverse respiratory, cardiovascular, endocrine and gastrointestinal associations with regular marijuana use have also been established. Good screening tools and promising brief intervention and behavioral treatment programs are available to clinicians, who are in a position to identify problematic marijuana use among adolescents and refer for services.
Summary
A common misperception among youth is that marijuana use is without harm. However, adolescent marijuana use may have measurable, durable and potentially irreversible effects on later cognitive function and mental health.
Keywords: adolescent, cannabis, marijuana abuse, drug abuse
INTRODUCTION
Second to alcohol, marijuana is the most commonly used substance among adolescents, despite its status as an illegal drug in many settings [1–3]. There is a growing body of evidence linking youth marijuana use to adverse short- and long-term health outcomes [4]. For decades, a well-established public health campaign has showcased the adverse effects of cigarettes, but a similar campaign has not been as robust or successful for marijuana [5]. Accordingly, the proportion of youth who believe marijuana use carries risk has declined rapidly in recent years [2]. Therefore, it is imperative that clinicians understand the current body of literature on adolescent marijuana use in order to counsel youth on potential health effects in an evidence-informed manner.
Marijuana Policy Changes
In the United States (US) and elsewhere, marijuana policy is rapidly evolving, with some jurisdictions decriminalizing the possession of small quantities of cannabis, others allowing use of marijuana for medical purposes, and still others fully legalizing the drug for adults and regulating and taxing its sale. In 2012, ballot measures were approved in Colorado and Washington State, with Colorado having implemented legal marijuana sales on January 1, 2014. In late 2013, Uruguay became the first country in the world to legalize the cultivation and sale of marijuana at the national level. Large professional organizations, including the American Academy of Pediatrics [6], the American Medical Association [7], the American Society of Addiction Medicine [8], and the American Academy of Child and Adolescent Psychiatry [9] all have policy statements identifying marijuana as a public health concern and currently oppose further steps towards legalization.
Conversely, others have argued that the criminalization of young drug users is harmful for the individual and for society. A recent report by the Annie E. Casey Foundation highlighted that the average annual cost of incarceration in a juvenile corrections facility in the US approaches $90,000 per youth, and that many of those jailed are disadvantaged adolescents whose development, education and normal integration into society becomes permanently disrupted [10]. In another recent report, the Global Commission on Drug Policy stressed that youth worldwide are exposed to undue violence and corruption as a result of purchasing marijuana on the black market [11]. In the case of full legalization and regulation of marijuana, some have illustrated how taxes accrued from sales might be invested in evidence-based drug prevention and treatment programs targeted at youth [12].
Regardless of possible benefits to society, the movement towards legalization should carefully consider how more lenient policies might change the prevalence of adolescent marijuana use and dependence. On the one hand, permissive marijuana policies may increase availability and decrease the cost of marijuana, result in greater social acceptability of its use, and reduce perceptions of its potential harmful effects [2, 13]. On the other hand, steps towards legalization may not noticeably increase the prevalence of use of a drug as widespread as marijuana that is already effectively decriminalized in many settings, as was found in a recent epidemiologic study [14]. How newly instituted policies affect adolescent marijuana use is likely to be an area of intense study in years to come.
Epidemiology of use
Marijuana is the most commonly used illicit drug in developed countries [2, 3, 15]. In the US, three recurring surveys of the general adolescent population track youth marijuana use. The 2013 Monitoring the Future survey of US middle and high school students demonstrates that youth marijuana use rates have risen in recent years even as alcohol and tobacco use rates have declined [2]. The US Centers for Disease Control and Prevention 2011 Youth Risk Behavior Surveillance System (YRBSS) highlights that approximately four in ten high school students have used marijuana in their lifetime, with prevalence highest among males and among black and Hispanic youth [1]. According to YRBSS, use begins early in adolescence; by the 9th grade, one in three boys and one in four girls have used marijuana. The 2012 US National Survey on Drug Use and Health (NSDUH), a household rather than school-based survey, confirms that daily or near-daily use of marijuana has recently increased among adolescents [3].
DRUG EFFECTS, DEPENDENCE AND WITHDRAWAL
Marijuana, derived from the plant Cannabis sativa and often referred to simply as ‘cannabis’ (with the terms ‘marijuana’ and ‘cannabis’ used interchangeably throughout the present review), exerts its effects primarily through Δ-9-tetrahydrocannabinol (THC). A fat-soluble compound, THC readily crosses the blood-brain barrier as well as the placenta [16]. Its lipophilicity and accumulation in fat results in a long elimination half-life of several days to one week. THC and its metabolites act on the body’s endogenous cannabinoid receptors, present both in the central and peripheral nervous systems and critical to normal neurodevelopment [17].
Marijuana is most commonly smoked but may also be ingested. The potency of THC in marijuana preparations has more than doubled in the last two decades [18]. New delivery systems similar to those used for e-cigarettes allow users to inhale vaporized plant material, a process resulting in decreased inhalation of smoke byproducts [19]. The late 2000s saw the emergence and increasing popularity of ‘synthetic cannabinoids’, designer drugs with cannabinoid receptor agonists with effects similar to THC [15]. Synthetic cannabinoids are often contained in herbal mixtures marketed as “Spice”, “K2”, or “Kronic”, and many have been classified as Schedule I substances in the US [20].
Psychologic and physiologic effects
The acute effects of marijuana peak at 30 minutes after inhalation and one to six hours after ingestion, lasting for two to four hours [21]. Psychologic effects of marijuana vary by individual and by dose. Positive effects include relaxation, euphoria, heightened perception, sociability, sensation of time slowing, increased appetite, and decreased pain. Negative effects include paranoia, anxiety, irritability, impaired short-term memory, poor attention and judgement, and hindered coordination and balance. Physiologically, marijuana causes tachycardia of 20 to 50 beats per minute above baseline (an effect amplified by co-ingestion with ethanol), elevated blood pressure, bronchial relaxation, dry mouth and throat, and conjunctival injection [21, 22].
Cannabis dependence
In 2013, the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) combined previously separate cannabis abuse and dependence diagnoses into a single “cannabis use disorder” [23]. Clinically, marijuana dependence remains an important concept, and is marked by loss of control and ongoing use despite physical, psychological or social harms [4, 23]. Earlier age of onset of marijuana use is associated with greater likelihood of dependence, occurring in approximately one in six adolescent users [24]. Recent data from the US Substance Abuse and Mental Health Services Administration demonstrate that, second only to alcohol, marijuana accounts for the largest number of adolescent admissions to substance use treatment programs [25].
Cannabis withdrawal syndrome
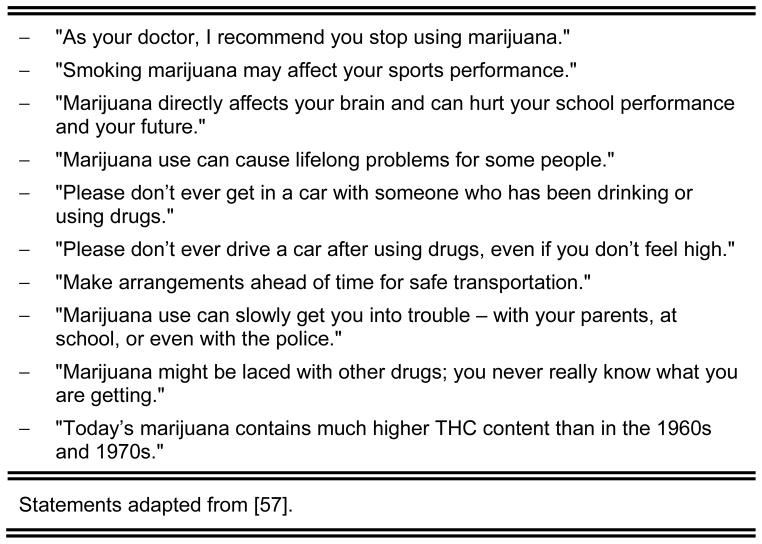
A “cannabis withdrawal syndrome” was added to the DSM-5 in 2013 [23]. Its features are listed in Figure 1.
FIGURE 1.
Features of the cannabis withdrawal syndrome*.
HEALTH OUTCOMES OF CHRONIC MARIJUANA USE
Establishing causal relationships between marijuana use and adverse health outcomes has been difficult because most studies of marijuana users are observational studies, requiring researchers to carefully consider the possibility of reverse causation and of confounding by use of other drugs or alcohol [4]. Additionally, how “chronic” or “regular” marijuana use is defined varies across studies. For the adolescent, it is often defined as near-daily use over several years [2–4]. Because of inconsistencies across studies, there is no clear indication as to whether a ‘safe’ amount of marijuana use exists for adolescents. The following text and corresponding Table present the recent body of literature examining chronic marijuana use and adverse associations.
TABLE.
Known associations between chronic* marijuana use and adverse health outcomes to help guide physicians in counseling adolescent patients.
| System | Known association | Reference(s) |
|---|---|---|
| Respiratory | – Regular users likely to experience wheezing, cough, and mucous production | [27] |
| – No established associations with lung cancer or with long-term changes in lung function | [26–28] | |
| Cardiovascular | – No established association with adverse cardiovascular outcomes among adolescents | [30] |
| – Among adults, elevated mortality among cannabis smokers who have had a prior myocardial infarction | [30, 32] | |
| Endocrine | – Among males, results in dose-related decrease in testosterone levels | [33] |
| – Associations with erectile dysfunction, oligospermia, and inhibition of orgasm in males | [33, 34] | |
| – Association with gynecomastia among males has been reported, but poorly characterized | [33] | |
| Gastrointestinal | – Frequent use may result in cannabis hyperemesis syndrome, marked by nausea, vomiting, epigastric abdominal pain, and occasionally diarrhea, with symptoms characteristically relieved by hot showers or baths | [35] |
| Neurocognitive | – Any use results in short-term decline in attention, executive function and memory, lasting at least one to several days after acute intoxication, with subtle effects at one month | [38] |
| – Use results in near doubling of odds of motor vehicle accident and fatal collision | [39] | |
| – Regular use during adolescence and into adulthood associated with decline in IQ; cessation may not result in restored IQ | [41] | |
| Psychiatric | – Association with psychosis and schizophrenia, with even greater odds among frequent users | [44, 45] |
| – No established association with depression; possible association with anxiety | [44, 46–48] | |
| Psychosocial | – Associations with poor school performance, negative attitudes toward school, and decreased odds of completing high school; however, cause-effect relationship not established | [49] |
| – Association with poor employment outcomes | [50–52] | |
| – Marijuana use itself per se likely does not cause use of other harder drugs, but purchasing marijuana may offer opportunities to purchase of other illicit drugs on the black market, such as heroin, cocaine, amphetamines | [54] |
Respiratory
Recent systematic reviews examining long-term effects on pulmonary function [26] and risk of lung cancer [27] have not established a firm association of chronic marijuana use with either outcome. Studies are variable in quality because associations are subject to confounding by cigarette smoking. A recent large longitudinal study of young adults directly compared marijuana and tobacco exposure and showed no effect of occasional marijuana exposure on pulmonary function [28]. Nonetheless, marijuana smoke contains many of the same irritants and carcinogens as cigarette smoke at similar or even higher concentrations [29]. Clinicians may counsel that regular marijuana users are significantly more likely than non-users to experience wheezing, cough, and mucous production [27].
Cardiovascular
Acutely, marijuana causes an increase in heart rate, but otherwise, chronic marijuana use is not associated with adverse cardiovascular outcomes among healthy adolescents [30]. Studies considering associations between marijuana use and cardiovascular risk factors, such as obesity, hypertension, hyperlipidemia, elevated fasting glucose levels, and insulin resistance have been inconclusive, likely due to confounding comorbid behaviors such as tobacco smoking [31]. However, clinicians should be aware that for adolescent patients with risk factors for ischemic heart disease, marijuana use later in life may be harmful in light of evidence showing elevated mortality among cannabis smokers who have had a prior myocardial infarction [30, 32].
Endocrine
A 2012 review by Gorzalka and colleagues summarizes the known effects of marijuana use on the hypothalamic-pituitary-gonadal axis [33]. Among males, chronic marijuana use is associated with a dose-related decrease in testosterone levels, and with erectile dysfunction and oligospermia. Marijuana exerts direct effects on testicular Leydig cells, and inhibits the release of luteinizing hormone (LH) from the pituitary and gonadotropin-releasing hormone (GnRH) from the hypothalamus. An association between marijuana use and gynecomastia in males has long been described but has not undergone rigorous study to date. Although marijuana also suppresses LH and GnRH release among females, interactions between the hypothalamus-pituitary-gonadal (HPG) axis in females are more complex and their clinical implications less well understood. For both males and females, low doses of marijuana may enhance sexual desire, but high doses tend to inhibit it, and may even prevent men from reaching orgasm [34].
Gastrointestinal
The cannabis hyperemesis syndrome is a newly described clinical phenomenon. In a recent case series, the largest to date on the topic, Simonetto and colleagues summarize this syndrome in which frequent marijuana use results in nausea, vomiting, abdominal pain most commonly epigastric in location, and occasionally diarrhea [35]. Symptoms are characteristically relieved by hot showers or baths and are worse in the morning. Resolution ultimately only occurs with cessation of use, usually several months after quitting. The majority of patients with cannabis hyperemesis syndrome use marijuana at least daily, and almost 95% of all patients use it at least weekly. Longer duration of marijuana is not required for development of the syndrome; indeed, one-third of all patients have only used marijuana for less than one year.
Neurocognitive
Heavy marijuana use is associated with short-term declines in attention, executive function and memory [36]. Acute intoxication results in decreased coordination, distorted spatial perception, and altered awareness of the passage of time, all of which may be detrimental to, for example, the adolescent athlete [37]. Clinicians may counsel youth that many of the above effects exhibit a ‘hangover’ period lasting at least one day and perhaps even several days after last use, with some subtle effects evident even one month later [38]. In the acute intoxication period, marijuana use clearly results in a near doubling of the odds of motor vehicle accident and fatal collision [39], despite the belief among many youth that marijuana does not impair driving abilities [40].
A recent prospective study by Meier and colleagues demonstrated that regular cannabis use in adolescence was associated with an 8-point decline in intelligence quotient (IQ) measured at 38 years of age in adulthood [41]. This effect persisted despite controlling for comorbid drug and alcohol use, mental illness, and educational level. Among the adolescent cannabis users, cessation of cannabis use was not associated with restored IQ in adulthood, suggesting that during this critical period of brain development, long-lasting and non-modifiable changes may be taking place.
Chronic marijuana users may exhibit reduced brain volume in memory centers such as the hippocampus and amygdala [42, 43]. Cannabinoid receptors, which are intricately involved in normal brain development, may mediate these long-term changes [17, 42]. Perhaps most vulnerable to regular marijuana use is white matter, with functional imaging studies showing impaired axonal connectivity that is worsened by earlier age at onset of use [43].
Psychiatric
Of the associations of marijuana with mental health outcomes, the strongest is with schizophrenia. A recent meta-analysis demonstrated that lifetime use of cannabis is associated with a 41% increase in the odds of subsequent psychosis and that odds are even greater odds among heavy users [44]. These data are supported by another recent prospective cohort study [45]. Although marijuana use preceded the development of symptoms of schizophrenia in the longitudinal studies conducted to date, an underlying common cause leading to both use of marijuana and to subsequent psychosis is possible.
The evidence linking marijuana with depression and anxiety is conflicting. Two recent systematic reviews both concluded that there was an association between heavy marijuana use and depressive symptoms, but acknowledged that effects were reduced or eliminated after adjusting for confounders [44, 46]. A recent longitudinal study of high school students not included in these meta-analyses showed that heavy marijuana use preceded depression, but not suicidal ideation or attempt [47]. One of the above two systematic reviews also examined anxiety disorders and concluded that studies differed so greatly in methodology and findings that further research was needed [44]. A more recent study following adolescents into adulthood showed that those continuing daily use at age 29 years had nearly triple the odds of an anxiety disorder [48].
Psychosocial
Studies examining educational outcomes among marijuana-using youth are hampered by cross-sectional design and an inability to determine causality. These cross-sectional studies note that marijuana use is associated with poor school performance, negative attitudes toward school, and decreased high school completion [49]. A number of recent studies of regular marijuana users have also shown poor employment outcomes [50–52].
A subject of great debate has been whether marijuana is a ‘gateway’ drug – that is, a drug whose use causes youth to transition to ‘harder’ illicit drugs. Indeed, early studies demonstrated that heavy marijuana users are more likely to use other illicit drugs later on [53]. Although one explanation for this observation is that using marijuana makes adolescents more inclined to use other drugs, alternative explanations have emerged. Most plausible among these is that marijuana users, who in most jurisdictions are forced to buy cannabis on the black market, are likely to be also offered opportunities to purchase other illicit drugs at the point of sale [54]. Clinicians might consider counseling youth that black market purchases of marijuana are likely to also offer opportunities to obtain other drugs with potentially hazardous effects.
SCREENING AND TREATMENT
Given the high prevalence of marijuana use, efforts have been made to identify the subset of youth who engage in problematic use. Although some adolescents may present with symptoms of a cannabis use disorder, others may present with any of the adverse health outcomes outlined above. For youth who present with symptoms of depression or anxiety, clinicians should wait for four weeks of abstinence before diagnosing youth with a psychiatric condition [21], since intoxication and withdrawal can both mimic symptoms of depression or anxiety [23].
Screening
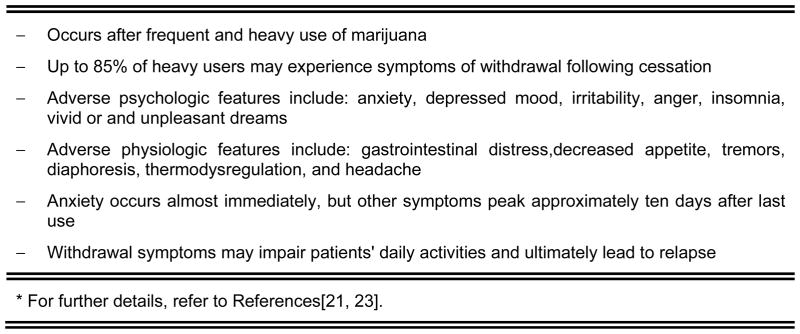
Clinicians should screen youth annually for use of marijuana and other substances [55]. A simple 6-item instrument, the CRAFFT screen, has been validated among adolescents for assessment of alcohol and drug use [56]. The instrument, shown in Figure 2, requires straight-forward ‘yes/no’ responses and is developmentally appropriate for adolescents.
FIGURE 2.
The CRAFFT screen for assessing marijuana use among adolescents.
Treatment
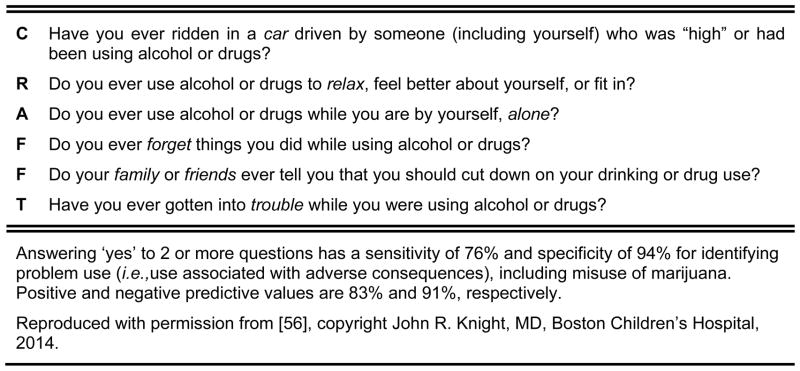
Adolescents who screen positive for marijuana use should receive a brief intervention, such as brief patient-centered advice, from the clinician and/or referral to a drug treatment program [57, 58]. Suggested statements for brief advice are shown in Figure 3. Of the available referral-based treatment programs for adolescents, evidence most strongly supports motivational enhancement therapy, cognitive-behavioral therapy, and contingency management [59], with the highest abstinence rates when these approaches are combined [60]. Unfortunately, across studies, abstinence is generally maintained at one year by only a minority of youth [59].
FIGURE 3.
Sample statements of brief advice on marijuana reduction and cessation.
Although medications are not currently standard of care for treatment of marijuana, a growing evidence base supports pharmacologic therapy used with behavioral treatment. Promising drugs include dronabinol (oral THC) used as maintenance therapy to reduce withdrawal symptoms and craving [61]; buspirone, also commonly used for nicotine addiction [62]; N-acetyl cysteine [63]; and gabapentin [64]. A recent trial examining the selective serotonin reuptake inhibitor escitalopram showed no effect [65].
Barriers may prevent youth from accessing treatment, including lack of awareness of available options, absence of youth-friendly programs, excessively long waiting lists, and the perceived stigma of seeking treatment [66]. Novel approaches that preserve adolescent autonomy and confidentiality show promise, such as self-guided Internet-based treatment [67]. Future studies will likely combine behavioral approaches, medications and novel delivery methods, and further delineate the most effective treatment regimens for adolescents.
CONCLUSION
The adverse health effects associated with marijuana are myriad, and adolescents demonstrate particular susceptibility to long-term neurocognitive and psychiatric changes from chronic marijuana use. Despite the growing body of evidence showing potential harm to youth, an effective public health campaign similar to that of the anti-cigarette movement has yet to emerge for marijuana. There is movement towards legalization of marijuana for medical or recreational use in many North American and international settings. Clinicians are in a unique position to at once understand the health ramifications as well as screen for adolescent substance use. If marijuana becomes increasingly available to youth as a result of drug policy changes, clinicians will inevitably play a critical role in identifying and helping youth who engage in problematic use.
KEY POINTS.
Marijuana is the most commonly used illicit substance among adolescents, and amidst a movement towards legalization of marijuana for medical and recreational purposes in many jurisdictions, its adverse health effects remain poorly understood.
Onset of daily or near-daily marijuana use during adolescence is associated with adult decline in neurocognitive and psychiatric function, including decreased intelligence quotient (IQ) and risk of psychotic, mood and anxiety disorders.
Effective screening tools, most notably including the CRAFFT instrument, can help pediatricians identify problematic use of marijuana, provide brief advice, and in many settings, refer to a behavioral treatment program.
Acknowledgments
Drs. Hadland and Harris are supported by the Division of Adolescent and Young Adult Medicine at Boston Children’s Hospital and the Leadership Education in Adolescent Health Training Program T71 MC00009 (MCH/HRSA). Dr. Harris is also supported by the National Institute on Alcohol Abuse and Alcoholism (1R01AA021904).
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
References
- 1*.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162. The first of three important US nationwide surveys of drug use among the general adolescent population. A school-based survey on youth risk behaviors providing data on lifetime and recent use of marijuana and other substances. [PubMed] [Google Scholar]
- 2*.Johnston LD, O’Mally PM, Bachman JG, et al. Monitoring the Future national results on drug use: 2013 Overview, Key Findings on Adolescent Drug Use. 2013 [cited 2013 30 December]; Available from: http://www.monitoringthefuture.org/data/13data.htmlThe second of three important US nationwide surveys of drug use among the general adolescent population. A school-based survey on substance use providing important data on the increasing prevalence of daily or near-daily marijuana use.
- 3*.SAMHSA. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13–4795. 2013 [cited 2013 19 September]; Available from: http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/NationalFindings/NSDUHresults2012.htmThe third of three important US nationwide surveys of drug use among the general adolescent population. A household-based survey including questions on adolescent substance use that highlights important epidemiologic trends.
- 4**.Hall W, Degenhardt L. The adverse health effects of chronic cannabis use. Drug Test Anal. 2014;6(1–2):39–45. doi: 10.1002/dta.1506. A comprehensive review of the myriad associations of marijuana with adverse physical and mental health outcomes. [DOI] [PubMed] [Google Scholar]
- 5.Levy S. Effects of marijuana policy on children and adolescents. JAMA Pediatr. 2013;167(7):600–602. doi: 10.1001/jamapediatrics.2013.2270. [DOI] [PubMed] [Google Scholar]
- 6.Joffe A. Legalization of marijuana: potential impact on youth. Pediatrics. 2004;113(6):1825–1826. [PubMed] [Google Scholar]
- 7.AMA. H-95.998 AMA Policy Statement on Cannabis (Marijuana) 2012 [cited 2014 24 January]; Available from: http://www.ama-assn.org/resources/doc/PolicyFinder/policyfiles/HnE/H-95.998.HTM.
- 8.ASAM. White Paper on State-Level Proposals to Legalize Marijuana. 2012 [cited 2014 24 January]; Available from: http://www.asam.org/docs/publicy-policy-statements/state-level-proposals-to-legalize-marijuana-final2773DD668C2D.pdf.
- 9.AACAP. AACAP Medical Marijuana Policy Statement. 2012 [cited 2014 24 January]; Available from: http://www.aacap.org/AACAP/Policy_Statements/2012/AACAP_Medical_Marijuana_Policy_Statement.aspx.
- 10.AECF. No Place for Kids: The Case for Reducing Juvenile Incarceration. 2011 [cited 2013 6 October]; Available from: http://www.aecf.org/~/media/Pubs/Topics/JuvenileJustice/DetentionReform/NoPlaceForKids/JJ_NoPlaceForKids_Full.pdf.
- 11.GCODP. War on Drugs: Report of the Global Commission on Drug Policy. 2011 [cited 2013 6 October]; Available from: http://www.globalcommissionondrugs.org/wp-content/themes/gcdp_v1/pdf/Global_Commission_Report_English.pdf.
- 12.Werb D, Nosyk B, Kerr T, et al. Estimating the economic value of British Columbia’s domestic cannabis market: implications for provincial cannabis policy. Int J Drug Policy. 2012;23(6):436–441. doi: 10.1016/j.drugpo.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Caulkins JP, Kilmer B, MacCoun RJ, et al. Design considerations for legalizing cannabis: lessons inspired by analysis of California’s Proposition 19. Addiction. 2012;107(5):865–871. doi: 10.1111/j.1360-0443.2011.03561.x. [DOI] [PubMed] [Google Scholar]
- 14*.Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013;103(8):1500–1506. doi: 10.2105/AJPH.2012.301117. A carefully conducted epidemiologic study of cannabis use in the US before and after implementation of medical marijuana laws in several states that did not demonstrate worsening prevalence of adolescent use. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UNODC. World Drug Report 2013. 2013 [cited 2013 7 October]; Available from: http://www.unodc.org/unodc/secured/wdr/wdr2013/World_Drug_Report_2013.pdf.
- 16.Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42(4):327–360. doi: 10.2165/00003088-200342040-00003. [DOI] [PubMed] [Google Scholar]
- 17.Harkany T, Guzmán M, Hurd YL. Endocannabinoid Functions in Neurogenesis, Neuronal Migration, and Specification. In: Köfalvi A, editor. Cannabinoids and the Brain. New York, NY: Springer Science + Business Media, LLC; 2008. pp. 237–256. [Google Scholar]
- 18.Mehmedic Z, Chandra S, Slade D, et al. Potency trends of Delta9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J Forensic Sci. 2010;55(5):1209–1217. doi: 10.1111/j.1556-4029.2010.01441.x. [DOI] [PubMed] [Google Scholar]
- 19.Abrams DI, Vizoso HP, Shade SB, et al. Vaporization as a smokeless cannabis delivery system: a pilot study. Clinical pharmacology and therapeutics. 2007;82(5):572–578. doi: 10.1038/sj.clpt.6100200. [DOI] [PubMed] [Google Scholar]
- 20.Sacco LN, Finklea K. Synthetic Drugs: Overview and Issues for Congress. 2013 [cited 2013 7 October]; Available from: http://www.fas.org/sgp/crs/misc/R42066.pdf.
- 21.Winstock AR, Ford C, Witton J. Assessment and management of cannabis use disorders in primary care. BMJ. 2010;340:c1571. doi: 10.1136/bmj.c1571. [DOI] [PubMed] [Google Scholar]
- 22.Bramness JG, Khiabani HZ, Morland J. Impairment due to cannabis and ethanol: clinical signs and additive effects. Addiction. 2010;105(6):1080–1087. doi: 10.1111/j.1360-0443.2010.02911.x. [DOI] [PubMed] [Google Scholar]
- 23*.APA. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, DC: American Psychiatric Association; 2013. The DSM-V contains a new diagnosis of cannabis use disorder that is of clinical relevance to practicing pediatric and mental health providers. [Google Scholar]
- 24.Dennis M, Babor TF, Roebuck MC, et al. Changing the focus: the case for recognizing and treating cannabis use disorders. Addiction. 2002;97 (Suppl 1):4–15. doi: 10.1046/j.1360-0443.97.s01.10.x. [DOI] [PubMed] [Google Scholar]
- 25.SAMHSA. Treatment Episode Data Set (TEDS). Highlights - 2007. National Admissions to Substance Abuse Treatment Services. DASIS Series: S-45, DHHS Publication No. (SMA) 09-4360. 2009 [cited; Available from: http://wwwdasis.samhsa.gov/teds07/tedshigh2k7.pdf.
- 26.Tetrault JM, Crothers K, Moore BA, et al. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167(3):221–228. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mehra R, Moore BA, Crothers K, et al. The association between marijuana smoking and lung cancer: a systematic review. Arch Intern Med. 2006;166(13):1359–1367. doi: 10.1001/archinte.166.13.1359. [DOI] [PubMed] [Google Scholar]
- 28.Pletcher MJ, Vittinghoff E, Kalhan R, et al. Association between marijuana exposure and pulmonary function over 20 years. JAMA. 2012;307(2):173–181. doi: 10.1001/jama.2011.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moir D, Rickert WS, Levasseur G, et al. A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem Res Toxicol. 2008;21(2):494–502. doi: 10.1021/tx700275p. [DOI] [PubMed] [Google Scholar]
- 30*.Thomas G, Kloner RA, Rezkalla S. Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: what cardiologists need to know. Am J Cardiol. 2014;113(1):187–190. doi: 10.1016/j.amjcard.2013.09.042. A review of the current evidence surrounding cardiovascular outcomes among marijuana users highlighting areas for future research. [DOI] [PubMed] [Google Scholar]
- 31.Penner EA, Buettner H, Mittleman MA. The impact of marijuana use on glucose, insulin, and insulin resistance among US adults. Am J Med. 2013;126(7):583–589. doi: 10.1016/j.amjmed.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Mukamal KJ, Maclure M, Muller JE, et al. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155(3):465–470. doi: 10.1016/j.ahj.2007.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gorzalka BB, Dang SS. Minireview: Endocannabinoids and gonadal hormones: bidirectional interactions in physiology and behavior. Endocrinology. 2012;153(3):1016–1024. doi: 10.1210/en.2011-1643. [DOI] [PubMed] [Google Scholar]
- 34.Smith AM, Ferris JA, Simpson JM, et al. Cannabis use and sexual health. J Sex Med. 2010;7(2 Pt 1):787–793. doi: 10.1111/j.1743-6109.2009.01453.x. [DOI] [PubMed] [Google Scholar]
- 35.Simonetto DA, Oxentenko AS, Herman ML, et al. Cannabinoid hyperemesis: a case series of 98 patients. Mayo Clin Proc. 2012;87(2):114–119. doi: 10.1016/j.mayocp.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crean RD, Crane NA, Mason BJ. An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions. J Addict Med. 2011;5(1):1–8. doi: 10.1097/ADM.0b013e31820c23fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huestis MA, Mazzoni I, Rabin O. Cannabis in sport: anti-doping perspective. Sports Med. 2011;41(11):949–966. doi: 10.2165/11591430-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Medina KL, Hanson KL, Schweinsburg AD, et al. Neuropsychological functioning in adolescent marijuana users: Subtle deficits detectable after a month of abstinence. J Int Neuropsychol Soc. 2007;13(05):807–820. doi: 10.1017/S1355617707071032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39**.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. A meta-analysis of nine studies highlighting the increased risk of motor vehicle accident following marijuana use. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.SADD LM. Hazy Logic: Liberty Mutual Insurance/SADD Study Finds Driving Under the Influence of Marijuana a Greater Threat to Teen Drivers than Alcohol. 2012 [cited 2013 30 Dec]; Available from: http://www.sadd.org/press/presspdfs/MarijuanaTeenRelease.pdf.
- 41**.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657–2664. doi: 10.1073/pnas.1206820109. A carefully conducted longitudinal study that showed that chronic marijuana use starting in adolescence persisting into adulthood was associated with a mean decline in IQ of 8 points, and that cessation of use did not reverse this decline in IQ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schacht JP, Hutchison KE, Filbey FM. Associations between cannabinoid receptor-1 (CNR1) variation and hippocampus and amygdala volumes in heavy cannabis users. Neuropsychopharmacology. 2012;37(11):2368–2376. doi: 10.1038/npp.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zalesky A, Solowij N, Yucel M, et al. Effect of long-term cannabis use on axonal fibre connectivity. Brain. 2012;135(Pt 7):2245–2255. doi: 10.1093/brain/aws136. [DOI] [PubMed] [Google Scholar]
- 44.Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 45.Manrique-Garcia E, Zammit S, Dalman C, et al. Cannabis, schizophrenia and other non-affective psychoses: 35 years of follow-up of a population-based cohort. Psychol Med. 2012;42(6):1321–1328. doi: 10.1017/S0033291711002078. [DOI] [PubMed] [Google Scholar]
- 46.Horwood LJ, Fergusson DM, Coffey C, et al. Cannabis and depression: an integrative data analysis of four Australasian cohorts. Drug Alcohol Depend. 2012;126(3):369–378. doi: 10.1016/j.drugalcdep.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 47.Rasic D, Weerasinghe S, Asbridge M, et al. Longitudinal associations of cannabis and illicit drug use with depression, suicidal ideation and suicidal attempts among Nova Scotia high school students. Drug Alcohol Depend. 2013;129(1–2):49–53. doi: 10.1016/j.drugalcdep.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 48.Degenhardt L, Coffey C, Romaniuk H, et al. The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction. 2013;108(1):124–133. doi: 10.1111/j.1360-0443.2012.04015.x. [DOI] [PubMed] [Google Scholar]
- 49.Lynskey M, Hall W. The effects of adolescent cannabis use on educational attainment: a review. Addiction. 2000;95(11):1621–1630. doi: 10.1046/j.1360-0443.2000.951116213.x. [DOI] [PubMed] [Google Scholar]
- 50.Arria AM, Garnier-Dykstra LM, Cook ET, et al. Drug use patterns in young adulthood and post-college employment. Drug Alcohol Depend. 2013;127(1–3):23–30. doi: 10.1016/j.drugalcdep.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hara M, Huang DY, Weiss RE, et al. Concurrent life-course trajectories of employment and marijuana-use: exploring interdependence of longitudinal outcomes. J Subst Abuse Treat. 2013;45(5):426–432. doi: 10.1016/j.jsat.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hyggen C. Does smoking cannabis affect work commitment? Addiction. 2012;107(7):1309–1315. doi: 10.1111/j.1360-0443.2012.03796.x. [DOI] [PubMed] [Google Scholar]
- 53.Swift W, Coffey C, Degenhardt L, et al. Cannabis and progression to other substance use in young adults: findings from a 13-year prospective population-based study. J Epidemiol Community Health. 2012;66(7):e26. doi: 10.1136/jech.2010.129056. [DOI] [PubMed] [Google Scholar]
- 54.Wagner FA, Anthony JC. Into the world of illegal drug use: exposure opportunity and other mechanisms linking the use of alcohol, tobacco, marijuana, and cocaine. Am J Epidemiol. 2002;155(10):918–925. doi: 10.1093/aje/155.10.918. [DOI] [PubMed] [Google Scholar]
- 55.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 56.Knight JR, Sherritt L, Shrier LA, et al. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156(6):607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 57.Brooks T, Knight JR. Screening and Brief Intervention for Adolescents. In: Ries RC, Miller SA, Saitz R, editors. Addiction Medicine. 5. Philadelphia, PA: Lippincott Williams & Wilkins; In press. [Google Scholar]
- 58.Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128(5):e1330–1340. doi: 10.1542/peds.2011-1754. [DOI] [PubMed] [Google Scholar]
- 59.Denis C, Lavie E, Fatseas M, et al. Psychotherapeutic interventions for cannabis abuse and/or dependence in outpatient settings. Cochrane Database Syst Rev. 2006;(3):CD005336. doi: 10.1002/14651858.CD005336.pub2. [DOI] [PubMed] [Google Scholar]
- 60.Hoch E, Buhringer G, Pixa A, et al. CANDIS treatment program for cannabis use disorders: Findings from a randomized multi-site translational trial. Drug Alcohol Depend. 2014;134:185–193. doi: 10.1016/j.drugalcdep.2013.09.028. [DOI] [PubMed] [Google Scholar]
- 61.Levin FR, Mariani JJ, Brooks DJ, et al. Dronabinol for the treatment of cannabis dependence: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2011;116(1–3):142–150. doi: 10.1016/j.drugalcdep.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McRae-Clark AL, Carter RE, Killeen TK, et al. A placebo-controlled trial of buspirone for the treatment of marijuana dependence. Drug Alcohol Depend. 2009;105(1–2):132–138. doi: 10.1016/j.drugalcdep.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gray KM, Carpenter MJ, Baker NL, et al. A double-blind randomized controlled trial of N-acetylcysteine in cannabis-dependent adolescents. Am J Psychiatry. 2012;169(8):805–812. doi: 10.1176/appi.ajp.2012.12010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mason BJ, Crean R, Goodell V, et al. A proof-of-concept randomized controlled study of gabapentin: effects on cannabis use, withdrawal and executive function deficits in cannabis-dependent adults. Neuropsychopharmacology. 2012;37(7):1689–1698. doi: 10.1038/npp.2012.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weinstein AM, Miller H, Bluvstein I, et al. Treatment of cannabis dependence using escitalopram in combination with cognitive-behavior therapy: a double-blind placebo-controlled study. Am J Drug Alcohol Abuse. 2014;40(1):16–22. doi: 10.3109/00952990.2013.819362. [DOI] [PubMed] [Google Scholar]
- 66.Gates P, Copeland J, Swift W, et al. Barriers and facilitators to cannabis treatment. Drug Alcohol Rev. 2012;31(3):311–319. doi: 10.1111/j.1465-3362.2011.00313.x. [DOI] [PubMed] [Google Scholar]
- 67.Rooke S, Copeland J, Norberg M, et al. Effectiveness of a self-guided web-based cannabis treatment program: randomized controlled trial. J Med Internet Res. 2013;15(2):e26. doi: 10.2196/jmir.2256. [DOI] [PMC free article] [PubMed] [Google Scholar]