A 65-year-old female at a district place with aches, pains and weakness of a couple of hour's duration visits an outpatient clinic. A few investigations of calcium and vitamin D are advised in addition to blood glucose levels and thyroid function test, and she is advised to do a dual energy X-ray absorptiometry (DXA) scan, which she didn’t manage for next few months as the same is available in a bigger city, which is 3 h travel and ultimately lands up with a hip fracture. The same is treated, and she is discharged with advice to get a DXA scan and treatment of osteoporosis is deferred for same. In the same place is a 26-year healthy girl who is prescribed once a month ibandronate at basic medical practitioner level because calcaneal bone density T-score is -2.8, the test being done as a door to door screening. The two cases represent a paradox of inappropriate omission and commission, respectively.
With increasing population and life expectancy the burden of chronic diseases is on the rise in India. Though illness such as diabetes, hypertension, and cardiac problems get priority osteoporosis remains a relatively neglected public health problem.[1]
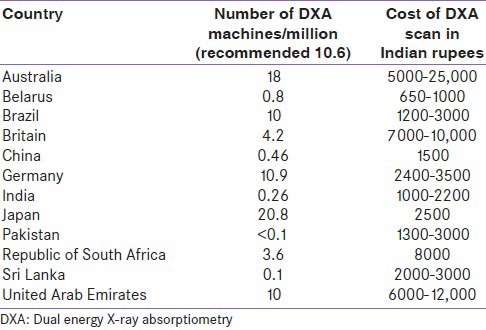
The prevalence of diabetes in India is 65 million and of osteoporosis is 50 million as per the International Diabetes Federation and International Osteoporosis Federation databases, respectively.[2,3] Though most of the diabetics are detected and receive care most of the osteoporotics are not detected and are deprived of same. Moreover, cost of annual therapy of diabetes is much more than the cost of annual therapy for osteoporosis if a basic agent like bisphosphonate is considered. One of the reasons for the neglect might be though both diabetes and osteoporosis are silent illness a very easily available measure of blood glucose levels is available for screening and monitoring of diabetes, but for osteoporosis the gold standard diagnostic modality remains DXA scan, which is far from available even in major cities. As per the report from International Osteoporosis Federation the availability of DXA machines in India is 0.26/million which is far from recommended 10.6/million.[3] Also most of the DXA machines are centered in urban areas. Even many cities do not have DXA facility. Furthermore, the fact remains that cost of DXA and osteoporosis treatment is largely not covered by the insurers. We compare badly to more developed Asian colleagues like Japan and Korea where availability of DXA is much better (20.8 and 24.5/million) as well as with the rest of the world. However, availability of DXA is poor all over Southeast Asia (South Asian Association for Regional Cooperation) region which hosts 1/5th of the world population [Table 1]. Quantitative ultrasound though is cheaper (cost in India 1200-2400 Indian rupees) also lacks trained personnel as well as good quality standardized machines.[3]
Table 1.
Availability and cost of DXA scan in few representative countries (as per the time to time audits conducted by International Osteoporosis Federation)
While the fact remains that we are far lagging behind in terms of diagnosis of osteoporosis, the other end treatment for prevention of fractures can also be initiated without DXA scan by doing a FRAX algorithm, and data that can be extrapolated to Indian population is now available. However, DXA is less commonly available, FRAX being easily available is least used. Qfracture is another web based calculator tool from population in United Kingdom, which predicts risks of osteoporotic fractures. It also has separate data of Indian, Pakistan, and Bangladesh immigrants in United Kingdom and can be used to estimate osteoporotic fracture risk over next 10 years.[4,5,6]
There remain other known risk factors for osteoporosis where there is established guidelines for prevention fracture like in case of glucocorticoid use. However, even in tertiary care centers of excellence the use of bisphosphonates along with glucocorticoids for fracture prevention is far below satisfaction (nearly 66% patients given no or inadequate prophylaxis) as seen from an audit in Mumbai hospital. A similar audit from another hospital showed that only 3 out of 105 given glucocorticoids received bisphosphonates.[7,8]
Also remains the fact that a sizable number of patients who actually land up with osteoporotic fracture go untreated. At the other end there are also odd cases of DXA scan done in nonindicated patients and blanket initiation of osteoporotic treatment for vague symptoms like bone pains. Indeed one of the studies shows that 47% of patients referred for DXA scan at a large tertiary care hospital are indeed <50-year-old screening for osteoporosis recommended beyond 65 years in females and 70 years in males unless there is special indication.[9]
Hence, we are in a situation where an important public health problem is being neglected due to lack of the facility of detection, and unawareness about the other tools of assessing fracture risk and prevention. A few minimum things that can be done is increasing the number of DXA machines in public care setting, increasing awareness about FRAX tools, not depriving patients who already had fractures from osteoporosis treatments, ensure better implementation and awareness about preexisting guidelines as for glucocorticoid induced osteoporosis, at the same time awareness also in the direction of preventing abuse of medications for treatments for osteoporosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in Southeast Asian and African regions: Need for effective strategies for prevention and control in primary health care settings. Int J Hypertens 2013. 2013:409083. doi: 10.1155/2013/409083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Unwin N, Whiting D, Guariguata L, Ghyoot G, Gan D, editors. 5th ed. Belgium: International Diabetes Federation; 2011. Diabetes Atlas. [Google Scholar]
- 3.Mithal A, Ebeling P. International Osteoporosis Federation. The Asia Pacific Regional audit: Epidemology, costs and burden of osteoporosis in 2013. [Last accessed on 2014 April 16]. Available from: http://www.iofbonehealth.org/sites/default/files/media/PDFs/Regional%20Audits/2013-Asia_Pacific_Audit_0_0.pdf . [DOI] [PMC free article] [PubMed]
- 4.Kalra S, Kalra B, Baruah M. Diagnosing osteoporosis made easier: The FRAX tool gets better. J Med Nut Nutraceut. 2012;1:61–2. [Google Scholar]
- 5.Kalra S. Diagnosing osteoporosis the easy way: FRAX and QFracture. J Pak Med Assoc 2013. 2013;63:421–2. [PubMed] [Google Scholar]
- 6.Qfracture ®-2013 risk calculator. [Last accessed on 2014 Apr 16]. Available from: http://www.qfracture.org .
- 7.Shrinivas N, Sharma V, Chitnis N, Mangat G, Samant R, Canchi B. Primary prophylaxis for steroid-induced osteoporosis: Are we doing enough? – An audit from a tertiary care centre. Indian J Rheumatol. 2010;5:176–9. [Google Scholar]
- 8.Gera C, Vij AS. Glucocorticoid-induced osteoporosis: Unawareness or negligence in India? Int J Rheum Dis. 2009;12:230–3. doi: 10.1111/j.1756-185X.2009.01415.x. [DOI] [PubMed] [Google Scholar]
- 9.Paul T, Mruthunjaya M, Shyamsundar A, Naik D, Rajaratnam S, Thomas N. Proceedings at the Society of Endocrinology Conference; 2013. Harrogate, UK: Bioscientifica; 2013. Mar 18-21, Audit of patients referred for DXA scanning at South Asian Tertiary Care Centre. [Google Scholar]


