COUNTRY OVERVIEW
India, with a population of 1.2 billion people, is the second largest emerging economy and second most populated country in the world. Life expectancy is 67 years and is expected to increase to 71 years by 2025 and to 77 years by 2050 [Figure 1].[1] Currently, approximately 10% of India's population (more than 100 million) is aged over 50 years. Based on current patterns of growth, India's population is expected to grow by 16% to reach 1.4 billion by 2025. From 2025 to 2050 the population will increase by a further 34%, reaching 1.88 billion [Figure 2].[1] Those above the age of 50 years will constitute 22% of the population in 2025 and 33% of the population in 2050. With estimates showing that approximately 80% of the urban Indian population is vitamin D deficient[2] and hip fractures occur about a decade earlier than in Western nations[3], osteoporosis is a major concern for this ageing population.
Figure 1.
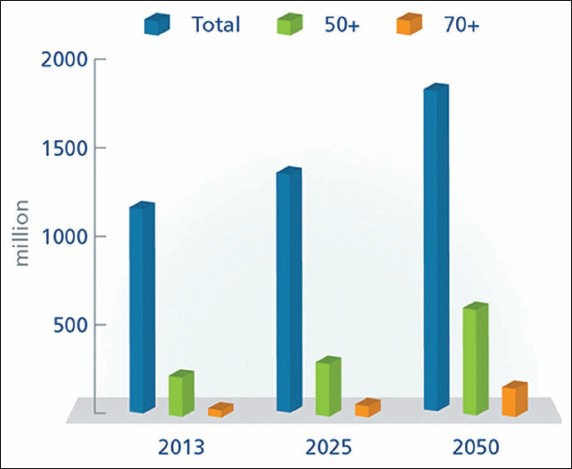
Life expectancy in India
Figure 2.
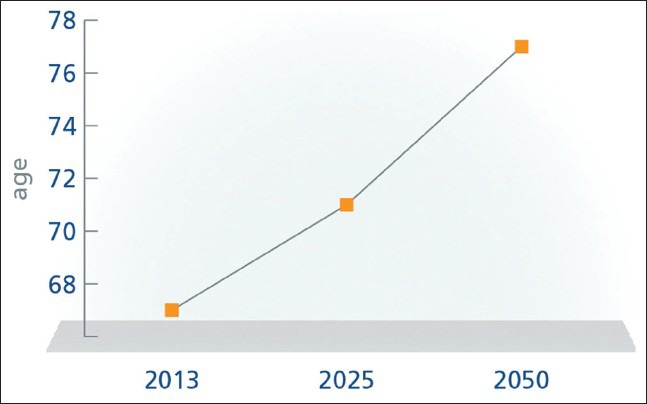
Population projection for India until 2050
State of osteoporosis/osteopenia
In the 2009 International Osteoporosis Foundation (IOF) Asian Audit, expert groups estimated that the number of osteoporosis patients in India was approximately 26 million in 2003, with projections indicating that this would rise to 36 million patients by 2013.[4] Now, in 2013, sources estimate that 50 million people in India are either osteoporotic (T-score lower than -2.5) or have low bone mass (T-score between -1.0 and -2.5).[5]
In a study among Indian women aged 30-60 years from low-income groups, bone mineral density (BMD) at all skeletal sites was much lower than values reported from developed countries, with a high prevalence of osteopenia (52%) and osteoporosis (29%), thought to be due to inadequate nutrition.[6] In a more recent study from Delhi, 792 males and 808 postmenopausal females with a mean age of 57.67 ± 9.46 years were evaluated. Osteoporosis was present in 35.1% of subjects (M-24.6%, F-42.5%) and osteopenia in 49.5% (M-54.3%, F-44.9%).[7] Both of these studies used the manufacturer's White Caucasian reference database.
In an attempt to generate an India-specific database, the Indian Council for Medical Research (ICMR) carried out a large multicenter study, which confirmed data from smaller, single-center studies, and showed that Indians have lower BMD than their North American counterparts.[8] A study involving more than 3,500 subjects carried out at a tertiary care center in South India to study the effect of the newly generated ICMR database (ICMRD) on the diagnosis of osteoporosis reported that a greater proportion were diagnosed as having osteoporosis with Hologic as compared to the ICMR database. Osteoporosis at the spine and hip was present in 42.7% and 11.4% subjects using the Hologic database and in 27.7% and 8.3% subjects using the ICMR database.[9]
Similarly in a study from North India where age-specified BMD reference ranges were established in females between 18-85 years, the prevalence of osteoporosis among women aged older than 50 yearswas significantly higher based on Caucasian T-scores as opposed to using peak BMD/standard deviation values from the population under review at lumbar spine. However, there was no major difference observed at femoral neck.[10]
Reasons ascribed for lower BMD in Indians include possible genetic differences, nutritional deficiency, and smaller skeletal size.[11]
Lifestyle
Widespread vitamin D deficiency has been shown unequivocally across all ages throughout India. More than 80% of urban Indians have serum 25(OH) D levels below 20 ng/mL. This includes pregnant women and their newborns, children and adolescents, young adults, and the elderly. Vitamin D deficiency during childhood and adolescence decreases peak bone mass in adults and may increase the risk of developing osteoporosis.[11] Studies indicate approximately 80-90% of hip fracture patients are vitamin D deficient.[12,13] The high rate of vitamin D deficiency may be due to several causes such as low sun exposure, inadequate dietary vitamin D intake, lack of food fortification with vitamin D, pigmented skin, environmental pollution, and traditional dress code.[4] To combat the low levels of vitamin D a couple of states have recently initiated vitamin D fortification of edible oil and milk fortification, which can be an effective means of delivering vitamin D.[14]
Nutritionally, the Indian population consumes much lower amounts of calcium (300-500 mg/day) than the ideal daily intake.[15] Additionally, tea is a popular beverage consumed by the Indian population; however, due to the high caffeine content, some studies have suggested that it may be associated with a greater risk of hip fracture.[16]
As in other Asian countries, urbanization also appears to be associated with an increase in prevalence of osteoporosis due to lifestyle changes, lower physical activity, increase in indoor living, and lower sun exposure [Figure 3].[17,18]
Figure 3.
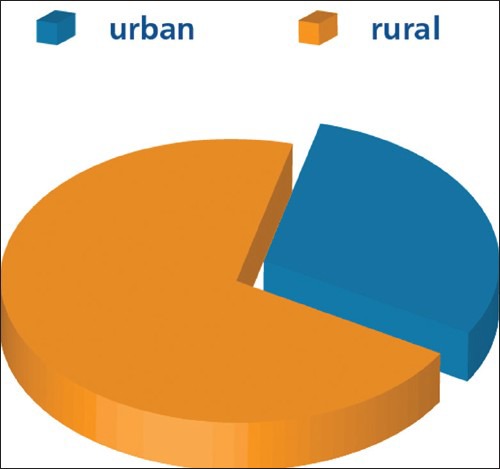
Urban versus rural population in India
Glucocorticoids are taken on a long-term basis by an estimated 1% of the Indian adult population, especially the elderly. This is a contributing factor to osteoporosis in India.[19]
Expatriate Indians also show evidence of poorer bone health than their western counterparts. Experts have found that women from India who have migrated to western countries are at increased risk of accelerated age-related bone loss when compared to their counterparts living in the same geographic region due to their darker skin, dressing habits, and lower bone mass.[20]
Level of awareness
Awareness of osteoporosis is low in India with a number of small-scale surveys indicating that in the urban population approximately 10-15% are familiar with the disease. However, awareness varies widely according to the level of education and those with a family history of the disease. One study reveals that Indians find information about osteoporosis mostly through the television and radio (55%) when compared with family/friends, newspaper, and doctors (approximately 20% each). Unfortunately, information from the media is not always accurate, and with only 20% of information coming from physicians there is a clear need for increased involvement of doctors in educating patients about osteoporosis.[21]
FRACTURE RATES
Hip fracture
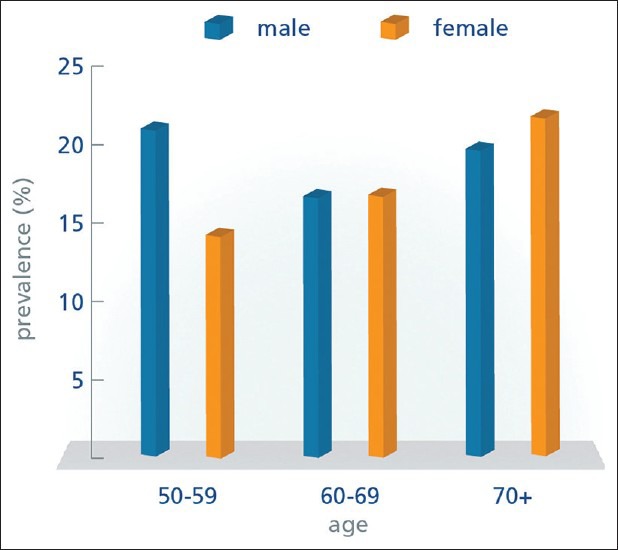
Hospital-based studies suggest that hip fractures are common in India too.[22] A study on expatriate Indians in Singapore showed that hip fracture rates in Indians are somewhat lower than in the Chinese and higher than in Malays.[23] This study has been used to develop the Fracture Risk Assessment Tool (FRAX) model for India. A recent study from Rohtak district in North India shows an annual incidence rate of 163 and 121 per 100,000 per year in women and men, respectively, above the age of 55 years [Figure 4].[24] However, with the rapid increase in the ageing population, an exponential rise is expected in the absolute numbers of fractures in the next decade.[1]
Figure 4.
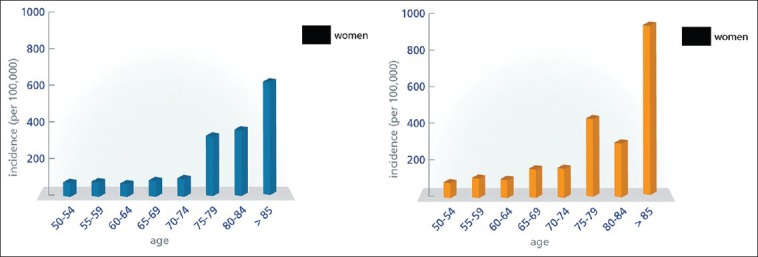
The age- and sex-specific hip fracture incidence in Rohtak district, North India during 2009
SOURCE Dhanwal D.K. et al. (2013) Incidence of hip fracture in Rohtak district, North India
The female preponderance of hip fractures that is observed in western populations is less striking in India.[3,24] In Caucasians, hip fractures are twice as common in women, whereas in India the ratio of hip fractures in women to men is more in the order of 3:2.[24] Additionally, it has been suggested that hip fractures occur at an earlier age in Indians in comparison with western counterparts with the peak age for hip fractures in Indians occurring in their 60s.[3] This may be a function of a shorter life span. Studies of osteoporotic, postmenopausal women in India found that on average, 34% were aged below 60 years.[24] The 1-year mortality after hip fractures is high at over 30% in the public hospital setting.[24]
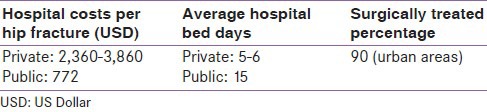
India does not have standardized criteria for the management and treatment of hip fractures, and procedures vary by hospital setting. The Indian Society of Bone and Mineral Research (ISBMR) estimate that 90% or more of hip fractures are managed surgically in urban areas. While the average waiting time for hip surgery is less than one day in private hospitals, Indians often wait over three days for hip surgery in public hospitals where the majority of cases are seen. The proportion of patients undergoing surgery in rural areas is likely to be much lower.
Other fragility fractures
In a large questionnaire-based study involving 14,271 subjects, population prevalence of low trauma fractures at hip, spine, and wrist was 34.3/100,000.[25]
Vertebral fractures
Vertebral fractures are common in Indians, with 15-20% of older urban adults aged over 50 years showing evidence of at least one vertebral fracture. The prevalence of radiographic vertebral fractures in older adults in Delhi has been recently reported to be 17.9% (18.8% male and 17.1% female); indicating that vertebral fracture prevalence in India is similar to Western populations [Figure 5].[26]
Figure 5.
Prevalence of vertebral fractures in males and females according to age strata
SOURCE Marwaha R.K. et al. (2012). The prevalence of and risk factors for radiographic vertebral fractures in older Indian women and men: Delhi Vertebral Osteoporosis Study
COSTS OF FRACTURE
Costs vary according to town, bed type, and whether or not the hospital is governmental, public, or private. In private hospitals, the total cost of hip surgery is between Rs 150,000 to 250,000 (2,360-3,860 USD), and in public hospitals the cost is approximately Rs 50,000 (772 USD) [Table 1]. Private hospitals generally report shorter bed days of 5-6 days than public hospitals where the stay can often be 15 days.
Table 1.
Hip fracture in India: Hospital costs, bed days, and surgically treated percentage
Fracture registries
There are no official fracture registries in India although there could possibly be some at the hospital level.
Fracture liaison services
India does not have any coordinator-based models of care, otherwise known as fracture liaison services (FLS) for secondary fracture prevention. However, at least two hospitals in New Delhi are in the early stages of developing a FLS.
SPECIALISTS RESPONSIBLE FOR OSTEOPOROSIS
The general management of osteoporosis is by orthopaedists and endocrinologists, but other specialities also manage patients, including family doctors, rheumatologists, gynecologists, endocrinologists, geriatricians, rehabilitation specialists, and internal medicine physicians.
There is little osteoporosis-related education at the medical undergraduate level. However, osteoporosis is a recognized component of specialty training for endocrinologists. Various aspects of osteoporosis are also a component of training for orthopaedic surgeons, gynecologists, rheumatologists, and rehabilitation medicine physicians.
GOVERNMENT POLICIES
Osteoporosis as a documented national health priority
Osteoporosis is not a national health priority (NHP) in India. Of the NHPs, the one that will most closely impact osteoporosis is the nutritional program aimed at school children to provide vitamins and minerals including vitamin D and calcium. Although not formally recognized in health programs, vitamin D deficiency is increasingly becoming an important public-health issue, and there is a proposal currently under review for musculoskeletal diseases to be a NHP.
Guidelines
The Indian guidelines on glucocorticoid-induced osteoporosis, ‘Indian Rheumatology Association guidelines for management of glucocorticoid-induced osteoporosis (GIOP)’ were published in 2011 as collaboration between the Indian Rheumatology Association, the Endocrine Society of India, and the Indian Society of Bone and Mineral Research.[27]
Postmenopausal Osteoporosis guidelines are in the process of development jointly by the Endocrine Society of India and ISBMR and are expected to be released in late 2013.
There are numerous initiatives and programmes hosted by ISBMR, promoting osteoporosis awareness and education, such as:
Education programmes and conferences for doctors
Research grants for young investigators awarded annually
Bone densitometry courses
Web-based education on osteoporosis
Printed educational material produced.
Additionally, there are numerous campaigns targeted toward health care providers:
Orthopaedic and gynecologic Initiative
IOF/International Society for Clinical Densitometry (ISCD) courses
Osteoporosis for students
National Bone Health Quiz for medical students organized every few years
Essay competition for nutritionists.
Audit and quality indicator systems in place
Audit and quality indicator systems are not in place in India.
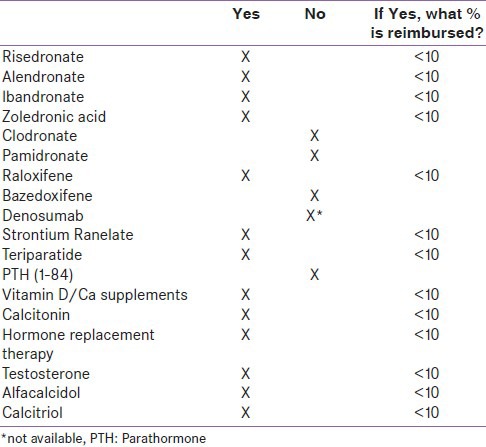
TREATMENT (REIMBURSEMENT OF MEDICATION)
In general, patients pay for treatment directly out of pocket. Health care coverage is limited to less than 10% of users. Those with health insurance (e.g. central government employees, state insurance, or private coverage) are generally only reimbursed for hospital-based services. Outpatient services, including diagnostics and medications, are not commonly reimbursed. This is true for osteoporosis care as well with designated first-line treatments such as bisphosphonates, vitamin D, and calcium, which are paid for by the patients [Table 2]. In cases where reimbursement is available, it is based on the doctor's prescription without any strict regulations. However, “cheaper” generic medications are available and are usually preferred in public/government systems. And, because only hospitalized patients are reimbursed by insurance companies, several doctors prefer to infuse zoledronic acid in the hospital setting. For those who have health care coverage, the chart below summarizes treatment coverage in India.
Table 2.
Treatments available in India and reimbursement levels
DIAGNOSTICS
Most Indian women cannot afford dual-energy X-ray absorptiometry (DXA) due to the costs involved.[28] Like medication treatments, reimbursement is also limited for the diagnoses of osteoporosis. In general, DXA and ultrasound are not reimbursed, and patients pay for scans out of pocket [Table 3]. There are approximately 0.26 DXA machines per 1 million of the general population[29] and very few of these are based at the government hospitals, a fact which further limits access. In the private centers where DXA is available, there is no waiting time for DXA, but again a very small proportion of the population is reimbursed through the private sector.
Table 3.
Diagnostic access and costs in India
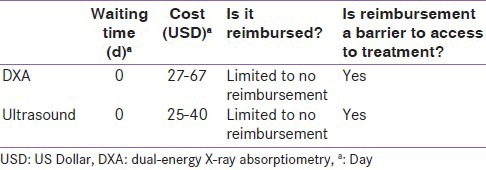
Due to the limited reimbursement for DXA and ultrasound, cost is a barrier to access. In general, DXA costs 27-67 USD. Ultrasound has no waiting time and costs between 25-40 USD.
RECOMMENDATIONS
While there has been considerable progress in research and epidemiology of osteoporosis in India since the last IOF Asian Audit in 2009, numerous gaps still exist. Some of the high priority areas for action over the next 3 years are listed below.
Prevention
Fortification of food with vitamin D needs to be introduced as a universal government program.
Greater emphasis is needed on attainment of peak bone mass/childhood adolescent bone health by nutrition and life style measures. Intensive, sustained, awareness, and intervention programs need to be initiated at the school level.
Treatment
Establishment of reliable, accurate hip fracture registries is urgently needed and is a prerequisite to the improvement of hip fracture care and implementation of secondary prevention strategies.
Introduction of fracture liaison services (FLS) will considerably help secondary fracture prevention efforts.
Research
There is a need for multicenter, large-scale hip fracture incidence studies for which attempts are being made by ISBMR. The validation of a FRAX tool specifically for India would enable better use of diagnostic facilities and improve selection of patients requiring treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Government of India: Ministry of Home Affairs 2011, Office of the Registrar General and Census Commissioner, India. [Last accessed on 2013 Sep 01]. Available from: http://censusindia.gov.in .
- 2.Beloyartseva M, Mithal A, Kaur P, Kalra S, Baruah MP, Mukhopadhyay S, et al. Widespread vitamin D deficiency among Indian health care professionals. Arch Osteoporos. 2012;7:187–92. doi: 10.1007/s11657-012-0096-x. [DOI] [PubMed] [Google Scholar]
- 3.Malhotra N, Mithal A. Osteoporosis in Indians. Indian J Med Res. 2008;127:263–8. [PubMed] [Google Scholar]
- 4.Mithal A, Dhingra V, Lau E. The Asian Audit: Epidemiology, costs and burden of osteoporosis in Asia. Int Osteoporos Foundation. 2009:24–9. [Google Scholar]
- 5.Mithal A, Kaur P. Osteoporosis in Asia: A call to action. Curr Osteoporos Rep. 2012;10:245–7. doi: 10.1007/s11914-012-0114-3. [DOI] [PubMed] [Google Scholar]
- 6.Shatrugna V, Kulkarni B, Kumar PA, Rani KU, Balakrishna N. Bone status of Indian women from a low-income group and its relationship to the nutritional status. Osteoporos Int. 1827:16. doi: 10.1007/s00198-005-1933-1. [DOI] [PubMed] [Google Scholar]
- 7.Marwaha RK, Tandon N, Garg MK, Kanwar R, Narang A, Sastry A, et al. Bone health in healthy Indian population aged 50 years and above. Osteoporos Int. 2011;22:2829. doi: 10.1007/s00198-010-1507-8. [DOI] [PubMed] [Google Scholar]
- 8.New Delhi: ICMR Publication; Published by Director General; 2010. Population based reference standards of peak bone mineral density of Indian males and females: An ICMR multi-center task force study’; pp. 1–24. [Google Scholar]
- 9.Paul T, Asha HS, Mahesh DM, Naik D, Rajaratnam S, Thomas N, et al. The diagnosis of osteoporosis among subjects of southern Indian origin above 50 years of age – The impact of the Indian council of medical research versus Caucasian bone mineral density reference standards Department of Endocrinology, Diabetes and Metabolism, Christian Medical College, Vellore, India. Indian J Endocrinol Metab. 2012;16:S514–24. [Google Scholar]
- 10.Marwaha R, Tandon N, Kaur P, Mani KJ. Establishment of age-specified bone mineral density reference range for Indian females using dual-energy X-ray absorptiometry. J Clin Dens. 2012;15:241. doi: 10.1016/j.jocd.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Shivane V, Sarathi V, Lila A, Bandgar T, Joshi S, Menon P, et al. Peak Bone Mineral Density and Its Determinants in an Asian Indian Population. J Clin Dens. 2012;15:152–8. doi: 10.1016/j.jocd.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Dhanwal DK, Sahoo S, Gautam VK, Saha R. Hip fracture patients in India have vitamin D deficiency and secondary hyperparathyroidism. Osteoporos Int. 2013;24:553–7. doi: 10.1007/s00198-012-1993-y. [DOI] [PubMed] [Google Scholar]
- 13.Khadgawat R, Brar KS, Gahlo M, Yadav CS, Malhotra R, Guptat N, et al. High Prevalence of Vitamin D Deficiency in Asian Indian patients with fragility hip fracture: A pilot study. JAPI. 2010;58:539–42. [PubMed] [Google Scholar]
- 14.Khadgawat R, Marwaha RK, Garg MK, Ramot R, Oberoi AK, Sreenivas V, et al. Impact of vitamin D fortified milk supplementation on vitamin D status of healthy school children. Osteoporos Int. 2013;24:2335–43. doi: 10.1007/s00198-013-2306-9. [DOI] [PubMed] [Google Scholar]
- 15.Shatrugna V, Kulkarni B, Kumar PA, Rani KU, Balakrishna N. Bone status of Indian women from a low-income group and its relationship to the nutritional status. Osteoporos Int. 2005;16:1827. doi: 10.1007/s00198-005-1933-1. [DOI] [PubMed] [Google Scholar]
- 16.Jha R, Mithal A, Malhotra N, Brown E. Pilot case control investigation of risk factors for hip fractures in the urban Indian population. BMC Musculoskeletal Disord. 2010;11:49. doi: 10.1186/1471-2474-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harinarayan CV, Ramalakshmi T, Prasad UV. High Prevalence of low dietary calcium, high phytate consumption and vitamin D deficiency in healthy south Indians. Am J Clin Nutr. 2007;85:1062–7. doi: 10.1093/ajcn/85.4.1062. [DOI] [PubMed] [Google Scholar]
- 18.Rural Population (% Of Total Population) In India 2013. Trading Economics, viewed. 2013. Sep 01, [Last accessed on 2013 Sep 01]. Available from: http://www.tradingeconomics.com/india/rural- population- percent-of-total-population-wb-data.html .
- 19.Saigal R, Mathur V, Prashant RK, Mittal V. Glucocorticoid induced osteoporosis. Indian J Rheumatol. 2006;1:20–6. [Google Scholar]
- 20.Alekel DL, Mortillaro E, Hussain EA, West B, Ahmed N, Peterson CT, et al. Lifestyle and biologic contributors to proximal femur bone mineral density and hip axis length in two distinct ethnic groups of premenopausal women. Osteoporosis Int. 1999;9:327–8. doi: 10.1007/s001980050155. [DOI] [PubMed] [Google Scholar]
- 21.Patil Sapna S, Hasamnis Ameya A, Jena SK, Rashid AK, Narayan KA. Low Awareness of Osteoporosis Among Women Attending an Urban Health Centre in Mumbai, Western India. Malays J Public Health Med. 2010;10:6–13. [Google Scholar]
- 22.Sankaran B. New Delhi: South East Asia Regional Office, World Health Organisation; 2000. Clinical studies: Incidence of fracture neck of femur and intertrochanteric fractures in three Delhi hospitals; pp. 9–18. [Google Scholar]
- 23.Koh LK, Saw SM, Lee JJ, Leong KH, Lee J. Hip fracture Incidence rates in Singapore 1991-1998. Osteoporos Int. 2001;12:311–8. doi: 10.1007/s001980170121. [DOI] [PubMed] [Google Scholar]
- 24.Dhanwal DK, Siwach R, Dixit V, Mithal A, Jameson K, Cooper C. Incidence of hip fracture in Rohtak district, North India. Arch Osteoporos. 2013;8:135–9. doi: 10.1007/s11657-013-0135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tandon N, Mithal A, Anjana RM, Pradeepa R, Deepa M, Mani K, et al. Population prevalence of fragility fractures in India based on a nationwide questionnaire based epidemiological study. Abstract submitted in IOF regionals-2nd Asia-Pacific Osteoporosis and Bone meeting to be conducted by ANZBMS and JSBMR; September 4-8, 2011. Gold Coast Convention and Exhibition Center. 2011 [Google Scholar]
- 26.Marwaha RK, Tandon N, Gupta Y, Bhadra K, Narang A, Mani K, et al. The prevalence of and risk factors for radiographic vertebral fractures in older Indian women and men: Delhi Vertebral Osteoporosis Study (DeVOS) Arch Osteoporos. 2012;7:201–7. doi: 10.1007/s11657-012-0098-8. [DOI] [PubMed] [Google Scholar]
- 27.Krishnamurthy V, Sharma A, Aggarwal A, Kumar U, Amin S, Rao UR, et al. Indian rheumatology association guidelines for management of glucocorticoid-induced osteoporosis. Indian J Rheumatol. 2011;6:68–75. [Google Scholar]
- 28.Aggarwal N, Raveendran A, Khandelwal N, Sen RK, Thakur RS, Dhaliwal LK, et al. Prevalence and related risk factors of osteoporosis in peri- and postmenopausal Indian women. J Midlife Health. 2011;2:81–5. doi: 10.4103/0976-7800.92537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat, World Population Prospects: The 2008 Revision, viewed. 2011. Mar 28, [Last accessed on 2011 Mar 28]. Available from: http://esa.un.org/unpp .


