Abstract
The purpose of this review is to conduct a concise review of the literature to evaluate the knowledge, awareness, and medical practice of Asian Americans/Pacific Islanders (API) supporting the relationship of chronic hepatitis B infection. Liver cancer is the fifth most common cause of cancer death in men and the ninth most common cause of death in women in the United States. On average, Asian Americans are three times more likely to die from liver cancer than other racial/ethnic groups, with Chinese Americans at six times, Koreans eight times and Vietnamese 13 times higher than non-Hispanic Whites. In the United States, about 80% of liver cancer is etiologically associated with hepatitis B virus (HBV) infection. Asian Americans and Pacific Islanders (API) account for over half of the 1.3 million chronic hepatitis B cases and for over half of the deaths resulting from chronic hepatitis B infection. Relevant studies were identified in PubMed (Medline) using the following search structure: (Hepatitis B or synonyms) AND (liver cancer or synonyms) AND (Asian Americans or synonyms). Further studies were identified by citations in retrieved papers and by consultation with experts. Twenty publications were included in this review. Compared to other racial/ethnic groups, Asians, especially those born in China or Southeast Asia, have significantly poorer knowledge regarding hepatitis B and liver cancer. Knowledge, awareness and medical practice among Asian Americans regarding HBV infection were dependent upon age, gender, race/ethnicity, immigrant status and length of residency. Despite increased risk for chronic hepatitis B and liver cancer, many Asian Americans are uninformed, untested, and unprotected against the disease.
Keywords: Knowledge, Awareness and Medical Practice, Hepatitis B, Liver Cancer, Asian Americans, Pacific Islanders
I. INTRODUCTION
Liver cancer is the fifth most common cause of cancer death in men and the ninth most common cause of death in women in the United States (U.S.) (National Cancer Institute, 2008). The National Cancer Institute estimates that there will be 22,620 new cases of liver cancer and 18,160 deaths in 2009. More than 90 percent of all liver cancer cases occur in men and women aged 45 and older. Liver cancer is not a disease of the young : the average age at which a person is diagnosed with liver cancer is 64 years old (American Cancer Society, 2009). After diagnosis, the overall five-year survival rate is less than 10 percent
Liver cancer incidence rates among non-Hispanic whites in the U.S. are 3.7 per 100,000 for males and 1.5 per 100,000 for females (McBride, 2008). The mortality rate from viral hepatitis B for non-Hispanic blacks was 1.6 times higher compared to non-Hispanic Whites (Office of Minority Health, 2011). On average, Asian Americans are three times more likely to die from liver cancer than other racial/ethnic communities, with Chinese Americans at six times, Koreans eight times and Vietnamese 13 times higher than their white counterparts (Hsu et al., 2007). Vietnamese American males have the highest incidence rate of liver cancer in the U.S. (41.8 per 100,000) followed by Hmong American males (25.7 per 100,000). Among women, Korean Americans have the highest incidence rate of liver cancer (10.0 per 100,000) followed by Hmong Americans (8.8 per 100,000) (McBride, 2008).
1. Background
In the U.S., about 80 percent of primary liver cancer (hepatocellular carcinoma, HCC) is etiologically associated with hepatitis B virus (HBV) infection (Juon et al., 2008). Asian Americans and Pacific Islanders (APIs) account for over half of the 1.3 million chronic hepatitis B cases and for over half of the deaths resulting from chronic hepatitis B infection. The disparity in liver cancer incidence and mortality is largely due to the disproportionately high prevalence of chronic HBV infection among Asian Americans (Lang, 2006; Parkin, 2006). As many as 10 percent of API adults in the U.S. are chronically infected with HBV compared to 0.1 percent of White Americans (McBride, 2008), and up to two-thirds of Asian Americans are unaware that they are infected (Hutton et al., 2007).
Asian Americans and Pacific Islanders constitute a growing minority population in the U.S., containing a substantial number of immigrants. Because most (68.9 percent) APIs living in the U.S. are foreign-born, chronic HBV infection represents a serious public health problem (Lavanchy, 2004; Shepard et al., 2006). Chronic HBV infection is defined by the presence of hepatitis B surface antigen (HBsAg) (Nomura et al., 1996) for more than six months (Carey, 2009). Individuals who are positive for HBsAg may also express another antigen that serves as a marker for heightened infectivity, the HB e antigen (HBeAg).
2. Goal and Objectives
The purpose of this review is to conduct a concise review of the literature to evaluate the knowledge, awareness, and medical practice of Asian Americans/Pacific Islanders (API) supporting the relationship of chronic hepatitis B infection and liver cancer. In addition, we will show a known cause of liver cancer. The objectives were as follows: (1) determine the risk factors and modes of transmission for HBV and (2) review the current health education, screening and vaccination activities on changing the knowledge, attitudes, and behaviors of APIs in reducing chronic hepatitis B infection, a known cause of liver cancer.
II. METHODS
1. Search Strategy
Studies on chronic HBV and liver cancer were identified through a systematic search of scholarly databases and reference mining. A comprehensive search of PubMed was used to identify relevant studies meeting the inclusion criteria using the following search terms:
(“hepatitis b”[MeSH Terms] OR “hepatitis b”[All Fields]) AND (“liver neoplasms”[MeSH Terms] OR (“liver”[All Fields] AND “neoplasms”[All Fields]) OR “liver neoplasms”[All Fields] OR (“liver”[All Fields] AND “cancer”[All Fields]) OR “liver cancer”[All Fields]) AND (“asian americans”[MeSH Terms] OR (“asian”[All Fields] AND “americans”[All Fields]) OR “asian americans”[All Fields] OR (“asian”[All Fields] AND “american”[All Fields]) OR “asian american”[All Fields]).
2. Inclusion Criteria
Studies were included if they (i) were published in English in peer-reviewed journals; (ii) studied an API adult population in the United States; (iii) focused on the relationship between chronic hepatitis B infection and liver cancer disease among APIs; and (iv) included vaccination data or vaccination strategy; or (v) included educational intervention that was used to improve knowledge or change the attitude and/or behavior; or (vi) assessed subjects’ knowledge, attitude or behavior of the studied population about HBV and liver cancer both before and after the intervention.
3. Data Extraction
Data extraction of relevant study information for articles meeting inclusion criteria will be performed. For articles referencing previous publications (e.g., describing needs assessments or interventions), the original publication will be retrieved and relevant data summarized. Articles were also identified by reviewing the references of studies that fit the above criteria.
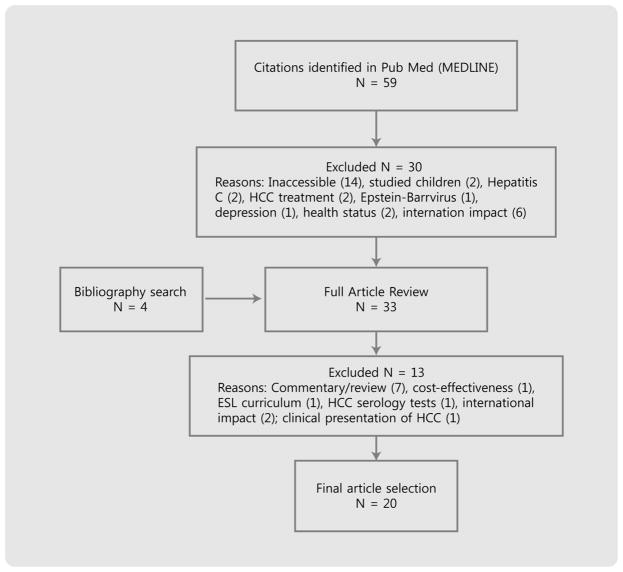
The article selection process is described in Figure 1. My initial PubMed search identified 59 articles. I excluded articles that there were not accessible (14), focused on hepatocellular carcinoma treatment only (2), studied children (2); focused on the Epstein Barr virus (1); focused on hepatitis C (2); focused on depression (1); reviewed health status (2); and those that focused on the international impact of the disease (6). Twenty-nine full-text articles were reviewed and ten studies were excluded. The bibliographic search of included studies yielded 4 additional articles.
Figure 1.
Flowchart of article selection process
4. Data Synthesis
Since a variety of methods were used to obtain the data for the eligible articles, a meta-analysis was not performed. Results of the review are summarized in evidence tables that include major findings and conclusions.
III. RESULTS
A total of 20 studies have been included in this review (Table 1). The articles were published between 2002 and 2009. A variety of host (age at infection, gender, ethnicity, immigrant status, length of residency in the U.S., immune status); viral (viral load, genotype, mutation); and external (concurrent viral infections, alcohol consumption, chemotherapy) factors influence knowledge, awareness and medical practice of Asian Americans in the disease progression of HBV. Despite their increased risk for chronic hepatitis B and liver cancer, many Asian Americans remain uninformed and untested (Chao et al., 2009; Lin et al., 2007; Ma et al., 2007; Nguyen et al., 2007; Taylor et al., 2002; Taylor et al., 2005; Wu et al., 2007).
Table 1.
Characteristics of included articles on HBV risk factors and modes of transmission
| Study | Study Design | Study Population | Sample Size | Age (Mean) | Study Location | Outcome Variables |
|---|---|---|---|---|---|---|
| Taylor et al. (2002) | Randomized control trial design | Cambodian women | 320 | 49 | Seattle | Knowledge Serologic Testing |
| Taylor et al. (2004) | Cross-sectional study | Vietnamese men | 345 | 18–50+ | Seattle | HBV Testing |
| Choe et al. (2005) | Cross-sectional study | Korean immigrants | 30 interviews 18 focus group |
18–64 (47, 52) | Seattle-Tacoma | Beliefs |
| Taylor et al. (2005) | Cross-sectional study | Vietnamese women | 370 | 18–64 | Seattle | Knowledge Serologic Testing |
| Taylor et al. (2005) | Cross-sectional study | Vietnamese men Vietnamese women |
345 370 |
18–64 | Seattle | HBV Awareness, Serologic Testing, Knowledge |
| Coronado et al. (2007) | Cross-sectional study | Chinese men Chinese women |
206 224 |
20–64 | Seattle | Serologic Testing |
| Hsu et al. (2007) | Quasi-experimental | Asian Americans | 807 | 36–45 | Montgomery County, MD | Screening Behavior Serologic Testing |
| Lin et al. (2007) | Cross-sectional study | Asian Americans | 3163 | 18–101 (Median =52.9) | San Francisco Bay Area | Serologic Testing |
| Ma et al. (2007) | Cross-sectional study | Vietnamese | 256 | 18–66+ (41.8) | Greater Philadelphia and New Jersey area | Knowledge, Attitudes, Screening Behavior |
| Wu et al. (2007) | Cross-sectional study | Asian Americans | 199 | 18–60+ (Median 40–59) | San Francisco Bay Area | Knowledge Behavior |
| Chang et al. (2008) | Cross-sectional study | Chinese | 47 | 18–74 | San Francisco | Attitudes |
| Hwang et al. (2008) | Cross-sectional study | Vietnamese men Vietnamese women |
251 | 18+ (18.7 Men) (17.4 Women) | Houston | Knowledge Predictors of HBV |
| Juon et al. (2008) | Cross-sectional study | Korean, Vietnamese, Chinese | 1775 | 1–70+ | Baltimore-Washington area | Screening Behavior Serologic Testing |
| Ma et al. (2008) | Cross-sectional study | Chinese | 429 | 19–66+ (57.1) | New York City | Knowledge, Attitudes, Screening Behavior |
| Nguyen et al. (2009) | Cross-sectional study | Vietnamese | 567 | 45 | San Francisco Bay Area | Genotypes Serologic Testing |
| Grytdal et al. (2009) | Longitudinal study | Cambodian | 2049 | 18–64 | Lowell, MA King County, WA Santa Clara County, CA Los Angeles, Orange Counties, CA | Screening Behavior |
1. HBV Awareness and Knowledge
Compared to other racial/ethnic groups, Asians, especially those born in China or Southeast Asia, have significantly poorer knowledge regarding HBV and liver cancer (Hwang et al., 2008; Wu et al., 2007). In one study, nearly one-half (56 percent) of the Cambodian respondents were not familiar with “the disease or virus called hepatitis B” until it was explained to them in terms of “a liver problem that makes the skin and eyes go yellow” (Taylor et al., 2002). In many of the studies, knowledge and attitudes were assessed by the following: HBV can be transmitted during sexual intercourse with an infected person, from mother to child during childbirth, by sharing toothbrushes with an infected person, by eating food that has been pre-chewed by an infected person, by someone who looks and feels healthy, HBV is more easily spread than AIDS, people with HBV can be infected for life, HBV can cause liver cancer, people can die from HBV, and ethnic group is more likely to get HBV than Whites (Chang et al., 2008; Choe et al., 2005; Coronado et al., 2007; Hsu et al., 2007; Hwang et al., 2008; Juon et al., 2008; Lin et al., 2007; Ma et al., 2007; 2008; Taylor et al., 2002, 2004, 2005; Wu et al., 2007).
The proportion of respondents who had heard of HBV (awareness) varied across Asian subpopulations by race/ethnicity, gender, and age. APIs are more likely to be aware of HBV if they are younger and more educated. Among Cambodian women, the factors associated with having heard of HBV were younger age, higher educational level, younger age at immigration, and having family members who were chronic carriers (Taylor et al., 2002). Those with higher levels of knowledge were more likely to have more years of education, prefer Western medicine for the treatment of liver disease, and have family members chronically infected with HBV (Taylor et al., 2002). In the Vietnamese population, the age of the study participant determined whether they were more likely to have heard of HBV or receive the vaccination (Hwang et al., 2008; Taylor et al., 2005). In a study of adults aged 18 to 50-plus in Seattle, older Vietnamese adults were more likely to have heard of hepatitis B than younger individuals (Taylor et al., 2005).
Gender and education were significantly associated with HBV awareness (Taylor et al., 2005). Lower levels of education were associated with lower levels of HBV knowledge and serologic testing among Cambodians (Taylor et al, 2002). In the Taylor et al. study (2005), women were significantly more likely to have heard of HBV than men (76 percent, p = 0.002). Women were significantly less educated (p < 0.001), more likely to have immigrated recently (p < 0.001), and less likely to speak English fluently or well (p < 0.001) than males (Taylor et al., 2005). Among Vietnamese college students, those who had undergone screening, vaccination or had a family member with HBV or liver disease had significantly higher levels of HBV knowledge (Hwang et al., 2008). Only 29.9 percent knew that Asian Americans are at high risk for HBV and that hepatitis B can be cured (33.9 percent) (Hwang et al., 2008). However, a large proportion of the college students knew that hepatitis B can impair liver function (81.3 percent) and increase the risk of liver cancer (70.1 percent). They also knew that hepatitis B could be prevented by vaccination (80.5 percent) and avoiding infected needles (73.3 percent). According to Hwang et al. (2008), those with higher knowledge scores were more likely to have received HBV vaccination (OR = 1.11, 95% CI = 1.01–1.21).
According to a study by Ma et al. (2007), 46.3 percent of the Vietnamese Americans sampled in the greater Philadelphia and New Jersey area had heard of HBV or knew about the availability of screening (32.6 percent) or vaccination (35.5 percent). The mean age of the participants was 41.8 years and 55.1 percent had a high school education. A majority of the participants was born outside the U.S. (95.7 percent) and lived in the U.S. for an average of 11 years (Ma et al., 2007). One-third of participants thought that cancer was beyond their control (60.6 percent); over half did not know that cancer was curable (59.2 percent) or that it could be prevented (58.8 percent). Close to half of the participants (46.3 percent) had no knowledge about HBV; and about a third were aware of the existence of a screening test for HBV (32.6%) and vaccination (35.5 percent). The majority thought that HBV could be transmitted through sharing food plates with a carrier (59.9 percent), sharing or using needles (49.6 percent), from mother to child during birth (62 percent), or sharing toothbrushes (41.6 percent) (Ma et al., 2007). However, 70.5 percent felt that getting vaccinated would prevent HBV.
2. HBV Screening and Vaccinations
Most Asian Americans do not have a usual source of care. Only one in five Asian Americans aged 18 to 64 report not having health insurance or being uninsured at some point in the past year (Asian American Health Initiative, 2005). In one study, a substantial proportion (44.1 percent) had not received an annual check-up (Ma et al., 2007). Fewer than 60 percent of Asian Americans have been tested for HBV and only 44 percent have had their children vaccinated (Wu et al., 2007).
Because many Asian Americans are not serologically tested for HBV, many APIs are unprotected (Juon et al., 2008, Lin et al., 2007; Wu et al., 2007). Having a regular source of care, physician recommendation, and knowing HBV can be spread during childbirth increased the odds of getting tested and vaccinated against HBV (Taylor et al., 2004). Most APIs have not undergone hepatitis B testing or vaccination because their providers have not recommended these procedures to them (Choe et al., 2006; Ma et al., 2007; Taylor et al., 2002; 2004; 2006; 2009; Wu et al., 2007). Compared to those who did not receive a recommendation for HBV testing, Vietnamese women who received a recommendation for testing had nearly a five times higher odds of testing (Taylor et al., 2005). According to Chang, Nguyen & So (2008), the primary motivations for hepatitis B vaccination were protection of future health and avoidance of hepatitis B. Those with higher levels of knowledge were more likely to have received the vaccine (Hwang et al., 2008). However, factors that discouraged them from testing or vaccination included costs, lack of health insurance, fear of side effects, worries about reliability or efficacy, poor patient-doctor communication, reliance on professional opinion, apparent good health, inconvenience, and personal preference (Chang et al., 2008).
Asian Americans face cultural and linguistic barriers that may discourage or prevent them from accessing health care services that can help them get screened and vaccinated for HBV. Asian Americans deal with illness and disease very differently than the general population. For example, 38 percent of the Chinese participants thought that HBV infection could be prevented by taking Chinese medicines (Coronado et al., 2007). Slightly more than half believed that HBV could be prevented with a positive attitude (Coronado et al., 2007).
Approximately 1 in 10 foreign-born Asian adults living in the United States is chronically infected with HBV (Chang et al., 2009; Hsu et al., 2007; Lin et al., 2007). Many of the study participants in the reviewed articles were born outside of the U.S. (>90%) (Chang et al., 2008; Coronado et al., 2007; Grytdal et al., 2009; Ma et al, 2007; Ma et al., 2008; Taylor et al, 2006). Of those who were born outside of the U.S., the average length of residency in the U.S. ranged from 10 to 19 years (Chang et al., 2008; Coronado et al., 2007; Grytdal et al., 2009; Ma et al., 2007; Ma et al., 2008, Taylor et al, 2005, 2006). Hsu et al. (2007) found that infection rates increased by the length of U.S. residency. In addition, the length of residency in the U.S. affects HBV vaccination (Hwang et al., 2008). For example, Vietnamese college students who are less acculturated (determined by higher Vietnamese language skills) were less likely to have received HBV vaccination (Hwang et al., 2008).
There are many factors that motivate Asian Americans to get tested and vaccinated. Vietnamese- and Cambodian-American respondents who were born in the US, younger, and had at least some college education were more likely to have been vaccinated against hepatitis B (Grytdal et al., 2009; Hwang et al., 2008). The factors that motivated Chinese men and women to be tested for hepatitis B included peace of mind, prevention of transmission to others, informed decision-making, convenience, and pre-vaccination screening (Chang et al., 2008). The factors associated (p < 0.01) with ever having tested included believing that Chinese were more likely than Whites to get HBV (p = 0.004), having a doctor recommend testing (p < 0.001), asking a doctor for the test (p < 0.001) and not needing an interpreter for doctors visits (p = 0.002) (Coronado et al., 2007).
Compared to other Asian subpopulations, Cambodian immigrants have lower levels of HBV knowledge, serologic testing, and vaccination. (Taylor et al, 2002). Cambodian-Americans were less likely than Vietnamese-Americans to have been tested for HBV. Of those who had been tested and thought they were susceptible, two-thirds (67 percent) had not been vaccinated. Less than one-quarter (23 percent) of the study group thought that asymptomatic individuals can transmit the disease to others. Most thought that HBV infection can cause liver cancer (54 percent) and death (72 percent). However, a minority thought that infection can be lifelong (24 percent) and incurable (15 percent). Ninety percent thought liver disease should be treated with Western medicine and 8 percent reported that they had family members chronically infected with HBV.
Ma et al (2007) report that 74.6 percent of the Vietnamese Americans surveyed have received at least one general health check-up in the U.S. while 86.5 percent have received at least one general health check-up in their lifetime. For Vietnamese women, the factors associated with previous HBV testing are being aware that HBV can spread during childbirth, during sexual intercourse, and by sharing toothbrushes; doctors had recommended testing or family members or friends had suggested testing; and family members were chronically infected with HBV (Taylor et al., 2005). For Vietnamese men, the factors for previous HBV testing included older age, a short proportion of life in the U.S., low English fluency, private health insurance, identifying a regular source of medical care, reporting no long waits for medical appointments, and having access to interpreter services (Choe et al., 2006). In the Taylor et al. study (2004), the factors associated with previous testing included having a regular source of care and regular provider, knowing that HBV can be spread during childbirth, believing HBV can cause liver cancer, and doctor(s) had recommended testing as well as had asked doctor(s) for testing (P < 0.01). Vietnamese American college students who were less acculturated (as shown by greater fluency in written and spoken Vietnamese) were less likely to have received HBV vaccination (Hwang et al., 2008). Additionally, students who had been around others with HBV (OR = 0.40, 95% CI = 0.18–0.86) were less likely to have received the vaccine (Hwang, Huang & Yi, 2008).
3. HBV Modes of Transmission
Because of the poor knowledge about hepatitis B, there are many misconceptions about the transmission of the disease (Choe et al., 2005, 2006; Hwang et al., 2008; Ma et al., 2007; Taylor et al., 2002, 2005, 2006; Wu et al., 2007). Although the majority of Asian American adults in the San Francisco Bay Area had at least a college education, they lacked knowledge regarding HBV transmission, prevention, symptoms, risks, and occurrence (Wu et al., 2007).
There are viral factors that can influence the disease progression. In one study, Vietnamese patients with CHB in San Francisco were nearly three times more likely to carry HBV genotype B than genotype C (74 percent and 25 percent) while Chinese patents were nearly as likely to have genotype C as genotype B (55 percent and 43 percent, P = 0.001) (Nguyen et al. 2009). In another study, those with higher knowledge levels were significantly more likely to have been tested, vaccinated, and to have had their children vaccinated for HBV (Hwang et al., 2008).
APIs are unaware that chronic hepatitis B is usually asymptomatic or that sexual intercourse with an infected person can result in hepatitis B (Ma et al., 2007; Taylor et al., 2002, Wu et al., 2007). Only 22.6% of the Vietnamese respondents were aware that HBV was transmitted through sexual intercourse (Ma et al., 2007). In addition, less than one-third were able to correctly identify the actual modes of transmission and over half falsely believed that hepatitis B could be transmitted through contaminated or improperly cooked food (Ma et al., 2007). As a result, many APIs are afraid to share meals with chronically infected individuals. Finally, less than one-quarter of those surveyed thought that hepatitis B infection was a lifelong disease or was incurable (Taylor et al, 2002). While Koreans in Western Washington were more aware of hepatitis B, their personal beliefs about transmission and prevention were more applicable to other forms of hepatitis (Choe et al., 2005).
In the Taylor et al. study (2005), over three-quarters of all Vietnamese survey participants knew that hepatitis B can be spread during childbirth (83 percent) and by someone who looks and feels healthy (78 percent). Between one-half and three-quarters knew that HBV can be spread by eating food that has been pre-chewed by an infected person (71 percent), is not spread by holding hands (75 percent), can be spread during sexual intercourse (69 percent), can be spread by sharing toothbrushes (72 percent), can be spread by sharing razors (63%), and can be spread by lancet therapy (66 percent). Less than one-half knew that hepatitis B is not spread by eating food that has been prepared by an infected person (36 percent), nor by coughing (31 percent), and is more easily spread than AIDS (19 percent). Men were more likely than women to know that hepatitis B is not spread by eating food that has been prepared by an infected person (p < 0.001), coughing (p < 0.001), and holding hands (p = 0.035); and HBV can be spread by someone that looks and feels healthy (p = 0.019) (Taylor et al., 2005). In contrast, women were more likely to know that HBV can be spread by eating food that has been pre-chewed by an infected person (p = 0.001), sharing toothbrushes (p = 0.003), and sharing razors (p = 0.014) (Taylor et al., 2005).
4. Current and Emerging Interventions
To address the screening and vaccination problems with hepatitis B, several campaigns are under way. The San Francisco Hep B Free Campaign, one of the best known programs, aims to make San Francisco the first HBV-free city in the U.S. (McBride, 2008). San Francisco has the highest rate of liver cancer rates in the country. The plan is to screen, vaccinate, and treat all of San Francisco’s Asian and Pacific Islander residents who make up about a third of the city’s population for HBV (McBride, 2008). The campaign hopes to promote routine blood tests for HBV in the Asian and Pacific Islander community, making sure the results get to the city’s health department; improve referrals and access to care for people with chronic HBV; increase the number of San Francisco hospitals that offer low-cost or free screening and vaccinations for HBV; and educate physicians about the need for lifelong management of patients with chronic HBV (McBride, 2008).
The Asian American Network for Cancer Awareness, Research, and Training (AANCART) is another campaign that hopes to increase the proportion of Asian American adults who are tested for HBV infection (McBride, 2008). The investigators are currently concentrating on the three groups who face a particularly higher burden of the disease, Vietnamese, Hmong, and Korean Americans, living in three California cities.
The 3 For Life program was launched in September 2004 by the San Francisco Department of Public Health and Stanford University’s Asian Liver Center to increase HBV awareness and reduce the high prevalence of undiagnosed chronic HBV infection and susceptibility among API adults (Chang et al., 2009). This pilot program targeted primarily foreign-born Chinese adults and offered low-cost HBV vaccination with free HBV testing. Over the course of a year, semimonthly screening and vaccination clinics were held. A total of 1206 adults between the ages of 18 and 87 (median = 46 years) used the program. Participants paid a discounted fee for a full vaccine series against HBV, hepatitis A virus, or both. Participants also provided blood samples for HBV testing and received the results in the mail. Of the 1106 adults who were screened for HBsAg and anti-HB, nine percent of adults were chronically infected with HBV and 53 percent were unprotected. Eighty-five percent of the unprotected adults completed the HBV vaccine series. The probability of completing a recommended vaccine series was similar across most sociodemographic groups with slightly higher completion rates among middle-aged between the ages of 40 and 50 and Chinese participants.
The Jade Ribbon Campaign is a culturally targeted, community-based outreach program to promote the prevention, early detection, and management of chronic hepatitis B virus infection and liver cancer among Asian Americans (Chao et al., 2009). At a HBV screening clinic and educational seminar in 2001, 476 Chinese American adults from the San Francisco Bay Area attended. The prevalence of chronic HBV infection was 13 percent with only 8 percent of participants showing serologic evidence of protective antibody from prior vaccination. The prevalence was higher in men than in women. In addition, the prevalence of HBcAb seropositivity increased with age. Before the clinic, participants reported low preventive action, but after one year, 67 percent of those with chronic HBV infection had consulted a physician for liver cancer screening, and 78 percent of all participants had encouraged family members to be tested for HBV (Chao et al., 2009).
IV. CONCLUSIONS
Hepatitis B is a highly resilient virus that can be prevented through effective screening and vaccination efforts. Knowledge, awareness and medical practice among Asian Americans regarding HBV were dependent upon age, gender, race/ethnicity, immigrant status and length of residency. In comparison to other race/ethnic groups, Asian American men are at a greater risk of developing the disease. Asian Americans who were infected with HBV as an infant and/or have a family history of liver cancer are at a greater risk of developing the disease than those who are infected late in life. In terms of immigrant status and residential history, foreign-born Asian Americans are more likely to be HBV carriers and less likely to be vaccinated against the disease. Infection rates among immigrants are increased by the length of U.S. residency. Most APIs have not undergone hepatitis B testing or vaccination, and many health care providers do not routinely recommend these procedures to their API patients. Patients with HBV genotype B are more likely to develop liver cancer because they are more likely to undergo seroconversion of hepatitis B e antigen at an earlier and higher rate. In addition, chronic hepatitis B infection increases the risk of developing liver cancer later in life.
Despite increased risk for chronic hepatitis B and liver cancer, many Asian Americans are uninformed, untested, and unprotected against the disease. Even though they tend to be more educated, they have poor knowledge about the disease and have misconceptions about the transmission of the disease. Although there is general awareness of HBV, there are serious gaps in knowledge that may be attributed to poor English language proficiency, ineffective health communication in communities, physical and psychological barriers, and culture that prevent the exchange of information on intimate subjects, such as sex.
As shown, there have been numerous studies conducted to increase hepatitis B and liver cancer awareness and prevention among specific APIs. This review adds to the current literature. First, it looks at the epidemiological evidence that has been collected among the highest risk adult groups. Previously, a large amount of immunization programs has been focused on Asian American children with very few studies on adult Asian Americans. Second, it documents the risk factors and modes of transmission for HBV for specific Asian subpopulations. Asian Americans are a heterogeneous group with respect to demographic factors and health risk factors. They are composed of multiple racial, ethnic, gender, and cultural identities. Last, it evaluates the current interventions that will aid in the prevention and detection of HBV to lower the risk of liver cancer of APIs.
There were several limitations in this review. First, it was limited by the data collection methods used by the original researchers. In one study, the researchers were only able to collect data from 6 out of the nine study sites due to lack of computer knowledge among volunteers and lack of time for screening administrators to record the data. Second, some of the studies had small sample sizes. Both the quantity and quality of these data need to be improved with respect to appropriate gender and ethnic group representation. APIs are also usually underrepresented in current surveillance studies leading to the underestimation of the true number of infected individuals. Last, the studies focused on particular groups. Hence, making it only generalizable to the particular population studied.
HBV is a serious public health problem in the United States. Efforts to reduce the HBV in APIs will improve the health of everyone. To substantially improve knowledge of preventing the disease in the Asian communities, HBV programs should be culturally tailored. Health education programs for immigrant populations should be based on a thorough understanding of the target population’s knowledge, awareness, and health medical practice. It is important that the development and implementation of future community-based interventions focus on education, vaccination, screening, and early detection of HBV. An effective model program must include screening tests to determine immunization status, vaccination strategy for lifetime protection, an educational component culturally tailored to the population, and pre and post assessments to test knowledge. In addition, proper monitoring and treatment of chronic HBV infection are necessary in order to reduce the number of deaths from liver disease among those with undetected chronic infection.
Contributor Information
ThuyQuynh N. Do, University of Texas Medical Branch
Sanggon Nam, University of Texas Medical Branch.
References
- American Cancer Society. What Are The Key Statistics About Liver Cancer? 2009 Retrieved Oct. 9, 2009, from http://www.cancer.org/docroot/CRI/content/CRI_2_4_1X_What_are_the_key_statistics_for_liver_cancer_25.asp.
- Asian American Health Initiative. 2005 Retrieved Dec. 7, 2009, from http://www.aahiinfo.org/english/asianAmericans.php.
- Carey WD. The prevalence and natural history of hepatitis B in the 21st century. Cleve Clin J Med. 2009;76(Suppl 3):2–5. doi: 10.3949/ccjm.76.s3.01. [DOI] [PubMed] [Google Scholar]
- Chang ET, Keegan TH, Gomez SL, Le GM, Clarke CA, So SK, Glaser SL. The burden of liver cancer in Asians and Pacific Islanders in the Greater San Francisco Bay Area, 1990 through 2004. Cancer. 2007;109(10):2100–2108. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang ET, Nguyen BH, So SK. Attitudes toward hepatitis B and liver cancer prevention among Chinese Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2008;9(4):605–613. [PubMed] [Google Scholar]
- Chang ET, Sue E, Zola J, So SK. 3 For Life: a model pilot program to prevent hepatitis B virus infection and liver cancer in Asian and Pacific Islander Americans. Am J Health Promot. 2009;23(3):176–181. doi: 10.4278/ajhp.071025115. [DOI] [PubMed] [Google Scholar]
- Chao SD, Chang ET, So SK. Eliminating the threat of chronic hepatitis B in the Asian and Pacific Islander community: a call to action. Asian Pac J Cancer Prev. 2009;10(3):507–512. [PubMed] [Google Scholar]
- Choe JH, Taylor VM, Yusui Y, et al. Health care access and sociodemographic factors associated with hepatitis B testing in Vietnamese American men. J Immigr Minor Health. 2006;8:193–201. doi: 10.1007/s10903-006-9322-1. [DOI] [PubMed] [Google Scholar]
- Choe JH, Chan N, Do HH, Woodall E, Lim E, Taylor VM. Hepatitis B and liver cancer beliefs among Korean immigrants in western Washington: report of a qualitative study. Cancer. 2005;104(Suppl 12):2955–2988. doi: 10.1002/cncr.21518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronado GD, Taylor VM, Tu SP, Yasui Y, Acorda E, Woodall E, Yip MP, Li L, Hislop TG. Correlates of hepatitis B testing among Chinese Americans. J Community Health. 2007;32(6):379–390. doi: 10.1007/s10900-007-9060-x. [DOI] [PubMed] [Google Scholar]
- Do S. The natural history of hepatitis B in Asian Americans. Asian American and Pacific Islander Journal of Health. 2001;9(2):141–153. [PubMed] [Google Scholar]
- Grytdal SP, Liao Y, Chen R, Garvin CC, Grigg-Saito D, Kagawa-Singer M, Liang S, McPhee SJ, Nguyen TT, Tran JH, Gallagher KM. Hepatitis B testing and vaccination among Vietnamese- and Cambodian-Americans. J Community Health. 2009;34(3):173–180. doi: 10.1007/s10900-008-9141-5. [DOI] [PubMed] [Google Scholar]
- Hann HL. Hepatocellular carcinoma in Asian Americans. Cancer. 1998;83(Suppl 8):1723–1729. [Google Scholar]
- Hsu CE, Liu LC, Juon HS, Chiu YW, Bawa J, Tillman U, Li M, Miller J, Wang M. Reducing liver cancer disparities: a community-based hepatitis-B prevention program for Asian-American communities. J Natl Med Assoc. 2007;99(8):900–907. [PMC free article] [PubMed] [Google Scholar]
- Hutton DW, Tan D, So SK, Brandeau ML. Cost-effectiveness of screening and vaccinating Asian and Pacific Islander adults for hepatitis B. Ann Intern Med. 2007;147(7):460–469. doi: 10.7326/0003-4819-147-7-200710020-00004. [DOI] [PubMed] [Google Scholar]
- Hwang JP, Huang CH, Yi JK. Knowledge about hepatitis B and predictors of hepatitis B vaccination among Vietnamese American college students. J Am Coll Health. 2008;56(4):377–382. doi: 10.3200/JACH.56.44.377-382. [DOI] [PubMed] [Google Scholar]
- Juon H, Strong C, Oh TH, Castillo T, Tsai G, Oh LDH. Public health model for prevention of liver cancer among Asian Americans. J Community Health. 2008;33(4):199–205. doi: 10.1007/s10900-008-9091-y. [DOI] [PubMed] [Google Scholar]
- Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11(2):97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- Lang L. CDC points to higher prevalence of chronic HBV infection among Asian/Pacific Islanders. Gastroenterology. 2006;131(1):7. [Google Scholar]
- Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: A cross-sectional study of Asians in California. Hepatology. 2007;46(4):1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Fang C, Feng Z, Parameswaran L, Pham A, Khanh C. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. J Health Care Poor Underserved. 2007;18(1):62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Toubbeh JI, Tan Y, Wu D. Knowledge, attitudes, and behaviors of Chinese hepatitis B screening and vaccination. Am J Health Behav. 2008;32(2):178–187. doi: 10.5555/ajhb.2008.32.2.178. [DOI] [PubMed] [Google Scholar]
- McBride G. Hepatitis B virus-induced liver cancer in Asian Americans: a preventable disease. J Natl Cancer Inst. 2008;100(8):528–529. doi: 10.1093/jnci/djn120. [DOI] [PubMed] [Google Scholar]
- Nguyen TT, Taylor V, Chen MS, Jr, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge, and screening among Asian Americans. J Cancer Educ. 2007;22(4):266–272. doi: 10.1007/BF03174128. [DOI] [PubMed] [Google Scholar]
- Nguyen LH, Ha NB, Vutien P, Ha NB, Garcia RT, Trinh HN, Nguyen HA, Nguyen KK, Keefe EB, Nguyen MH. Prevalence of hepatitis B virus genotype B in Vietnamese patients with chronic hepatitis B. Hepatol Int. 2009;3:461–467. doi: 10.1007/s12072-009-9141-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura A, Stemmermann GN, Chyou PH, Tabor E. Hepatitis B and C virus serologies among Japanese Americans with hepatocellular carcinoma. J Infect Dis. 1996;173(6):1474–1476. doi: 10.1093/infdis/173.6.1474. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health. Hepatitis and African Americans. 2011 Retrieved from http://minorityhealth.hhs.gov/templates/content.aspx?ID=6493.
- Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030–3044. doi: 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- Shepard CW, Simard EP, Finelli L, Fiore AE, Bell BP. Hepatitis B virus infection: epidemiology and vaccination. Epidemiol Rev. 2006;28:112–125. doi: 10.1093/epirev/mxj009. [DOI] [PubMed] [Google Scholar]
- Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing and knowledge among Vietnamese American men and women. J Community Health. 2005;30(6):477–490. doi: 10.1007/s10900-005-7282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Jackson JC, Chan N, Kuniyuki A, Yasui Y. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. J Community Health. 2002;27(3):151–163. doi: 10.1023/a:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Seng P, Acorda E, Sawn L, Li L. Hepatitis B knowledge and practices among Cambodian immigrants. J Cancer Educ. 2009;24(2):100–104. doi: 10.1080/08858190802664750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Tu SP, Woodall E, Acorda E, Chen H, Choe J, Li L, Yasui Y, Hislop TG. Hepatitis B knowledge and practices among Chinese immigrants to the United States. Asian Pac J Cancer Prev. 2006;7(2):313–317. [PubMed] [Google Scholar]
- Taylor VM, Yasui Y, Burke N, Choe JH, Acorda E, Jackson JC. Hepatitis B awareness, testing and knowledge among Vietnamese American women. Ethnicity & Disease. 2005;15:761–767. [PubMed] [Google Scholar]
- Taylor VM, Yasui T, Burke N, Nguyen T, Chen A, Acorda E, Choe JH, Jackson JC. Hepatitis B tesing among Vietnamese American men. Cancer Detect Prev. 2004;28(3):170–177. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2007;8(1):127–134. [PubMed] [Google Scholar]
- Yu MC, Yuan J, Lu SC. Alcohol, cofactors and the genetics of hepatocellular carcinoma. J Gastroenterol Hepatol. 2008;23(Suppl 1):92–97. doi: 10.1111/j.1440-1746.2007.05293.x. [DOI] [PMC free article] [PubMed] [Google Scholar]