ABSTRACT
BACKGROUND
Older adults are encouraged to walk ≥100 steps∙minute−1 for moderate-intensity physical activity (i.e., brisk walking). It is unknown if the ability to walk ≥100 steps∙minute−1 predicts mortality.
OBJECTIVE
To determine if the ability to walk ≥100 steps∙minute−1 predicts mortality among older adults.
DESIGN, SETTING, AND PATIENTS
A population-based cohort study among 5,000 older adults from the Third National Health and Nutrition Survey (NHANES III; 1988–1994). Vital status and cause of death were collected through December 31, 2006. Median follow-up was 13.4 years. Average participant age was 70.6 years.
MEASUREMENTS
Walking cadence (steps∙minute−1) was calculated using a timed 2.4-m walk. Walking cadence was dichotomized at 100 steps∙minute−1 (≥100 steps∙minute−1 versus <100 steps∙minute−1) to demarcate the lower threshold of absolutely defined moderate-intensity physical activity. Walking cadence was also analyzed as a continuous variable. Predicted survival was compared between walking cadence and gait speed. The primary outcome was all-cause mortality. Secondary outcomes included cardiovascular-specific and cancer-specific mortality and mortality from other causes.
RESULTS
Among 5,000 participants, 3,039 (61 %) walked ≥100 steps∙minute−1. During follow-up, 3,171 subjects died. In multivariable-adjusted analysis, ability to walk ≥100 steps∙minute−1 predicted a 21 % reduction in all-cause mortality (hazard ratio [HR], 0.79; 95 % confidence interval [95 % CI], 0.71–0.89, p < 0.001). Each ten-step increase in walking cadence predicted a 4 % reduction in all-cause mortality (HR, 0.96, [0.94–0.98], p < 0.001). In secondary analyses, ability to walk ≥100 steps∙minute−1 predicted reductions in cardiovascular-specific mortality (HR, 0.79 [0.67–0.92], p = 0.002), cancer-specific mortality (HR, 0.76 [0.58–0.99], p = 0.050), and mortality from other causes (HR, 0.82 [0.68–0.97], p = 0.025). Predicted survival, adjusted for age and sex, was not different using walking cadence versus gait speed.
LIMITATIONS
Walking cadence was a cross-sectional measurement.
CONCLUSIONS
The ability to walk ≥100 steps∙minute−1 predicts a reduction in mortality among a sample of community-dwelling older adults.
KEY WORDS: physical function, disability, mobility, aging, physical activity
INTRODUCTION
Preservation of physical health among older adults (age ≥ 60), the fastest growing segment of the US population,1,2 is an important public health objective.3–5 The loss of physical function among older adults confers an increased risk of premature mortality,6,7 while physical activity preserves physical function and can reduce and delay morbidity and premature mortality.8–11 The American College of Sports Medicine (ACSM) recommends older adults participate in 150-min per week of moderate-intensity aerobic activity, such as brisk walking.8 Walking is increasingly acknowledged as a highly efficacious and safe modality of physical activity for older adults.8,12 It has been recommended that ≥100 steps∙minute−1 is a walking cadence consistent with moderate-intensity physical activity13 and is appropriate for older adults.12 The use of walking cadence as a method to monitor the intensity of physical activity among older adults is intuitive, economical, and encourages the use of pedometers,14,15 which have been successfully used to promote physical activity in clinical practice.16–18
Despite the use of walking cadence to quantify intensity of physical activity, it is unknown whether walking cadence could be additionally leveraged as an objective measure of physical function to prognosticate mortality. Specifically, it is unknown whether the ability to walk ≥100 steps∙minute−1 distinguishes older adults at risk for premature mortality. Furthermore, it is unknown how walking cadence predicts mortality relative to established physical function metrics such as gait speed.19 Establishing the relationship between walking cadence and mortality may help clinicians convey the prognostic importance of physical function to patients using a metric that is readily understood by older adults.14 Such metrics may empower motivated older adults with the ability to self-monitor their physical function longitudinally.
We sought to explore the hypothesis that objectively measured walking cadence distinguishes older adults at risk for premature mortality. We hypothesized that the ability to walk ≥100 steps∙minute−1 would predict mortality among a population-based sample of community-dwelling older adults. We also sought to quantify and describe the dose-response relationship between walking cadence as a continuous measure with risk of premature mortality. Lastly, we compared the accuracy of walking cadence to predict 5- and 10-year mortality relative to gait speed, which is a validated prognostic marker of physical function.19
METHODS
Study Population and Design
The Third National Health and Nutrition Examination Survey, 1988–1994 (NHANES III) was a stratified multistage study designed to provide health information on a nationally representative sample of US civilians.20 Participants aged ≥60 years were invited to complete a physical performance evaluation.6,21 The physical performance evaluation was administered to 5,403 individuals, of which 5,000 (93 %) completed the requisite measures for this analysis.21 Participants provided written informed consent prior to completing any study-related activities.
Walking Cadence
Walking cadence was assessed using a 2.4-m walk. Participants were instructed to complete the walk at a pace twice that of their usual walking speed.21 Time required to complete the course was recorded to the nearest tenth of a second using a stopwatch. The number of steps required to complete the course was recorded to the nearest whole number by the study technician. Walking cadence (i.e., steps∙minute−1) was calculated as:
 |
Mortality Outcome
Vital status and cause of death were identified using the National Death Index (NDI) database through December 31, 2006. Participants were linked to the NDI database using probabilistic matching that included 12 identifiers such as Social Security number, sex, and date of birth.22 Cause of death was categorized using the International Classification of Diseases 10th edition (ICD-10).23 Cardiovascular-specific mortality was categorized using ICD-10 codes I00–I078. Cancer-specific mortality was categorized using ICD-10 codes C00–C97. Mortality from other causes included deaths not classified as cardiovascular specific or cancer specific.
Covariates
With the exception of body mass index (BMI), which was calculated using measured height and weight (kilograms/meters2), all other covariates (see Table 1) were collected by self-report using standardized questionnaires.20
Table 1.
Characteristics of the Study Sample
| Characteristic | Overall [mean (SE) or n (%)] | Died during follow-up | P-value | |
|---|---|---|---|---|
| Yes (n = 3,171) | No (n = 1,829) | |||
| Age, years | 70.6 (0.13) | 73.6 (0.18) | 66.8 (0.16) | <0.001 |
| Sex, n (%) | <0.001 | |||
| Male | 42.6 % | 61.2 % | 38.8 % | |
| Female | 57.4 % | 53.2 % | 46.7 % | |
| Race, n (%) | 0.026 | |||
| White | 89.6 % | 56.6 % | 43.3 % | |
| Black | 8.3 % | 60.5 % | 39.5 % | |
| Other | 2.1 % | 41.0 % | 59.0 % | |
| Education—years | <0.001 | |||
| 0–8 | 24.5 % | 65.5 % | 34.5 % | |
| 9–11 | 17.4 % | 60.7 % | 39.3 % | |
| 12 | 30.5 % | 54.0 % | 46.0 % | |
| ≥13 | 27.6 % | 48.9 % | 51.1 % | |
| Height, m | 1.65 (0.002) | 1.64 (0.002) | 1.65 (0.003) | 0.088 |
| Body mass index, kg/m2 | <0.001 | |||
| <18.5 | 2.3 % | 88.6 % | 11.4 % | |
| 18.5–24.9 | 35.2 % | 59.5 % | 40.5 % | |
| 25.0–29.9 | 38.6 % | 54.6 % | 45.4 % | |
| ≥30.0 | 23.9 % | 52.6 % | 47.4 % | |
| Smoking status, n (%) | <0.001 | |||
| Never | 44.0 % | 51.2 % | 48.8 % | |
| Former | 40.4 % | 57.9 % | 42.1 % | |
| Current | 15.6 % | 68.6 % | 31.4 % | |
| No. of alcoholic drinks consumed in past week | 1.05 (0.05) | 0.89 (0.05) | 1.26 (0.08) | <0.001 |
| No. of comorbid health conditions* | <0.001 | |||
| 0 | 19.0 % | 48.5 % | 51.5 % | |
| 1 | 29.1 % | 52.5 % | 47.5 % | |
| 2 | 25.8 % | 56.4 % | 43.6 % | |
| ≥3 | 26.1 % | 67.5 % | 32.5 % | |
| ≥1 hospitalization(s) in past 1 year, n (%) | 17.4 % | 66.9 % | 33.1 % | <0.001 |
| Self-reported health (best–worst: 1–5) | 2.86 (0.02) | 3.08 (0.03) | 2.57 (0.03) | <0.001 |
| No. of bouts of walking in past week, n (%) | <0.001 | |||
| 0 | 68.3 % | 62.5 % | 37.5 % | |
| 1–3 | 10.7 % | 43.5 % | 56.5 % | |
| ≥3 | 21.0 % | 44.2 % | 55.8 % | |
| Walking cadence (steps∙minute−1) | 106.7 (0.42) | 103.2 (0.54) | 111.3 (0.63) | <0.001 |
*Includes hypertension, diabetes, hyperlipidemia, asthma, cancer, arthritis, heart attack, stroke, and heart failure
Statistical Analysis
The primary outcome was all-cause mortality. Secondary outcomes included cardiovascular-specific mortality, cancer-specific mortality, and mortality from other causes. The primary analysis specified walking cadence as a binary variable: <100 steps∙minute−1 or ≥100 steps∙minute−1. We also analyzed walking cadence as a continuous variable. We used Cox proportional hazards regression models to estimate the hazard ratio [HR] and 95 % confidence interval [95 % CI] of walking cadence and mortality. Models were estimated unadjusted (model 1), adjusted for sex and age (model 2), and fully adjusted for demographic and clinical characteristics (model 3). We confirmed the assumption of proportional hazards using log-log plots.24 We explored whether certain population subgroups modified the relationship between walking cadence and all-cause mortality using statistical interactions in multivariable-adjusted regression models (i.e., pinteraction). To compare the discriminative capacity of walking cadence and gait speed to predict 5- and 10-year mortality, we calculated the area under the receiver-operating characteristic (ROC) curve, known as the C-statistic, using logistic regression models that adjusted for age and sex. The minimal meaningful difference between C-statistics was set at ± 0.025,25 which indicates a clinically meaningful difference in predictive accuracy.19 All statistical analyses incorporated sample weights to account for nonresponse bias, multistage sampling probabilities, and the subpopulation of participants that completed the physical performance evaluation.26 Stata/SE v.12.1 statistical software was used for all analyses.
RESULTS
Baseline Characteristics Associated with Mortality
Participant characteristics stratified by vital status (Table 1) demonstrate that those who died were likely to be male, white, older, less physically active, and with fewer years of education. Being overweight or obese, a current or past smoker, having more comorbid health conditions, and utilizing more health care services were all variables that were associated with mortality on univariate testing.
Walking Cadence Characteristics
A total of 3,039 (61 %) participants could walk ≥100 steps∙minute−1. Among all participants, mean walking cadence was 107 steps∙minute−1 [106–108]. The mean walking cadence was 118 [117–119] steps∙minute−1 among participants who walked ≥100 steps∙minute−1 and 82 [81–84] steps∙minute−1 among participants who walked <100 steps∙minute−1. Walking cadence correlated with gait speed measurements (r = 0.74; p < 0.0001).
Walking Cadence and All-Cause Mortality
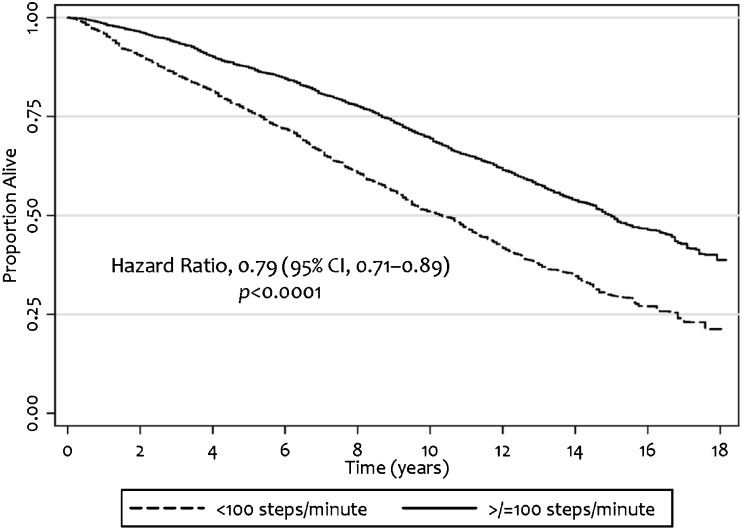
During a median of 13.4 years of follow-up, we observed 3,171 deaths. Median survival was 15.0 years in the ≥100 steps∙minute−1 group as compared with 10.3 years in the <100 steps∙minute−1 group (Fig. 1). In multivariable-adjusted analyses, the ability to walk ≥100 steps∙minute−1 predicted a 21 % reduction in the risk of all-cause mortality (HR, 0.79 [0.71–0.89], p < 0.001; Table 2) relative to <100 steps∙minute−1. Each ten-step increase in walking cadence predicted a 4 % reduction in the risk of all-cause mortality (HR, 0.96 [0.94–0.98], p < 0.001).
Fig. 1.
Kaplan-Meier curve of all-cause mortality by walking cadence
Table 2.
Walking Cadence and Risk of Mortality
| Outcome | No. at risk | No. of deaths | Hazard ratio (95 % confidence interval) | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1* | P | Model 2† | P | Model 3‡ | P | |||
| All-cause mortality | ||||||||
| <100 steps∙min−1 | 1,961 | 1,449 | 1.00 | 1.00 | 1.00 | |||
| ≥100 steps∙min−1 | 3,039 | 1,722 | 0.88 (0.81–0.98) | 0.016 | 0.71 (0.63–0.78) | <0.001 | 0.79 (0.71–0.89) | <0.001 |
| Steps∙min−1, per ten-step increase (continuous) | 5,000 | 3,171 | 0.98 (0.96–0.99) | 0.010 | 0.93 (0.91–0.95) | <0.001 | 0.96 (0.94–0.98) | <0.001 |
| Cardiovascular-specific mortality | ||||||||
| <100 steps∙min−1 | 1,961 | 693 | 1.00 | 1.00 | 1.00 | |||
| ≥100 steps∙min−1 | 3,039 | 813 | 0.87 (0.76–0.99) | 0.049 | 0.71 (0.61–0.83) | <0.001 | 0.79 (0.67–0.92) | 0.002 |
| Steps∙min−1, per ten-step increase (continuous) | 5,000 | 1,506 | 0.97 (0.95–1.00) | 0.067 | 0.94 (0.91–0.97) | <0.001 | 0.96 (0.93–0.99) | 0.014 |
| Cancer-specific mortality | ||||||||
| <100 steps∙min−1 | 1,961 | 209 | 1.00 | 1.00 | 1.00 | |||
| ≥100 steps∙min−1 | 3,039 | 264 | 0.84 (0.65–1.08) | 0.176 | 0.66 (0.51–0.87) | 0.003 | 0.76 (0.58–0.99) | 0.050 |
| Steps∙min−1, per ten-step increase (continuous) | 5,000 | 473 | 0.96 (0.92–1.01) | 0.143 | 0.92 (0.88–0.97) | 0.003 | 0.95 (0.90–1.00) | 0.060 |
| Other causes of mortality | ||||||||
| <100 steps∙min−1 | 1,961 | 547 | 1.00 | 1.00 | 1.00 | |||
| ≥100 steps∙min−1 | 3,039 | 645 | 0.93 (0.79–1.10) | 0.414 | 0.71 (0.60–0.85) | <0.001 | 0.82 (0.68–0.97) | 0.025 |
| Steps∙min−1, per ten-step increase (continuous) | 5,000 | 1,192 | 0.98 (0.95–1.01) | 0.250 | 0.93 (0.90–0.96) | <0.001 | 0.96 (0.93–0.99) | 0.037 |
*Model 1 is unadjusted (crude)
†Model 2 is adjusted for age and sex
‡Model 3 adjusted for age, sex, race, level of education, height, body mass index, smoking status, number of alcoholic drinks consumed each week, number of comorbid health conditions, prior hospitalization in the past 1 year, self-rated health, and number of bouts of walking in the past week
Walking Cadence and Cause-Specific Mortality
In multivariable-adjusted analyses, the ability to walk ≥100 steps∙minute−1 predicted a 21 % reduction in the risk of cardiovascular-specific mortality (HR, 0.79 [0.67–0.92], p = 0.002), 24 % reduction in the risk of cancer-specific mortality (HR, 0.76 [0.58–0.99], p = 0.050), and 18 % reduction in the risk of mortality from other causes (HR, 0.82 [0.68–0.97], p = 0.025) relative to <100 steps∙minute−1.
Each ten-step increase in walking cadence predicted a 4 % reduction in the risk of cardiovascular-specific mortality (HR, 0.96 [0.93–0.99], p = 0.014) and mortality from other causes (HR, 0.96 [0.93–0.99], p = 0.037), but did not predict a reduction in the risk of cancer-specific mortality (HR, 0.95 [0.90–1.00], p = 0.060).
Walking Cadence Among Population Subgroups
No population subgroups modified the relationship between walking cadence and all-cause mortality. We explored demographic subgroups including: age (pinteraction = 0.486), sex (pinteraction = 0.538), race (pinteraction = 0.961), and education (pinteraction = 0.823). We also explored clinical subgroups including: BMI (pinteraction = 0.482), smoking status (pinteraction = 0.111), alcohol consumption (pinteraction = 0.572), number of comorbid health conditions (pinteraction = 0.584), prior hospitalization in the past year (pinteraction = 0.425), self-reported health (pinteraction = 0.872), and weekly bouts of walking (pinteraction = 0.694).
Comparison Between Walking Cadence and Gait Speed
In multivariable-adjusted analyses that accounted for age and sex, walking cadence had acceptable discrimination predicting 5-year mortality (C-statistics ranged between 0.710 and 0.765) and 10-year mortality (C-statistics ranged between 0.730 and 0.800; Table 3). The difference in discrimination between walking cadence and gait speed for all 5- and 10-year mortality outcomes did not exceed the pre-specified threshold of ±0.025.
Table 3.
Discriminative Characteristics for 5- and 10-Year Mortality between Walking Cadence and Gait Speed
| Outcome | C-statistic (95 % confidence interval)* | |||||
|---|---|---|---|---|---|---|
| 5-year mortality | 10-year mortality | |||||
| Walking cadence | Gait speed | Difference† | Walking cadence | Gait speed | Difference† | |
| All-cause mortality | 0.738 (0.720–0.755) | 0.750 (0.733–0.767) | −0.012 (−0.016 to −0.008) | 0.771 (0.759–0.784) | 0.780 (0.768–0.793) | −0.009 (−0.012 to −0.006) |
| Cardiovascular-specific mortality | 0.765 (0.743–0.787) | 0.775 (0.753–0.797) | −0.010 (−0.015 to −0.006) | 0.800 (0.783–0.816) | 0.807 (0.791–0.823) | −0.007 (−0.010 to–0.004) |
| Cancer-specific mortality | 0.717 (0.679–0.754) | 0.726 (0.689–0.763) | −0.009 (−0.016 to −0.001) | 0.730 (0.700–0.759) | 0.736 (0.706–0.766) | −0.006 (−0.012 to −0.001) |
| Other causes of mortality | 0.710 (0.681–0.740) | 0.727 (0.698–0.755) | −0.017 (−0.027 to −0.005) | 0.752 (0.731–0.772) | 0.766 (0.746–0.786) | −0.014 (−0.020 to −0.009) |
*Predicted from multivariable (age and sex) adjusted logistic regression models
†Calculated as the difference between the C-statistic of walking cadence minus the C-statistic of gait speed. The minimal clinically meaningful difference in C-statistics was specified at ± 0.025
Walking Cadence, Gait Speed, and All-Cause Mortality
In multivariable-adjusted analyses, when walking cadence and gait speed were entered simultaneously into the regression model, both factors retained statistical significance. For each 0.1-m/s increase in gait speed, the risk of premature mortality decreased by 11 % (HR, 0.89 [0.86–0.93], p < 0.001). Each ten-step increase in walking cadence predicted a 4 % increase in all-cause mortality (HR, 1.04 [1.01–1.08], p = 0.039). We did not identify a statistical interaction between walking cadence and gait speed (pinteraction = 0.707). The simultaneous inclusion of walking cadence and gait speed did not substantively change the discrimination of models to predict 5-year all-cause mortality (C-statistic, 0.751 [0.734–0.767]) or 10-year all-cause mortality (C-statistic, 0.781 [0.769–0.794]).
DISCUSSION
The principal finding of this study is that community-dwelling older adults who can walk ≥100 steps∙minute−1 are 21 % less likely to die prematurely relative to those who can walk <100 steps∙minute−1. This relationship was consistent with our secondary analyses of cause-specific mortality. Walking cadence has been advocated as an intuitive means for older adults to quantify the intensity of physical activity, with the current recommendation that 100 steps∙minute−1 defines the lowest cadence sufficient for moderate-intensity physical activity.12 Our results suggest a threshold of 100 steps∙minute−1 may also identify community-dwelling older adults at risk for premature mortality. A major benefit of walking cadence as a metric of physical function is the fact that older adults find walking cadence intuitive.14 Furthermore, our findings promote motivated patients who wish to self-monitor their physical function to do so with a simple and non-invasive metric.
We compared the discriminative characteristics for 5- and 10-year mortality between walking cadence and gait speed. In a previous pooled analysis of 34,485 community-dwelling older adults, gait speed, age, and sex predicted all-cause mortality similarly to more complex models that included factors such as BMI, systolic blood pressure, smoking history, comorbidity, and prior hospitalization.19 In the current analysis, using the C-statistics from logistic regression models, our analyses suggest that walking cadence and gait speed do not substantively differ in their discriminative characteristics. The largest difference in C-statistics observed between walking cadence and gait speed was 5-year mortality from other causes, which did not meet the minimal clinically meaningful difference of 0.025 between C-statistics.25
We also quantified the prognostic importance of walking cadence while simultaneously adjusting for gait speed. In our multivariable-adjusted analyses, holding gait speed constant, each ten-step increase in walking cadence predicted a 4 % increase in mortality. Walking cadence and gait speed may represent separate physical function constructs given that each factor retained statistical significance when simultaneously included in a multivariable-adjusted regression model. This observation is consistent with the hypothesis that at a given gait speed, those who require more steps to complete a fixed distance may have underlying disease relative to those who take fewer larger steps. The term “senile gate” has been used to characterize walking impairments in older adults that manifest as a broad-based, cautious, shuffling pattern.27 This shuffling pattern would result in a greater number of steps taken and may explain the observed increase in risk of mortality while adjusting for gait speed. Despite the independence of walking cadence and gait speed as predictors of mortality, their simultaneous inclusion did not substantively change the discrimination predicting 5- or 10-year all-cause mortality relative to predictive models that included walking cadence or gait speed individually.
Older adults take 2,000–9,000 steps per day on average.12 However, these steps are generally accrued throughout the day at a cadence <100 steps∙minute−1. The ACSM guidelines recommend that older adults participate in 150-min per week of brisk walking at a pace of 100 step∙minute−1.8 However, among adults in the NHANES cohort, only approximately 5 min per day includes walking at a cadence ≥100 step∙minute−1.28 Our study bolsters the argument that higher walking cadence is associated with improved survival and provides additional motivation for older adults to participate in physical activity, which is known to increase walking cadence29 and gait speed.11 While it is known that improvements in gait speed predict reductions in the risk of mortality,30 it is unknown whether improvements in walking cadence predict similar reductions in the risk of mortality. Nevertheless, it is acknowledged that participation in physical activity such as brisk walking provides numerous health benefits to older adults. Such health benefits include reductions in BMI, systolic blood pressure,15 and cardiovascular events.31
To promote regular participation in physical activity, clinicians may encourage patients to pursue step count targets. Giving patients a target such as walking 10,000 steps per day has been shown to significantly increase daily step counts.15 Notably, any increase in daily step count relative to baseline values could confer health benefits among sedentary older adults.12 Though the measurement of walking cadence in our study was cross-sectional, our data are consistent with such a hypothesis. In multivariable-adjusted regression models, each ten-step increase in walking cadence predicted a significant 4 % reduction in the risk of premature all-cause mortality. Participating in brisk walking with a cadence of ≥100 step∙minute−1 is feasible through ambulatory activity required for daily living. For example, among 936 adults living in New York City, the mean walking cadence was 112 steps∙minute−1.32 Alternatively, brisk walking with a cadence of ≥100 step∙minute−1 may be completed through treadmill walking.29,33 The heuristic of 1,000 steps in 10 min or 3,000 steps in 30 min (100 step∙minute−1) is useful to help patients recall the walking cadence sufficient in intensity to confer health benefits.
The estimated walking cadence in this study was consistent with other studies that have used accelerometers.12,28 However, the main limitation to this study is that walking cadence was calculated from a 2.4-m walk rather than directly measured using the number of steps walked in 1 min. Consequently, our prediction may overestimate or underestimate the actual walking cadence.34 Unlike gait speed, which uses time (usually to the nearest tenth of a second), walking cadence uses whole numbers and does not allow for partial values. This limitation may restrict sensitivity to subtle yet potentially important changes in walking cadence. Another limitation is that walking cadence was a cross-sectional measurement. It is unknown whether improving walking cadence over time would translate to a reduction in the risk of premature mortality. The main strength of this study is the large sample size that, based on the sampling framework from NHANES, is representative of the US population of community-dwelling older adults.35
Walking cadence is a uniquely useful physical function metric, given its simple interpretation and its concurrent use to indicate the intensity of physical activity.12 Informing older adults about the importance of walking ≥100 steps∙minute−1 holds potential to educate patients about the prognostic importance of physical function. Discussing the relationship of walking cadence with mortality reinforces the importance of participating in regular physical activity to patients. Future studies are needed to confirm our findings and to determine whether changes in walking cadence over time (e.g., from improving physical fitness) alter the risk for mortality in older adults. In conclusion, the ability to walk ≥100 steps∙minute−1 is associated with a reduction in premature mortality. The observed relationship between walking cadence and mortality warrants further investigation.
ACKNOWLEDGEMENTS
Justin C. Brown had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Meera N. Harhay has received training grants (5T32DK007006-38 and F32DK096758-01) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Michael O. Harhay is supported as a pre-doctoral fellow by National Cancer Institute (NCI) grant R01 CA159932. Justin C. Brown is supported as a pre-doctoral fellow by NCI grant U54 CA155850. This study was completed without funding.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in the United States: 2010 to 2050. Current Population Reports. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2010. p. P25-1138. [Google Scholar]
- 2.Manton KG, Vaupel JW. Survival after the age of 80 in the united states, Sweden, France, England, and Japan. N Engl J Med. 1995;333(18):1232–1235. doi: 10.1056/NEJM199511023331824. [DOI] [PubMed] [Google Scholar]
- 3.Katz S, Branch LG, Branson MH, Papsidero JA, Beck JC, Greer DS. Active life expectancy. N Engl J Med. 1983;309(20):1218–1224. doi: 10.1056/NEJM198311173092005. [DOI] [PubMed] [Google Scholar]
- 4.Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the american geriatrics Society/National institute on aging research conference on frailty in older adults. J Am Geriatr Soc. 2006;54(6):991–1001. doi: 10.1111/j.1532-5415.2006.00745.x. [DOI] [PubMed] [Google Scholar]
- 5.Lonergan ET, Krevans JR. A national agenda for research on aging. N Engl J Med. 1991;324(25):1825–1828. doi: 10.1056/NEJM199106203242527. [DOI] [PubMed] [Google Scholar]
- 6.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.M85. [DOI] [PubMed] [Google Scholar]
- 7.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295(17):2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 8.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the american college of sports medicine and the american heart association. Med Sci Sports Exerc. 2007;39(8):1435. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 9.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults: a critical review and recommendations. Am J Prev Med. 1998;15(4):316–333. doi: 10.1016/S0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 10.United States. Public Health Service. Office of the Surgeon General, National Center for Chronic Disease Prevention, Health Promotion (US), President’s Council on Physical Fitness, Sports (US). Physical Activity and Health: A Report of the Surgeon. Jones & Bartlett Learning; 1996.
- 11.LIFE Study Investigators. Pahor M, Blair SN, et al. Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for elders pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 12.Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough for older adults and special populations? Int J Behav Nutr Phys Act. 2011;8(1):80. doi: 10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marshall SJ, Levy SS, Tudor-Locke CE, et al. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36(5):410–415. doi: 10.1016/j.amepre.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 14.Bouchard DR, Langlois M, Boisvert-Vigneault K, Farand P, Paulin M, Baillargeon J. Pilot study: can older inactive adults learn how to reach the required intensity of physical activity guideline? Clin Interv Aging. 2013;8:501–508. doi: 10.2147/CIA.S42224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health. JAMA. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 16.McKay J, Wright A, Lowry R, Steele K, Ryde G, Mutrie N. Walking on prescription: the utility of a pedometer pack for increasing physical activity in primary care. Patient Educ Couns. 2009;76(1):71–76. doi: 10.1016/j.pec.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Eakin EG, Brown WJ, Marshall AL, Mummery K, Larsen E. Physical activity promotion in primary care: bridging the gap between research and practice. Am J Prev Med. 2004;27(4):297–303. doi: 10.1016/j.amepre.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 18.Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies. J Fam Pract. 2000;49(2):158–168. [PubMed] [Google Scholar]
- 19.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plan and operation of the third national health and nutrition examination survey, 1988–94. series 1: Programs and collection procedures. Vital Health Stat 1. 1994;(32)(32):1–407. [PubMed]
- 21.Ostchega Y, Harris TB, Hirsch R, Parson VL, Kington R, Katzoff M. Reliability and prevalence of physical performance examination assessing mobility and balance in older persons in the US: data from the third national health and nutrition examination survey. J Am Geriatr Soc. 2000;48(9):1136–1141. doi: 10.1111/j.1532-5415.2000.tb04792.x. [DOI] [PubMed] [Google Scholar]
- 22.Rogot E, Sorlie P, Johnson NJ. Probabilistic methods in matching census samples to the national death index. J Chron Dis. 1986;39(9):719–734. doi: 10.1016/0021-9681(86)90155-4. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems. World Health Organization; 2004.
- 24.Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer; 2001.
- 25.Apfel CC, Kranke P, Greim CA, Roewer N. What can be expected from risk scores for predicting postoperative nausea and vomiting? Br J Anaesth. 2001;86(6):822–827. doi: 10.1093/bja/86.6.822. [DOI] [PubMed] [Google Scholar]
- 26.Korn EL, Graubard BI. Epidemiologic studies utilizing surveys: accounting for the sampling design. Am J Public Health. 1991;81(9):1166–1173. doi: 10.2105/AJPH.81.9.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salzman B. Gait and balance disorders in older adults. Am Fam Physician. 2010;82(1):61–68. [PubMed] [Google Scholar]
- 28.Tudor-Locke C, Camhi SM, Leonardi C, et al. Patterns of adult stepping cadence in the 2005–2006 NHANES. Prev Med. 2011;53(3):178–181. doi: 10.1016/j.ypmed.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 29.Silver KH, Macko RF, Forrester LW, Goldberg AP, Smith GV. Effects of aerobic treadmill training on gait velocity, cadence, and gait symmetry in chronic hemiparetic stroke: a preliminary report. Neurorehabil Neural Repair. 2000;14(1):65–71. doi: 10.1177/154596830001400108. [DOI] [PubMed] [Google Scholar]
- 30.Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55(11):1727–1734. doi: 10.1111/j.1532-5415.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- 31.Yates T, Haffner SM, Schulte PJ, et al. Association between change in daily ambulatory activity and cardiovascular events in people with impaired glucose tolerance (NAVIGATOR trial): a cohort analysis. Lancet. 2014;383(9922):1059–1066. doi: 10.1016/S0140-6736(13)62061-9. [DOI] [PubMed] [Google Scholar]
- 32.Drillis R. Objective recording and biomechanics of pathological gait. Ann N Y Acad Sci. 1958;74(1):86–109. doi: 10.1111/j.1749-6632.1958.tb39534.x. [DOI] [PubMed] [Google Scholar]
- 33.Wass E, Taylor NF, Matsas A. Familiarisation to treadmill walking in unimpaired older people. Gait Posture. 2005;21(1):72–79. doi: 10.1016/j.gaitpost.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Dean CM, Richards CL, Malouin F. Walking speed over 10 metres overestimates locomotor capacity after stroke. Clin Rehabil. 2001;15(4):415–421. doi: 10.1191/026921501678310216. [DOI] [PubMed] [Google Scholar]
- 35.Ezzati TM, Massey J, Waksberg J, Chu A, Maurer K. Sample design: Third national health and nutrition examination survey. Vital and health statistics.Series 2, Data evaluation and methods research. 1992(113):1–35. [PubMed]