ABSTRACT
BACKGROUND
The Medicare Accountable Care Organization (ACO) programs encourage integration of providers into large groups and reward provider groups for improving quality, but not explicitly for reducing health care disparities. Larger group size and better overall quality may or may not be associated with smaller disparities.
OBJECTIVE
To examine differences in patient characteristics between provider groups sufficiently large to participate in ACO programs and smaller groups; the association between group size and racial disparities in quality; and the association between quality and disparities among larger groups.
DESIGN AND PARTICIPANTS
Using 2009 Medicare claims for 3.1 million beneficiaries with cardiovascular disease or diabetes and linked data on provider groups, we compared racial differences in quality by provider group size, adjusting for patient characteristics. Among larger groups, we used multilevel models to estimate correlations between group performance on quality measures for white beneficiaries and black–white disparities within groups.
MAIN MEASURES
Four process measures of quality, hospitalization for ambulatory care-sensitive conditions (ACSCs) related to cardiovascular disease or diabetes, and hospitalization for any ACSC.
KEY RESULTS
Beneficiaries served by larger groups were more likely to be white and live in areas with less poverty and more education. Larger group size was associated with smaller disparities in low-density lipoprotein (LDL) cholesterol testing and retinal exams, but not in other process measures or hospitalization for ACSCs. Among larger groups, better quality for white beneficiaries in one measure (hospitalization for ACSCs related to cardiovascular disease or diabetes) was correlated with smaller racial disparities (r = 0.28; P = 0.02), but quality was not correlated with disparities in other measures.
CONCLUSIONS
Larger provider group size and better performance on quality measures were not consistently associated with smaller racial disparities in care for Medicare beneficiaries with cardiovascular disease or diabetes. ACO incentives rewarding better quality for minority groups and payment arrangements supporting ACO development in disadvantaged communities may be required for ACOs to promote greater equity in care.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2900-3) contains supplementary material, which is available to authorized users.
KEY WORDS: delivery of health care, accountable care organizations, medicare, disparities, quality of health care
BACKGROUND
The Medicare Accountable Care Organizations (ACO) programs are designed to encourage lower spending and better quality of care through new payment incentives to large provider groups.1 To contract with Medicare as ACOs, provider groups must meet a minimum size threshold and demonstrate structural capacity for care coordination and quality improvement. ACOs that meet minimum performance targets on a set of quality measures are then eligible to share in savings with Medicare if spending is lower than expected for attributed beneficiaries.2
Although the ACO programs encourage delivery system integration and quality improvement, concerns have been raised that they may not redress, and may even exacerbate, health care disparities.3,4 Because care for racial and ethnic minorities is concentrated among physicians and hospitals with fewer resources,5–10 advanced provider groups ready to participate in ACO programs may disproportionately care for white patients. Consolidation of physicians into larger organizations has been associated with greater structural capacity for care coordination and quality improvement,11–15 and larger physician groups perform better on process measures of quality of care than smaller groups.16 The relationship between organizational size and health care disparities, however, has not been elucidated. Moreover, prior research suggests that overall improvements in quality have not been consistently associated with reduced disparities, particularly in clinical outcomes.17–19 Thus, while provider integration and quality improvement fostered by ACO programs might improve care for many patients, such gains may or may not be associated with reductions in health disparities.
Using Medicare claims for beneficiaries with cardiovascular disease or diabetes and linked data from the American Medical Association (AMA) Group Practice File, we examined differences in patient characteristics and quality of care between provider groups sufficiently large to participate in ACO programs and smaller groups. Among larger groups potentially eligible for ACO programs, we examined the association between quality of care for white beneficiaries and within-group racial disparities in care, and assessed the extent to which overall disparities were attributable to racial differences within or between provider groups.
METHODS
Data Sources and Study Population
We analyzed 2009 Medicare claims for traditional fee-for-service Medicare beneficiaries who were continuously enrolled in Parts A and B, received at least one primary care service during the year, and had a history of cardiovascular disease or diabetes (conditions emphasized by quality measures in ACO contracts). Specifically, we used dates of first diagnosis from the Chronic Condition Warehouse (CCW), which draws from claims since 1999, to identify beneficiaries with any of the following conditions before 2009: diabetes, ischemic heart disease, acute myocardial infarction, congestive heart failure, and stroke.20 We limited analyses to beneficiaries age 50 or older because of the lower prevalence of these conditions among younger adults. We also limited our study to beneficiaries classified as black or white in Medicare enrollment files, because other racial and ethnic groups were not as reliably identified by these administrative data.21,22 Finally, we excluded residents of US territories as well as long-term nursing home residents identified by a validated algorithm23 to limit provider organizations to those providing outpatient primary care services (the basis for beneficiary attribution to provider groups).
The AMA Group Practice File identifies the practice site(s) of physicians in the AMA Physician Masterfile who practice in groups of ≥ 3 physicians and their parent organization if part of a larger group. We linked this information to Medicare claims via physicians’ National Provider Identifiers (NPIs). Of primary care physicians (PCPs) serving Medicare beneficiaries in 2009, 96 % were linked to the Masterfile. Of PCPs in the Masterfile practicing in groups of ≥ 3 physicians, 90 % were linked to the Group Practice File (Online Appendix).
Study Variables
Size of Beneficiaries’ Assigned Provider Groups
Using claims for physician services for a 20 % random sample of beneficiaries and following the Medicare Shared Savings Program assignment rules, we assigned each beneficiary to the provider group accounting for the most allowed charges for primary care services among all groups providing primary care services to the beneficiary.2 To identify provider groups, we used both groupings of NPIs from the AMA Group Practice File and tax identification numbers (TINs) indicating billing entities in Medicare claims. We applied the assignment algorithm to each beneficiary twice, using each of these two sources of group identifiers independently. For groups identified by the Group Practice File as members of larger organizations, we used the highest level of organization to which they were connected (through up to five levels of hierarchical affiliations) when assigning beneficiaries. Because TINs and AMA Group Practice data were complementary in identifying higher levels of provider organization,16,24 for each beneficiary we used the larger of the two assigned groupings for analyses, as determined by the number of beneficiaries assigned to each (Online Appendix).
We categorized the size of provider groups according to eligibility for the two major Medicare ACO programs: small groups ineligible for ACO programs (< 5,000 assigned beneficiaries); medium-sized groups eligible for the Shared Savings Program (5,000–14,999); and large groups eligible for the Pioneer or Shared Savings Program (≥ 15,000), scaling eligibility thresholds to the 20 % sample.
Measures of Quality of Care for Cardiovascular Disease and Diabetes
Our dependent variables included four process measures adapted from the Healthcare Effectiveness Data and Information Set (HEDIS®) and two summary indicators of potentially avoidable hospitalizations for ambulatory care-sensitive conditions (ACSCs) adapted from the Agency for Healthcare Research and Quality (AHRQ) Prevention Quality Indicators (PQIs).25 Specifically, for beneficiaries in a 5 % sample, for whom we had claims for both inpatient and outpatient care, we assessed low-density lipoprotein (LDL) cholesterol testing in 2009 for beneficiaries with cardiovascular disease (ischemic heart disease, history of acute myocardial infarction, congestive heart failure, or history of stroke) and three services for beneficiaries with diabetes, including hemoglobin A1c and LDL cholesterol testing in 2009 and a diabetic retinal exam in 2008 or 2009.26,27 We also created a composite indicator denoting receipt of all three recommended diabetes services.
For beneficiaries in the 20 % sample, for whom we had claims for inpatient care, we created an indicator of hospitalization in 2009 for ACSCs related to cardiovascular disease or diabetes, including hospitalization for uncontrolled diabetes, short-term complications of diabetes, long-term complications of diabetes, lower-extremity amputation, hypertension, angina without procedure, and congestive heart failure.25 We also created an indicator of hospitalization in 2009 for any ACSC included in the AHRQ set of PQIs relevant to elderly adults (additionally including chronic obstructive pulmonary disease, dehydration, bacterial pneumonia, urinary tract infection, and asthma). Two PQIs are included as quality metrics in Medicare ACO contracts (congestive heart failure and chronic obstructive pulmonary disease).
Beneficiary Characteristics
From Medicare enrollment files, we determined age, sex, race (black or white), disability upon enrollment in Medicare, presence of end-stage renal disease, and Medicaid eligibility. From CCW indicators and dates of diagnosis, we assessed the presence of 21 conditions prior to 2009.20 From 2006–2010 U.S. Census data, we additionally assessed educational attainment and poverty rates among elderly adults in beneficiaries’ zip code tabulation areas (ZCTA).28
Statistical Analysis
In unadjusted descriptive analyses (Table 1), we compared beneficiaries’ sociodemographic and clinical characteristics by the size of their assigned provider groups. To compare racial differences in quality of care between small provider groups and those sufficiently large to be eligible for ACO programs (Figs. 1–2), we fitted linear regression models predicting each quality indicator as a function of the size of beneficiaries’ assigned groups (small, medium-sized, or large), an indicator of black race, interactions between black race and group size, county fixed effects, and the sociodemographic and clinical characteristics described above. We adjusted standard errors for clustering at the provider-group level.29,30
Table 1.
Sociodemographic and Clinical Characteristics of Medicare Beneficiaries with Diabetes or Cardiovascular Disease by Size of Assigned Provider Group*
| Size of Assigned Provider Group† | |||||
|---|---|---|---|---|---|
| Small N = 1,940,061 | Medium-sized N = 576,238 | Large N = 586,555 | Total N = 3,102,854 | ||
| Age (%) | |||||
| Under 65 years | 8.6 | 8.4 | 7.8 | 8.4 | |
| 65–69 years | 12.8 | 12.8 | 12.7 | 12.8 | |
| 70–74 years | 20.0 | 20.0 | 20.0 | 20.0 | |
| 75–79 years | 20.6 | 20.9 | 21.1 | 20.7 | |
| 80–84 years | 18.5 | 18.9 | 19.1 | 18.7 | |
| 85 years and older | 19.6 | 19.1 | 19.4 | 19.5 | |
| Female (%) | 58.6 | 58.4 | 57.8 | 58.4 | |
| Race (%) | |||||
| White | 90.1 | 91.0 | 92.0 | 90.6 | |
| Black | 9.9 | 9.0 | 8.0 | 9.4 | |
| Medicaid (%) | 15.3 | 12.7 | 11.6 | 14.1 | |
| ZCTA—level characteristics, mean | |||||
| % below federal poverty line | 9.4 | 8.8 | 8.4 | 9.1 | |
| % with high school degree or higher | 74.8 | 76.3 | 77.6 | 75.6 | |
| % with college degree or higher | 19.2 | 19.6 | 20.0 | 19.4 | |
| Population Area (%) | |||||
| Metropolitan county, 1 million or more | 45.6 | 39.4 | 41.9 | 43.7 | |
| Metropolitan county, less than 1 million | 29.1 | 39.2 | 36.4 | 32.3 | |
| Non-metropolitan county | 25.3 | 21.4 | 21.8 | 23.9 | |
| Chronic Conditions from the CCW (%) | |||||
| Diabetes mellitus | 50.7 | 49.0 | 48.3 | 50.0 | |
| Ischemic heart disease | 74.6 | 73.7 | 72.6 | 74.0 | |
| Acute myocardial infarction | 6.9 | 7.5 | 7.4 | 7.1 | |
| Congestive heart failure | 39.3 | 38.1 | 37.0 | 38.7 | |
| Stroke | 20.2 | 20.3 | 20.0 | 20.2 | |
| Atrial fibrillation | 18.2 | 19.5 | 19.4 | 18.7 | |
| Chronic obstructive pulmonary disease | 28.2 | 26.8 | 25.7 | 27.4 | |
| Chronic kidney disease | 21.3 | 22.5 | 22.8 | 21.8 | |
| Alzheimer’s disease | 4.7 | 4.3 | 4.2 | 4.5 | |
| Dementia | 12.1 | 11.4 | 11.2 | 11.8 | |
| Osteoporosis | 36.9 | 35.9 | 34.8 | 36.3 | |
| History of hip fracture | 3.5 | 3.5 | 3.5 | 3.5 | |
| Depression | 28.2 | 30.1 | 30.1 | 28.9 | |
| Arthritis | 36.9 | 35.9 | 34.8 | 36.3 | |
| Breast cancer | 4.6 | 5.1 | 5.4 | 4.8 | |
| Colon cancer | 2.9 | 2.8 | 2.9 | 2.9 | |
| Prostate cancer | 5.7 | 5.9 | 6.1 | 5.8 | |
| Lung cancer | 1.5 | 1.6 | 1.6 | 1.5 | |
| Endometrial cancer | 0.6 | 0.6 | 0.7 | 0.6 | |
| Cataract | 69.3 | 70.9 | 70.9 | 69.9 | |
| Glaucoma | 24.0 | 23.9 | 23.5 | 23.9 | |
| 3 or more conditions | 73.5 | 73.8 | 72.8 | 73.4 | |
| 4 or more conditions | 70.6 | 71.2 | 70.2 | 70.7 | |
| 5 or more conditions | 37.9 | 37.6 | 36.4 | 37.6 | |
| Mean number of chronic conditions | 5.0 | 5.0 | 4.9 | 5.0 | |
ZCTA = zip code tabulation area; CCW = Chronic condition warehouse
*Tests of statistical significance were conducted using chi-square tests for categorical variables and analysis of variance for continuous variables. Differences across the three categories of provider group size were statistically significant at a P < 0.01 level except for history of hip fracture. Sums of percentages may not equal 100 % due to rounding
† Size of provider groups was categorized according to eligibility for the two major Medicare ACO programs: small groups ineligible for ACO programs (< 5,000 assigned beneficiaries); medium-sized groups eligible for the Shared Savings Program (5,000–14,999 assigned beneficiaries); and large groups eligible for the Pioneer or Shared Savings Program (≥ 15,000 assigned beneficiaries), scaling eligibility thresholds to the 20 % sample
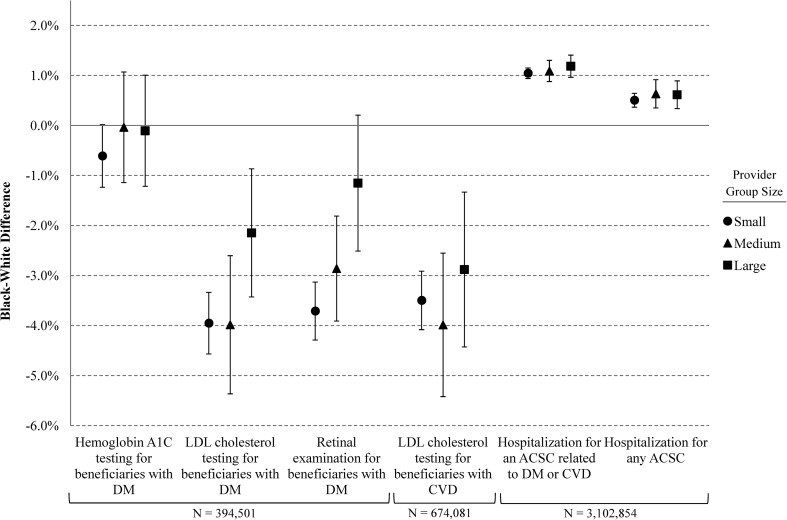
Figure 1.
Quality of care for beneficiaries with cardiovascular disease or diabetes by race and size of provider group. Performance on six quality measures (Panels A–F) are displayed by provider group size and race. Compared with small provider groups, racial differences in LDL cholesterol testing (Panel B) and retinal exams (Panel C) were significantly smaller for large groups (P ≤ 0.01) as a result of higher rates for black beneficiaries with diabetes, but racial differences in other quality measures did not differ by group size. Compared with small groups, both medium-sized and large groups performed better on all process measures for both white and black beneficiaries (P ≤ 0.01) but did not have lower rates of hospitalization for ACSCs. ACSC = ambulatory care sensitive condition; DM = diabetes mellitus; CVD = cardiovascular disease; LDL = low-density lipoprotein.
Figure 2.
Racial difference in quality for beneficiaries with cardiovascular disease or diabetes by provider group size. Black–white differences in six quality measures are displayed by the size of beneficiaries’ assigned provider group. Categories of provider group size are based on eligibility thresholds for participation in the Medicare ACO programs: small or ineligible for ACO programs (≤ 5,000 assigned beneficiaries); medium-sized or eligible for the Shared Savings Program but not for the Pioneer program (5,000–14,999 assigned beneficiaries); and large or eligible for the Pioneer program (≥ 15,000 assigned beneficiaries). Error bars indicate 95 % confidence intervals. ACSC = ambulatory care sensitive condition; DM = diabetes mellitus; CVD = cardiovascular disease; LDL = low-density lipoprotein.
We used multilevel models to quantify the relationship between quality of care for white beneficiaries and racial disparities in quality among groups sufficiently large to be ACOs (Fig. 3). Specifically, for beneficiaries assigned to medium-sized or large groups, we fitted linear regression models predicting each quality indicator as a function of race, the same set of sociodemographic and clinical covariates, and provider-group-level random effects for the average quality for whites and the black–white difference for each provider group:
 |
where Y is the quality indicator for beneficiary i assigned to provider group j; β0 is the overall mean for white beneficiaries; β1 is the overall mean black–white difference; β2 is a vector of coefficients for the sociodemographic and clinical covariates described above; u0j are the provider-group-specific random effects for white beneficiaries; and u1j are the random effects for black–white differences. To describe the relationship between the provider group averages for whites and the racial differences within provider groups, from an unstructured covariance matrix for the random effects, we calculated a correlation coefficient for each quality measure as
 |
where σu0u1 is the covariance between u0j and u1j, and σ2u0 and σ2u1 are the variances of u0j and u1j, respectively. To facilitate interpretation of these correlations, we categorized beneficiaries’ assigned provider groups by quartile of performance for white beneficiaries and present adjusted racial differences in quality by these quartiles.
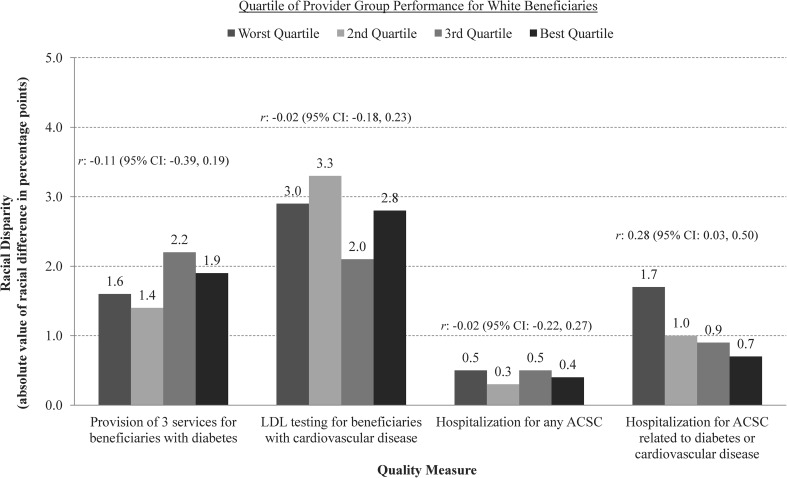
Figure 3.
Racial disparities in quality of care by quartile of provider group performance for white beneficiaries among provider groups sufficiently large for ACO programs. For each quality measure, provider groups sufficiently large to participate in ACO programs (medium-sized and large groups) were categorized into quartiles according to their performance for white beneficiaries. For each quartile, the adjusted racial disparity (absolute value of the difference between black and white beneficiaries) is shown for each of the following measures: provision of all three diabetes services (hemoglobin A1c testing, LDL cholesterol testing, and retinal examination) to beneficiaries with diabetes; LDL cholesterol testing for patients with cardiovascular disease; hospitalization for an ACSC related to diabetes or cardiovascular disease; and hospitalization for any ACSC. For each quality measure, the correlation between performance for white beneficiaries and the black–white difference in performance is presented with 95 % confidence intervals and two-sided p-values. Lower rates of hospitalization of white beneficiaries for ACSCs related to diabetes or cardiovascular disease were correlated with smaller black–white differences. Correlations between quality for white beneficiaries and black–white difference were not statistically significant for other quality measures.
For each quality measure, we also estimated the share of the total unadjusted racial difference attributable to black–white differences within provider groups by standardizing the racial composition of assigned populations across provider groups (Fig. 4). Specifically, we calculated the black–white difference in the quality measure for each group, and then calculated the mean of these differences, weighted by the black assigned population. We then subtracted the weighted mean within-group difference from the total difference to calculate the portion of the total racial difference attributable to differences between provider groups in racial composition of patient populations.
Figure 4.
Racial disparities in quality of care within and between provider groups sufficiently large for ACO programs. For each quality measure, the total disparity among provider groups of sufficient size to participate in ACO programs (medium-sized and large groups) was decomposed into within-group differences in quality and differences in quality related to between-group differences in racial composition. The proportion of the total unadjusted racial disparity attributable to racial differences within provider groups ranged from 53 % [2.1/(2.1 + 1.9)] to 95 % [2.0/(2.0 + 0.1)] across quality measures, while differences between groups in the racial composition of assigned populations of beneficiaries accounted for the remaining 5 % to 47 %.
All analyses were performed using Stata statistical software, version 11.2 (StataCorp, College Station, TX). The study protocol was approved by the Human Studies Committee of Harvard Medical School and the Centers for Medicare and Medicaid Services Privacy Board.
RESULTS
Of 6,259,028 traditional Medicare beneficiaries in the 2009 20 % sample, we excluded 394,681 (6.3 %) nursing home residents, 406,396 (6.5 %) beneficiaries who received no primary care services in 2009, 299,315 (4.8 %) beneficiaries under age 50, and 17,803 (0.3 %) beneficiaries with missing census data. Of remaining beneficiaries, 4,894,813 (95.2 %) were identified as white or black in enrollment files. Of this group, our analyses focused on 3,102,854 (63.4 %) beneficiaries with cardiovascular disease or diabetes, including 1,550,338 (31.7 %) with diabetes and 2,644,271 (54.0 %) with cardiovascular disease. As expected, approximately 25 % of these study populations in the 20 % sample were available in the 5 % sample for analyses of process measures.
Beneficiary Characteristics by Provider Group Size
Compared with beneficiaries with cardiovascular disease or diabetes who were assigned to small groups (63.3 %), those assigned to medium-sized (18.2 %) and large provider groups (18.6 %) were more likely to be white and less likely to be eligible for Medicaid (P < 0.001), as described in the Table. Beneficiaries assigned to larger provider groups also lived in areas with lower poverty rates and higher educational attainment (P < 0.001).
Overall Disparities
In adjusted overall comparisons (results not shown in Figures), black beneficiaries with diabetes were significantly less likely than white beneficiaries with diabetes to receive LDL cholesterol testing (adjusted proportion for black vs. white beneficiaries: 74.5 % vs. 78.1 %; P < 0.001) and retinal exams (66.3 % vs. 69.4 %; P < 0.001), but equally likely to receive A1c testing (71.4 % vs. 71.8 %; P = 0.13). Black beneficiaries with cardiovascular disease were also less likely to have their LDL cholesterol tested (65.4 % vs. 68.8 %; P < 0.001). Black beneficiaries with cardiovascular disease or diabetes were more likely to be hospitalized for ACSCs (4.6 % vs. 4.1 %; P < 0.001), particularly for conditions related to diabetes or cardiovascular disease (2.5 % vs. 1.4 %; P < 0.001).
Disparities by Provider Group Size
These racial differences did not differ by provider group size with two exceptions. Compared with small provider groups, racial differences were significantly smaller for large groups in LDL cholesterol testing (adjusted black–white difference:-4.0 vs. -2.1 percentage points for small vs. large groups; P = 0.01) and retinal exams (−3.7 vs. -1.2; P < 0.001) as a result of higher rates for black beneficiaries with diabetes (Figs. 1–2). Compared with small groups, both medium-sized and large groups performed better on all process measures for both white and black beneficiaries (P ≤ 0.01) but did not have lower rates of hospitalization for ACSCs.
Correlation Between Quality and Disparities Among Provider Groups Sufficiently Large for ACO Programs
As shown in Figure 3, among provider groups sufficiently large to participate in ACO programs (medium-sized and large groups), adjusted correlations between quality of care for white beneficiaries and within-group racial differences in quality were weak and not statistically significant for all quality measures except hospitalization for ACSCs related to cardiovascular disease and diabetes (r = 0.28; P = 0.02). Medium-sized and large groups in the best quartile of hospitalization rates for these conditions among white beneficiaries exhibited racial differences that were less than half as large, on average, as differences among groups in the worst quartile (Fig. 3).
Decomposition of Disparities into Between Versus Within-Group Differences Among Provider Groups Sufficiently Large for ACO Programs
Among medium-sized and large groups, the proportion of the total unadjusted racial difference attributable to racial differences within provider groups ranged from 53 % to 95 % across quality measures, while differences between groups in the racial composition of assigned populations of beneficiaries accounted for the remaining 5 % to 47 % (Fig. 4).
DISCUSSION
In this national study of Medicare beneficiaries with cardiovascular disease or diabetes, those served by provider groups sufficiently large to participate in ACO programs were more likely to be white and lived in more socioeconomically advantaged areas than beneficiaries served by smaller groups. Larger groups potentially eligible for ACO programs exhibited smaller racial disparities in some process measures of quality but not in potentially avoidable hospitalizations for complications of cardiovascular disease and diabetes. Moreover, among these larger groups, higher performance on quality measures was not associated with smaller racial disparities in five of the six quality measures we examined. Thus, while larger group size and better performance on quality measures—both encouraged by ACO programs—were associated with no worse and often better quality of care for black patients, neither were consistently associated with smaller racial differences between black and white patients.
These findings are consistent with concerns that Medicare ACO programs may not effectively address health disparities.3,4 Because ACO programs are likely to be dominated by currently eligible rather than newly integrated provider groups,31 the sociodemographic differences between patients served by larger and smaller groups suggest that any clinical benefits achieved by ACOs may accrue disproportionately to white patients in more affluent areas. Previous research11–16 and ACO program requirements2,32 suggest that provider integration encouraged by ACO programs might be associated with enhanced abilities to monitor and improve quality of care, but we found that larger provider groups achieved smaller racial disparities in only two of six quality measures we analyzed. Finally, to the extent that new payment incentives improve the quality of care provided by ACOs, our findings and previous studies17–19 suggest these potential gains may not be associated with consistently reduced racial disparities in quality. Thus, although quality improvement due to ACO initiatives would benefit a substantial number of black Medicare beneficiaries served by ACOs, such improvement may not be associated with smaller disparities among ACOs or nationally.
Among provider organizations sufficiently large to be ACOs, we found that racial disparities in care for cardiovascular disease and diabetes were explained largely by racial differences in quality of care within organizations, rather than differences in the racial composition of patients between organizations. The substantial contributions of within-organization differences to overall differences, in combination with our other findings, suggest that incorporating additional incentives in ACO contracts to improve quality of care specifically for racial and ethnic minorities may be important for ACO initiatives to address disparities. For example, performance targets for each of the 33 quality metrics currently included in Shared Savings Program contracts could be stratified by race and ethnicity, and ACOs could be required to meet standards of high quality of care for minority groups to be eligible for shared savings.33
Furthermore, extending ACO programs to providers that disproportionately serve disadvantaged patients—particularly those not yet integrated into ACO-eligible groups—may be necessary to limit unintended effects of ACO programs on disparities. The Medicare Advance Payment ACO Model, for example, provides initial payments to ACOs with insufficient resources to develop the infrastructure necessary for care management and quality improvement.34 To the extent that ACO incentives improve overall quality for ACO patients, our results suggest that initiatives involving more fragmented parts of the delivery system would affect larger proportions of black patients.
Our study had several limitations. First, we identified provider groups sufficiently large to participate in ACO programs, but not actual participants. Participating organizations may differ from other size-eligible organizations in structural capabilities that could influence quality and disparities. Nevertheless, larger provider groups are much more likely to participate in ACO programs than smaller groups,31 suggesting that differences in disparities between ACOs and other providers should be reflected in our results. Furthermore, compared with analyses of early ACOs, our analyses of size-eligible groups may better generalize to future sets of organizations participating in the rapidly growing Shared Savings Program.35
Second, because our analysis relied on administrative claims data, we could not examine disparities in disease control. Even in a large well-integrated provider group focused on reducing racial disparities, prior research has shown how difficult it can be to eliminate disparities in measures of disease control.19,36–38 Third, like readmission rates, AHRQ indicators of potentially avoidable hospitalizations may reflect market-level or organizational drivers of admissions other than the quality of ambulatory care.39 Such factors, however, would be expected to affect both black and white beneficiaries in a given provider group or county, and thus would not likely obscure strong relationships between overall rates and disparities in rates of truly preventable hospitalizations. Finally, due to limitations of the Medicare enrollment data we analyzed, we were unable to examine disparities in quality of care for racial or ethnic minority groups other than black adults.21,22
The impact of ACOs on racial disparities in quality will not be known for several years. Nevertheless, our findings are consistent with concerns that quality improvements achieved by Medicare ACO programs may not be associated with substantial reductions in health disparities, and may even be associated with larger disparities nationally if these programs disproportionately engage physicians and hospitals serving fewer minority patients. Additional incentives and novel payment arrangements may be required for ACOs to promote greater equity in care.
Electronic supplementary material
(DOCX 50 kb)
Acknowledgements
Funders: Supported by grants from the Doris Duke Charitable Foundation (Clinical Scientist Development Award #2010053), Beeson Career Development Award Program (National Institute on Aging K08 AG038354 and the American Federation for Aging Research), National Institute on Aging (P01 AG032952), the Malcolm Weiner Center at Harvard Kennedy School, the Dean’s Summer Research Fellowship at Washington University School of Medicine, St. Louis, and by the Health Disparities Research Program of Harvard Catalyst/The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers).
Prior Presentations
Society of General Internal Medicine Annual Meeting, 26 April 2013 (poster presentation)
AcademyHealth Annual Research Meeting, 24 June 2013 (oral presentation)
Conflicts of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.McClellan M, McKethan AN, Lewis JL, Roski J, Fisher ES. A national strategy to put accountable care into practice. Health Aff (Millwood) 2010;29(5):982–990. doi: 10.1377/hlthaff.2010.0194. [DOI] [PubMed] [Google Scholar]
- 2.Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations; Final Rule, 42 CFR Part 425. (2011). [PubMed]
- 3.Lewis VA, Larson BK, McClurg AB, Boswell RG, Fisher ES. The promise and peril of accountable care for vulnerable populations: a framework for overcoming obstacles. Health Aff (Millwood) 2012;31(8):1777–1785. doi: 10.1377/hlthaff.2012.0490. [DOI] [PubMed] [Google Scholar]
- 4.Pollack CE, Armstrong K. Accountable care organizations and health care disparities. JAMA. 2011;305(16):1706–1707. doi: 10.1001/jama.2011.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 6.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005;43(4):308–319. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spertus JA, Jones PG, Masoudi FA, Rumsfeld JS, Krumholz HM. Factors associated with racial differences in myocardial infarction outcomes. Ann Intern Med. 2009;150(5):314–324. doi: 10.7326/0003-4819-150-5-200903030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Groeneveld PW, Laufer SB, Garber AM. Technology diffusion, hospital variation, and racial disparities among elderly Medicare beneficiaries: 1989–2000. Med Care. 2005;43(4):320–329. doi: 10.1097/01.mlr.0000156849.15166.ec. [DOI] [PubMed] [Google Scholar]
- 11.Rittenhouse DR, Casalino LP, Gillies RR, Shortell SM, Lau B. Measuring the medical home infrastructure in large medical groups. Health Aff (Millwood) 2008;27(5):1246–1258. doi: 10.1377/hlthaff.27.5.1246. [DOI] [PubMed] [Google Scholar]
- 12.Rittenhouse DR, Shortell SM, Gillies RR, et al. Improving chronic illness care: findings from a national study of care management processes in large physician practices. Med Care Res Rev. 2010;67(3):301–320. doi: 10.1177/1077558709353324. [DOI] [PubMed] [Google Scholar]
- 13.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small and medium-size physician practices use few patient-centered medical home processes. Health Aff (Millwood) 2011;30(8):1575–1584. doi: 10.1377/hlthaff.2010.1210. [DOI] [PubMed] [Google Scholar]
- 14.Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289(4):434–441. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- 15.Friedberg MW, Safran DG, Coltin KL, Dresser M, Schneider EC. Readiness for the Patient-Centered Medical Home: structural capabilities of Massachusetts primary care practices. J Gen Intern Med. 2009;24(2):162–169. doi: 10.1007/s11606-008-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McWilliams JM, Chernew ME, Zaslavsky AM, Hamed P, Landon BE. Delivery System Integration and Health Care Spending and Quality for Medicare Beneficiaries. JAMA Intern Med. 2013;173(15):1447–1456. doi: 10.1001/jamainternmed.2013.6886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 18.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 19.Sequist TD, Adams A, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of quality improvement on racial disparities in diabetes care. Arch Intern Med. 2006;166(6):675–681. doi: 10.1001/archinte.166.6.675. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Medicare and Medicaid Services. Chronic Condition Data Warehouse. Available at: http://www.ccwdata.org/index.htm. Accessed May 7, 2014.
- 21.Zaslavsky AM, Ayanian JZ, Zaborski LB. The validity of race and ethnicity in enrollment data for Medicare beneficiaries. Health Serv Res. 2012;47(3 Pt 2):1300–1321. doi: 10.1111/j.1475-6773.2012.01411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arday SL, Arday DR, Monroe S, Zhang J. HCFA’s racial and ethnic data: current accuracy and recent improvements. Health Care Financ Rev. 2000;21(4):107–116. [PMC free article] [PubMed] [Google Scholar]
- 23.Yun H, Kilgore ML, Curtis JR, et al. Identifying types of nursing facility stays using medicare claims data: an algorithm and validation. Health Serv Outcome Res Methodol. 2010;10(1):100. doi: 10.1007/s10742-010-0060-4. [DOI] [Google Scholar]
- 24.McWilliams JM, Chernew ME, Zaslavsky AM, Landon BE. Post-acute care and ACOs—who will be accountable? Health Serv Res. 2013;48(4):1526–1538. doi: 10.1111/1475-6773.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agency for Healthcare Research and Quality. Prevention Quality Indicators Overview. Available at: http://www.qualityindicators.ahrq.gov/modules/pqi_resources.aspx. Accessed May 7, 2014.
- 26.Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: A profile at state and national levels. JAMA. 2000;284(13):1670–1676. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- 27.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998–1999 to 2000–2001. JAMA. 2003;289(3):305–312. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Census Bureau. 2010 American Community Survey 5-year estimates. Available at: http://factfinder2.census.gov. Accessed May 7, 2014.
- 29.Huber P. The Behavior of Maximum Likelihood Estimates Under Non-standard Conditions. Berkeley: University of California Press; 1967. [Google Scholar]
- 30.White H. Maximum likelihood estimation of misspecified models. Econometrica. 1982;50:1–26. doi: 10.2307/1912526. [DOI] [Google Scholar]
- 31.Auerbach DI, Liu H, Hussey PS, Lau C, Mehrotra A. Accountable care organization formation is associated with integrated systems but not high medical spending. Health Aff (Millwood) 2013;32(10):1781–1788. doi: 10.1377/hlthaff.2013.0372. [DOI] [PubMed] [Google Scholar]
- 32.Pioneer Accountable Care Organization (ACO) Model Request for Application. Washington, DC: Department of Health and Human Services and Centers for Medicare and Medicaid Services; 2011. [Google Scholar]
- 33.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 34.Center for Medicare and Medicaid Innovation. Advance Payment ACO Model. Available at: http://innovation.cms.gov/initiatives/Advance-Payment-ACO-Model. Accessed May 7, 2014.
- 35.Centers for Medicare and Medicaid Services. More partnerships between doctors and hospitals strengthen coordinated care for Medicare beneficiaries. Available at: http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-Releases/2013-Press-Releases-Items/2013-12-23.html. Accessed May 7, 2014.
- 36.Sequist TD, Fitzmaurice GM, Marshall R, et al. Cultural competency training and performance reports to improve diabetes care for black patients: a cluster randomized, controlled trial. Ann Intern Med. 2010;152(1):40–46. doi: 10.7326/0003-4819-152-1-201001050-00009. [DOI] [PubMed] [Google Scholar]
- 37.Thorlby R, Jorgensen S, Ayanian JZ, Sequist TD. Clinicians' views of an intervention to reduce racial disparities in diabetes outcomes. J Natl Med Assoc. 2011;103(9–10):968–977. doi: 10.1016/s0027-9684(15)30454-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones RG, Trivedi AN, Ayanian JZ. Factors influencing the effectiveness of interventions to reduce racial and ethnic disparities in health care. Soc Sci Med. 2010;70(3):337–341. doi: 10.1016/j.socscimed.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 50 kb)