ABSTRACT
BACKGROUND
Expansion of health insurance coverage, and hence clinical preventive services (CPS), provides an opportunity for improvements in the health of adults. The degree to which expansion of health insurance coverage affects the use of CPS is unknown.
OBJECTIVE
To assess whether Massachusetts health reform was associated with changes in healthcare access and use of CPS.
DESIGN
We used a difference-in-differences framework to examine change in healthcare access and use of CPS among working-aged adults pre-reform (2002–2005) and post-reform (2007–2010) in Massachusetts compared with change in other New England states (ONES).
SETTING
Population-based, cross-sectional Behavioral Risk Factor Surveillance System surveys.
PARTICIPANTS
A total of 208,831 survey participants aged 18 to 64 years.
INTERVENTION
Massachusetts health reform enacted in 2006.
MEASUREMENTS
Four healthcare access measures outcomes and five CPS.
KEY RESULTS
The proportions of adults who had health insurance coverage, a healthcare provider, no cost barrier to healthcare, an annual routine checkup, and a colorectal cancer screening increased significantly more in Massachusetts than those in the ONES. In Massachusetts, the prevalence of cervical cancer screening in pre-reform and post-reform periods was about the same; however, the ONES had a decrease of −1.6 percentage points (95 % confidence interval [CI] −2.5, −0.7; p <0.001). As a result, the prevalence of cervical cancer screening in Massachusetts was increased relative to the ONES (1.7, 95 % CI 0.2, 3.2; p = 0.02). Cholesterol screening, influenza immunization, and breast cancer screening did not improve more in Massachusetts than in the ONES.
LIMITATIONS
Data are self-reported.
CONCLUSIONS
Health reform may increase healthcare access and improve use of CPS. However, the effects of health reform on CPS use may vary by type of service and by state.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2865-2) contains supplementary material, which is available to authorized users.
KEY WORDS: health insurance, healthcare access, clinical preventive services
BACKGROUND
The 2010 Affordable Care Act (ACA; PL 111–148; PL 111–152)1 provides an important opportunity to substantially improve the health of all adults in the United States (U.S.)2–4 by providing access to clinical preventive services (CPS) through wider access to health insurance coverage. The ACA, in addition to extending insurance coverage to more people, provides for coverage without cost-sharing for CPS given an A or B recommendation by the U.S. Preventive Services Task Force (USPSTF)1 and for immunizations recommended by the Advisory Committee on Immunization Practices (ACIP).5
The potential impact of the ACA on use of adult CPS may be informed by the experience in Massachusetts, which passed comprehensive health reform legislation in April, 2006 that included coverage for preventive services but, unlike the ACA, with cost-sharing.6,7 Researchers have used a number of different surveys8–19 to examine potential impacts of the Massachusetts (MA) health reform legislation on health insurance coverage, barriers to use of services, and service use both overall and among different segments of the Massachusetts population. Some of this research has compared coverage, barriers, and use in Massachusetts with experiences in other states.16,19–22 This research has generally reported that in Massachusetts, health insurance coverage increased after passage of health reform,9,11,16,19,20,22 that barriers to service use were reduced,9,11,16,20,22 and use of clinical services increased.9,12 In addition, these improvements have been found to be greater in Massachusetts than in comparison groups of other New England states (ONES).19,20,22 However, none of the reports examined changes in use of the CPS recommended by the USPSTF and ACIP and identified in the ACA.
Considering that Massachusetts may provide an example of how implementation of the ACA may increase use of CPS, for this study data collected from the U.S. Centers for Disease Control and Prevention’s (CDC) state-based telephone survey, the Behavioral Risk Factor Surveillance System (BRFSS),23,24 were used to examine changes in use of adult CPS recommended by the USPSTF and ACIP after passage of health reforms in Massachusetts. The proportions of adults using these CPS before health reform was passed (2002 through 2005) and after health reform (2007 through 2010) in Massachusetts were contrasted with those proportions in five neighboring ONES (Connecticut, Maine, New Hampshire, Rhode Island, and Vermont) that did not pass health reform legislation. This examination focused on adults aged 18 to 64 years.
We hypothesized that, compared to the ONES, Massachusetts would have a greater increase in the proportions of adults aged 18 to 64 years (working-aged) with increased healthcare access. We also hypothesized that, in a 4-year post-health reform period, a greater increase in the proportions of working-aged Massachusetts adults with increased use of CPS than in the ONES would be found.
METHODS
Design Overview
Established in 1984, the BRFSS is an ongoing, state-based, random-digit-dialed telephone survey conducted by state health departments in collaboration with the CDC. Data regarding health risk behaviors, healthcare access, and use of CPS, primarily related to chronic disease, injury, and infectious disease, are obtained monthly through telephone surveys of randomly selected community-dwelling adults aged ≥ 18 years in each state.23,24 Prevalence estimates derived from the BRFSS have been shown to be valid and reliable compared with other national surveys.25,26 All BRFSS questionnaires, data, and reports are available at www.cdc.gov/BRFSS. Institutional review board approval was not necessary because this study involved analysis of publicly available surveillance data.
In this study, changes in healthcare access and use of the adult CPS recommended by USPSTF and ACIP in Massachusetts between pre-reform (2002 through 2005) and post-reform (2007 through 2010) were compared, and contrasted with pre-reform to post-reform changes in access and service use in five ONES. These states were chosen as the comparison group unexposed to the 2006 Massachusetts health reform, and because of the geographic, socioeconomic, and cultural similarities they share with Massachusetts. All analyses were conducted in 2012. Among the six states, the median BRFSS cooperation rate ranged from 70.9 in 2002 to 76.4 % in 2010 (minimum: 65.0 in 2007; maximum: 76.4 % in 2010), and the median BRFSS response rate ranged from 52.0 in 2002 to 49.7 % in 2010 (minimum: 39.3 in 2007; maximum: 52.0 % in 2002).
The final sample was 208,831 (66,788 from Massachusetts [32 %] and 142,043 from the ONES [68 %]). Respondents with incomplete data (i.e., missing data, don’t know/not sure response, or refused to answer) and those who may have qualified for extra coverage because of age or pregnancy were excluded from the final sample.27 Respondent characteristics used in this analysis included age, sex, race/ethnicity, education, employment status, marital status, household size, annual household income, and general health status. Because the USPSTF and ACIP recommendations are for specific age categories of men and/or women, those analyses were based on relevant subsamples. In addition, sample sizes for specific outcomes varied because questions for some outcomes were not asked each year.
Outcomes
Table 1 lists definitions for four healthcare access outcomes and five CPS recommended by the USPSTF and ACIP, for which data are collected in BRFSS. BRFSS data on respondent health insurance coverage, healthcare access (having a healthcare provider, financial barriers to care, and having a medical checkup in the past year), and CPS (five different outcomes recommended by the USPSTF and ACIP and identified in the ACA, as shown in Table 1) were assessed. Responses for having a usual healthcare provider were dichotomized into “one or more” and “none,” and responses for having had a medical checkup in the past year into “within the past year” or “not within the past year.” The wording of the questions from year to year was assessed for consistency. Except for cervical cancer screening, colorectal cancer screening, and influenza immunization, the wording of survey questions was consistent across all years for all outcomes.
Table 1.
Characteristics of Measures of Healthcare Access and Use of Clinical Preventive Services*
| Measure | Definition | Age group, years | Years |
|---|---|---|---|
| Healthcare access | |||
| Health insurance coverage | Had any kind of healthcare coverage | 18–64 | 2002, 2003, 2004, 2005, 2007, 2008, 2009, 2010 |
| Usual source of healthcare | Had personal doctor(s) or healthcare provider(s) | 18–64 | 2002, 2003, 2004, 2005, 2007, 2008, 2009, 2010 |
| Cost barrier to healthcare | Had unmet needed healthcare in the past 12 months because of cost | 18–64 | 2003, 2004, 2005, 2007, 2008, 2009, 2010 |
| Routine medical checkup | Received routine checkup in past year | 18–64 | 2005, 2007, 2008, 2009, 2010 |
| Clinical preventive services | |||
| Breast cancer screening† | Received mammogram in past 2 years | 50–64 | 2002, 2004, 2008, 2010 |
| Cervical cancer screening | Received Papanicolaou test in past 3 years (women with an intact uterus) | 21–64 | 2002, 2004, 2008, 2010 |
| Colorectal cancer screening | Received fecal occult blood test in past year or sigmoidoscopy or colonoscopy in past 5 years | 50–64 | 2002, 2004, 2008, 2010 |
| Cholesterol screening | Received cholesterol screening in past 5 years | men, 35–64; women, 45–64 | 2003, 2005, 2007, 2009 |
| Influenza immunization‡ | Received influenza vaccine in past year | 50–64 | 2002, 2003, 2004, 2005, 2007, 2008, 2009, 2010 |
*Affordable care act preventive services mandate (PL 111–148; PL 111–152)
†The affordable care act will require coverage of mammograms beginning at age 40 years
‡In 2004, a question was added to capture introduction of the nasal influenza vaccine. In 2005, the introductory wording for the influenza injection question changed and wording was added to define the nasal influenza vaccine as FluMist™. The introductory wording was changed on both influenza questions in 2010
Statistical Analysis
Due to insufficient repeated observations over BRFSS survey years, the data did not satisfy a time-series panel structure required for an interrupted time-series design. Thus, we used a difference-in-differences (DiD) framework to estimate change in healthcare access and in use of CPS in Massachusetts with equivalent changes in the ONES (Online Appendix).28–30 Logistic regression modeling was used to estimate the prevalence of healthcare access and use of CPS outcomes and their 95 % confidence intervals (CIs), both unadjusted and adjusted for age, gender, race/ethnicity, education, employment status, marital status, household size, annual household income, and general health status. Because the exclusion of respondents with missing information on characteristics used for the adjusted analysis may have affected study results, the unadjusted analysis was performed on both the study population for which needed data on healthcare access and use of CPS were available and on the study population for which complete information on the characteristics used in the adjusted analysis were also available. SAS31 and SAS-callable SUDAAN32 and respondent weights were used in all analyses to account for the complex survey design of the BRFSS.
Results
Characteristics of Study Respondents
In both the pre-reform and post-reform periods, Massachusetts and the ONES had similar proportions in terms of gender, those residing in a household with an annual income <$25,000, and reporting fair or poor health (Table 2). In the pre-reform period, Massachusetts and the ONES had similar composition in terms of proportions with less than a high school education, those unable to work, and respondents having an annual household income <$25,000. In the post-reform period, the average age in both groups was 42 years, and Massachusetts and the ONES had similar composition in terms of marital status and working-aged adults who were unemployed.
Table 2.
Characteristics of Massachusetts and Other New England States’ Working-Aged Adults Pre-reform (2002–2005) and Post-reform (2007–2010)
| Characteristics | 2002–2005 Pre-reform | 2007–2010 Post-reform | ||
|---|---|---|---|---|
| Massachusetts (n = 21,750) | ONES (n = 63,390) | Massachusetts (n = 45,038) | ONES (n = 78,653) | |
| % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| Age (years) | ||||
| 18–34 | 35.1 (34.2,36.0) | 32.3 (31.8,32.9) | 28.3 (27.5,29.1) | 30.2 (29.6,30.9) |
| Age (years; mean) | 40.3 (40.1,40.6) | 41.0 (40.8,41.1) | 42.1 (41.9,42.3) | 42.2 (42.0,42.4) |
| Sex | ||||
| Female | 49.6 (48.7,50.5) | 49.3 (48.7,49.9) | 49.8 (49.1,50.6) | 49.3 (48.7,49.9) |
| Race/ethnicity | ||||
| White, non-Hispanic | 82.8 (82.1,83.5) | 87.4 (87.0,87.9) | 79.0 (78.3,79.7) | 87.5 (87.1,88.0) |
| Black, non-Hispanic | 3.8 (3.5,4.1) | 3.1 (2.9,3.3) | 5.0 (4.7,5.4) | 2.7 (2.5,3.0) |
| Hispanic | 8.3 (7.8,8.8) | 5.6 (5.3,5.9) | 8.6 (8.2,9.1) | 5.3 (5.0,5.6) |
| Other, non-Hispanic | 5.1 (4.7,5.5) | 3.9 (3.6,4.1) | 7.3 (6.9,7.8) | 4.4 (4.1,4.7) |
| Education | ||||
| <High school | 6.4 (5.9,6.9) | 6.0 (5.8,6.3) | 5.3 (4.9,5.7) | 4.5 (4.3,4.8) |
| High school | 23.1 (22.3,23.8) | 27.7 (27.3,28.2) | 21.4 (20.8,22.0) | 24.8 (24.3,25.3) |
| Some college | 24.8 (24.0,25.6) | 25.9 (25.4,26.4) | 23.3 (22.7,24.0) | 25.1 (24.6,25.6) |
| ≥College | 45.8 (44.9,46.7) | 40.3 (39.8,40.8) | 50.0 (49.2,50.8) | 45.6 (45.0,46.2) |
| Marital status | ||||
| Married | 57.4 (56.5,58.3) | 60.7 (60.2,61.3) | 64.0 (63.2,64.8) | 64.2 (63.6,64.8) |
| Previously married | 12.7 (12.2,13.2) | 13.8 (13.5,14.1) | 11.6 (11.2,12.0) | 11.8 (11.5,12.1) |
| Never married | 29.9 (29.0,30.8) | 25.5 (24.9,26.0) | 24.4 (23.7,25.1) | 24.0 (23.3,24.6) |
| Employment status | ||||
| Employed for wages | 66.5 (65.7,67.4) | 66.7 (66.2,67.2) | 68.4 (67.7,69.1) | 65.4 (64.8,65.9) |
| Self-employed | 9.5 (9.0,10.0) | 11.0 (10.7,11.4) | 9.0 (8.6,9.4) | 10.5 (10.1,10.8) |
| Unemployed | 6.3 (5.8,6.7) | 5.3 (5.0,5.5) | 6.4 (6.0,6.8) | 6.4 (6.1,6.7) |
| Student/Homemaker/Retired | 13.8 (13.2,14.5) | 13.3 (12.9,13.7) | 11.6 (11.1,12.1) | 13.6 (13.1,14.0) |
| Unable to work | 3.9 (3.6,4.3) | 3.8 (3.6,3.9) | 4.6 (4.4,4.9) | 4.2 (4.0,4.4) |
| Household size (mean) | 3.2 (3.1,3.2) | 3.1 (3.1,3.1) | 3.3 (3.3,3.4) | 3.2 (3.2,3.2) |
| Annual household income | ||||
| <$25 K | 17.3 (16.6,18.0) | 17.7 (17.3,18.1) | 15.4 (14.9,16.0) | 14.8 (14.4,15.2) |
| $25 K − <$50 K | 23.9 (23.1,24.6) | 27.2 (26.7,27.7) | 18.2 (17.6,18.8) | 20.9 (20.4,21.4) |
| ≥$50 K | 58.9 (58.0,59.7) | 55.1 (54.5,55.6) | 66.4 (65.7,67.1) | 64.3 (63.8,64.9) |
| Self-rated general health | ||||
| Excellent | 28.9 (28.1,29.7) | 28.1 (27.6,28.6) | 28.5 (27.8,29.1) | 26.0 (25.5,26.5) |
| Very good | 36.8 (36.0,37.7) | 37.6 (37.1,38.1) | 37.5 (36.8,38.3) | 39.2 (38.6,39.7) |
| Good | 24.6 (23.8,25.4) | 24.6 (24.1,25.1) | 24.6 (23.9,25.2) | 25.3 (24.8,25.8) |
| Fair | 7.4 (7.0,7.9) | 7.4 (7.1,7.7) | 7.3 (6.9,7.6) | 7.2 (6.9,7.5) |
| Poor | 2.3 (2.0,2.5) | 2.3 (2.1,2.5) | 2.2 (2.0,2.4) | 2.4 (2.2,2.5) |
n sample size, % weighted percentage, CI confidence interval, ONES other New England states
Healthcare Access and CPS Outcomes
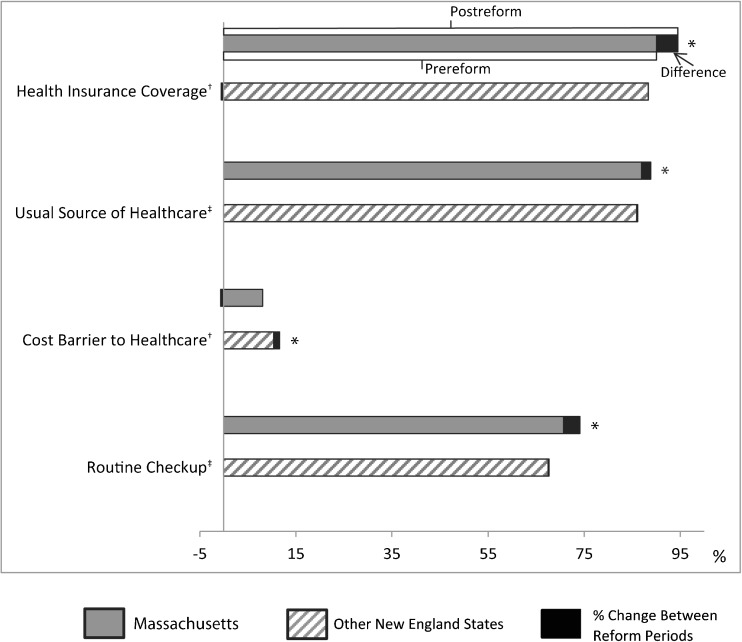
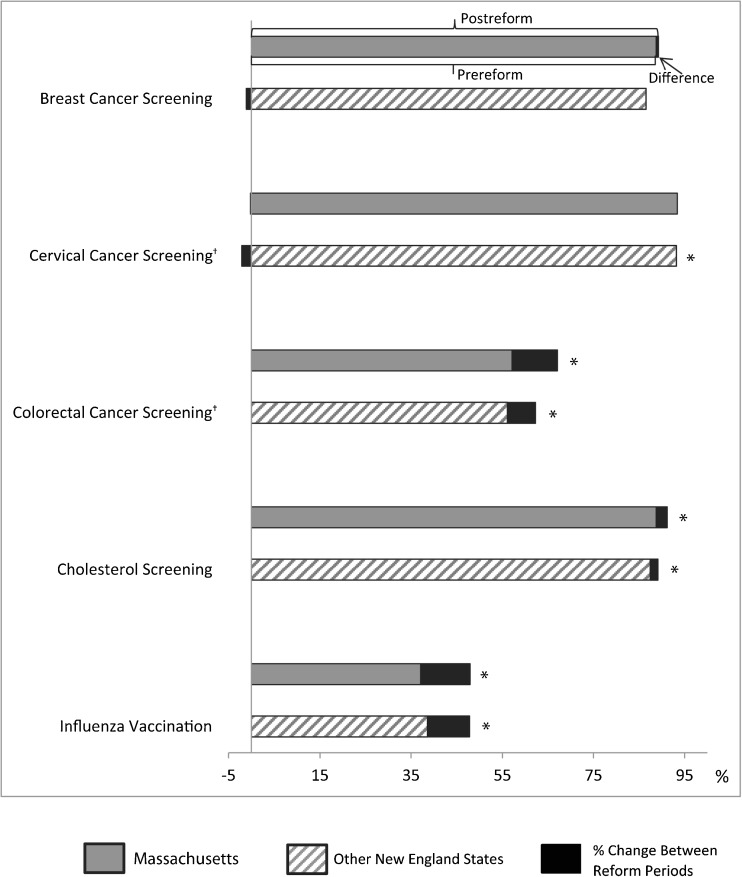
Unadjusted and adjusted pre-reform (2002–2005) and post-reform (2007–2010) prevalence estimates for the healthcare access and CPS outcomes and the changes in prevalence between these two periods for Massachusetts and the ONES are presented in the Online Appendix and Table 3, respectively. The adjusted results are also depicted in Figs. 1 and 2.
Table 3.
Adjusted Prevalence Estimates of Healthcare Access and Clinical Preventive Services* Use and Change Between Pre-reform (2002–2005) and Post-reform (2007–2010) Period, and Massachusetts and Other New England States
| Massachusetts | Other New England States | DiD† | |||||
|---|---|---|---|---|---|---|---|
| Post-reform | Pre-reform | Differences | Post-reform | Pre-reform | Differences | ||
| % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| Healthcare access‡ | |||||||
| Health insurance coverage (n = 208,831) | 94.4 (94.1,94.8) | 90.0 (89.5,90.5) | 4.5¶ (3.8,5.1) | 87.8 (87.4,88.2) | 88.3 (88.0,88.7) | −0.5 (−1.0,0.1) | 4.9¶ (4.1,5.8) |
| Usual source of healthcare (n = 208,545) | 88.8 (88.3,89.3) | 86.9 (86.3,87.5) | 1.9¶ (1.1,2.7) | 86.1 (85.6,86.5) | 85.9 (85.5,86.3) | 0.2 (−0.4,0.8) | 1.7‖ (0.7,2.7) |
| Cost barrier to healthcare in the past 12 months (n = 189,029) | 7.5 (7.1,7.9) | 8.1 (7.6,8.6) | −0.6 (−1.3,0.0) | 11.6 (11.2,12.0) | 10.4 (10.0,10.8) | 1.2¶ (0.7,1.8) | −1.9¶ (−2.8,-1.0) |
| Routine checkup within the past year (n = 145,907) | 74.1 (73.4,74.8) | 70.7 (69.0,72.4) | 3.4¶ (1.6,5.2) | 67.6 (67.1,68.2) | 67.5 (66.3,68.6) | 0.2 (−1.1,1.5) | 3.2‖ (1.0,5.4) |
| Clinical preventive services | |||||||
| Breast cancer screening | |||||||
| Mammogram within the past 2 years, women aged 50–64 years (n = 25,197) | 89.2 (88.0,90.3) | 88.7 (87.0,90.5) | 0.5 (−1.6,2.6) | 85.4 (84.4,86.4) | 86.5 (85.4,87.6) | −1.1 (−2.6,0.4) | 1.6 (−1.0,4.2) |
| Cervical cancer screening | |||||||
| Papanicolaou test within the past 3 years, women aged 21–64 years (n = 50,900) | 93.2 (92.4,94.0) | 93.4 (92.5,94.3) | −0.2 (−1.4,1.0) | 91.1 (90.4,91.8) | 93.2 (92.7,93.8) | −2.1¶ (−3.0,-1.2) | 1.9§ (0.5,3.4) |
| Colorectal cancer screening | |||||||
| Fecal occult blood test within the past year or sigmoidoscopy/colonoscopy within the past 5 years, adults aged 50–64 years (n = 42,421) | 67.1 (65.7,68.4) | 57.1 (54.9,59.3) | 10.0¶ (7.4,12.5) | 62.3 (61.3,63.4) | 56.1 (54.8,57.4) | 6.2¶ (4.6,7.9) | 3.8§ (0.7,6.8) |
| Cardiovascular screening | |||||||
| Cholesterol screening within the past 5 years, men aged 35–64 years and women aged 45–64 years (n = 68,671) | 91.2 (90.5,91.9) | 88.7 (87.7,89.7) | 2.5¶ (1.3,3.7) | 89.1 (88.5,89.6) | 87.4 (86.8,88.1) | 1.7¶ (0.8,2.5) | 0.8 (−0.6,2.3) |
| Immunization | |||||||
| Influenza vaccination within the past year, adults aged 50–64 years (n = 86,934) | 47.9 (46.9,48.9) | 37.1 (35.6,38.5) | 10.8¶ (9.1,12.6) | 47.9 (47.1,48.6) | 38.6 (37.8,39.5) | 9.2¶ (8.1,10.4) | 1.6 (−0.5,3.7) |
% weighted percentage, CI confidence interval, DiD difference-in-differences. Adjusted for gender (where applicable), age (where applicable), race/ethnicity, education, employment status, marital status, household size, annual household income, and general health status
*Affordable care act preventive services mandate (PL 111–148; PL 111–152)
†DiD: difference in adjusted prevalence between post-reform (2007–2010) and pre-reform (2002–2005) years in Massachusetts minus that difference in other New England States
‡Adults aged 18–64 years
§ p <0.05; ‖ p <0.01; and ¶ p <0.001
Figure 1.
Adjusted prevalence estimates of healthcare access and change between pre-reform (2002–2005) and post-reform (2007–2010) periods. *p <0.001. †, ‡: Statistically significant difference in adjusted prevalence between post-reform and pre-reform years in Massachusetts minus that difference in other New England states (p <0.001 and p <0.01, respectively).
Figure 2.
Adjusted prevalence estimates of clinical preventive services and change between pre-reform (2002–2005) and post-reform (2007–2010) periods. *p <0.001. †Statistically significant difference in adjusted prevalence between post-reform and pre-reform years in Massachusetts minus that difference in other New England states (p <0.05).
Health Insurance Coverage
After adjustment, the prevalence of health insurance coverage for working-aged MA adults was 90.0 % in the pre-reform period and 94.4 % in the post-reform period; a statistically significant increase of 4.5 % (95 % CI 3.8, 5.1; p <0.001; Fig. 1; Table 3). However, the adjusted prevalence of health insurance coverage for working-aged ONE adults remained relatively stable between these two reform periods (88.3 and 87.8 %, respectively; −0.5, 95 % CI −1.0, 0.1). Thus, the adjusted change in health insurance coverage in Massachusetts increased more than that in the ONES (DiD = 4.9, 95 % CI 4.1, 5.8; p <0.001; Fig. 1; Table 3).
Other Healthcare Access Outcomes
In Massachusetts, the adjusted prevalence of having a usual healthcare provider and having a routine medical checkup in the past year increased statistically significantly from the pre-reform period to the post-reform period (1.9, 95 % CI 1.1, 2.7; p <0.001 and 3.4, 95 % CI 1.6, 5.2; p <0.001, respectively; Fig. 1; Table 3), whereas, after adjustment, the prevalence of unmet healthcare due to cost remained relatively stable between these two reform periods (−0.6 percentage point, 95 % CI −1.3, −0.0). In the ONES, after adjustment, the only healthcare access outcome that increased significantly between reform periods was unmet healthcare due to cost (1.2, 95 % CI 0.7, 1.8; p <0.001; Fig. 1; Table 3). The increase in having a usual healthcare provider and a routine medical checkup in Massachusetts significantly exceeded that for the ONES (1.7, 95 % CI 0.7, 2.7 and 3.2, 95 % CI 1.0, 5.4, respectively); as did the decrease in having unmet healthcare due to cost (−1.9, 95 % CI −2.8, −1.0; Fig. 1; Table 3).
Breast Cancer Screening
In both Massachusetts and the ONES, the adjusted prevalence of breast cancer screening for women aged 50 to 64 years remained relatively stable between the pre-reform and the post-reform periods (Fig. 2 and Table 3). Thus, the adjusted change in this screening was similar between Massachusetts and the ONES (1.6, 95 % CI −1.0, 4.2) (Table 3).
Cervical Cancer Screening
In Massachusetts, the adjusted prevalence of cervical cancer screening in pre-reform and post-reform periods was approximately the same for women aged 21 to 64 years (−0.2, 95 % CI −1.4, 1.0). However, the ONES experienced a statistically significant decrease in the adjusted prevalence (−2.1, 95 % CI −3.0, −1.2; p <0.001; Fig. 2 and Table 3). As a result, the adjusted prevalence receiving a Papanicolaou test in Massachusetts was increased relative to the ONES (1.9, 95 % CI 0.5, 3.4; p = 0.01, respectively; Fig. 2 Table 3).
Colorectal Cancer Screening
In both Massachusetts and the ONES, the adjusted prevalence of colorectal cancer screening for adults aged 50 to 64 years increased statistically significantly from the pre-reform period to the post-reform period (10.0, 95 % CI 7.4, 12.5 and 6.2, 95 % CI 4.6, 7.9, respectively; p <0.001 for both; Fig. 2; Table 3). However, the adjusted change in colorectal cancer screening in Massachusetts increased more than that in the ONES (3.8, 95 % CI 0.7, 6.8; p = 0.02; Fig. 2; Table 3).
Cholesterol Screening
In both Massachusetts and the ONES, the adjusted prevalence for having a cholesterol screening in the past 5 years (for men aged 35 to 64 years and women aged 45 to 64 years) was statistically significantly higher in post-reform than pre-reform (2.5, 95 % CI 1.3, 3.7 and 1.7, 95 % CI 0.8, 2.5, respectively; p <0.001 for both; Fig. 2; Table 3). The adjusted change in this screening was similar between Massachusetts and the ONES (0.8, 95 % CI −0.6, 2.3; Table 3).
Influenza Immunization
The adjusted prevalence of having an annual influenza immunization for both Massachusetts and ONES adults aged 50 to 64 years increased by approximately 10 percentage points from the pre-reform period to the post-reform period (10.8, 95 % CI 9.1, 12.6; p <0.001 and 9.2, 95 % CI 8.1, 10.4, respectively; p <0.001 for both; Fig. 2 and Table 3). Thus, the adjusted change in influenza immunization was similar between Massachusetts and the ONES (1.6, 95 % CI −0.5, 3.7; Table 3).
DISCUSSION
Using a naturally occurring framework, we had several key findings. We found greater improvement in Massachusetts than in ONES in access to healthcare, including health insurance coverage, having a usual healthcare provider, having a routine checkup, and not having unmet healthcare needs due to cost. Of the CPS, Massachusetts appeared to have greater increases in colorectal cancer screening and not to have had a decline in cervical cancer screening as was observed in the ONES.
To the best of our knowledge, this analysis is the first to examine the effects of health reform on use of CPS in Massachusetts in comparison with the ONES, though other researchers have examined its impact on use of preventive services within the state.9,12,17 In general, our findings of changes over time within Massachusetts were similar to the findings in these previous studies.
The first hypothesis of a higher increase in health insurance coverage between pre-reform and post-reform in Massachusetts as compared to the ONES was supported. The second hypothesis that, in a 4 year post-health reform period, there would be a greater increase in the proportions of working-aged Massachusetts adults with increased use of CPS than in the ONES is somewhat nuanced. On the surface, some of the findings indicate little or no significant difference-in-differences between MA and ONES, and between pre-reform and post-reform periods. This may be an artifact of already high prevalence of breast and cervical cancer and cardiovascular screenings, leaving little room for improvement in absolute terms. Despite strong evidence of its effectiveness, colorectal cancer screening prevalence33 continues to lag behind that of other screening-amenable cancers (i.e., breast and cervical)34,35 but now appears to show a secular improvement in both MA and ONES, with relatively higher improvement in MA.
These findings may indicate that of the increased proportions of newly insured individuals in Massachusetts, approximately 74 % were able to access primary care services to obtain a routine checkup compared to approximately 45 % in the ONES, and, hence may have increased use of CPS in Massachusetts (adjusted: ∼75 % vs. ∼−40 %, respectively). Nevertheless, given that the improvements in use of services were small relative to the changes in the ONES and that CPS are underutilized even in insured populations,36,37 improving more than access to care may be needed to improve use of these services. Stakeholders may need to take additional steps to implement proven strategies to increase use of CPS.36 Research has demonstrated that a number of health system-based and community-based interventions can be effective in increasing use of CPS.38 Such interventions include helping new patients find a doctor (especially one with whom there can be reciprocal communications),9,13,16 and using patient tracking systems (e.g., patient and provider reminders about the need for and timing of CPS).36,38 Various communications and education strategies for the public also have been found to increase service use. For example, Colorado formed a prevention council, to ensure stakeholders would reach consensus on the minimum health standards of recommendations for CPS, with the goal of establishing clarity on the recommended CPS for healthcare providers and consumers alike.39.
The impact of health reform for other states on the use of preventive services is uncertain. Although it seems logical that, as a greater proportion of the population obtains insurance coverage, access to services would improve and that use of CPS would increase, state experiences may vary substantially due to differences in coverage, access, and use of such services before health reform. Even with national legislation, states and communities, health insurers, and care providers are largely responsible for implementation of the reform in terms of how Medicaid systems are changed, how health insurance develops, and what provisions are instituted for cost-sharing and subsidies.36 Furthermore, the social, cultural, and political norms of each state and their human and financial resources may temper or intensify improvement in CPS use.7,40–42
This study has limitations. First, the BRFSS has suffered from declines in response rate largely due to the increased prevalence of cell phone only households, changes in telecommunication technology, and telemarketing. The use of sampling weights, however, aids in the correction of nonresponse bias, and research suggests that nonresponse biases in random-digit-dial (RDD) telephone surveys, such as the BRFSS, are most likely modest.43,44 In addition, prior to 2011, only adults with landline telephones were in the BRFSS sampling frame. Thus, these results may not be representative of cell-phone-only households, those without telephones, or institutionalized populations; and, might result in either overestimates or underestimates. Second, the study relied on self-reported data, which may be subject to recall and social desirability biases; however, biases are likely to be consistent over the study time period. Nevertheless, these biases may limit our ability to associate any changes in CPS use solely with health reform. Third, many of the USPSTF-recommended CPS were not assessed because they are not part of the BRFSS. Thus, the impact of health reform in Massachusetts on these unexamined CPS could not be ascertained. Finally, while five neighboring New England states were used as a comparison group to control for underlying secular trends in healthcare access and CPS use, and adjusted analysis was conducted for factors known to influence access and use of CPS, residual confounding may remain.
This study also has analytic strengths. BRFSS data have been consistently and uniformly collected by trained telephone interviewers since 1984. Also, the RDD telephone survey approach used by the BRFSS is a cost effective and efficient way to collect self-reported data at a population-level.44 The availability of these state-level data permitted an examination of healthcare access and five CPS using a DiD framework. BRFSS could provide data for similar health reform analyses in the future, as well as to examine changes in healthcare access and use of CPS over time at state-level.
CONCLUSION
Study findings suggest that within 4 years, providing health insurance coverage increased use of appropriate cervical and colorectal cancer screening in Massachusetts compared with other New England States, whereas, breast cancer and cholesterol screenings and influenza immunization did not improve more in Massachusetts than in the ONES. However, the effects of health reform on use of other clinical preventive services may be delayed or be uncertain in other states.
Electronic Supplementary Material
(DOCX 22 kb).
Acknowledgements
We thank the BRFSS coordinators in the states of Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont for their participation in data collection for this analysis and the staff of CDC’s Division of Behavioral Surveillance for their valuable assistance in developing the database for analysis. The authors would also like to express their thanks to Elena A. Hawk, Ph. D., Massachusetts BRFSS coordinator, and Tara W. Strine, Ph. D. for reviewing and commenting on the final draft of this work.
Funding Source
No funding was received for this study.
Prior Presentation
This article was presented at the 46th Annual Society for Epidemiologic Research Meeting, 18–21 June 2013, in Boston, Massachusetts.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.CCH Incorporated. Patient Protection and Affordable Care Act; Health Care and Education Reconciliation Act of 2010: text of P.L. 111–148, as signed by the President on March 23, 2010; text of P.L. 111–152, as signed by the President on March 30, 2010: JCT technical explanation of P.L. 111–148 and P.L. 111–152. 2010, Chicago, IL: CCH; 2010
- 2.Bernstein J, Chollet D, Peterson S. Issue brief: how does insurance coverage improve health outcomes? Mathematica Policy Research, Inc.: 2010:1–5.
- 3.Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies. Med Care. 2008;46:1023–1032. doi: 10.1097/MLR.0b013e318185c913. [DOI] [PubMed] [Google Scholar]
- 4.Milstein B, Homer J, Briss P, Burton D, Pechacek T. Why behavioral and environmental interventions are needed to improve health at lower cost. Health Aff (Millwood) 2011;30:823–832. doi: 10.1377/hlthaff.2010.1116. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Recommended adult immunization schedule—United States, 2010. MMWR Morbid Mortal Wkly Rep. 2010;59(1):1–4. [PubMed] [Google Scholar]
- 6.The 187th General Court of the Commonwealth of Massachusetts. Chapter 58 of the Acts of 2006. An act providing access to affordable, quality, accountable health care. April 12, 2006: The 187th General Court of the Commonwealth of Massachusetts; 2006.
- 7.U.S. Department of Health and Human Services. HealthyPeople.gov. How the health care law is making a difference for the people of Massachusetts. 2013; http://www.healthcare.gov/law/information-for-you/ma.html. Accessed March 10, 2014.
- 8.Long SK. On the road to universal coverage: impacts of reform in massachusetts at one year. Health Aff (Millwood). 2008;27(4):w270–84. [DOI] [PubMed]
- 9.Long SK, Stockley K. Sustaining health reform in a recession: an update on Massachusetts as of fall 2009. Health Aff (Millwood) 2010;29:1234–1241. doi: 10.1377/hlthaff.2010.0337. [DOI] [PubMed] [Google Scholar]
- 10.Long SK. Who gained the most under health reform in Massachusetts? Urban Institute; 2008
- 11.Long SK, Stockley K, Dahlen H. Massachusetts health reforms: uninsurance remains low, self-reported health status improves as state prepares to tackle costs. Health Aff (Millwood) 2012;31(2):444–451. doi: 10.1377/hlthaff.2011.0653. [DOI] [PubMed] [Google Scholar]
- 12.Clark CR, Soukup J, Govidarejulu U, Riden HE, Tovar DA, Johnson PA. Lack of access due to costs remains a problem for some in Massachusetts despite the state’s health reforms. Health Reform. 2011;30(2):247–255. doi: 10.1377/hlthaff.2010.0319. [DOI] [PubMed] [Google Scholar]
- 13.Maxwell J, Cortes DE, Schneider KL, Graves A, Rosman B. Massachusetts’ health care reform increased access to care for Hispanics, but disparities remain. Health Aff (Millwood) 2011;30(8):1451–1460. doi: 10.1377/hlthaff.2011.0347. [DOI] [PubMed] [Google Scholar]
- 14.Tinsley L, Andrews B, Hawk H, Cohen B. Short-term effects of health-care coverage legislation—Massachusetts, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(9):262–267. [PubMed] [Google Scholar]
- 15.Gettens J, Mitra M, Henry AD, Himmelstein J. Have working-age people with disabilities shared in the gains of Massachusetts health reform? Inquiry. 2011;48:183–196. doi: 10.5034/inquiryjrnl_48.03.03. [DOI] [PubMed] [Google Scholar]
- 16.Long SK, Stockley K. The impacts of state health reform initiatives on adults in New York and Massachusetts. Health Serv Res. 2011;46(1 Pt 2):365–387. doi: 10.1111/j.1475-6773.2010.01211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kolstad JT, Kowalski AE. The impact of health care reform on hospital and preventive care: evidence from Massachusetts. National Bureau of Economic Research; 2010
- 18.Long SK. Another look at the impacts of health reform in Massachusetts: evidence using new data and a stronger model. Am Econ Rev. 2009;99(2):508–511. doi: 10.1257/aer.99.2.508. [DOI] [PubMed] [Google Scholar]
- 19.Dhingra SS, Zack MM, Strine TW, Druss BG, Simoes E. Change in health insurance coverage in Massachusetts and other New England states by perceived health status: potential impact of health reform. Am J Public Health. 2013;103:e107–e114. doi: 10.2105/AJPH.2012.300997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pande AH, Ross-Degnan D, Zaslavsky AM, Salomon JA. Effects of healthcare reforms on coverage, access, and disparities: quasi-experimental analysis of evidence from Massachusetts. Am J Prev Med. 2011;41(1):1–8. doi: 10.1016/j.amepre.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Chen C, Scheffler G, Chandra A. Massachusetts’ health care reform and emergency department utilization. N Engl J Med. 2011;365(12):e25. doi: 10.1056/NEJMp1109273. [DOI] [PubMed] [Google Scholar]
- 22.Zhu J, Brawarsky P, Lipsitz S, Huskamp H, Haas JS. Massachusetts health reform and disparities in coverage, access and health status. J Gen Intern Med. 2010;25(12):1356–1362. doi: 10.1007/s11606-010-1482-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment. recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep. 2003;52(RR-9):1–12. [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Operational and User’s Guide. Version 3.0. 2006; http://ftp.cdc.gov/pub/Data/BRFSS/userguide.pdf. Accessed March 10, 2014.
- 25.Fahimi M, Link M, Mokdad A, Schwartz DA, Levy P. Tracking chronic disease and risk behavior prevalence as survey participation declines: statistics from the Behavioral Risk Factor Surveillance System and other national surveys. Prev Chronic Dis. 2008;5(3):A80. [PMC free article] [PubMed] [Google Scholar]
- 26.Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med. 2012;54(6):381–387. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 28.Ashenfelter O. Estimating the effect of training programs on earnings. Review of Economics and Statistics. 1978;60(1):47–57. doi: 10.2307/1924332. [DOI] [Google Scholar]
- 29.Ashenfelter O, Card D. Using the Longitudinal Structure of Earnings to estimate the effect of training programs. Review of Economics and Statistics. 1985;67(4):648–660. doi: 10.2307/1924810. [DOI] [Google Scholar]
- 30.Wooldridge JM. Econometric analysis of cross section and panel data. 2nd ed. MIT Press; 2007.
- 31.SAS Institute Inc. SAS for Windows. Version 9.2 (TS2M0). SAS Institute; 2008.
- 32.Research Triangle Institute. SUDAAN User’s Manual. Research Triangle Institute; 2008.
- 33.Centers for Disease Control and Prevention (CDC) Vital signs: colorectal cancer screening, incidence, and mortality—United States, 2002--2010. MMWR Morb Mortal Wkly Rep. 2011;60(26):884–889. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (CDC) Vital signs: breast cancer screening among women aged 50–74 years—United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(26):813–816. [PubMed] [Google Scholar]
- 35.Swan J, Breen N, Graubard BI, et al. Data and trends in cancer screening in the United States: results from the 2005 National Health Interview Survey. Cancer. 2010;116(20):4872–4881. doi: 10.1002/cncr.25215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coates RJ, Ogden L, Monroe JA, Buehler J, Yoon PW, Collins JL. Conclusions and future directions for periodic reporting on the use of selected adult clinical preventive services—United States. MMWR Morbid Mortal Wkly Rep. 2012;61(Suppl):73–79. [PubMed] [Google Scholar]
- 37.Shenson D, Adams M, Bolen J, Anderson L. Routine checkups don’t ensure that seniors get preventive services. J Fam Pract. 2011;60(1):E1–10. [PubMed]
- 38.Guide to Community Preventive Services. The community guide: what works to promote health. 2012; http://www.thecommunityguide.org/library/book/index.html. Accessed March 10, 2014.
- 39.Rodriguez SR, Osborne D, Jacobellis J. Health plan implementation of U.S. Preventive Services Task Force A and B recommendations—Colorado, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(39):1348–1350. [PubMed] [Google Scholar]
- 40.Malhotra K, Heiman HJ. Public health policy is political. Am J Public Health. 2012;102 (7):el; author reply el-2. doi:10.2105/AJPH.2012.300801 [DOI] [PMC free article] [PubMed]
- 41.Liao Y, Bang D, Cosgrove S, et al. Surveillance of health status in minority communities—Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. MMWR Surveill Summ. 2011;60(6):1–44. [PubMed] [Google Scholar]
- 42.Goldberg DS. Against the very idea of the politicization of public health policy. Am J Public Health. 2012;102(1):44–49. doi: 10.2105/AJPH.2011.300325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System. BRFSS. 2012; http://www.cdc.gov/brfss/. Accessed March 10, 2014.
- 44.Simon TR, Mercy JA, Barker L. Can we talk? Importance of random-digit-dial surveys for injury prevention research. Am J Prev Med. 2006;31(5):406–410. doi: 10.1016/j.amepre.2006.07.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 22 kb).