Abstract
Gingival squamous cell carcinoma (GSCC) is a relatively rare malignant neoplasm of the oral cavity. It represents less than 10% of diagnosed intraoral carcinoma. Because of its close proximity to the teeth and periodontium, the tumour can mimic tooth-related benign inflammatory conditions. This case report describes a patient diagnosed with GSCC presenting as localised periodontitis.
Background
Gingival squamous cell carcinoma (GSCC) is an infrequent oral tumour.1–3 It represents less than 10% of diagnosed intraoral carcinoma.4 Early detection is crucial, as survival is most significantly linked to the stage of disease.5 In general, the main risk factors for oral squamous cell carcinoma (SCC) are tobacco and alcohol consumption.6 In contrast to oral SCC, GSCC is weakly associated with these risk factors and its aetiology is not yet well established. The most common area to be affected with SCC is the lateral part of tongue followed by the floor of the mouth. Clinically, GSCC usually appears as an exophytic mass with a granular, papillary or verrucous surface or it presents as an ulcerative lesion.7 Gingival pain is the most predominant symptom but in the early stages, the disease may be asymptomatic.3 4 Because of its various appearances and similarity to common periodontal lesions, GSCC may be misdiagnosed on clinical examination.8 9
Case presentation
A 46-year-old woman presented to the department of periodontics with pain and swelling in the lower right back teeth region for the last 15 days. The patient had no history of tobacco consumption in any form. She was found to be systemically healthy. The intraoral examination revealed a swelling on the buccal and lingual aspect of teeth 44 and 45, extending from the mesial aspect of tooth 44 to the distal aspect of tooth 45. The gingival lesion appeared erythematous with speckled non-scrapable white patches and the surface was eroded and ulcerated. Clinically, the lesion confined to attached gingiva and interdental papilla of teeth 44 and 45. The margins of the lesion were well-defined with raised edges (figure 1). The lesion was firm to hard on palpation with a fixed broad base. Periodontal examination revealed bleeding on probing with no exudation and tenderness on palpation. Pocket probing depth ranging from 6 to 8 mm was present in relation to teeth 44 and 45. The teeth were not mobile. There was no tenderness on lateral and vertical percussion on teeth 44 and 45. The gingiva and alveolar mucosa at the adjacent sites were clinically normal with minimal plaque accumulation. Extraoral palpation revealed no lymph nodes involvement.
Figure 1.

Intraoral lesion.
A provisional diagnosis was carried out as localised chronic periodontitis with respect to teeth 44 and 45.
Investigations
Intraoral periapical radiographic examination revealed moderate horizontal bone loss in relation to teeth 44 and 45 and bony involvement of the lesion (figure 2).
Figure 2.
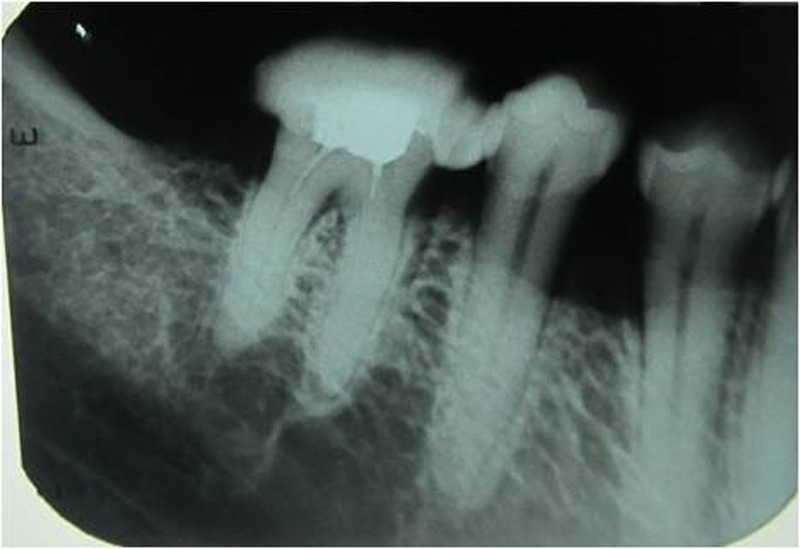
lntraoral periapical of the affected region.
Differential diagnosis
Gingivitis, chronic localised periodontitis, pyogenic granuloma, or benign conditions like verruciform xanthoma, erythroleucoplakia, deep fungal infections (blastomycosis, histoplasmosis, coccidioidomycosis, cryptococcosis) and chronic traumatic ulcer.
Treatment
Routine periodontal phase I therapy including scaling and root planning was performed in relation to teeth 44 and 45 with systemic antibiotics. The patient was advised to take amoxicillin 250 mg+clavulanic acid 125 mg three times a day, diclofenac 50 mg+paracetamol 500 mg twice daily for 5 days and clorhexidine mouthwash twice daily for 7 days.
Outcome and follow-up
On recall after 7 days, the patient reported with severe pain and discomfort on the right side of the mandible with referred pain to neck and shoulder on the same side. Clinical examination revealed an extensive erythematous and granular appearing hyperplastic tissue on the facial and lingual aspect of teeth 44 and 45. A deep linear ulcer measuring about 2 cm was noticed at the depth of the vestibule on the lingual aspect, corresponding to teeth 44 and 45 (figure 3). The lesion was tender on palpation. Tablet tramadol 50 mg three times a day for 3 days was prescribed and incisional biopsy was planned.
Figure 3.

Lesion after phase I therapy.
Multiple incisional biopsies were performed on the right mandibular buccal (0.5×0.5×0.5 cm) and lingual (1.0×0.5×0.5 cm) gingiva in relation to teeth 44 and 45 the next day.
One week after incisional biopsy, the intraoral picture revealed incomplete healing of the gingival tissue (figure 4).
Figure 4.

Lesion 1-week postoperatively after incisional biopsy.
Histological examination of the incised tissue with H&E stain revealed hyperplastic surface epithelium with a prominent endophytic growth pattern. The squamous proliferation showed focal epithelial detachment, individual cell keratinisation and keratin pearls (figure 5). Based on the histological findings, the final diagnosis was carried out as GSCC.
Figure 5.
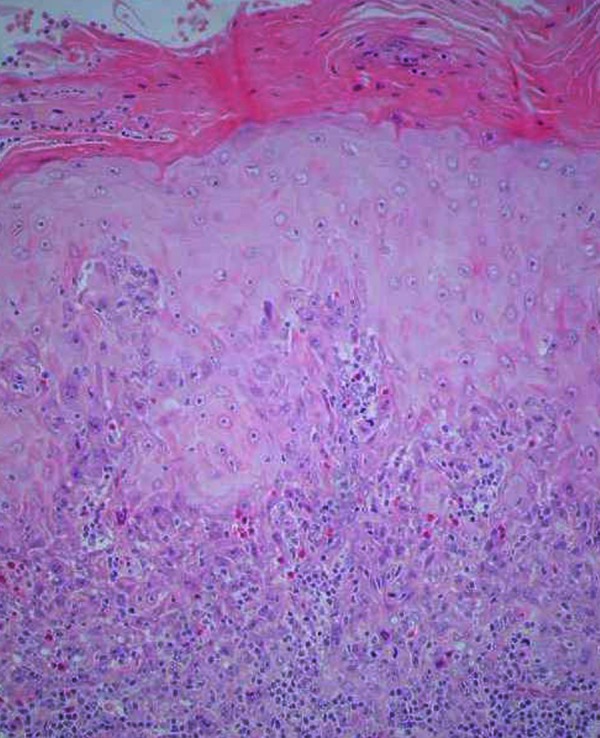
Histopathological view of the lesion showing the loss of the epithelial-connective tissue (H&E stain).
The patient was referred to the department of oncology for further needful management. Based on the histopathological examination and lymph node biopsy, she was diagnosed with moderately differentiated gingival SCC (T1N1M0). The patient underwent right-sided marginal mandibulectomy of the teeth 44 and 45 region with level 5 radical neck dissection.
Discussion
SCC is an epithelial tumour and the most common malignant tumour of the oral cavity.10 Gingival SCC accounts for <10% of all intraoral SCC and the majority of gingival SCCs occur in the mandible.5
Over the past 40 years, despite advances made in diagnosis, the overall 5-year survival rate for oral SCC has remained relatively constant at around 50%.11 Several reasons may account for this: high-risk patients do not seek medical attention, oral cancer examinations are not frequently performed and existing lesions are often overlooked by the general dentist, and delays to the onset of signs/symptoms to clinical diagnosis are also common.12
GSCC is often asymptomatic and the initial symptoms are usually an intraoral mass or swelling, ulceration, pain, ill fitting dentures, mobility of teeth or unhealed extraction wounds. These tumours frequently resemble inflammatory lesions affecting the periodontium such as pyogenic granuloma, gingivitis, periodontitis or benign conditions such as verruciform xanthoma. At the early stage, the lesion often closely simulates advanced periodontitis associated with minimal pain and may lead to a diagnostic delay.8 13 Other differential diagnosis could be erythroleucoplakia, deep fungal infections and chronic traumatic ulcer.
Chronic traumatic/reactive ulcers are usually covered by a yellow membrane and are surrounded by elevated margins that may show hyperkeratosis or induration due to scar formation. They are most frequently seen on the tongue and show chronic cell infiltration on histopathological evaluation.14
Deep fungal infections (blastomycosis, histoplasmosis, coccidioidomycosis, cryptococcosis) may also present as a chronic erythematous ulcerated area with indurated margins, but they are characterised by primary involvement of the lungs and microscopic examination reveals granulomatous inflammation with organism, which was ruled out in this case.15
Erythroplakia mostly present as well demarcated red lesions of flat, macular and velvety appearance. Most of the clinically diagnosed erythroplakia re-present as severe dysplasia or carcinoma in histopathological examination. If left untreated, 90% of the cases transform into cancer. Among them 51% into grade-I oral squamous cell carcinoma, 40% into carcinoma in situ or severe epithelial dysplasia and 9% mild to moderate epithelial dysplasia.16
In the present case, the patient had a well-defined erythromatous, eroded and ulcerated lesion against the normal appearing healthy mucosa, which mimics clinically as an erythroleucoplakic lesion. But the histological examination showed focal epithelial detachment, individual cell keratinisation and keratin pearls, which confirms the lesion as gingival squamous cell carcinoma. Thus, it was excluded after histological examination.
Most gingival tumours are well-differentiated and arise from keratinised mucosa of the mandibular posterior gingiva in which the tumour may destroy the underlying bone structure, causing tooth mobility.4 In accordance with the epidemiological data, the tumour in the present case report affected a middle-aged woman without any tobacco smoking or alcohol drinking habit. However, the tumour was located in the posterior gingiva of the mandibular teeth and no mobility of teeth 44 and 45 was observed. Gingival pain is the most predominant symptom, but in the early stage the tumour may be asymptomatic.3 5 Moreover, the clinical similarity between gingival tumours and periodontal disease may increase the difficulty in diagnosing these tumours early.
Squamous cell carcinoma of the gingiva is an aggressive disease, with survival best correlated with surgical stage.2 In one study of 595 patients with oral cancer, 8% were gingival carcinomas and of these patients 52% saw a dentist as their initial professional contact.17
In a 20-year survey of cases, Cady and Caplin noted that over 60% of patients were initially seen by dentists. Among them half were immediately referred for appropriate therapy either before or after biopsy.
In the present case, the patient had no history of tobacco consumption in any form. Gingival SCC is rarely associated with tobacco consumption, despite the main risk factors for oral SCC being smoking or consumption of any chewable form of tobacco and drinking of alcohol.1
Learning points.
Gingival squamous cell carcinoma (SCC) is quite different from other SCCs, mimicking localised periodontal disease.
It can be misdiagnosed as localised chronic periodontitis, speckled erythroplakia, deep fungal infection, chronic traumatic ulcer, SCC or metastatic carcinoma (from the lungs and vestibule).
Appropriate oral cancer screening and appropriate referral is important.
Gingival verrucous, white patches and persistent ulcers and swellings should be biopsied promptly.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Barasch A, Gofa A, Krutchkoff DJ, et al. Squamous cell carcinoma of the gingival: a case series analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:183–7 [DOI] [PubMed] [Google Scholar]
- 2.Gomez D, Faucher A, Picot V, et al. Outcome of squamous cell carcinoma of the gingiva: a follow-up study of 83 cases. J Craniomaxillofac Surg 2000;28:331–5 [DOI] [PubMed] [Google Scholar]
- 3.Cady B, Catlin D. Epidermoid carcinoma of the gum. A 20-year survey. Cancer 1969;23:551–69 [DOI] [PubMed] [Google Scholar]
- 4.Levi PA, Jr, Kim DM, Harsfield SL, et al. Squamous cell carcinoma presenting as an endodonticperiodontic lesion. J Periodontol 2005;76:1798–804 [DOI] [PubMed] [Google Scholar]
- 5.Soo KC, Spiro RH, King W, et al. Squamous carcinoma of the gums. Am J Surg 1988;156:281–5 [DOI] [PubMed] [Google Scholar]
- 6.Khan SM, Gossweiler MK, Zunt SL, et al. Papillary squamous cell carcinoma presenting on the gingiva. J Periodontol 2005;76:2316–21 [DOI] [PubMed] [Google Scholar]
- 7.Lee JJ, Cheng SJ, Lin SK, et al. Gingival squamous cell carcinoma mimicking a dentoalveolar abscess: report of a case. J Endod 2007;33:177–80 [DOI] [PubMed] [Google Scholar]
- 8.Seoane J, Varela-Centelles PI, Walsh TF, et al. Gingival squamous cell carcinoma: diagnostic delay or rapid invasion? J Periodontol 2006;77:1229–33 [DOI] [PubMed] [Google Scholar]
- 9.Alsharif MJ, Jiang WA, He S, et al. Gingival squamous cell carcinoma in young patients: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:696–700 [DOI] [PubMed] [Google Scholar]
- 10.Casiglia J, Woo SB. A comprehensive review of oral cancer. Gen Dent 2001;49:72–82 [PubMed] [Google Scholar]
- 11.Greenlee RT, Murray T, Bolden S, et al. Cancer statistics. CA Cancer J Clin 2000;50:7–33 [DOI] [PubMed] [Google Scholar]
- 12.Pitiphat W, Diehl SR, Laskaris G, et al. Factors associated with delays in the diagnosis of oral cancer. J Dent Res 2002;81:192–7 [PubMed] [Google Scholar]
- 13.Tolman A, Jerrold L, Alarbi M. Squamous cell carcinoma of attached gingiva. Am J Orthod Dentofacial Orthop 2007;132:378–81 [DOI] [PubMed] [Google Scholar]
- 14.Sook Bin Woo, Martin S. Greenberg. Ulcerative, vesicular and Bullous lesions. In: Burket's oral medicine, diagnosis & treatment. Greenberg, ed. Burkit's Oral Medicine, eleventh edn. Hamilton: B C Decker Inc; 2008:72–3
- 15.Regezi JA, Sciubba JJ, Jordan RC. Oral pathology, clinical pathologic correlations. 5th edn Saunders: Elesvier, 2009 [Google Scholar]
- 16.Reibel J. Prognosis of oral pre-malignant lesions: significance of clinical, histopathological, and molecular biological characteristics. Crit Rev Oral Biol Med 2003;14:47–62 [DOI] [PubMed] [Google Scholar]
- 17.Silverman S. Oral cancer. 3rd edn Atlanta: American Cancer Society, 1990:1–6 [Google Scholar]


