Abstract
Asymptomatic spontaneous coronary artery spasm is rare and there are no case reports in literature presenting with acute ST elevation on routine ECG. We present the case of a 68-year-old Caucasian man who presented to a primary care physician for a routine ECG as part of hypertension follow-up. ECG revealed ST elevation in inferior leads II, III and aVF with reciprocal ST depression in leads I, aVL and also ST depression in anterior leads V1, V2 and V3 suggesting ongoing inferoposterior ST elevation myocardial infarction. The patient was completely well, stable and asymptomatic and he was rushed immediately to the coronary care unit via emergency ambulance. The patient was subjected to a battery of urgent investigations which were all normal. Also an urgent coronary angiogram was undertaken which showed completely normal coronary anatomy.
Background
In spite of great emphasis on controlling cardiac risk factors, coronary artery disease is on a rise. Patients can have major coronary abnormalities even without having any cardiac risk factors. Vasospasm has been proved in a large number of patients presenting with chest pain and ECG changes both in patients without coronary artery disease and with significant coronary artery disease. Our patient was completely asymptomatic and significant pathological ST elevation was recorded on routine ECG twice with unobstructed coronaries. This is a very rare presentation and we believe this case report is first of its kind.
Case presentation
We describe a fit and well 68-year-old part time worker in a factory with a history of mild hypertension for 2 years and mildly high cholesterol for 1 year presented to his primary care physician for a routine ECG. He was routinely taking aspirin 75 mg once daily and simvastatin 40 mg. The patient denied any history of chest pain, shortness of breath, palpitations or any other symptoms of being unwell. There was no family history of coronary artery disease or sudden cardiac deaths. His routine ECG confirmed ST elevation in inferior leads along with reciprocal ST depression in leads L1 and aVL and ST depression in anterior leads (figure 1). He was transferred to the coronary care unit in an emergency ambulance. On arrival at the hospital the ECG normalised without ST elevation and only T wave inversions was recorded in anterior chest leads (figure 2). The patient was completely well and haemodynamically stable all through his hospital stay. The patient was subjected to a battery of investigations which were all normal. He was spotted around 14:00 next day to have recorded massive pathological ST elevation which lasted only 2–3 min during cardiac monitoring in the coronary care unit (figure 3) and yet again the patient had no chest pain or any other symptoms and was haemodynamically stable. A 12-lead ECG performed was in sinus rhythm with normal rate, with no ST elevation and T wave inversions recorded in anterior leads.
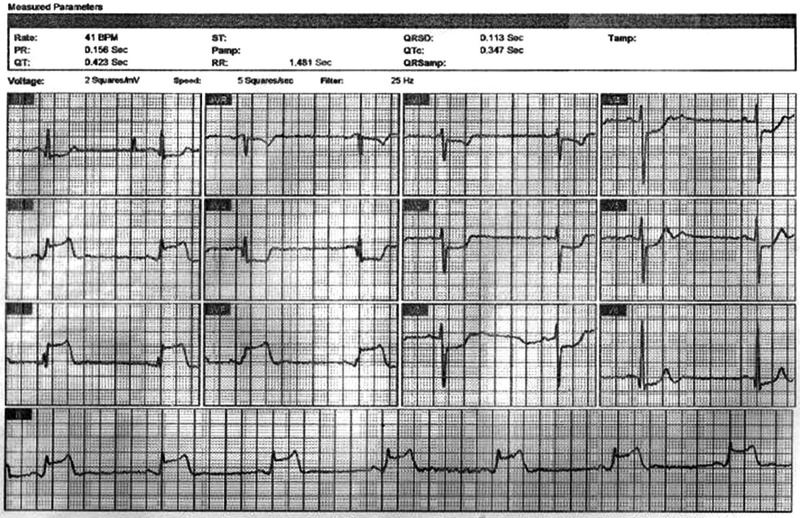
Figure 1.
First ECG at general practitioner (GP) surgery showing inferior ST elevation and posterolateral ST depression along with reciprocal ST depression changes in leads L1 and aVL which prompted admission to the coronary care unit.
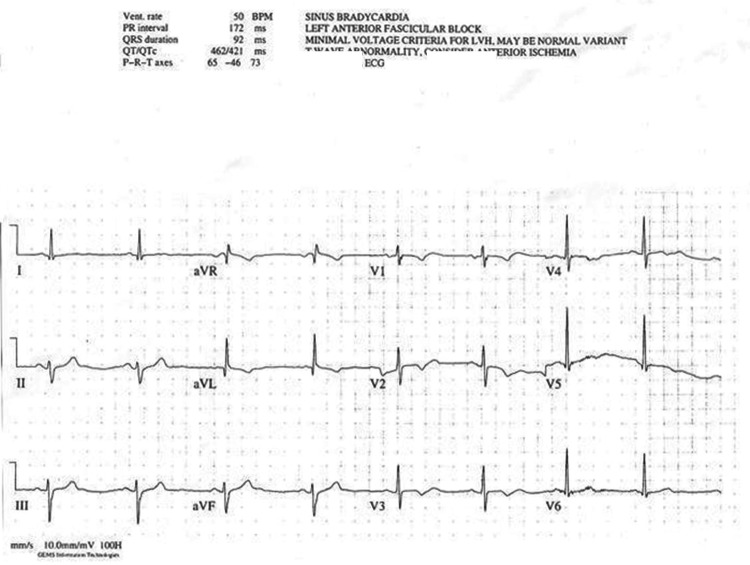
Figure 2.
ECG on arrival with no ST elevation but sinus rhythm with T wave changes anteriorly.
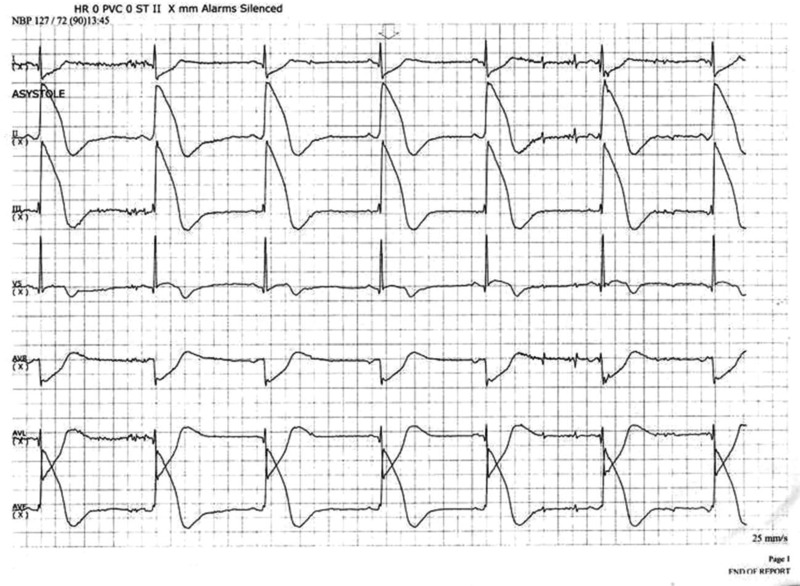
Figure 3.
Telemetry recordings showing significant pathological ST elevation without any symptoms.
Clinical examination was unremarkable and all baseline blood investigations including full blood count, electrolytes, renal parameters, liver function tests and cardiac enzymes including 12 h troponin T were normal. Chest X-ray was normal.
Transthoracic echocardiogram showed a normal-sized left ventricle with no regional wall motion abnormalities and normal systolic and diastolic function. Valves and other chambers of the heart were normal too.
Coronary angiogram was performed immediately showing normal left and right coronary arteries (figures 4 and 5). Other coronary artery branches were normal. The left ventricuolgram was normal. Transoesophageal echocardiography was performed with a view to visualise specifically the left ventricle and other chambers and valves to rule out cardiomyopathy. This study was completely normal with normal size and function of left ventricle and other chambers and valves. The patient was reassured and discharged with advice for primary prevention of coronary artery disease.
Figure 4.
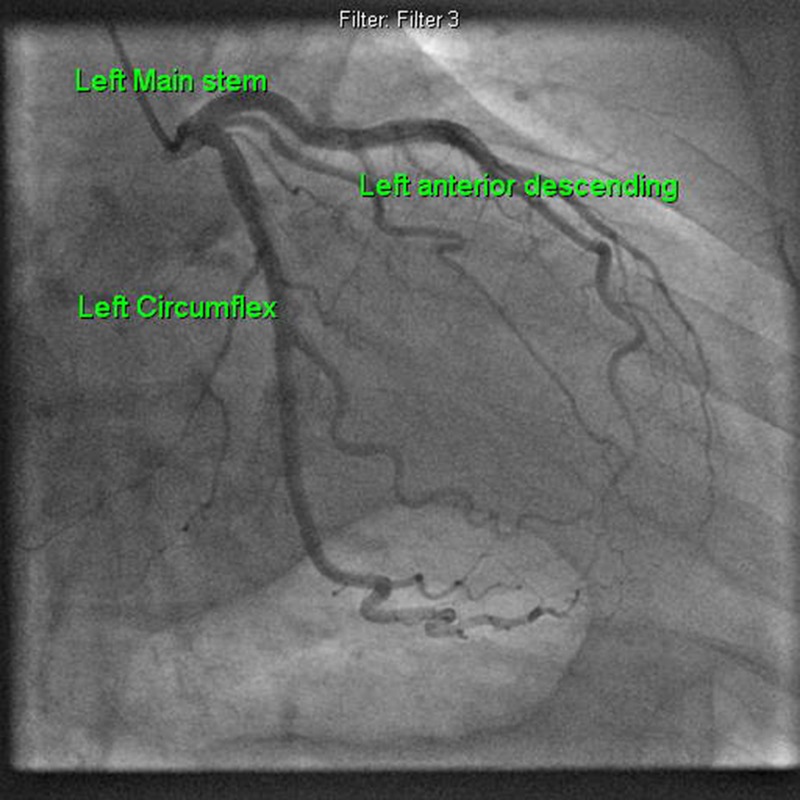
Normal left coronary angiogram.
Figure 5.
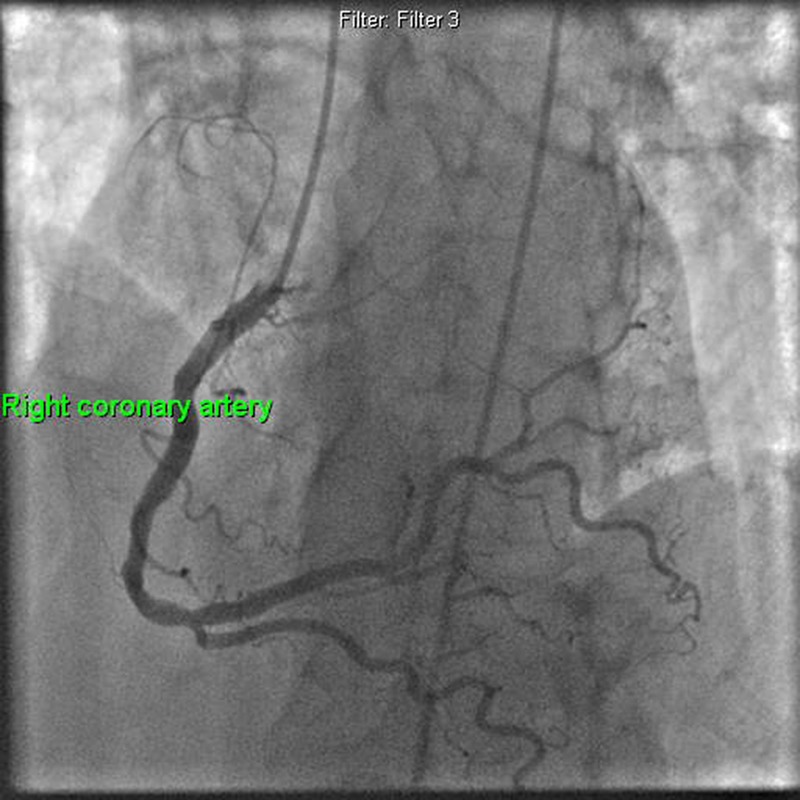
Normal right coronary angiogram.
Cases have been reported from different parts of the world and also from the UK but all of these patients had chest pain and ST elevation with normal coronary angiograms. Some case reports with normal angiograms were described with chest pain during tilt table testing, exercise testing or chest pain on background of cocaine, amphetamines and marijuana abuse.
Investigations
A full series of investigations are needed when there is undiagnosed acute ST elevation on ECG. The patient had serial 12 lead ECGs and continuous cardiac monitoring. Baseline haematology and biochemistry investigations were ordered like full blood count, blood sugar, electrolytes including calcium and magnesium, liver function tests, coagulation profile and also cardiac enzymes including cardiac troponins. He underwent coronary angiography next day and also transthoracic echocardiography. After about 3 months the patient underwent transoesophageal echocardiogram which was normal and did not show any left ventricular abnormalities.
Differential diagnosis
Acute ST elevation on ECG with chest pain is acute myocardial infarction until proven otherwise. Other causes for ST elevation can be due to pericarditis, myocarditis, coronary vasospasm, illicit drug abuse like cocaine and amphetamines, left ventricular aneurysm, Tatkasubo cardiomyopathy, etc. It can be sometimes early repolarisation changes on ECG. A normal variant ST elevation pattern has been identified in Afrocaribbean men.
Treatment
Coronary vasospasm has always been treated with calcium channel blockers, nitrates, nicorandil, etc both as intracoronary and as oral or intravenous medications with excellent response rates. This patient was also started on calcium channel blockers for suspected possible coronary vasospasm and has been advised regarding aggressive primary prevention measures for coronary artery disease.
Outcome and follow-up
Routine follow-up for patients with documented coronary artery spasm without coronary artery disease is mostly necessary when patients are troubled a lot with symptoms. This patient is booked for another routine follow-up with repeat echocardiogram in 1 year time.
Discussion
Asymptomatic coronary spasm is very rare.1 Management of vasospastic angina or asymptomatic coronary spasm is by medical treatment with nitrates, calcium channel blockers, etc. In some studies coronary vasospasm was treated with intracoronary stents and high rates of restenosis were demonstrated suggesting only medical treatment is of benefit in vasospastic coronaries.2
There are numerous case reports in the literature describing patients presenting with chest pain and acute ST elevation on 12 lead ECG and subsequently found to have normal coronary angiogram.3 4 But there are no case reports of spontaneous ST elevation without chest pain due to coronary spasm. Coronary spasm has always been described with chest pain with or without ECG changes ranging from T wave changes, ST depression and also ST elevation.5 Other causes of chest pain and ST elevation with normal coronary angiography have been described in patients with pericarditis, myocarditis, usage of illicit drugs like cocaine and amphetamines,4 Tatkasubo cardiomyopathy and other forms of cardiomyopathy. In some young Afrocaribbean men ST elevation or ‘high take off’ has been described as a normal variant. Some cases of acute chest pain and ST elevation on ECG have been described with coronary angiogram showing acute obstruction of coronary artery with a thrombus and no coronary lesion found after aspiration of thrombus.6 Coronary spasm is also postulated to increase the number of small-sized platelet aggregates resulting in a higher chance of thrombus formation.6
In some studies high frequency of T wave alternans on 24 h ECG monitoring was shown as correlating to repolarisation abnormalities and observed in patients with vasospastic angina.7 In these patients with vasospastic angina who were treated with medications, the episodes of T wave alternans were reduced. So it is possible that during asymptomatic periods there is a risk for tachyarrhythmias in these patients7 8 but ST elevation during asymptomatic periods has not been described before.
While we acknowledge coronary spasm is very well known and can be present in patients without chest pain as described in numerous publications dating back as far as 30 years,3 a study by Nosaka and Nobuyoshi9 looked at coronary spasm in asymptomatic patients by doing coronary angiogram in patients referred for angiogram for reasons other than chest pain and found incidence of coronary spasm to be 2.7%; however, there was no ST elevation in any of these patients.
We also acknowledge that the significance surrounding the clinical relevance of searching for these patients with asymptomatic coronary spasm in general population at large is unknown.8 However patients presenting with symptoms with or without ECG changes meet the criteria for further investigation and to diagnose and treat coronary spasm if present.
All patients with ST elevation should be urgently assessed by cardiologists and management and investigational protocol formalised. In asymptomatic patients with ST elevation on ECG an effort should always be made to compare with old ECGs. In patients with prior myocardial infarction persistent ST elevation is sometimes found and correlates with infracted segment of the myocardium and aneurismal change in the myocardium. Some studies have demonstrated the ability of multislice CT to detect coronary-artery spasm.1 The utility of nitrate administration, as routinely performed during conventional invasive angiography, is undisputed and can promptly treat acute coronary vasospasm with or without chest pain.5
Drugs like ergonovine and acetylcholine are popular to test for coronary spasm. Lot of studies have demonstrated usefulness and safety of these drugs to test for coronary vasospasm in symptomatic patients, but routine vasospasm testing in UK practice is not common. Ergonovine has been shown to have diffuse vasoconstrictive properties on vascular smooth muscle in general.
The coronary artery spasm due to ergonovine differs from the normal response. The degree of vascular narrowing is greater, the spasm is segmental and it mostly occurs after very small doses of ergonovine.
Ergonovine causes coronary spasm and can be correlated with spontaneous coronary artery spasm in patients with variant angina. Ergonovine produces two types of coronary artery spasm: focal and diffuse.
On transthoracic echocardiography detection of regional wall motion abnormality during ergonovine challenge has been projected as a screening procedure to detect coronary spasm.
The concern of fear of irreversible spasm leading to arrhythmia and death due to the provocative testing for coronary spasm remains.
The complication rates of provocative ischaemia testing itself are around rates of 1.3–1.5% in various large studies.
Some studies have demonstrated vasospastic angina to be associated with slightly increased incidence of sudden cardiac death and potentially fatal arrhythmias but statistical significance was meagre.10 11
In another study by Araki et al12 ST elevation was described in 26 patients with vasospastic angina on follow-up with 24 h ambulatory ECG monitoring. In these 26 patients 364 episodes of significant ST elevation were recorded and 79% of these ST elevations were asymptomatic. However, only five patients had normal or near normal coronary angiogram in this study.
Learning points.
Acute ST elevation in patients with chest pain is always acute ST elevation myocardial infarction until proved otherwise.
ST elevation on ECG can be associated with coronary vasospasm. Mostly patients have chest pain and rarely as in above case can present without chest pain.
All ST elevations on ECG need cardiologist's review and full further investigations.
ST elevation on ECG can be due to many other conditions as well apart from acute myocardial infarction.
Acknowledgments
Labiba Bahjat.
Footnotes
Contributors: IM was involved in case design and write up and revisions. MSEZ was involved in image format and corrections. NT was involved in case collection and obtaining consent. MIK supervised, supported and was involved in corrections.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review : Not commissioned; externally peer reviewed.
References
- 1.Hamon M, Hamon M. Asymptomatic coronary-artery spasm. N Engl J Med 2006;355:2236. [DOI] [PubMed] [Google Scholar]
- 2.Huang ZY, Qian JY, Yang HBet al. Clinical and angiographic outcomes of coronary drug-eluting stenting in treating vasospastic angina patients with severe organic stenosis. Zhonghua Xin Xue Guan Bing Za Zhi 2012;40:560–4 [PubMed] [Google Scholar]
- 3.Maseri A, Severi S, Nes MD, et al. “Variant” angina: one aspect of a continuous spectrum of vasospastic myocardial ischemia. Pathogenetic mechanisms, estimated incidence and clinical and coronary arteriographic findings in 138 patients. Am J Cardiol 1978;42:1019–35 [DOI] [PubMed] [Google Scholar]
- 4.Arora S, Goyal H, Aggarwal P, et al. ST-segment elevation myocardial infarction in a 37-year-old man with normal coronaries—it is not always cocaine. Am J Emerg Med 2012;30:2091.e3–5 [DOI] [PubMed] [Google Scholar]
- 5.De Servi S, Specchia G, Angoli L, et al. Coronary arterial spasm in angina at rest associated with transient ST-segment changes. Clin Cardiol 1980;3:54–60 [DOI] [PubMed] [Google Scholar]
- 6.Miyamoto S, Ogawa H, Soejima H, et al. Formation of platelet aggregates after attacks of coronary spastic angina pectoris. Am J Cardiol 2000;85:494–7, A10 [DOI] [PubMed] [Google Scholar]
- 7.Shimada H, Nishizaki M, Fujii H, et al. Ambulatory electrocardiogram-based T-wave alternans in patients with vasospastic angina during asymptomatic periods. Am J Cardiol 2012;110:1446–51 [DOI] [PubMed] [Google Scholar]
- 8.Myerburg RJ, Kessler KM, Mallon SM, et al. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N Engl J Med 1992;326:1451–5 [DOI] [PubMed] [Google Scholar]
- 9.Nosaka H, Nobuyoshi M. Coronary arterial spasm and symptomatology in ischaemic and non-ischaemic heart diseases: study of the ergonovine maleate provocative test in 3,000 consecutive patients. J Cardiogr Suppl 1987;12:35–47 [PubMed] [Google Scholar]
- 10.Koyanagi S, Takeshita A, Nakamura M. Clinical characteristics of sudden cardiac death in patients with vasospastic angina. Jpn Circ J 1989; 53:1541–5 [DOI] [PubMed] [Google Scholar]
- 11.Kodama S, Inoue Y, Mihara H, et al. Prognostic factors for the long-term survival in patients with vasospastic angina. Analysis of effects of patients’ characteristics and therapeutic drugs. J Cardiol 2009;54:10–20 [DOI] [PubMed] [Google Scholar]
- 12.Araki H, Koiwaya Y, Nakagaki O, et al. Diurnal distribution of ST-segment elevation and related arrhythmias in patients with variant angina: a study by ambulatory ECG monitoring. Circulation 1983;67:995–1000 [DOI] [PubMed] [Google Scholar]