Abstract
The purpose of this case report is to describe the clinical presentation of a patient who suffered from a fracture of the lateral tubercle of the posterior talar process caused by a fall while rock-climbing. The initial evaluation revealed diffuse ankle swelling, tenderness, and pain at the distal aspect of both malleoli. Plain film radiography revealed a fracture of the posterior process of the talus. Computed tomography (CT) outlined the extension of the fracture line in the postero-lateral aspect of the body of the talus with minimal displacement. The patient was treated conservatively with an Aircast© walking boot for 6 weeks (non–weight-bearing) followed by a 2-week period of partial weight bearing. At the 8 week follow-up, he reported minimal tenderness and normal ankle function. Clinicians should be aware that talar fracture identification on plain films is difficult and computed tomography or magnetic resonance imaging may be required.
Keywords: talus, athletic injuries, diagnostic imaging, radiology, rock-climbing
Abstract
L’objectif de ce rapport de cas est de décrire la présentation clinique d’un patient qui a subi une fracture du tubercule latéral du processus talaire postérieur suite à une chute d’escalade. L’évaluation initiale a révélé un œdème diffus de la cheville et de la douleur sur l’aspect distal des deux malléoles. Les radiographies ont révélé une fracture de l’apophyse postérieure du talus. La tomodensitométrie a démontré que la ligne de fracture atteignait l’aspect postéro- latérale du corps du talus avec déplacement minimal. Le patient a été traité avec une botte Aircast© pour 6 semaines (sans mise en charge) suivie d’une période de 2 semaines de mise en charge partielle. Après 8 semaines, il rapporte un inconfort minimal ainsi qu’une fonction normale de sa cheville. Les cliniciens doivent être conscient que ce type de fracture requiert une évaluation minutieuse des radiographies. La tomodensitométrie ou l’imagerie par résonance magnétique sont parfois nécessaires.
Keywords: talus, blessures sportives, imagerie diagnostique, radiologie, escalade
Introduction
Fractures and dislocations of the talus are considered rare, accounting for 0.1% to 0.85% of all fractures.1,2 Nevertheless, the talus is the second most frequent tarsal bone fracture after the calcaneus.2,3 Talar fractures have been described by Fortin and are classified according to their anatomical location: head, body, or neck.2
Fractures of the talar body can be further subdivided into three groups: 1) cleavage fractures (horizontal, sagittal, shear, or coronal); 2) talar process or tubercle fractures; and 3) compression fractures.2 Fractures of the tubercles of the posterior talar process are considered rare. Since, they have mainly been reported as case study or case series it is impossible to appreciate their incidence.4–10 Despite the relative rarity of this injury, it is often mis-diagnosed (or underdiagnosed) as an ankle sprain.10,11 The purpose of this paper is to present a retrospective case study of a lateral tubercle of the posterior talar process fracture sustained by a young adult rock climber.
Case presentation
A 29-year-old male patient sustained a right ankle injury during a fall. His foot somehow collided with the rock wall while trying to stop the fall. The patient had to walk approximately 500 meters in order to seek help. The initial evaluation revealed diffuse ankle swelling, tenderness, and pain at the distal aspect of both malleoli. The patient presentation satisfied the criteria of the Ottawa ankle rules12, and AP, medial oblique and lateral radio-graphs of the ankle were obtained. A mildly posteriorly displaced fracture of the posterior process of the talus was seen (figure 1). Due to the unusual presentation of the fracture, computed tomography (CT) was then ordered. The CT outlined the extension of the fracture line through the postero-lateral aspect of the body of the talus with minimal displacement (figure 2).
Figure 1:
Lateral ankle radiographs showing a fracture of the lateral tubercle of the posterior talar process.
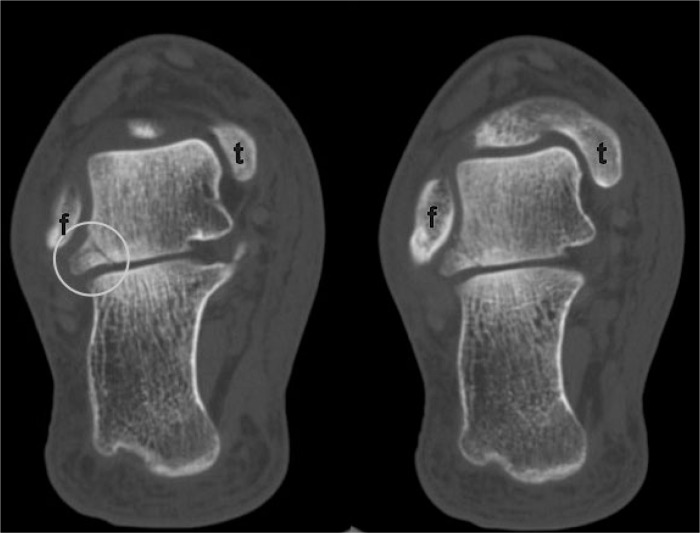
Figure 2:
Computed tomography images through the talocalcaneal joint. The images were obtained on the day of the injury. A comminuted fracture line is seen through the lateral tubercle of the posterior talar process and extending into the body of the bone. The fibula is depicted by the letter « f » and the medial malleolus of the tibia is shown by the letter « t ».
The patient was referred to a hospital-based orthopaedic clinic. He was treated conservatively with an Aircast© walking boot for 6 weeks (non–weight-bearing) followed by a 2-week period of partial weight bearing. At 6 weeks following the injury, a repeated radiographic examination demonstrated a non-union of the tubercle fragment with minimal displacement (figure 3). The patient gradually resumed all his occupational and sports activities and reported minimal tenderness and normal ankle function. Further follow-up was not needed.
Figure 3:
Lateral radiograph of the ankle obtained 6 weeks after the injury. Union of the fragment with the talus is very unlikely at this stage. Since the patient’s condition was improving steadily, surgical removal of the fragment was not considered.
Discussion
The posterior process of the talar body is formed by the lateral and medial tubercles.13 The tubercles are separated by a groove in which courses the flexor hallucis longus tendon. The lateral tubercle is larger and serves as the attachment site for the posterior talofibular and the posterior talocalcaneal ligaments.10,13 The medial tubercle serves as the attachment of the deltoid ligament.10,13 The os trigonum is an accessory ossicle commonly located posteriorly to the lateral tubercle and should not be mistaken for a fracture of the posterior process of the talus.14
Fractures of the posterior talar process have been only described as case reports or case series, making it difficult to generalize the usual presentation, cause and associated symptoms. It has been suggested that fracture of the lateral tubercle may be caused by excessive plantar flexion (compression fracture) or inversion (avulsion fracture), while fractures of the medial tubercle would be the result of dorsiflexion with pronation (avulsion fracture).10,11 Like other talar fractures, they occur when a person falls from a certain height or during sports who require kicking such as football.2,11
The clinical presentation of a patient with fracture of the lateral tubercle usually includes pain and swelling in the posterolateral area of the ankle.10,11 Deep palpation of that area should reveal tenderness and reproduce pain as well as plantar flexion or dorsiflexion of the great toe.11 Patients with fractures of the medial tubercle may only suffer from mild pain, especially while walking.15 Typically, pain and swelling will be localized posterior to the medial malleolus.11,15 Fractures of both tubercles are commonly misdiagnosed as ankle sprains.10,11 Paulos has reported that 85% of his cases were not initially adequately diagnosed.10
Fractures of the lateral tubercle are usually best visualized on lateral radiograph of the foot. It is important not to dismiss a fracture fragment located at the posterosuperior aspect of the talus as a normal variant: an accessory ossicle called the os trigonum.14 Accessory ossicles tend to be rounded with a well corticated margin, while fracture fragments may be irregular and demonstrate jagged edges. Fractures of the medial tubercle are generally not well seen on the standard 3 view ankle series. To visualize this injury, an external oblique view with approximately 40 degrees of external rotation may be required.8,11,16
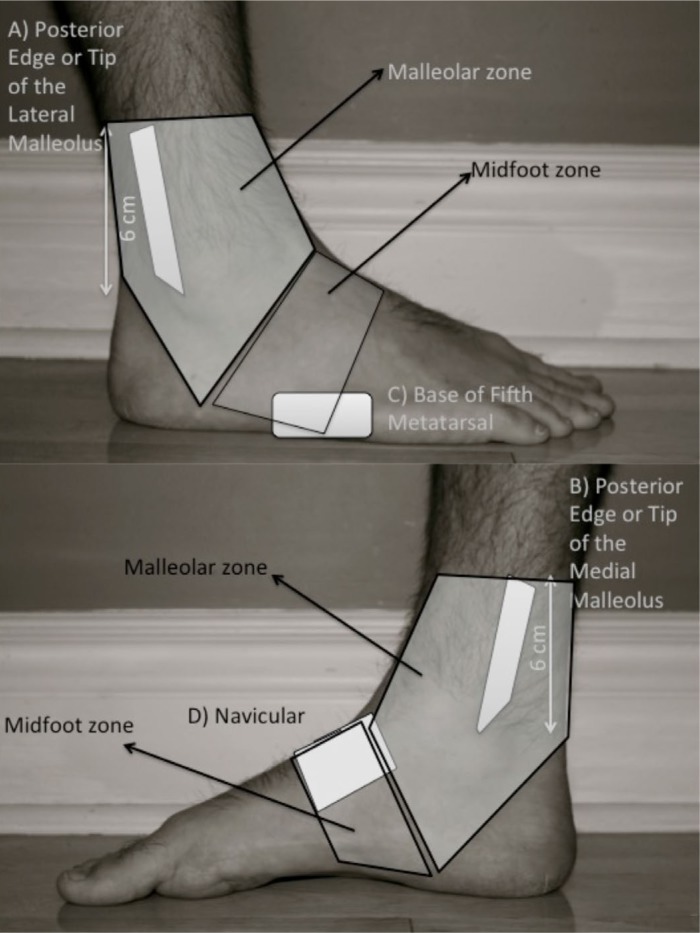
The Ottawa ankle rules (figure 4) are now generally used to determine the indication of ankle radiograph because it has demonstrated a very high sensitivity, moderate specificity, therefore, a very low rate of false negatives.12 The implementation of the Ottawa ankle rules contributed to reducing the number of unnecessary investigations. Unfortunately, fractures of the talus were rarely encountered in the Ottawa ankle trials and some authors have suggested that talus fracture might fall in a “blind spot”.17 Judd suggested that: “the Ottawa ankle rules is likely to allow detection of talus and calcaneus fracture because patients will not often be able to bear weight”.11 In this case study, the patient could bear weight, but had pain in both the lateral and medial malleolus areas. Radiographic analysis might be considered, according to clinical judgement and experience, when the mechanism of injury suggests a fracture or when a suspected ankle sprain does not improve over time. When suspicion is present, CT or MRI will better demonstrate this type of fracture.16
Figure 4:
Ottawa Ankle Rules: An ankle radiographic series is only required if there is pain in the malleolar zone and any of these findings: – Bone tenderness at A – Bone tenderness at B – Inability to bear weight.
A foot radiographic series is only required if there is pain in the midfoot zone and any of these findings: – Bone tenderness at C – Bone tenderness at D – Inability to bear weight.
(Adapted with permission from http://www.ohri.ca/emerg/cdr/docs/cdr_ankle_poster.pdf)
Fractures of both tubercles will usually be treated conservatively if there is minimal displacement.2,10,11 Non weight-bearing and short leg casts are recommended for 4 to 6 weeks followed by 2 weeks of weight bearing to tolerance. If the symptoms persist; an additional period of immobilization (4 to 6 weeks) might be required. Surgical excision of the fragment might be considered if the pain persists more than 6 months.2,11 Displaced fracture or larger fracture might require reduction and surgical fixation.2,7,8
Conclusion
This report demonstrates a case of fracture of the lateral tubercle of the posterior talar process caused by a rock-climbing fall. Clinicians should be aware that a fracture of posterior talar process may mimic the signs and symptoms of ankle sprains.
Acknowledgments
The patient would like to thank his climbing partner.
Footnotes
Sources of Financial Support: Dr. Marc-André Blanchette is funded by a PhD Fellowship from the CIHR. Dr. Julie-Marthe Grenier receives no funding.
References
- 1.Santavirta S, Seitsalo S, Kiviluoto O, Myllynen P. Fractures of the talus. J Trauma. 1984 Nov;24(11):986–989. doi: 10.1097/00005373-198411000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Fortin PT, Balazsy JE. Talus fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001 Mar-Apr;9(2):114–127. doi: 10.5435/00124635-200103000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Yochum TR, Rowe LJ. Essentials of skeletal radiology. Williams & Wilkins; Baltimore: 1996. p. 735. [Google Scholar]
- 4.Ahmad R, Ahmed SM. Fracture of the posterior process of the talus: an unusual injury. BMJ Case Rep. 2009;2009:bcr2006045609. doi: 10.1136/bcr.2006.045609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhanot A, Kaushal R, Bhan R, Gupta PN, Gupta RK, Bahadur R. Fracture of the posterior process of talus. Injury. 2004 Dec;35(12):1341–1344. doi: 10.1016/j.injury.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 6.Iyakutty PP, Singaravadivelu V. Fracture of the entire posterior process of the talus: a case report. J Foot Ankle Surg. 2000 May-Jun;39(3):198–201. doi: 10.1016/s1067-2516(00)80023-x. [DOI] [PubMed] [Google Scholar]
- 7.Mehrpour SR, Aghamirsalim MR, Sheshvan MK, Sorbi R. Entire posterior process talus fracture: a report of two cases. J Foot Ankle Surg. 2012 May-Jun;51(3):326–329. doi: 10.1053/j.jfas.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Nadim Y, Tosic A, Ebraheim N. Open reduction and internal fixation of fracture of the posterior process of the talus: a case report and review of the literature. Foot Ankle Int. 1999 Jan;20(1):50–52. doi: 10.1177/107110079902000111. [DOI] [PubMed] [Google Scholar]
- 9.Nyska M, Howard CB, Matan Y, et al. Fracture of the posterior body of the talus – the hidden fracture. Arch Orthop Trauma Surg. 1998;117(1–2):114–117. doi: 10.1007/BF00703458. [DOI] [PubMed] [Google Scholar]
- 10.Paulos LE, Johnson CL, Noyes FR. Posterior compartment fractures of the ankle. A commonly missed athletic injury. Am J Sports Med. 1983 Nov-Dec;11(6):439–443. doi: 10.1177/036354658301100611. [DOI] [PubMed] [Google Scholar]
- 11.Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002 Sep 1;66(5):785–794. [PubMed] [Google Scholar]
- 12.Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA. 1994 Mar 16;271(11):827–832. [PubMed] [Google Scholar]
- 13.Netter F. Atlas d’anatomie humaine. 2e ed. États-Unis: Novartis; 1997. pp. 488–496. [Google Scholar]
- 14.Resnick D. Bone and Joint Imaging. 2e ed. Philadelphia, Pennsylvania: W.B. Saunders; 1996. p. 1169. [Google Scholar]
- 15.Cedell CA. Rupture of the posterior talotibial ligament with the avulsion of a bone fragment from the talus. Acta Orthop Scand. 1974;45(3):454–461. doi: 10.3109/17453677408989168. [DOI] [PubMed] [Google Scholar]
- 16.Kim DH, Hrutkay JM, Samson MM. Fracture of the medial tubercle of the posterior process of the talus: a case report and literature review. Foot Ankle Int. 1996 Mar;17(3):186–188. doi: 10.1177/107110079601700314. [DOI] [PubMed] [Google Scholar]
- 17.Warren NP, Knottenbelt JD. The Ottawa Ankle Rules and missed fractures of the talus. Emerg Med J. 2001 Nov;18(6):521. doi: 10.1136/emj.18.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]