Abstract
Aim:
To determine adherence to clinical practice guidelines in the medical, physiotherapy and chiropractic professions for acute and subacute mechanical low back pain through best-evidence synthesis of the healthcare literature.
Methods:
A structured best-evidence synthesis of the relevant literature through a literature search of relevant databases for peer-reviewed papers on adherence to clinical practice guidelines from 1995 to 2013. Inclusion of papers was based on selection criteria and appraisal by two reviewers who independently applied a modified Downs & Black appraisal tool. The appraised papers were summarized in tabular form and analysed by the authors.
Results:
The literature search retrieved 23 potentially relevant papers that were evaluated for methodological quality, of which 11 studies met the inclusion criteria. The main finding was that no profession in the study consistently attained an overall high concordance rating. Of the three professions examined, 73% of chiropractors adhered to current clinical practice guidelines, followed by physiotherapists (62%) and then medical practitioners (52%).
Conclusions:
This review showed that quality papers in this area of research are very limited. Notwithstanding, chiropractors appear to adhere to clinical practice guidelines more so than physiotherapists and medical practitioners, although there is scope for improvement across all three professions.
Keywords: evidence based guidelines, chiropractic, low back pain, medicine, physiotherapy
Abstract
Objectif :
Évaluer la conformité, dans les professions médicale, de physiothérapie et de chiropratique, avec les directives de pratique clinique en ce qui concerne la lombalgie mécanique aiguë et subaiguë par une synthèse des données probantes de la documentation sur les soins de santé.
Méthodologie :
Une synthèse structurée des données probantes provenant de la documentation pertinente, par une recherche des bases de données des publications examinées par les pairs sur le respect des directives de pratique clinique entre 1995 et 2013. Le choix des publications a été fait selon des critères de sélection et des évaluations distinctes par deux examinateurs qui ont utilisé l’outil d’évaluation Downs & Black modifié. Les documents d’évaluation ont été résumés en tableaux et ont été analysés par les auteurs.
Résultats :
La recherche des documents a extrait 23 publications potentiellement pertinentes qui ont été examinées pour leur qualité méthodologique, et dont 11 satisfaisaient les critères de sélection. La principale conclusion était qu’aucune des professions à l’étude n’a atteint de façon consistante un taux global élevé de concordance. Parmi les trois professions à l’étude, 73 % des chiropraticiens respectaient les directives de pratique clinique, suivis par les physiothérapeutes (62 %), et les médecins (52 %).
Conclusions :
Cette étude a démontré la rareté des publications de qualité dans ce domaine de recherche. Cela dit, les chiropraticiens semblent respecter les directives de pratique clinique plus que les physiothérapeutes et les médecins, bien qu’il y ait des possibilités d’amélioration dans les trois professions.
Keywords: directives basées sur des données probantes, chiropratique, lombalgie, médecine, physiothérapie
Introduction
Mechanical low back pain (LBP) is a common condition, which until recently has been depicted as self-resolving and transient. Emerging evidence contradicts the traditional assumption that spontaneous recovery occurs in the majority of patients, with back pain being neither insignificant nor self-limiting.1,2 While the majority of people with an episode of acute LBP improve enough to return to work within the first two weeks, the probability of recurrence within the first year ranges from 30 to 60%.3,4 In as many as one-third of people, the initial episode of LBP persists for a year.5 Should the pain be present in multiple spinal regions, the prognosis is much worse.6 A recent Scandinavian study found only 19% of people could report a single day of the year without back pain.7
After respiratory conditions, the majority of conditions managed by medical practitioners are musculoskeletal, despite 39% of sufferers choosing not to seek the care of any health professional, and of these musculoskeletal conditions, back pain is the most common.8–10 Patients with back pain spend about 75% more annually on health care than people without back pain and this does not include costs for lost work time or diminished productivity.11 Indeed, productivity loss and directly related health care expenditure continue to escalate along with prevalence. Between 1997 and 2005 in the US, expenditures for back and neck pain rose 65%, adjusted for inflation.12 Spinal disorders are consistently within the top ten of the most expensive health care presentations.9,13 Health system administrators clearly have a powerful incentive to ensure concordance with guidelines to encourage management that demonstrates positive treatment outcomes, cost efficiency and is patient-centred. Currently, fewer than 10% of Australians with low back pain get access to evidence-informed management.14
Guidelines
Formulation of guidelines is the natural sequitur to the goal of implementation of evidence-based practice. Thus nations including Canada, USA, UK and Australia have set about standardizing practice and publishing guidelines for virtually all aspects of health care; there exists even a formal Guidelines International Network.15–18 Compliance with guidelines however seems to be as problematic as developing them in the first place, evidence-based guidelines and systematic reviews have flourished, but seem to have had little impact on actual primary care practices.19,20
Guideline concordance (“practising in agreement with or in a way that is consistent with guidelines”) can be broadly considered within two contexts: 1) clinical decision-making, and 2) clinical intervention or management. In turn, management includes passive (clinician-centric) and active (patient-centric) aspects. Clinical decision-making relates to the utilisation of health history taking, physical examination and the use of diagnostic tests. Evaluation of guideline concordance (adherence) can thus take the form of ‘triage concordance’ and/or ‘management concordance’. This paper is concerned with the latter.
Recommendations in guidelines are made on the basis of being: 1) effective, 2) benefits outweighing risks, 3) costs being reasonable compared to expected benefits, and 4) the recommended actions being practical and feasible.21
Guideline panels usually have letters and numbers to indicate the strength of the recommendations, however they use them differently. This is potentially confusing, thus a binary system is now preferred; for example as employed by the GRADE panel.22,23 In this system, the strength of a recommendation reflects the extent of confidence that desirable effects of an intervention outweigh undesirable effects. Strong recommendations mean that most informed patients would choose the recommended management and that clinicians can structure their interactions with patients accordingly (i.e. most people in the same situation would want the recommended course of action and only a small proportion would not). Weak recommendations mean that patients’ choices will vary according to their values and preferences, and clinicians must ensure that patients’ care is in keeping with their values and preferences (i.e. most people in the same situation would want the recommended course of action, but many would not).
Guidelines are sometimes embedded within ‘models of care’, ‘codes of conduct’ and ‘clinical frameworks’ which contain expectations of practitioners regardless of profession; i.e., manual care practitioners should perform a comprehensive health history and appropriate physical examination; form a clinical impression and/or diagnosis; develop an individual plan of management; provide patient feedback in a timely manner; obtain informed consent; initiate appropriate care in a timely manner within scope of practice; manage the patient according to best available evidence; provide management within a bio-psychosocial/holistic model; empower the patient; and measure response to management.24–27
Methods
Contemporary evidence-based guidelines for the management of non-specific acute and subacute LBP are broadly homogenous.5,15,16,18,28–32 We developed a composite list of recommendations drawn from three representative EBG examples: the first, Western Australian Government Department of Health ‘Spinal Pain Model of Care’, from the jurisdiction where the authors reside; and the other two, recently published guidelines at the time of the study from the state of Oregon (USA) and the Institute for Clinical Systems Improvement (USA).5,25,28
For the management of acute and/or subacute mechanical LBP, the following evidence-based treatment and “core” recommendations are offered:
Identify potentially serious causes, ‘red flags’ and neural compression syndromes as well as non-spine pain origins
- Provide patient advice and education, using The Back Book.33 Included in advice is:
- Reassure the patient: “Recovery is to be expected”
- Manage fear avoidance and psychosomatic issues: “Hurt does not equal harm”
- Promote effective self-management of symptoms through appropriate advice
- Discourage bed rest
- Encourage the patient to stay active and continue ordinary activities (including work)
- Do not advise back-specific exercises (‘general’ exercise should be recommended to reduce recurrence, however, no specific exercise is preferred)
- May recommend appropriate medication within scope of practice*
The use of spinal manipulation (grade V; manual, high-velocity, low-amplitude, thrust-type manipulation) as a first-line or adjunctive treatment.
-
Exercise therapy, back school, joint mobilization (with therapeutic intent), massage (with therapeutic intent), electrotherapy/physical agents (heat, cold), and traction/lumbar supports were considered, but excluded from the protocol because the evidence for their use is either insufficient, equivocal, or negative. Although clinical guidelines offer mixed support for spinal manipulation, a recent practice guideline recommends its use, and specific trials support the effectiveness of spinal manipulation in the subgroup of patients with acute LBP of short duration.27
* Only guideline adherence scores from medical practitioners were collected with respect to medication and injection therapy as they are the only health care professionals legally able to utilise such methods in most jurisdictions.
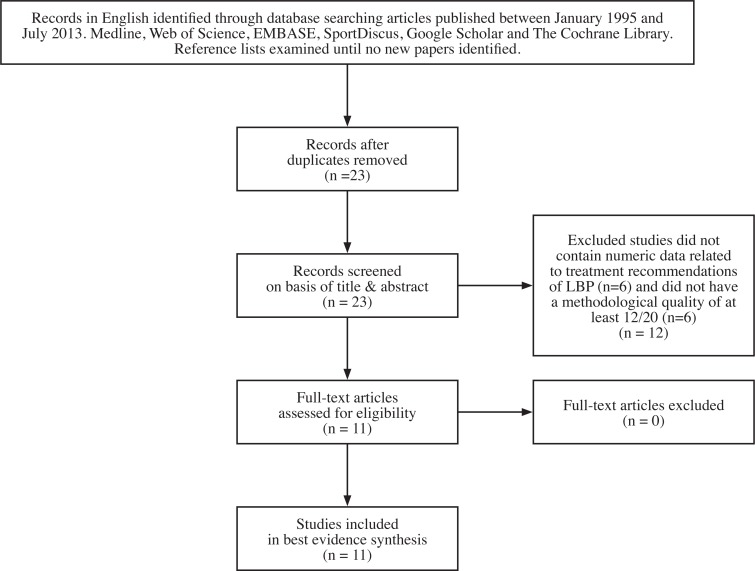
To obtain concordance data with guideline recommendations, six databases and search engines were searched for articles published between January 1995 and July 2013 [JL&RB]. These databases were Medline, Web of Science, EMBASE, SportDiscus, Google Scholar and The Cochrane Library. The search strategy is tabulated in Appendix 1. The abstracts of all papers returned by the search were assessed, and papers not directly relevant to Guideline Adherence for acute and/or subacute LBP were excluded. Inclusion of papers was based on selection criteria and appraised by two reviewers independently using a modified Downs & Black appraisal tool. Reference lists of included papers were examined and appropriate papers identified and reviewed. Any new papers in turn had their reference lists examined until no new papers were identified. Only papers written or transcribed in English were included, and papers were evaluated for methodological quality before inclusion in this study.
Measuring Methodological Quality
Each paper identified in the initial search was evaluated for methodological quality using a modified version of the system described by Downs and Black.34 Inclusion of papers were based on selection criteria and appraised by two independent reviewers. Scoring on the modified version could range between 0 and 20, with a higher score indicating higher methodological quality. Papers that scored below 12/20 (i.e. <60%) were deemed poor quality and excluded. This standard scoring methodology and inclusion criteria is considered valid and reliable for assessing randomized and nonrandomized studies and thus readily adapted for use in this context.35 This tool was chosen and adapted as there exists no “gold standard’ critical appraisal or widely accepted generic tool that can be applied equally well across study types and specifically not for allied health research requirements.36,37 Scoring was performed independently by two researchers [JL&RB], and although a third researcher [LA-W] was available in the event of disagreement, he was not required.
Concordance Evaluation Protocol
Evaluation was conducted using the following protocol:
When evidence was reported in the form of a statement but no figures were reported, the concordance score was not used in this study;
When numeric data were present, a fraction equal to the concordance to a particular recommendation was given, the denominator representing the total number of practitioners studied and the numerator representing the number of these practitioners that followed the recommendation. In some studies, numerators were determined from percentages, e.g., 50% concordance of 70 practitioners yielded a value of 35/70 and 25% concordance yielded 17.5/70 (numerators were not rounded to the nearest integer to avoid introducing further rounding errors);
When concordance scores for a particular recommendation were sourced from more than one study, a combined (pooled) score was calculated by adding both the numerators and denominators of the scores given, e.g., a concordance score of 35.5/70 and another of 40/60 yielded a value of 75.5/130 (58%).
Results
Of 23 studies initially identified, 6 did not contain numeric data related to treatment recommendations of LBP, and 6 did not have a methodological quality of at least 12/20 so were not included in this study. Thus, 11 studies met the inclusion criteria outlined above, were relevant within the framework of this study, and contained data that provided insight into guideline adherence. Methodological quality scores of the 11 studies included in this review ranged from 12 to 19, with a mean of 16.4 (Table I), and data from these studies were used to estimate concordance scores for the EBG recommendations (Table II).
Table I.
Methodological Quality Findings for Included Studies
| Question | Bishop and Wing (118) | Bishop et al (119) | Briggs et al (115) | Buchbinder and Jolley (120) | Coudeyre et al (121) | Harte et al (122) | Li & Bombardier (123) | Linton et al (124) | Little et al (125) | Pollentier & Langworthy (126) | Walker et al (127) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Is the hypothesis/aim/objective of the study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2. Are the main outcomes to be measured clearly described in the Introduction or Methods section? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| 3. Are the characteristics of the participants included in the study clearly described? | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 |
| 4. Are the distributions of principal confounders in each group of subjects to be compared clearly described? | 1 | 1 | 1 | 0 | 2 | 1 | 2 | 1 | 0 | 1 | 1 |
| 5. Are the main findings of the study clearly described? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 6. Does the study provide estimates of the random variability in the data for the main outcomes? | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 7. Have actual probability values been reported (e.g., 0.035 rather than <0.05) for the main outcomes except where the probability value is less than 0.001? | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 |
| 8. Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| 9. Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 10. Were the staff, places, and facilities representative of the treatment the majority of patients would receive? | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| 11. If any of the results of the study were based on ‘data dredging’, was this made clear? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 12. Were the statistical tests used to assess the main outcomes appropriate? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 13. Were the main outcome measures used accurate (valid and reliable)? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 14. Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 |
| 15. Did the study have sufficient power to detect clinically important effects? | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Total methodological quality points | 14 | 17 | 18 | 14 | 19 | 18 | 19 | 16 | 12 | 16 | 17 |
Included studies
1. Bishop PB., Wing PC. Compliance with clinical practice guidelines in family physicians managing worker’s compensation board patients with acute lower back pain. Spine J. 2003;3:442–50.
2. Bishop A, Foster N, Thomas E, Hay E. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135:187 – 95. PubMed PMID: doi:10.1016/j.pain.2007.11.010.
3. Briggs AM, Slater H, Smith AJ, Parkin-Smith GF, Watkins K, Chua J. Low back pain-related beliefs and likely practice behaviours among final-year cross-discipline health students. European Journal of Pain. 2012;doi: 10.1002/j.1532-2149.2012.00246.x.:[Epub ahead of print].
4. Buchbinder R, Jolley D. Improvements in general practitioner beliefs and stated management of back pain persist 4.5 years after the cessation of a public health media campaign. Spine (Phila Pa 1976). 2007;32:E156–62.
5. Coudeyre E, Rannou F, Tubach F, et al. General practitioners’ fear-avoidance beliefs influence their management of patients with low back pain. Pain. 2006; 124(330–7).
6. Harte A, Gracey J, Baxter G. Current use of lumbar traction in the management of low back pain: results of a survey of physiotherapists in the United Kingdom. Archives Physical Medicine Rehabilitation. 2005;86:1164–9.
7. Li L, Bombardier C. Physical therapy management of low back pain: an exploratory survey of therapist approaches. Phys Ther. 1999;81:1018 – 28.
8. Linton S, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002;12:223 – 32. PubMed PMID: doi:10.1023/A:1020218422974.
9. Little P, Smith L, Cantrell T, et al. General practitioners’ management of acute back pain: a survey of reported practice compared with clinical guidelines. BMJ. 1996 312:485–8.
10. Pollentier A, Langworthy J. The scope of chiropractic practice: A survey of chiropractors in the UK. Clinical Chiropractic. 2007;10:147 – 55. PubMed PMID: doi:10.1016/j.clch.2007.02.001.
11. Walker B, French S, Page M, O’Connor D, McKenzie J, Beringer K, et al. Management of people with acute low-back pain: a survey of Australian chiropractors. Chiropractic & Manual Therapies. 2011;19(1):29. PubMed PMID: doi:10.1186/2045-709X-19-29.
Table II.
GLC According to EBG Recommendation [Blank fields indicate no data]
| Recommendation topic | Study | Chiropractors | Physiotherapists | Medical Practitioners | |||
|---|---|---|---|---|---|---|---|
| Fraction | Percent | Fraction | Percent | Fraction | Percent | ||
| Self-management and appropriate advice | Briggs et al | 41.7/46 | 91% | 105.2/171 | 80% | 80.3/176 | 52% |
| Li and Bombardier | 255.6/274 | ||||||
| Linton et al | 54.0/71 | 34.2/60 | |||||
| Little et al | 94.5/163 | ||||||
| Bed rest | Briggs et al | 39.0/46 | 97% | 127.4/171 | 87% | 114.6/176 | 86% |
| Buchbinder and Jolley | 413.9/511 | ||||||
| Coudeyre et al | 785.9/845 | ||||||
| Li and Bombardier | 259.1/274 | ||||||
| Walker et al | 270.4/274 | ||||||
| Physical Activity (including work) | Bishop and Wing | 55% | 87% | 30.6/139 | 71% | ||
| Briggs et al | 35.5/46 | 117.4/171 | 91.7/176 | ||||
| Buchbinder and Jolley | 467.6/511 | ||||||
| Li and Bombardier | 267.7/274 | ||||||
| Walker et al | 139.7/274 | ||||||
| Spinal manipulation | Bishop and Wing | 76% | 18% | 70.2/139 | 34% | ||
| Buchbinder and Jolley | 143.1/511 | ||||||
| Li and Bombardier | 48.6/274 | ||||||
| Little et al | 33.2/66 | ||||||
| Walker et al | 208/274 | ||||||
| Acupuncture | Buchbinder and Jolley | 93% | 82% | 107.3/511 | 38% | ||
| Li and Bombardier | 223.8/274 | ||||||
| Little et al | 149.5/159 | ||||||
| Walker et al | 254.1/274 | ||||||
| Traction and short-wave diathermy | Buchbinder and Jolley | 95% | 54% | 281.1/511 | 55% | ||
| Harte et al | 644.3/1239 | ||||||
| Li and Bombardier | 175.4/274 | ||||||
| Walker et al | 260.2/274 | ||||||
| Recommends or uses physiotherapy | Bishop and Wing | 23% | 50% | 77.8/139 | 41% | ||
| Briggs et al | 10.6/46 | 85.3/171 | 40.3/176 | ||||
| Buchbinder and Jolley | 219.7/511 | ||||||
| Recommends or uses chiropractic | Briggs et al | 45.0/46 | 99% | 17.4/171 | 10% | 12.7/176 | 7% |
| Pollentier and Langworthy | 247.8/249 | ||||||
| Appropriate use of diagnostic imaging | Bishop and Wing | 32% | 88% | 132.1/139 | 81% | ||
| Bishop et al | 507.5/580 | 402.2/442 | |||||
| Buchbinder and Jolley | 393.5/511 | ||||||
| Walker et al | 87.7/274 | ||||||
| Medication | Bishop and Wing | N/A | N/A | 95.2/139 | 46% | ||
| Briggs et al | 50.9/176 | ||||||
| Buchbinder and Jolley | 224.8/511 | ||||||
| Trigger point injection therapy | N/A | N/A | |||||
| Lumbar support | Li and Bombardier | 91% | 258.6/274 | 94% | |||
| Walker et al | 250.7/274 | ||||||
| Heat | Li and Bombardier | 42% | 139.9/274 | 51% | |||
| Walker et al | 116.3/274 | ||||||
| Spinal mobilisation | Li and Bombardier | 69% | 90.3/274 | 33% | |||
| Walker et al | 189.2/274 | ||||||
| Red flags” and neural compression syndromes | Bishop and Wing | 60% | 7.0/139 | 5% | |||
| Li and Bombardier | 164.4/274 | ||||||
| Back-specific exercises | Li and Bombardier | 209.3/274 | 76% | ||||
| TENS | Buchbinder and Jolley | 47% | 132.9/511 | 49% | |||
| Li and Bombardier | 128.8/274 | ||||||
| LASER | Li and Bombardier | 267.2/274 | 98% | ||||
| Ultrasound | Li and Bombardier | 155.4/274 | 57% | ||||
| Massage | Walker et al | 134.8/274 | 49% | ||||
| Reassurance | |||||||
| Fear avoidance and psychosomatic issues | |||||||
| Total: Average for recommendations where all professions had data | 73.44% | 61.78% | 51.67% | ||||
| Total: Overall for recommendations common to all three professions | 70.15% | 63.06% | 47.08% | ||||
Fraction = concordance to a particular recommendation where the denominator represents the total number of practitioners studied and the numerator represents the number of practitioners who followed the recommendation.
Concordance Data
The numbers of EBG recommendations with concordance scores were 13 for chiropractors, 12 for medical practitioners and 17 for physiotherapists, and average concordance percentages over these recommendations were 70.2, 63.1 and 47.1 for each profession, respectively.
There were recommendations with concordance scores available for all three professions related to providing advice on self-management, bed rest and physical activity including work. Recommendations concerning the use of medications only had concordance scores for medical practitioners due to the inability of chiropractors and physiotherapists to prescribe medication. Only physiotherapists had concordance scores for guidelines pertaining to back exercises and use of LASER, and only chiropractors had a score for the use of massage therapy.
Of the recommendations common to all three professions, chiropractors had the highest concordance scores for six, but the lowest concordance scores for three, and their average concordance was 73.4%. Average concordance was 61.8% for physiotherapists and 51.7% for medical practitioners. The score for chiropractors was notably negatively affected by imaging use which may technically be considered a ‘triage guideline’.38
In regard to recommending their own therapy, chiropractors scored 99% for recommending or using their treatment, while physiotherapists only scored 50% for recommending or using physiotherapy. In regard to recommending each other’s discipline, chiropractors were more than twice as likely to recommend or use physiotherapy (23%) than physiotherapists were to recommend or use chiropractic (10%). Medical practitioners claim to recommended or use chiropractic and physiotherapy at very different rates: 41% for physiotherapy and 7% for chiropractic.
Although TENS and traction are considered ineffective or possibly harmful25, their dissuasion received a low concordance score of around 50% by physiotherapists. The use of spinal manipulation, received low recommendations from both medical practitioners and physiotherapists with 33% and 17%, respectively. Likewise, medical practitioners and physiotherapists were not overly concordant with identifying red flags (5% and 60% respectively). Furthermore, medical practitioners had a lower rating for promoting self-management through advice than the other two professions (52% versus 80% and 91%).
Discussion
We examined the guideline adherence for the management of non-specific acute and subacute LBP reported in the literature relating to the professions of medicine, physiotherapy and chiropractic. These three professions were chosen because, between them, they deliver the vast majority of management of these conditions in Western societies. It is an important consideration that guidelines are intended to enable, guide, motivate, or sometimes ‘cajole’ physicians and health care providers to deliver certain types of care. However, they do not directly determine the care provided to a particular patient.21 Although research is conducted and guidelines formulated for populations, their application in a specific case is still the domain of the individual practitioner. Our results, which demonstrated that no profession in the study consistently attained an overall high concordance rating (according to the Downs & Black scoring system), are consistent with other studies that demonstrate that many primary care physicians continue to be non-concordant.39–44
Utilisation
According to the Canadian Institute of Health Economics study by Scott et al. (2010), up to 25% of patients with back pain seek help from a health care provider, with 75% of these patients presenting to either a physician or a chiropractor.45,46 Primary care physicians undertake the initial evaluation in 65% of LBP cases and often ultimately become the sole provider for these patients.47 Most patients tend to visit more than one provider, and between 10% and 50% of patients receive physiotherapy.48–50 In Canada, chiropractic services have remained relatively stable over the last decade at about 11%. Utilization is higher in provinces where public funding was or continues to be available.51 North American and UK demographics are reflected in Australia where Sibbritt and Adams (2010) also found Australians with longer-term back pain tended to consult more with chiropractors, and Walker, Muller and Grant (2004) noted that chiropractors were the second-most utilised practitioners sought for care (19.1%) after medical care (22.4%) for back pain.52,53 In Australia, although the number of physiotherapists working in the private sector is 2.9 times larger than that of chiropractic, chiropractors provide approximately two and a half times more services than physiotherapists.54
Medicine
Medical practitioners are the health professionals most likely to be consulted for spinal pain in developed countries.46,53 Non-steroidal anti-inflammatory drugs and acetaminophen are popular treatments among medical practitioners and some studies find they are generally prescribed according to guidelines for acute LBP, and guideline recommendations against the use of antidepressants are followed. However, recent data from the USA demonstrate the opposite; ‘simple analgesia’ prescription rates are falling and inappropriate opioid prescription rates are rising, along with referral for surgical consultation for non-specific back pain.55 Up to 45% of medical practitioners do not follow guidelines and prescribe oral steroids for acute LBP.39 A recent Australian study found guideline adherence for opioid prescription was poor; in fact, no medical practitioner in the study was always compliant with all guideline items, and only 31% usually followed most items.56 Given the pathway to misuse and abuse and the known illicit market for this class of drug, this is of significant concern. The rise in use of opioids for pain relief has in fact become a major issue for health care, placing a significant economic strain on developed economies.55,57
Scott et al. found that the majority of Canadian medical practitioners correctly recommended the use of heat or ice and discouraged prolonged bed rest for patients with acute LBP, although some studies still recorded high rates of discordance regarding the prescription of bed rest.46 Medical practitioners are more likely to be receptive to a guideline when they are aware of shortcomings in the care that they provide, however, somewhat ironically, those with a special interest in LBP are probably the group in greatest need of guidance58–60 For example, Di Iorio et al (2000) measured overall concordance in a sample of 87 family medical practitioners and found that 68% adhered to guidelines on LBP, but only 6% achieved a concordance level greater than 90%.39 Overmeer et al (2005) found no significant difference in practice behaviour between Swedish medical practitioners who were familiar with guidelines and those who were not.61
Physiotherapy
Physiotherapists occupy a wide variety of roles in health care. These roles include working in hospitals, work-places, sports and community centres, women’s health centres, rehabilitation centres, aged care facilities, mental health centres, chronic disease management centres, the private sector, schools, education and research facilities, and even with animals.62
Multiple studies indicate that passive interventions, such as electrotherapies, remain popular with physiotherapists, notwithstanding their lack of evidence.61,63–69 Treatments supported by guidelines, such as spinal manipulation, are underused, whereas ineffective treatments are overused: specifically, contrary to guideline recommendations, transcutaneous electrical nerve stimulation (TENS) and ultrasound are still considered to be effective treatments for acute LBP by many physiotherapists (and medical practitioners).46,68 Contrary to the prevailing perception of the profession being strongly evidence-based, studies consistently demonstrate resistance to adoption of evidence-based practice among physiotherapists, even when specific education and post-graduate and professional development training is undertaken.70,71
Chiropractic
The demographics of chiropractic are much easier to quantify than either physiotherapy or medicine due to its relatively homogenous nature. Of approximately 82,000 chiropractors worldwide, the vast majority are in private practice and provide care directly to the public. Their care is usually funded by direct payment ‘out of pocket’ from their patients.72 About 1% are in academia and a tiny fraction are in full-time research.73 There are approximately 4,300 registered chiropractors in Australia, and each year it is estimated that over three million people (∼16% of the Australian population) consult a chiropractor at least once.25,74–76 A wide variety of manual and mechanically assisted spinal manipulative techniques are employed by chiropractors; however, chiropractic is still generically identified by its hallmark description of providing ‘non-pharmaceutical, non-surgical spinal care’.77–79 This is accomplished primarily by manual methods of spinal manipulation therapy (adjustment) (SMT) and active care and lifestyle advice.80 Wenban (2003) reported that, when compared to the many other studies of similar design that have evaluated the extent to which different medical specialties are evidence based, chiropractic practice was found to have the highest proportion of care (68.3%) supported by good-quality experimental (RCT) evidence.81 This compares favourably to mainstream medicine where, for example, Imrie and Ramney (2003) found an average of 37.0% of medical practice to be based on RCTs (notably excluding spinal care).82
General
Scott, Moga and Harstall use the term “Know-Do Gap” (2010) in their robust work and concluded that “Guidelines are often used to establish standards of care and provide a benchmark for evidence-based practice, but their directives are not always heeded”.46
Several studies have investigated possible explanations for the high levels of non-concordance with guidelines demonstrated by health professionals. Li and Bombardier (2001) concluded that only half of the (physical) therapists in their study confirmed the usefulness of practice guidelines in managing any clinical conditions, including LBP.63 This finding may indicate some reluctance to embrace guidelines, especially for managing acute lumbar impairment. Other studies included patients’ demands83, excessive commitment to particular modes of therapy, lack of awareness or outcome expectancy, inertia of previous practice43, and the health care practitioners’ own perceptions of treatment effectiveness84 as reasons for discordance with guidelines.
Education
Suboptimal guideline adherence by medical practitioners in the management of spinal pain may be related to deficiency of musculoskeletal medicine in undergraduate medical education, a phenomenon not lost on the World Health Organization.85–87 This observation has resulted in a number of follow-up studies highlighting the deficiencies of medical management of spinal pain compared to physiotherapists and chiropractors88,89 and medicine in general46,90. Our study is consistent with this phenomenon with medical practitioners scoring lowest of the three.
Red Flags
Of some concern is the lack of concordance in identifying ‘red flags’. Red flags are features of the patient’s medical history and clinical examination that may suggest a higher risk of serious disorders, such as infection, inflammatory disease, cancer or fracture.91–93 The exclusion of specific pathologies is step one of the clinical assessment, and clinical guidelines recommend that the identification of ‘red flags’ as the ideal method to accomplish this.94,95 Approximately 10% of all malignancies have symptomatic spine involvement as the initial manifestation of the disease, including multiple myeloma, non-Hodgkin’s lymphoma, and carcinoma of the lung, breast and prostate.96 Early detection and treatment of spinal malignancies are important to prevent further spread of metastatic disease and the development of complications such as vertebral fracture and spinal cord compression.97 One reason put forward for the low rate of concordance in the red flag category is that, despite their inclusion in the guidelines and their apparent clinical importance, the usefulness of screening using ‘red flags’ in patients with LBP continues to be robustly debated, and there remains very little information on their diagnostic accuracy and how best to use them in clinical practice.91,93,98
Medications
Our findings in regard to the administration of medications are also consistent with a number of recent studies that have examined comparative competence and attitudes toward evidence-based practice among primary spinal care practitioners. Di Iorio (2000) found many medical practitioners recommend drugs discouraged by the applicable guideline.39 Although we did not categorise the types of medications, this trend is consistent with other studies that show that, despite there being no clear evidence supporting the prescription of, for example; antidepressants in the treatment of LBP, up to 23% of general practice physicians prescribe antidepressants.39,99–102
Referral Patterns
The referral patterns in this study followed the trends set by other studies that demonstrated a significant difference between medical referrals to physiotherapists and to chiropractors. In our study overall 41% of medical practitioners would refer to physiotherapists while only 7% would refer to chiropractors. These data are an interesting paradox; considering about 38% of physicians admit using CAM treatments themselves for medical conditions, most notably acupuncture, chiropractic and osteopathy.103 Only 30% of medical practitioners in a study by Greene et al. (2006)104 and between 29–50% in various other studies105–107 have ever made a formal referral to a chiropractor. Several possible explanations for medical practitioners’ unwillingness to ‘formalise’ their relationships with chiropractors have been suggested and include the perception that alternative care providers could be a threat to their practices. Some of the medical practitioners also mentioned that they do not know enough about chiropractic to have an opinion or do not view chiropractic as a legitimate health profession; they thereby fear malpractice litigation108, or it may simply be a manifest lack of inter-professional trust109. Traditionally, medical practitioners receive little training in common musculo-skeletal problems in undergraduate medical school, during medical internship, and in post-graduate education and often have limited knowledge about the suite of nonpharmacological treatments available to patients. Surveys and interviews indicate that medical practitioners have a lack of confidence in examining and providing treatment to patients with back pain, and many medical practitioners feel ill-equipped, often relying on pharmacological management instead of referring to those musculoskeletal practitioners such as musculoskeletal physiotherapists, chiropractors and osteopaths that are specifically equipped to deliver manual therapy.58,110 The impact of low referral rates to chiropractors and other manual therapists is not benign but manifests in greater suffering and expense to the patients who present with LBP. Cost-effectiveness data from randomised clinical trials indicate that primary care for patients with LBP is not cost-effective unless it also involves one or more added components such as exercise, spinal manipulation or behavioural counselling.111,112 Indeed the North American Spine Society recommends spinal manipulation—5 to 10 sessions over 2 to 4 weeks—should be considered before surgery or narcotics.113
Another finding of this study was that 99% of chiropractors would recommend or use chiropractic care for treatment of LBP, but only 50% of physiotherapists would recommend or use physiotherapy. One reason for this trend may be that some physiotherapists still use modalities that have questionable effectiveness and result in unfavourable patient outcomes. For example, Li and Bombardier (2001) found mechanical spinal traction, which has consistently been shown to be of little benefit for acute and subacute lumbar impairment and is not recommended by the guidelines, was preferred by about 30% of the physical therapists in their study for acute sciatica. In the same study, Li and Bombardier also found that, despite the reported success of spinal manipulation in the treatment of LBP, only 5% of the physical therapists reported that they would use spinal manipulation to treat patients with acute lumbar impairment, as compared with more than a third of the therapists who indicated that they would use mobilisation, which may not be as effective.63 This discrepancy could be explained by the small number of therapists in the study who were trained to perform spinal manipulation. Although most of the respondents in the study had received postgraduate training in manual therapy, only 8.8% completed courses that included joint manipulation.
Beliefs
Another explanation may suggest a difference in belief systems that each profession holds with respect to treatment of LBP and the confidence level they hold for the desired patient outcomes. While some chiropractors may hold unorthodox views which are in contrast to current scientific paradigms, at least in Canada they are definitely a minority.114 In a study that looked specifically at beliefs held by 600 university undergraduate students in the health care professions, Briggs et al. (2012) found chiropractic, and to a lesser extent physiotherapy students, reported significantly more helpful beliefs for management of spinal pain compared with the other disciplines, while medical and pharmacy students reported the least helpful beliefs. Although this study did not look specifically at the interventions of practicing health professionals, one could predict that beliefs, at least to a certain degree, may influence actions. If this is true, the high levels of concordance with recommendations for physical activity, work and bed rest across disciplines may reflect practitioners’ beliefs.115 One is left to wonder what is worse, to know and not do, or not know in the first place?46
Given the substantial financial and other resources devoted to formulating guidelines, the question could be reasonably asked; “who cares, since so many practitioners don’t follow them?” Health authorities clearly care and at least in the third party payer context, are beginning to actually require practitioners to practice within clinical frameworks regardless of their profession.26 Efforts are underway to look at questions like this, from a quality perspective, not just a compliance one. For example in the USA, the National Center for Quality Assurance has best practices by which it judges physician behaviours, such as relates to both diagnosis and treatment and may reward practitioners for “best practices”.116 Our work may serve to corroborate existing evidence of the comparative cost-effectiveness of chiropractic.117
Limitations of the Study
The authors recognize the methodological study limitations with respect to adapting the appraisal tool to assess concordance and when comparing results from different studies that used various designs. In addition, while assessment of LBP can include ordering of imaging studies for some patients, concordance was not assessed in great detail in our study.
Lack of data in several categories for all professions limited our comparisons, although this seems to be minimal since averages of the guidelines where all professions had data (medicine 51.7%; physiotherapy 61.8%; chiropractic 73.4%) and the overall averages (medicine 47.1%; physiotherapy 63.1%; chiropractic 70.2%) were relatively unchanged.
This study was not designed as a systematic review, rather a best evidence synthesis so it was thorough but not exhaustive. Papers prior to 1995 were excluded; as there was less homogeneity of guidelines prior to that time, it would not be relevant to evaluate concordance to guidelines that did not exist at the time. While our study was ‘systematic’, it was not a systematic review (according to all the PRISMA protocols), due to the constraints of human and financial resources available.
Despite the limitations, we believe that the findings from this work are important. To our knowledge, this is the first in-depth study comparing the practice behaviors of medical practitioners, physiotherapists and chiropractors with respect to guideline adherence for acute and sub-acute non-malignant mechanical LBP.
The authors caution that this study should not be considered an end, but a beginning. Although the chiropractic profession in our study fared the best of the three, this is by no means a cause for complacency, rather it highlights the need for further research, especially within the chiropractic sector.
Conclusion
Adoption of evidence-based practice continues to be a challenge for chiropractors, physiotherapists and medical practitioners as no profession attained satisfactorily high guideline adherence in our view.
We found chiropractors have the highest levels of guideline adherence, and chiropractors and physiotherapists are both significantly more guideline concordant than medical practitioners with respect to management of acute and subacute low back pain. It seems clear that medical practitioners often rely on pharmacological management instead of referring to musculoskeletal practitioners, who are specifically equipped to deliver manual care and other appropriate management that has a robust evidence basis. The impact of low referral rates to chiropractors and other manual therapists is not benign but manifests in greater suffering and more expense to the patients who present with acute and subacute low back pain.
More quality research is urgently needed in order to accurately determine levels of guideline adherence and just as importantly identify the reasons that practitioners are not concordant with guidelines. Wider concordance with guidelines for management of spinal pain has the potential to result in significant savings in health care expenditure and a significant reduction in disability and morbidity.
Figure 1:
Flow Chart of Study
Acknowledgments
A.L Rosner for review of manuscript.
Abbreviations
- EBG:
Evidence-Based Guideline
- GP:
General Practitioner (Australia)
- LASER:
Light Amplification by Stimulated Emission of Radiation Therapy
- LBP:
Low Back Pain
- SMT:
Spinal Manipulative Therapy
- TENS:
Transcutaneous Electrical Nerve Stimulation
Appendix 1: Search Terms
| Main search terms | Relevant associated words |
|---|---|
| Clinical Guidelines | Guideline AND/OR Protocol AND/OR Clinical guideline AND/ OR Model of Care AND/OR evidence based guideline |
| Low Back Pain | Back pain AND/OR Low back pain AND/OR Non-malignant low back pain AND/OR Mechanical low back pain AND/OR Non-specific low back pain AND/OR Subacute low back pain |
| Facilitators | Enable* AND/OR support* AND/OR Adherence AND/OR Compliance AND/OR Concordance AND/OR Observance |
Footnotes
- LW conceived the work, conducted literature searches, drafted and reviewed the text.
- RB conducted literature searches, cross-checked and analysed results, drafted and reviewed the text.
- GPS reviewed and edited the text.
- JL compiled and analysed data and reviewed the text.
- AB drafted and reviewed the text, conducted statistical analysis.
- The authors declare they have no competing interests beyond LA-W, RB and GP-S being registered chiropractors.
- JL was supported with a stipend as a research assistant.
References
- 1.Itz CJ, Geurts JW, van Kleef M, Nelemans P. Clinical course of non-specific low back pain: A systematic review of prospective cohort studies set in primary care. European J Pain. 2013;17(1):5–15. doi: 10.1002/j.1532-2149.2012.00170.x. [DOI] [PubMed] [Google Scholar]
- 2.Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 2008:337. doi: 10.1136/bmj.a171. 2008-07-07 00:00:00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pengel L, Herbert R, Maher C, Refshauge K. Acute low back pain: systematic review of its prognosis. BJM. 2003;327:3. doi: 10.1136/bmj.327.7410.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayden J, van Tulder M, Malmivaara A, Koes B. Exercise therapy for treatment of non-specific low back pain (review) Cochrane Database Syst Rev . 2005:CD000335. doi: 10.1002/14651858.CD000335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goertz M, Thorson D, Bonsell J, Bonte B, Campbell R, Haake B, et al. Adult Acute and Subacute Low Back Pain. Institute for Clinical Systems Improvement [Internet]. Updated November 2012. Available from: https://www.icsi.org/_asset/bjvqrj/LBP.pdf.
- 6.Vasseljen O, Woodhouse A, Bjørngaard J, Leivseth L. Natural course of acute neck and low back pain in the general population: the HUNT study. Pain. 2013;154(8):1237–44. doi: 10.1016/j.pain.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 7.Leboeuf-Yde C, Lemeunier N, Wedderkopp N, Kjaer P. Absence of low back pain in the general population followed fortnightly over one year with automated text messages. Chiropractic & Manual Therapies. 2014;22(1):1. doi: 10.1186/2045-709X-22-1. PubMed PMID: doi:10.1186/2045-709X-22-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AIHW . Arthritis and musculoskeletal conditions in Australia. Canberra: Australian Institute of Health and Welfare; 2005. [Google Scholar]
- 9.Buchbinder R, Jolley D, Wyatt M. Breaking the back of back pain. Med J Aust. 2001;175:456–7. doi: 10.5694/j.1326-5377.2001.tb143675.x. [DOI] [PubMed] [Google Scholar]
- 10.Wildenhaus K. Feeling the economic effects of back pain. AHIP Coverage. 2004;45(3):78–80. 2, 4. [PubMed] [Google Scholar]
- 11.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656–64. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 12.Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997–2006. Spine. 2009;34(19):2077–84. doi: 10.1097/BRS.0b013e3181b1fad1. [DOI] [PubMed] [Google Scholar]
- 13.Foster N. Barriers and progress in the treatment of low back pain. BMC Med. 2011;9(1):108. doi: 10.1186/1741-7015-9-108. PubMed PMID: doi:10.1186/1741-7015-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slater H, Briggs AM, Smith AJ, Bunzli S, Davies SJ, Quintner JL. Implementing evidence-informed policy into practice for health care professionals managing people with low back pain in Australian rural settings: A preliminary prospective single-cohort study. Pain Medicine. 2014 doi: 10.1111/pme.12351. online preview. [DOI] [PubMed] [Google Scholar]
- 15.CMA Infobase: Clinical Practice Guidelines (CPGs): Canadian Medical Association Available from: http://www.cma.ca/cpgs/ [DOI] [PubMed]
- 16.UK Clinical Guidelines Available from: http://www.patient.co.uk/guidelines.asp.
- 17.National Guideline Clearinghouse US Department of Health & Human Services; Agency for Healthcare Research and Quality. Available from: http://www.guideline.gov/
- 18.(G-I-N) The Guidelines International Network. Available from: http://www.g-i-n.net/about-g-i-n.
- 19.Carthey J, Walker S, Deelchand V, Vincent C, Harrop Griffiths W. Breaking the rules: understanding non-compliance with policies and guidelines. BMJ. 2011:343. doi: 10.1136/bmj.d5283. 2011-09-13 00:00:00. [DOI] [PubMed] [Google Scholar]
- 20.Cherkin D, Kovacs F, Croft P, Borkan J, Foster N, Oberg B, et al. The Ninth International Forum For Primary Care Research On Low Back Pain. International Organizing Committee Of The Ninth International Forum For Primary Care Research On Low Back Pain And All The Participants. Spine. 2009;34:304–7. doi: 10.1097/BRS.0b013e3181928f9a. [DOI] [PubMed] [Google Scholar]
- 21.Eddy DM. Evidence-based medicine: A unified approach. Health Affairs. 2005;24(1):9–17. doi: 10.1377/hlthaff.24.1.9. [DOI] [PubMed] [Google Scholar]
- 22.Guyatt G, Oxman A, Kunz R, Falck-Ytter Y, Vist G, Liberati A, et al. Rating quality of evidence and strength of recommendations: Going from evidence to recommendations. BMJ. 2008;336(7652):1049–51. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schunemann H, Best D, Vist G, Oxman A. Letters, numbers, symbols and words: how to communicate grades of evidence and recommendations . CMAJ. 2003;169:677–80. [PMC free article] [PubMed] [Google Scholar]
- 24.CBA Code of Conduct for Chiropractors 2010. Available from: http://www.chiropracticboard.gov.au/index.php.
- 25.Department of Health WA . Spinal Pain Model of Care. Perth: Health Networks Branch, Department of Health, Western Australia; 2009. [Google Scholar]
- 26.TAC and WorkSafe Victoria Clinical Framework for the delivery of Health Services 2004. Available from: www.worksafe.vic.gov.au, www.tac.vic.gov.au.
- 27.Parkin-Smith GF, Norman IJ, Briggs E, Angier E, Wood TG, Brantingham JW. A structured protocol of evidence-based conservative care compared with usual care for acute nonspecific low back pain: A randomized clinical trial. Arch Phys Med Rehab. 2012;93(1):11–20. doi: 10.1016/j.apmr.2011.08.022. [DOI] [PubMed] [Google Scholar]
- 28.Livingston C, King V, Little A, Pettinari C, Thielke A, Gordon C. State of Oregon Evidence-based Clinical Guidelines Project Evaluation and management of low back pain: A clinical practice guideline based on the joint practice guideline of the American College of Physicians and the American Pain Society (Diagnosis and treatment of low back pain) Salem: Office for Oregon Health Policy and Research; 2011. [Google Scholar]
- 29.Guidelines for Chiropractic Quality Assurance Practice Parameters. New York: Aspen Publishers, Inc; 1993. [Google Scholar]
- 30.Airaksinen O, Brox J, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. COST B13 European guidelines for the management of chronic non-specific low back pain. Eur Spine J. 2006;15:S192–S300. doi: 10.1007/s00586-006-1072-1. PubMed PMID: doi:10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. The Spine Journal. 2010;10(6):514–29. doi: 10.1016/j.spinee.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 32.Koes B, van Tulder M, Lin C, Macedo L, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19:2075–94. doi: 10.1007/s00586-010-1502-y. PubMed PMID: doi:10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burton K, et al. The Back Book – UK Edition 2nd Edition: TSO (The Stationery Office) 2002. [Google Scholar]
- 34.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health . 1998 Jun;52(6):377–84. doi: 10.1136/jech.52.6.377. PMC1756728. Epub 1998/10/09. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaminskyj A, Frazier M, Johnstone K, Gleberzon BJ. Chiropractic care for patients with asthma: A systematic review of the literature. J Can Chiropr Assoc . 2010 Mar;54(1):24–32. PMC2829683. Epub 2010/03/03. eng. [PMC free article] [PubMed] [Google Scholar]
- 36.Crowe M, Sheppard L. A review of critical appraisal tools show they lack rigor: Alternative tool structure is proposed. J Clinical Epidemiology. 2011;64(1):79–89. doi: 10.1016/j.jclinepi.2010.02.008. 1// [DOI] [PubMed] [Google Scholar]
- 37.Katrak P, Bialocerkowski A, Massy-Westropp N, Kumar VS, Grimmer K. A systematic review of the content of critical appraisal tools. BMC Medical Research Methodology. 2004;4(1):22. doi: 10.1186/1471-2288-4-22. PubMed PMID: doi:10.1186/1471-2288-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ammendolia C, Côté P, Hogg-Johnson S, Bombardier C. Do chiropractors adhere to guidelines for back radiographs?: A study of chiropractic teaching clinics in Canada. Spine. 2007;32(22):2509–14. doi: 10.1097/BRS.0b013e3181578dee. [DOI] [PubMed] [Google Scholar]
- 39.Di Iorio D, Henley E, Doughty A. A survey of primary care physician practice patterns and adherence to acute low back problem guidelines. Arch Fam Med. 2000;9(10) doi: 10.1001/archfami.9.10.1015. [DOI] [PubMed] [Google Scholar]
- 40.Webster BS, CT, Huang YH, Matz S, Christiani DC. Physicians’ initial management of acute low back pain versus evidence-based guidelines. Influence of sciatica. J Gen Intern Med. 2005;20:1132–5. doi: 10.1111/j.1525-1497.2005.0230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mahmud M, Webster B, Courtney T, et al. Clinical management and the duration of disability for work-related low back pain. J Occup Env Med / American College of Occupational and Environmental Medicine. 2000;42:1178–87. doi: 10.1097/00043764-200012000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Schers H, Braspenning J, Drijver R, et al. Low back pain in general practice: reported management and reasons for not adhering to the guidelines in The Netherlands. British J General Practice : the Journal of the Royal College of General Practitioners. 2000;50:640–4. [PMC free article] [PubMed] [Google Scholar]
- 43.Cherkin D, Deyo R, Wheeler K, Ciol M. Physician views about treating low back pain. The results of a national survey. Spine (Phila Pa 1976) 1995;20:1–9. doi: 10.1097/00007632-199501000-00001. discussion -10. [DOI] [PubMed] [Google Scholar]
- 44.Fritz JM CJ, Brennan GP. Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Medical care. 2007;45:973–80. doi: 10.1097/MLR.0b013e318070c6cd. [DOI] [PubMed] [Google Scholar]
- 45.Nyiendo J, Haas M, Goldberg B, Sexton G. Pain, disability, and satisfaction outcomes and predictors of outcomes: A practice-based study of chronic low back pain patients attending primary care and chiropractic physicians. J Manip Physiol Ther. 2001;24:433–9. [PubMed] [Google Scholar]
- 46.Scott N, Moga C, Harstall C. Managing low back pain in the primary care setting: The know-do gap. Pain Res Manage. 2010;15(6):392. doi: 10.1155/2010/252695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Devereaux MW. Low back pain. Prim Care. 2004;31:33–51. doi: 10.1016/S0095-4543(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 48.Werner EL, Ihlebaek C, Skouen JS, Laerum E. Beliefs about low back pain in the Norwegian general population: Are they related to pain experiences and health professionals? Spine. 2005;30:1770–6. doi: 10.1097/01.brs.0000171909.81632.fe. [DOI] [PubMed] [Google Scholar]
- 49.Poitras S, Blais R, Swaine B, Rossignol M. Management of work-related low back pain: A population-based survey of physical therapists. Physical Therapy. 2005 Nov;85(11):1168–81. 2005. [PubMed] [Google Scholar]
- 50.Foster NE, Thompson KA, Baxter GD, Allen JM. Management of nonspecific low back pain by physiotherapists in Britain and Ireland: A descriptive questionnaire of current clinical practice. Spine. 1999;24(13):1332. doi: 10.1097/00007632-199907010-00011. [DOI] [PubMed] [Google Scholar]
- 51.McManus E, Mior S. ACC Conference Proceedings; Impact of provincial subsidy changes on chiropractic utilization in Canada. J Chiropr Educ. 2013;27(1):73. [Google Scholar]
- 52.Sibbritt D, Adams J. Back pain amongst 8,910 young Australian women: a longitudinal analysis of the use of conventional providers, complementary and alternative medicine (CAM) practitioners and self-prescribed CAM. Clinical Rheumatology. 2010;29(1):25–32. doi: 10.1007/s10067-009-1299-4. [DOI] [PubMed] [Google Scholar]
- 53.Walker BF, Muller R, Grant WD. Low back pain in Australian adults. Health provider utilization and care seeking. J Manipulative Physiol Ther. 2004;27(5):327–35. doi: 10.1016/j.jmpt.2004.04.006. PubMed PMID: doi:10.1016/j.jmpt.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 54.Engel R, Brown B, Swain M, Lystad R. The provision of chiropractic, physiotherapy and osteopathic services within the Australian private health-care system: a report of recent trends. Chiropractic & Manual Therapies. 2014;22(1):3. doi: 10.1186/2045-709X-22-3. PubMed PMID: doi:10.1186/2045-709X-22-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back painback pain treatment trendsback pain treatment trends. JAMA Internal Medicine. 2013;173(17):1573–81. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Holliday S, Magin P, Dunbabin J, Oldmeadow C, Henry J-M, Lintzeris N, et al. An evaluation of the prescription of opioids for chronic nonmalignant pain by Australian general practitioners. Pain Medicine. 2013;14(1):62–74. doi: 10.1111/j.1526-4637.2012.01527.x. [DOI] [PubMed] [Google Scholar]
- 57.Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12(4):E35–70. [PubMed] [Google Scholar]
- 58.Williams C, Maher C, Hancock M, et al. Low back pain and best practice care: A survey of general practice physicians. Arch Intern Med. 2010;170:271–7. doi: 10.1001/archinternmed.2009.507. [DOI] [PubMed] [Google Scholar]
- 59.Buchbinder R, Staples M, Jolley D. Doctors with a special interest in back pain have poorer knowledge about how to treat back pain. Spine. 2009;34(11):1218–26. doi: 10.097/BRS.0b013e318195d688. [DOI] [PubMed] [Google Scholar]
- 60.Rashidian A, Eccles M, Russell I. Falling on stony ground? A qualitative study of implementation of clinical guidelines’ prescribing recommendations in primary care. Health Policy. 2008;85:148–61. doi: 10.1016/j.healthpol.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 61.Overmeer T, Linton SJ, Holmquist L, Eriksson M, Engfeldt P. Do evidence-based guidelines have an impact in primary care? A cross-sectional study of Swedish physicians and physiotherapists. Spine. 2005;30:146–51. doi: 10.1097/00007632-200501010-00024. [DOI] [PubMed] [Google Scholar]
- 62. Australian Physiotherapy Association Website 2011. Available from: http://www.physiotherapy.asn.au/careers/overview.
- 63.Li LC, Bombardier C. Physical therapy management of low back pain: An exploratory survey of therapist approaches. Physical Therapy. 2001 Apr;81(4):1018–28. 2001. [PubMed] [Google Scholar]
- 64.Linton S, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002;12:223–32. doi: 10.1023/a:1020218422974. [DOI] [PubMed] [Google Scholar]
- 65.Scudds RJ, Scudds RA, Baxter GD, McDonough SM, Walsh DM. Transcutaneous electrical nerve stimulation for the treatment of pain in physiotherapy practices in Hong Kong and the United Kingdom—A survey of usage and perceived effectiveness compared with other pain relieving modalities. Hong Kong Physiotherapy J. 2009;27(1):11–20. [Google Scholar]
- 66.Hurwitz EL, Morgenstern H, Harber P, Kominsky GF, Belin TR, Yu F, et al. The effectiveness of physical modalities among patients with low back pain randomized to chiropractic care: Findings from the UCLA Low Back Pain Study. J Manip Physiol Thera. 2002;25(1):10–20. doi: 10.1067/mmt.2002.120421. [DOI] [PubMed] [Google Scholar]
- 67.van Tulder M, Koes B, Malmivaara A. Outcome of noninvasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006;15(Suppl 1):S64–81. doi: 10.1007/s00586-005-1048-6. PubMed PMID: doi:10.1007/s00586-005-1048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seco J, Kovacs FM, Urrutia G. The efficacy, safety, effectiveness, and cost-effectiveness of ultrasound and shock wave therapies for low back pain: a systematic review. The Spine Journal. 2011;11(10):966–77. doi: 10.1016/j.spinee.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 69.Balagué F, Dudler J. An overview of conservative treatment for lower back pain. International J Clin Rheum. 2011;6(3):281–90. [Google Scholar]
- 70.Daykin A, Richardson B. Physiotherapists’ pain beliefs and their influence on the management of patients with chronic low back pain. Spine. 2004;29(7):783–95. doi: 10.1097/01.brs.0000115135.19082.97. [DOI] [PubMed] [Google Scholar]
- 71.Stevenson K, Lewis M, Hay E. Do physiotherapists’ attitudes towards evidence-based practice change as a result of an evidence-based educational programme? J Evaluation In Clinical Practice. 2004;10(2):207–17. doi: 10.1111/j.1365-2753.2003.00479.x. Date Revised: 20060918. Date Created: 20040610. Date Completed: 20041007. Update Code: 20101124. Publication Type: Clinical Trial. [DOI] [PubMed] [Google Scholar]
- 72.Tetrault M. Chiropractic Diplomatic Corps. 2011. Available from: http://www.chiropracticdiplomatic.com/country/
- 73.Hoskins W, Pollard H, Reggars J, Vitiello A, Bonello R. Journal publications by Australian chiropractic academics: are they enough? Chiropractic & Osteopathy. 2006;14(1):13. doi: 10.1186/1746-1340-14-13. PubMed PMID: doi:10.1186/1746-1340-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Australian Bureau of Statistics National Health Survey: Summary of Results 2004–05. 2006 Feb; [Google Scholar]
- 75.ABS . Chiropractic and Osteopathic Services in Australia. Canberra: Australian Bureau of Statistics; 1998. [Google Scholar]
- 76.Charity M, French S, Forsdike K, Britt H, Polus B, Gunn J. Extending ICPC-2 PLUS terminology to develop a classification system specific for the study of chiropractic encounters. Chiropractic & Manual Therapies. 2013;21(1):4. doi: 10.1186/2045-709X-21-4. PubMed PMID: doi:10.1186/2045-709X-21-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lutzer K. Moving from Anecdote to Evidence. J Can Chiropr Assoc. 2006;50(4):235–7. [PMC free article] [PubMed] [Google Scholar]
- 78.DeVocht JW. History and overview of theories and methods of chiropractic: A counterpoint. Clinical Orthopaedics and Related Research. 2006;444:243–9. doi: 10.1097/01.blo.0000203460.89887.8d. [DOI] [PubMed] [Google Scholar]
- 79.Breen A, van Tulder M, Koes B, Jensen I, Reardon R, Bronfort G. Mono-disciplinary or multidisciplinary back pain guidelines? How can we achieve a common message in primary care? Eur Spine J. 2006;15(5):641–7. doi: 10.1007/s00586-005-0883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.The Free Medical Dictionary. Definition of Chiropractic 2011. Available from: http://medical-dictionary.thefreedictionary.com/chiropractic.
- 81.Wenban AB. Is chiropractic evidence based? A pilot study. J Manip Physiol Ther. 2003;26(1):47. doi: 10.1067/mmt.2003.2. [DOI] [PubMed] [Google Scholar]
- 82.Imrie R, Ramey DW. The evidence for evidence-based medicine. Complementary Therapies in Medicine. 2000;8(2):123–6. doi: 10.1054/ctim.2000.0370. [DOI] [PubMed] [Google Scholar]
- 83.Klingman D, Localio A, Sugarman J, et al. Measuring defensive medicine using clinical scenario surveys. J Health Politics, Policy and Law. 1996;21:185–217. doi: 10.1215/03616878-21-2-185. [DOI] [PubMed] [Google Scholar]
- 84.Tomlin Z, Humphrey C, Rogers S. General practitioners’ perceptions of effective health care. BMJ. 1999;318:1532–5. doi: 10.1136/bmj.318.7197.1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Åkesson K, Dreinhöfer K, II, Woolf A. Improved education in musculoskeletal conditions is necessary for all doctors. Bulletin of the World Health Organization. 2003 Sep;81:677–83. 2003. [PMC free article] [PubMed] [Google Scholar]
- 86.Freedman KB, Bernstein J. The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am. 1998;80(10):1421–7. doi: 10.2106/00004623-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 87.Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84-A:604–8. doi: 10.2106/00004623-200204000-00015. [DOI] [PubMed] [Google Scholar]
- 88.Childs J, Whitman J, Sizer P, Pugia M, Flynn T, Delitto A. A description of physical therapists’ knowledge in managing musculoskeletal conditions. BMC Musculoskeletal Disorders. 2005;6(1):32. doi: 10.1186/1471-2474-6-32. PubMed PMID: doi:10.1186/1471-2474-6–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Humphreys BK, Sulkowski A, McIntyre K, Kasiban M, Patrick AN. An examination of musculoskeletal cognitive competency in chiropractic interns. J Manip Physiol Ther. 2007;30(1):44–9. doi: 10.1016/j.jmpt.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 90.Carey T, Freburger J, Holmes G, Castel L, Darter J, Agans R, et al. A long way to go: Practice patterns and evidence in chronic low back pain care. Spine. 2009;34(7):718–24. doi: 10.1097/BRS.0b013e31819792b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Downie A, Williams CM, Henschke N, Hancock MJ, Ostelo RW, de Vet HC, et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ: British Medical Journal . :347. doi: 10.1136/bmj.f7095. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Waddell G. The back pain revolution. Churchill Livingstone; 2004. [Google Scholar]
- 93.Underwood M. Diagnosing acute nonspecific low back pain: Time to lower the red flags? Arthritis & Rheumatism. 2009;60(10):2855. doi: 10.1002/art.24858. [DOI] [PubMed] [Google Scholar]
- 94.Koes B, van Tulder M, Ostelo R, Burton A, Waddell G. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine. 2001;26:2504–13. doi: 10.1097/00007632-200111150-00022. PubMed PMID: doi:10.1097/00007632-200111150-00022. [DOI] [PubMed] [Google Scholar]
- 95.Amorin-Woods L, Parkin-Smith G. Clinical decision-making to facilitate appropriate patient management in chiropractic practice: ‘the 3-questions model’. Chiropr Man Therap. 2012;20(1):6. doi: 10.1186/2045-709X-20-6. PubMed PMID: doi:10.1186/2045-709X-20-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sciubba D, Gokaslan Z. Diagnosis and management of metastatic spine disease. Surgical Oncology. 2006;15:141–51. doi: 10.1016/j.suronc.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 97.Loblaw D, Perry J, Chambers A, Laperriere N. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative’s Neuro-Oncology Disease Site Group. J Clinical Oncology : official Journal of the American Society of Clinical Oncology. 2005;23:2028–37. doi: 10.1200/JCO.2005.00.067. [DOI] [PubMed] [Google Scholar]
- 98.Ferguson F, Holdsworth L, Rafferty D. Low back pain and physiotherapy use of red flags: the evidence from Scotland. Physiotherapy. 2010;96:282–8. doi: 10.1016/j.physio.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 99.Urquhart D, Hoving J, Assendelft W, et al. Antidepressants for non-specific low back pain. Cochrane Database Syst Rev . 2008:CD001703. doi: 10.1002/14651858.CD001703.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Salerno S, Browning R, Jackson J. The effect of antidepressant treatment on chronic back pain: a meta-analysis. Arch Intern Med. 2002;162:19–24. doi: 10.1001/archinte.162.1.19. [DOI] [PubMed] [Google Scholar]
- 101.Staiger T, Gaster B, Sullivan M, Deyo R. Systematic review of antidepressants in the treatment of chronic low back pain. Spine (Phila Pa 1976) 2003;28:2540–5. doi: 10.1097/01.BRS.0000092372.73527.BA. [DOI] [PubMed] [Google Scholar]
- 102.Schnitzer T, Ferraro A, Hunsche E, Kong S. A comprehensive review of clinical trials on the efficacy and safety of drugs for the treatment of low back pain. J Pain and Symptom Management. 2004;28:72–95. doi: 10.1016/j.jpainsymman.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 103.Peckham C. The Physician: Healthy, Wealthy, and Wise? Jan 23, 2014. Available from: http://www.medscape.com/viewarticle/819212_1.
- 104.Greene B, Smith M, Allareddy V, Haas M. Referral patterns and attitudes of primary care physicians towards chiropractors. BMC Complementary and Alternative Medicine. 2006;6:5. doi: 10.1186/1472-6882-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.White A, Resch K, Ernst E. Complementary medicine: use and attitudes among GPs. Family Practice. 1997;14:302–6. doi: 10.1093/fampra/14.4.302. [DOI] [PubMed] [Google Scholar]
- 106.Berman B, Singh B, Lao L, et al. Physicians’ attitudes toward complementary or alternative medicine: a regional survey. The Journal of the American Board of Family Practice / American Board of Family Practice. 1995;8:361–6. [PubMed] [Google Scholar]
- 107.Blumberg D, Grant W, Hendricks S, et al. The physician and unconventional medicine. Alternative Therapies in Health and Medicine. 1995;1:31–5. [PubMed] [Google Scholar]
- 108.Studdert D, Eisenberg D, Miller F, et al. Medical malpractice implications of alternative medicine. JAMA: the Journal of the American Medical Association. 1998;280:1610–5. doi: 10.1001/jama.280.18.1610. [DOI] [PubMed] [Google Scholar]
- 109.Nelson C, Lawrence D, Triano J, Bronfort G, Perle S, Metz RD, et al. Chiropractic as spine care: a model for the profession. Chiropractic & Osteopathy. 2005;13(1):9. doi: 10.1186/1746-1340-13-9. PubMed PMID: doi:10.1186/1746-1340-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Breen A, Austin H, Campion-Smith C, et al. “You feel so hopeless”: a qualitative study of GP management of acute back pain. Eur J Pain. 2007;11:21–9. doi: 10.1016/j.ejpain.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 111.Lin C, Haas M, Maher C, et al. Cost-effectiveness of general practice care for low back pain: a systematic review. Eur Spine J. 2011;20:1012–23. doi: 10.1007/s00586-010-1675-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Evidence-Based Care That Includes Chiropractic Manipulation More Effective Than Usual Medical Care. The Back Letter. 2008;23(1):3. doi: 10.1097/01.BACK.0000310518.20803.b3. [DOI] [Google Scholar]
- 113.Dagenais S, Gay RE, Tricco AC, Freeman MD, Mayer JM. NASS Contemporary concepts in spine care: Spinal manipulation therapy for acute low back pain. The Spine Journal. 2010;10(10):918–40. doi: 10.1016/j.spinee.2010.07.389. 10// [DOI] [PubMed] [Google Scholar]
- 114.McGregor M, Puhl A, Reinhart C, Injeyan H, Soave D. Differentiating intraprofessional attitudes toward paradigms in health care delivery among chiropractic factions: results from a randomly sampled survey. BMC Complementary and Alternative Medicine. 2014;14(1):51. doi: 10.1186/1472-6882-14-51. PubMed PMID: doi:10.1186/1472-6882-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Briggs AM, Slater H, Smith AJ, Parkin-Smith GF, Watkins K, Chua J. Low back pain-related beliefs and likely practice behaviours among final-year cross-discipline health students. European J Pain. 2012 doi: 10.1002/j.1532-2149.2012.00246.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 116.Back Pain Recognition Program: NCQA Available from: http://www.ncqa.org/Programs/Recognition/BackPainRecognitionProgramBPRP.aspx.
- 117.Davis MA, Martin BI, Coulter ID, Weeks WB. US Spending On Complementary And Alternative Medicine During 2002–08 Plateaued, Suggesting Role In Reformed Health System. Health Affairs. 2013 Jan 1;32(1):45–52. doi: 10.1377/hlthaff.2011.0321. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bishop PB, Wing PC. Compliance with clinical practice guidelines in family physicians managing worker’s compensation board patients with acute lower back pain. Spine J. 2003;3:442–50. doi: 10.1016/s1529-9430(03)00152-9. [DOI] [PubMed] [Google Scholar]
- 119.Bishop A, Foster N, Thomas E, Hay E. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135:187–95. doi: 10.1016/j.pain.2007.11.010. PubMed PMID: doi:10.1016/j.pain.2007.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Buchbinder R, Jolley D. Improvements in general practitioner beliefs and stated management of back pain persist 4.5 years after the cessation of a public health media campaign. Spine (Phila Pa 1976) 2007;32:E156–62. doi: 10.1097/01.brs.0000256885.00681.00. [DOI] [PubMed] [Google Scholar]
- 121.Coudeyre E, Rannou F, Tubach F, et al. General practitioners’ fear-avoidance beliefs influence their management of patients with low back pain. Pain. 2006;124(330–7) doi: 10.1016/j.pain.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 122.Harte A, Gracey J, Baxter G. Current use of lumbar traction in the management of low back pain: results of a survey of physiotherapists in the United Kingdom. Arch Phys Med Rehab. 2005;86:1164–9. doi: 10.1016/j.apmr.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 123.Li L, Bombardier C. Physical therapy management of low back pain: an exploratory survey of therapist approaches. Phys Ther. 1999;81:1018–28. [PubMed] [Google Scholar]
- 124.Linton S, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002;12:223–32. doi: 10.1023/a:1020218422974. PubMed PMID: doi:10.1023/A:1020218422974. [DOI] [PubMed] [Google Scholar]
- 125.Little P, Smith L, Cantrell T, et al. General practitioners’ management of acute back pain: a survey of reported practice compared with clinical guidelines. BMJ. 1996;312:485–8. doi: 10.1136/bmj.312.7029.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pollentier A, Langworthy J. The scope of chiropractic practice: A survey of chiropractors in the UK. Clinical Chiropractic. 2007;10:147–55. PubMed PMID: doi:10.1016/j.clch.2007.02.001. [Google Scholar]
- 127.Walker B, French S, Page M, O’Connor D, McKenzie J, Beringer K, et al. Management of people with acute low-back pain: a survey of Australian chiropractors. Chiropractic & Manual Therapies. 2011;19(1):29. doi: 10.1186/2045-709X-19-29. PubMed PMID: doi:10.1186/2045-709X-19-29. [DOI] [PMC free article] [PubMed] [Google Scholar]