Abstract
Clinicians routinely encounter patients suffering from both degenerative and acute spinal pain, often as a consequence of pathology affecting the intervertebral disc (IVD). The IVD is a complex structure essential to spinal function and is subject to degenerative disease and injury. However, due to the complexity of spinal pain syndromes it is often difficult to determine the extent of the IVD’s contribution to the genesis of spinal pain. The location of the IVD is within close proximity to vital neural elements and may in the event of pathological change or injury compromise those structures. It is therefore important that clinicians performing manual therapy understand the cellular and molecular biology of the IVD as well as its clinical manifestation of degeneration/injury in order to safely manage and appreciate the role played by the disc in the development of mechanical spinal pain syndromes.
Keywords: spine, degenerative, pain, disc, intervertebral
Abstract
Les cliniciens voient régulièrement des patients souffrant de douleurs vertébrales à la fois dégénératives et aiguës, souvent une conséquence d’une pathologie affectant le disque intervertébral (DIV). Le DIV est une structure complexe essentielle à la fonction rachidienne et peut être touché par des maladies dégénératives et des blessures. Toutefois, en raison de la complexité des syndromes de douleurs vertébrales, il est souvent difficile de déterminer la part de contribution du DIV à la genèse de cette douleur. L’emplacement du DIV est à proximité d’éléments neuronaux vitaux et peut, en cas de changement pathologique ou d’une blessure, compromettre ces structures. Il est donc important que les cliniciens administrant une thérapie manuelle comprennent la biologie cellulaire et moléculaire du DIV ainsi que la manifestation clinique de la dégénérescence et des blessures de celui-ci, afin de gérer en toute sécurité et d’apprécier le rôle joué par le disque dans le développement des syndromes de douleurs vertébrales mécaniques.
Keywords: colonne vertébrale, dégénératif, douleur, disque, intervertébral
Introduction:
The intervertebral disc (IVD) is a complex structure positioned between two adjacent vertebrae where in addition to protecting the spinal cord and segmental spinal nerves it confers flexibility, multi-axial spinal motion and load transmission to the spine. The IVD is vulnerable to injury and degeneration often leading to pain syndromes however much remains to be discovered concerning the development of axial and radicular pain syndromes, the biology of the disc and the capacity of the IVD to repair itself after injury.1 From the clinician’s perspective, familiarity with the biology of the IVD is vital in order to understand the natural history of disc-related injury/illness and to develop appropriate therapeutic strategies. The purpose of this review is to provide an overview of the salient characteristics of IVD pathology with a particular emphasis upon degenerative disease and its role in the generation of clinical spinal pain syndromes.
The disc as an organ:
Capping the IVD superiorly and inferiorly, the cartilaginous vertebral end plates (VEP) are thinnest in the central region contiguous with the NP and may be up to 1mm thick at their outer edge. Much like hyaline cartilage found within appendicular joints, VEPs are typically without vasculature or neural elements and although a minute arrangement of vessels exists at early stages, these will fade as skeletal maturity is reached and undergo calcification and significant loss of function with degenerative disease.2,3,4 Although the VEPs are without direct vascular supply, there are capillary networks abutting the central portion of the VEP that are directly connected with the vasculature of the vertebral body. Interestingly the capillary density is 4 times denser at the centre of the VEP (over the nucleus pulposus or ‘NP’) than the periphery; suggesting the importance of diffusion from these networks into and out of the NP.5
Encircling the NP and located between the superior and inferior VEPs, the annulus fibrosus (AF) confers ligament-like restraint properties to the IVD and thereby essential biomechanical support to the disc when subjected to loading.6 The AF adheres strongly to the periphery of the vertebral body in a symphysis type of attachment where many small diameter sensory nerve fibers surround the AF, normally penetrating only the outer few millimeters of the lamellae.7,8 These small diameter sensory fibers contribute to mechanotransduction properties and in the case of injury, also nocicieption.7,8 In addition to peripheral innervation, the AF also receives a meager vascular supply from the encircling veins and capillary networks.8 Although far removed from the outer AF fibers, the NP is in intimate proximity with the inner AF, forming the “transition zone”. In youth the “transition zone” boundary between the AF and NP is well defined, but with degenerative change and aging this distinction becomes blurred and loses its clear anatomical border.
It is important to consider that the IVD NP is an avascular, immune privileged and unique niche unlike any other tissue compartment in the body with unique cellular properties. The specific types of cells within the NP continue to be incompletely characterized resulting in the use of non-specific terms such as “NP cells” to define them. At present at least 3 different NP cell types: “chondrocyte-like” cells (NP), notochordal cells (NCs) and NP stem/ progenitor cells (NPPCs), have been identified within the NP.9,10 NP cells have evolved to tolerate the otherwise hostile conditions present within the NP where they extra-cellular matrix (ECM) that is a product of their synthesis. The ECM within the NP contains abundant collagen type II and to a lesser extent collagen I plus a rich amount of proteoglycans, specifically aggrecan. In particular the presence of aggrecan confers tremendous water-binding capacity to the NP with vital ECM-maintenance conferred by a number of other smaller single leucine-rich proteoglycans or “SLRPs”.11
Development and Cellular Configuration:
Development of the IVD involves both the embyronic mesenchyme and the NCs. During embryogenesis the NP consists predominantly of NC cells; a configuration that markedly changes with growth and development such that NCs are replaced by chondrocyte-like ‘NP cells’ by late adolescence.8 In some animal species such as nonchondrodystrophic dogs (mongrels), rats, rabbits and mice, NCs remain present in aging IVDs. An emerging hypothesis is that animals that retain NCs appear to be protected from the development of DDD due at least in part due to soluble factors secreted by NCs that contribute to IVD homeostasis.12–16 It has been reported that progenitor/stem cells are present in a number of human and non-human NPs and it is likely that these stem/progenitor cells migrate to the NP during development.17 One of the authors of this paper (WME) recently reported that NPPCs have multipotent differential potential including in vivo neuro-differentiation.10 Even in degenerative human IVDs, progenitor cells exist and have been shown to undergo chrondrogenic, osteogenic and adipogenic differentiation.10,18 An important consideration concerning the presence of NPPCs within the NP is the capacity (or failure) of these stem/progenitor cells to assist with renewal of the NP, and the nature of their interaction with other cells within the NP.
Molecular biology of the IVD:
Nucleus Pulposus: In youth the NP is a highly hydrated gelatinous structure composed of between 1–3% cells, with the remainder made up of ECM and water.19 With age the configuration of the NP changes such that with increasing degeneration the NP is subjected to diminished water content, declining numbers of viable cells and a significant change in the expression of many ECM molecules.20–23
Annulus Fibrosus: The peripheral fibers of the AF are mainly comprised of collagen type I, however more centrally the NP strongly expresses collagen type II.24 Due to a gradual advancement of AF fibers on the NP and a change in NP cell collagen biosynthesis, the proportion of type II is eventually supplanted by type I.23 The importance of collagen type II to normal function of the IVD NP is due to the its complex structure and ability to interact with the high water content of the NP ECM in a manner analogous to hyaline cartilage.
Vertebral Endplates: Ongoing cellular turnover acts in concert with nutrient diffusion through the IVD and the VEP’s, whereby the balance between anabolic and catabolic activity is maintained and controlled by complex growth factor and cytokine interaction.26,27 The hypoxic (2–5% O2), avascular, low pH and decreased levels of glucose combine to comprise the metabolic ‘niche’ unique to the NP where the energy source required by resident cells is provided via anaerobic glycolysis and ATP.25,26 When a decrease in anabolic activity is superseded by an increase in catabolic activity, the net result is a deterioration of the ECM and progressive cell death.27 Such an alteration may be associated with a decrease in cross linked collagen, which coupled with macroscopic changes such as cracks and fibrillations within the disc, may ultimately lead to a reduction in the NP’s overall biomechanical sufficiency.28,29
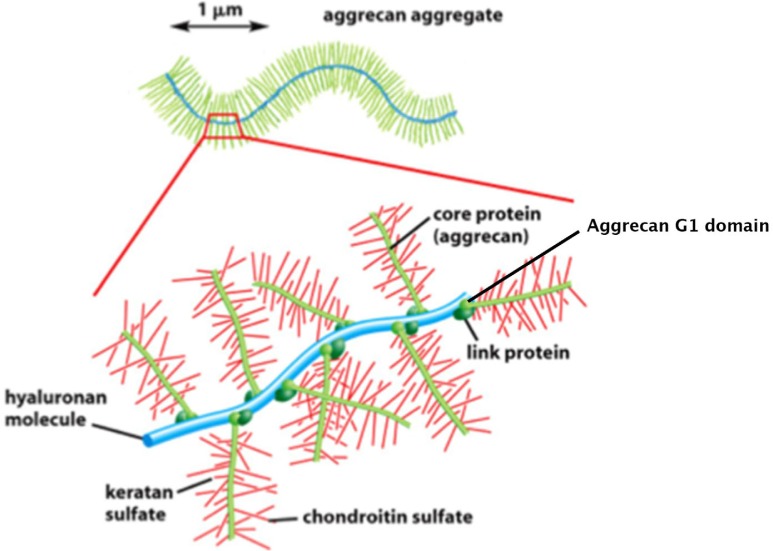
Extra-Cellular Matrix: When compressed under load, the primary purpose of the NP is to balance forces throughout the IVD structure, afford stability to the spine, and act as a conduit through which nutrient and wastes can diffuse into and out of the IVD.30,31 A family of molecules critical to the function of the IVD and the NP in particular, the proteoglycans (PGs) have evolved in order to provide such essential load-bearing characteristics. There are numerous species of PG, with the large aggregating species ‘aggrecan’ acting as the primary molecule responsible for the IVDs viscoelastic properties.
Proteoglycans: The glycosaminoglycan side chains (GAGs) are an essential component of the proteoglycan molecules and to the PG aggrecan in particular in that aggrecan substantially assists the IVD NP in load-bearing. The ability of the GAG side chains to strongly bind water molecules and thereby maintain a well-hydrated NP is due to the highly negative charges of the GAGs that in turn electrostatically bind polar water molecules. The GAGs are capable of functioning as water-binding molecules only when they are intact and bound to the PG core protein. The most abundant GAGs found within the disc (in particular with respect to aggrecan) are chondroitin sulfate (CS) and to a lesser degree, keratan sulfate (KS).32 In addition to their mechanical function PGs (notably the SLRPs) also have a play pivotal signal transduction roles since they are capable of binding and sequestering growth factors within the ECM.11 These biological/signaling properties assist with ECM maintenance in that the bio-availability of growth factors and other cytokines mediated by SLRPs are important for sustained cell survival (see review by Brown et al).11,33
The CD44 cell surface receptor secretes long chains of hyaluronic acid to which the GAG side chains are covalently attached via their G1 globular domains and stabilized by link proteins (Figure 1).34 As discussed above, GAGs and their rich sulfate residues attach to the aggrecan core protein, thereby conveying a high net negative charge to the molecule that electrostatically binds water. This charge contributes to the tremendous net swelling pressure of the IVD NP, resulting in its profound capacity to bear load.2,9,29,35,36 Since the cells of the fully developed disc rely on diffusion for their metabolic needs, a decrease in PGs (particularly aggrecan) can affect the flow of molecules in and out of the disc and in the case of SLRPs diminish the growth factor binding ability and contribute to ECM degradation. Therefore a depletion of aggrecan and fragmentation of SLRP core proteins such as through injury or degeneration can allow the migration of important ECM molecules out of the disc and a breakdown in vital cell-ECM communication.2,11,32 PGs and collagen molecules are degraded through the actions of a variety of proteases that serve to cleave the binding sites of PGs to hyaluronic acid or by degrading the collagen type II molecules.23,24,27 This loss of GAGS secondary to degeneration is of critical importance since when loaded, degenerated discs lose fluid more quickly due to a loss of GAGs, an overall reduction in net swelling pressure and therefore a loss of water, disc height and their ability to bear load. These cellular and molecular changes are often exhibited using sophisticated imaging such as MRI as a flattened or bulging discs.2,5,6,24,25,37,38,39,40
Figure 1:
Schematic of aggrecan aggregate. Arrow indicates large aggrecan aggregate with an enlarged area depicting aggrecan molecules consisting of a core protein, keratan and chondroitin sulfate GAGs linked via the G1 globular domain to the hyaluronic acid monomer. Modified from Fox AJS, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health: A Multidisciplinary Approach. 2012; 4: 340. DOI: 10.1177/1941738111429419
Pathobiology of IVD degeneration:
Aging and degenerative disc disease (DDD) are classifications of the disordered IVD that have been used interchangeably for many years however recently it has become increasingly accepted that they do not reflect the same biological events.1,24,31 DDD appears to include significant underlying patho-biological changes of the VEPs, such that the normal diffusion of essential molecules and gases are sufficiently altered contributing to cell death, degeneration of the IVD and endplates as well as subchondral bone (classified on MRI as modic changes).31 Conversely, normal aging does not result in a collapsed IVD with disorganized appearance, rather the associated changes are typified by darkening of the height of the NP on T2 MRI and degeneration of the IVD components but with good preservation of disc height.24,31
The degenerative process weakens the disc reducing its tolerance to load-bearing, which in turn increases aberrant forces along the end plate and through the encircling AF. Such impaired loadbearing results in remodeling of the disc/vertebral interface manifesting as zygapophyseal osteoarthrosis and ligament hypertrophy such as is typical with osteoarthritic changes of appendicular joints.2,7,41,42 Eventual fissuring and tears within the annulus may enable the ingrowth of nerves and blood vessels, both of which represent important biological occurrences since discs which may become pain generators must first exhibit structural disruption.24,43 At present apart from the use of provocative discography, such pathological changes are undetectable. Perhaps someday more sophisticated imaging will be able to detect such adaptations, potentially serving a diagnostic role in the identification of painful disc syndromes however at the present such changes are not clinically detectable.2,5,24,37,44,45,46
The disc as a source of pain:
The annular fissures and tears that develop in degenerative discs often exhibit granulation tissue that develops as part of the body’s attempt to heal.23,30,42 The presence of such tears and the resultant inflammatory tissue can lead to the attraction and ingrowth of nerves capable of expressing nociceptive information.24,43 This process involves the secretion of inflammatory pain-related mediators as well as an augmented expression of pain-related molecules such as nerve growth factor and its receptor (TrkA).20,30 This increased nociceptive capacity can lead to an amplified response or ‘peripheral sensitization’.20 This peripheral sensitization results in the activation of mechanically sensitive afferents mediated by the local secretion of inflammatory molecules which in the event of injury, may account for the disparity of painful degenerative discs as compared to degenerative discs that are not painful.47
In an elegant study involving the rabbit lumbar spine, Yamashita et al, reported that the annulus conveys both mechanosensitive as well as nociceptive input to the nervous system, suggesting the IVD is capable of mediating pain.48 They further indicated that the IVD annulus is likely sensitive to stronger more injurious stimuli as opposed to the lower thresholds of injury that may exist for muscle and facet joints.48 Given the pivotal role of the disc during weight bearing it makes biological sense that under normal conditions the tissues would have higher nociceptive activation thresholds that would not convey pain under normal loading conditions. These thresholds may well be lowered in the event of disease or injury and become pain sensitive under normal loadbearing; a common clinical observation of the back pain patient. A recent comprehensive review of the innervation of the lumbar IVD by Edgar hypothesized that the IVD could, unlike other joints have a unique visceral-type of nerve supply as opposed to the somatic innervation more typically exhibited by joints.47 Edgar also demonstrated that stimulation of the AF in the lower lumbar spine of rats resulted in a nociceptive afferent discharge to the L2 dorsal roots. These findings further support the increasing evidence that lumbar discogenic pain shares similarities with visceral pain. It follows that the innervation of the IVD annulus (and facet joints) serves to function as a proprioceptive network capable of activating paraspinal muscles for locomotion and stabilization of motion segments. When activated by injury/inflammation an up-regulation of muscle activation leads to the increased motor activity seen in most patients suffering from mechanical spinal pain (muscle spasm and local, segmental pain); this aberrant motor activity and the biomechanical/neuromuscular effects associated therewith may represent at least to some degree what is referred to in the manual therapy realm as a ‘subluxation’.21,22
Impact of cellular and molecular biology to the clinician:
Spinal pain reportedly affects up to 80% of the population with most people improving to varying degrees with or without treatment. However, although many patients “improve”, in the presence of significant injury/degeneration the disc should not be considered as fully healed. In fact, due to associated pathobiological changes many may not adequately recover and will continue to display recurrent and intermittent symptoms.2,22,41 Sources of spinal pain include the posterior zygapophyseal or facet joints, spinal and capsular ligaments, spinal musculature and other connective tissues. Although a number of approaches to treatment exist, there continues to be difficulty reaching a consensus regarding the most appropriate for spinal pain of mechanical nature.49,50 Chiropractors, physical therapists and other practitioners treat spinal pain primarily with mechanical approaches such as exercise, mobilization and manipulation of spinal joints and tissues. It is therefore imperative that clinicians be aware of the role these tissues play in the development of spinal pain as well as the ability of conservative therapies to affect these pain-related tissues. This review is based upon the important role played by the IVD in the genesis of mechanical spinal pain syndromes.50–53
Biochemical determinants of IVD-sourced pain:
Tissue samples taken from patients with low back pain have demonstrated the presence of associated degenerative disease in terms of increased expression of inflammatory cytokines and degradative enzymes.54 Furthermore, Burke et al., (2002) have demonstrated the expression of significantly higher levels of the inflammatory and pain-related cytokines interleukin-6 (IL-6) and interleukin-8 (IL-8) in surgical samples obtained from patients undergoing spinal fusion for discogenic pain, as compared to tissue from patients with sciatica.55 Also, in a recent study Shamji et al demonstrated increased amounts of IL-4, IL-6 and IL-12 present in surgical samples from patients with degenerative disc disease and disc herniation, versus non degenerate discs samples procured from autopsy. These findings strongly implicate the role played by inflammatory mediators in the biology of the internally disrupted disc and the likely development of disc related back pain secondary to such disruption.55,56
ECM Pathobiology:
The amount of collagen cross-linking within the IVD NP ECM increases with aging, as does non-enzymatic glycosylation that can result in impaired viscoelastic properties of the disc.23 Molecular degradation coupled with the variable depth and size of annular fissures and tears as well as progressive cell death render the disc more vulnerable to mechanical injury.2,23,37,41 As a consequence of this degradation the annulus forms one of three broad categories of tear: circumferential or delaminations due to the effects of shearing stress between the laminae of the AF; peripheral rim tears, frequently presenting in the anterior fibers of the AF; or radial fissures, which extend to the periphery of the AF in a posterior or posterolateral orientation.24 Despite a correlation between radial fissures and NP degeneration, the manner in which these events occur remains unknown and probably occurs within a continuum. In fact, most evidence suggests that disc prolapse is preceded by both radial fissures and tissue fragmentation, supporting the notion that prolapse is likely a late event in a cumulative, degenerative process as opposed to a purely traumatic occurrence.24,36,43,57
Due to cellular and molecular changes within the NP and degradation of the annulus the IVD becomes less hydrated and in fact loses its ability to bind water-in large part due to fragmentation of SLRPs, degraded aggrecan and progressive cell death. Therefore any therapy that could rejuvenate the IVD would be seen to as the “holy grail” of disc biological research and there are many laboratories worldwide actively seeking precisely this goal. Given the biology of IVD degeneration, it is difficult to imagine that any externally applied therapy could heal/regenerate or ‘rehydrate’ the IVD that does not provide cellular replacement, regeneration of the proteoglycan networks and/or the VEPs. However treatments have been proposed over the past years including “non-surgical spinal decompression’ that claim to re-hydrate the IVD by drawing water into the disc with claims to “heal from the inside out”. There is no doubt that traction helps some patients and this mode of therapy has been used since the time of Hippocrates for the treatment of spinal pain patients. However to date, there are no published studies detailing the cellular/molecular mechanisms whereby axial traction (with or without topically applied laser light, oxygen therapy or supplementation with chondroitin sulfate and other nutriceuticals) could re-hydrate the degenerative disc apart from poorly controlled case reports and testimonials. It is difficult to reconcile how an incompetent IVD NP with diminished water binding capacity could upon exposure to traction somehow heal from “the inside out”. It is left to the reader to reconcile the science of disc degeneration with such treatments that at this point must be considered to be at best unproven.
Spinal Manipulation and the IVD:
Bronfort et al., define spinal manipulative therapy (SMT), as “the application of high-velocity, low-amplitude manual thrusts to the spinal joints slightly beyond the passive range of joint motion” and spinal mobilization (MOB) as “the application of manual force to the spinal joints within the passive range of joint motion that does not involve a thrust.”58 During SMT and MOB, the effects of the externally applied force upon the spine have been shown to result in considerable load conveyed through the IVD.59
Most disc injuries occur spontaneously although a history of otherwise normal activity such as bending/lifting or coughing/sneezing prior to the onset of the patient’s symptoms is common.27 Suri et al confirmed that even though patients identified specific events with respect to the genesis of their lumbar disc herniation (LDH), the majority of LDH occurred without specific provocation.27,38 Furthermore, when the identification of possible inciting events was made they were more likely to be benign tasks of daily living rather than traumatic occurrences. In particular neither Suri et al, nor Brinckmann and Porter demonstrated that specific provocative events were significantly linked with severe clinical presentations.38,57 Structural and biochemical failure of the disc should therefore be considered to follow a continuum whereby degenerative changes predispose the structure to weaken such that further loading could result in incremental or acute failure. Depending upon the circumstances, a given patient presenting with a first episode of disc injury may have a good chance of recovery or yet another incident in a series of recurrent episodes. It must be considered likely that the disc is in some cases existing in a critically delicate condition and that only trivial trauma may be required to result in disc failure; otherwise simple activities of daily living such as bending could not result in the full-blown onset of acute symptoms. Under these circumstances it is inconsistent with biology to consider that manual therapy could “cause” an injury that is already underway.60 For example, the natural history of lumbar acute disc herniation often begins with acute back pain, followed by the development of radiculopathy hours, days, weeks or months later as the sequelae of the disc herniation proceed. In the more severe situation such as cauda equina, the symptoms follow a similar course depending upon the location and extent of the disc injury. Such progression may be deleteriously affected by activities of daily living such as lifting, bending, sitting and coughing therefore the possibility that the situation could be exacerbated by the application of external forces should not be discounted. Therefore the clinician ought to be vigilant for signs and symptoms suggestive of disc disorders given the commonplace occurrence of acute neck and or back pain and the potential ramifications of applied forces to the spine. The following clinical vignette represents an example of the IVD existing within such a delicate balance.
Clinical Vignette:
A 32 yr-old female presented with chief complaint of left neck, shoulder and arm pain and variable numbness extending to the thumb and forefinger of approximately one month duration. There was no history of recent trauma. The patient had been involved in a motor vehicle accident 11 years prior when the bicycle she was riding was struck head-on by an oncoming vehicle. At the time she was diagnosed with a closed-head injury, WAD II mechanical neck pain, fractured maxilla, two dislodged lower teeth and a chin laceration. Subsequently the patient’s neck pain was treated with non-operative methods including physical therapy/exercise, massage and activity modification. During the 12-year interval between the MVA until presentation, the patient suffered multiple exacerbations of neck and upper back pain that were primarily treated with physical therapies as above. Swimming offered relief as did occasional use of over the counter analgesics and anti-inflammatory medication. The patient complained of both legs ‘falling asleep’ easily after the accident as well as a rapid onset of bilateral numbness in the arms when they resting overhead on a pillow at night. Desk work also aggravated both the neck and arm pain.
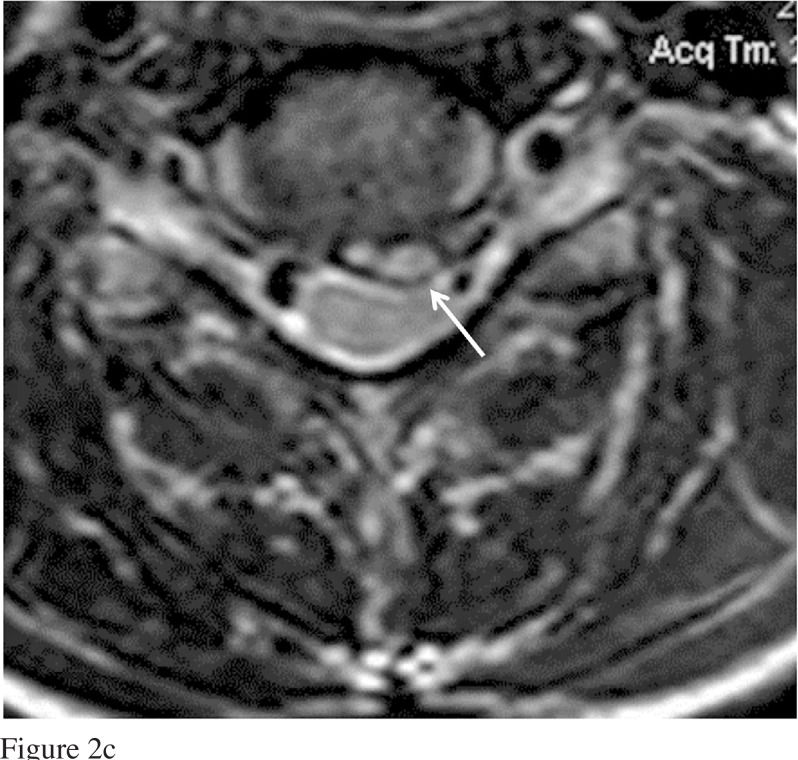
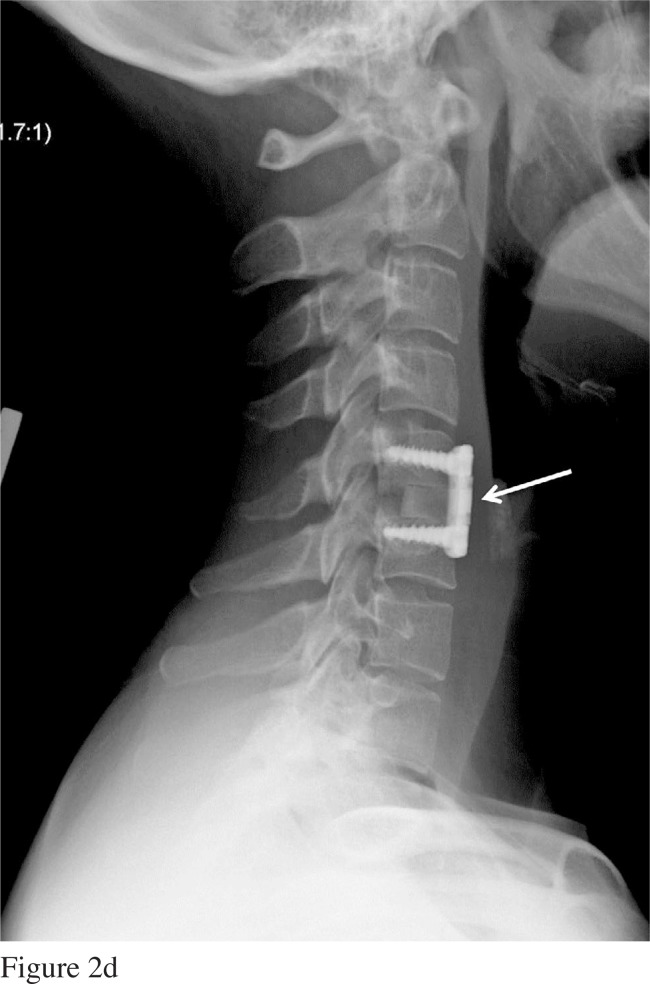
Physical examination revealed a moderate loss of left lateral bending of the cervical spine that caused an increase in left upper back, shoulder and arm pain (positive Spurling sign) and cradling the affected arm across the chest was relieving. Biceps and brachioradialis reflexes were diminished and there was a moderate reduction in wrist extension and triceps power graded as 4+ on the left. Furthermore, a mild, intermittently positive Hoffman sign affected the left hand that was not present on the right. There was a disturbance of tandem gait with the patient experiencing a modest but reproducible loss of balance. The plantar reflex was flexor with no clonus affecting either lower limb and there was no atrophy affecting ether of upper or lower extremities. A recent MRI examination revealed a large C5–6 posterior/left disc herniation significantly impinging on the spinal cord (Figure 2 a–c).
Figure 2:
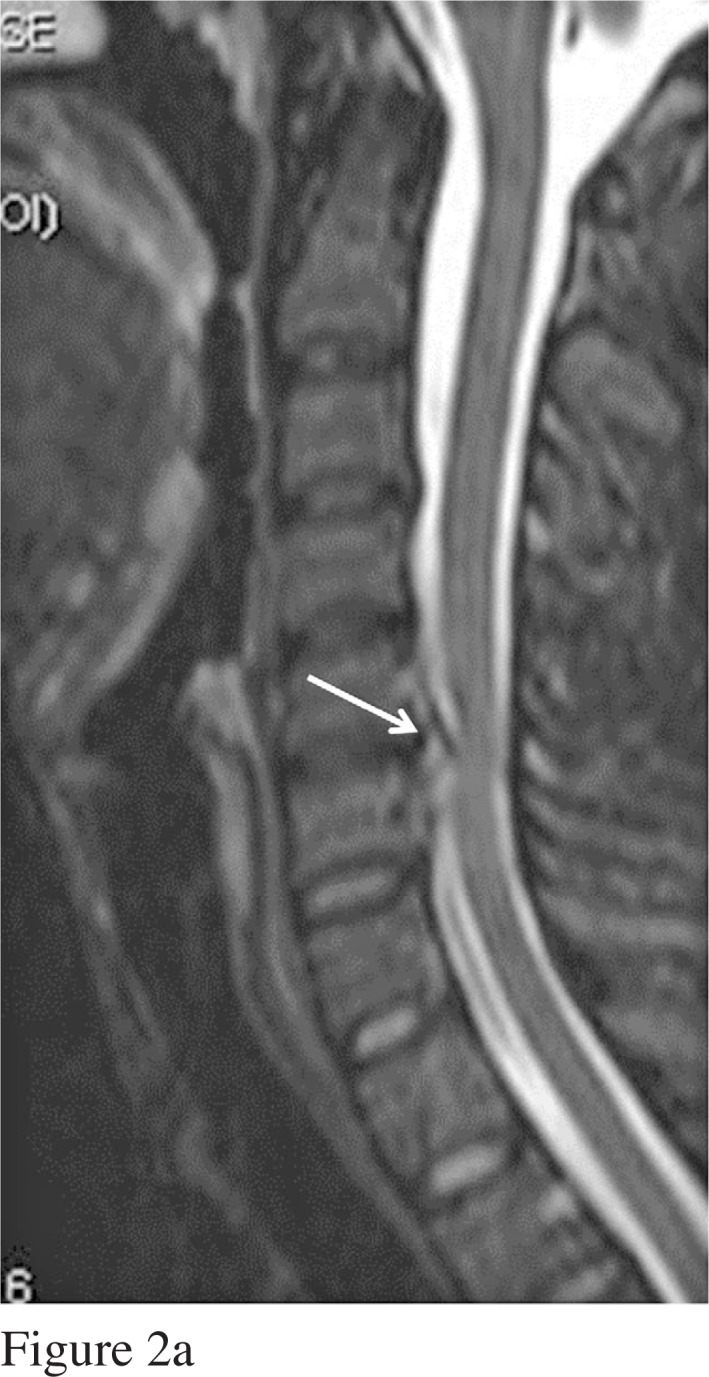

(a) T2-weighted sagittal MRI scan of patient’s cervical spine (2011) demonstrating significant right paracentral herniated nucleus pulposus of the C5–6 intervertebral disc (white arrows in all figures). (b) Sagittal T1 MRI of cervical spine depicting large C5–6 disc herniation and elevation of posterior longitudinal ligament, (c) Axial image of the same C5–6 disc as in (b), (d) Plain film radiographs of patient’s cervical spine post C5–6 anterior cervical decompression and fusion. Note interbody bone graft and plate affixed to the anterior aspect of the cervical spine (white arrow).
The patient was fitted with a rigid collar and monitored weekly for three weeks. Over the following three-week period the patient exhibited mild difficulty with balance and coordination, especially demonstrated when walking around corners and desks. Within the initial, few weeks after presentation and after repeated questioning regarding signs of long tract pathology, the patient related intermittent episodes when areas of the buttocks felt wet after sitting-even though none was palpable. Although subtle, signs of neural compromise were sufficient to warrant neurosurgical consultation ultimately resulting in an anterior cervical decompression and fusion of the C5–6 interspace (Figure 2d). Post operatively the patient recovered exceptionally well and following a course of strengthening and range of motion exercises, made a full recovery.
It is likely this patient actually suffered a spinal cord injury at the time of MVA including injury to the C5–6 IVD. It is also probable that injury to the spinal cord was responsible for many of the neurological symptoms of which the patient complained since these neurological symptoms have largely resolved following surgery. Important lessons learned from this case include the spontaneous development of symptoms of disc herniation, the onset of ‘hard’ neurological signs (demonstrative of spinal cord compression), and the likelihood that the large C5–6 cervical disc herniation occurred at some point many years after the MVA; without any further trauma and in the absence of any particular event. A previous cervical spine MRI performed in 2006 revealed mild bulging and loss of hydration of the C4–5 and C5–6 IVD as revealed by the T2-weighted MRI (Figure 3). Therefore, the development of the acute disc herniation in the absence of any further trauma occurred gradually, probably over many years and then manifested spontaneously. In this situation, an innocuous event such as a slip on the sidewalk or violent sneeze could have led to a worsening of the symptoms. Clearly in this case pathological changes affecting the disc were well underway and neurological compromise (although subtle), had already declared itself by the time of presentation. Providers of rehabilitation therapy need to bear extremely close attention to patients exhibiting signs and symptoms similar to those in this clinical vignette in order to obtain the best possible clinical outcome for their patients.
Figure 3:
T2-weighted sagittal MRI scan of patient’s cervical spine (2006) revealing minor bulging of the C5–6 intervertebral disc.
Conclusion:
By adulthood, the IVD is a largely fibrocartilaginous structure that permits limited motion while offering resistance against compressive loading. With degenerative change, there is a disruption in homeostatic regulation of the degenerative/damaged IVD leading to increased levels of catabolic and pain-causing cytokines in addition to granular or scar tissue formation rendering it vulnerable to further injury. With respect to non-operative treatment of spinal pain, numerous studies support the use of SMT and MOB; however, this remains controversial and lumbar disc herniation (LDH) remains the number one malpractice claim made against chiropractors 61. Another non-operative treatment for DDD is non-surgical spinal decompression however; there is no mechanistic, biological evidence to support the notion that this form of treatment can re-hydrate a degenerative disc. Therefore, prior to selecting a form of treatment, the clinician should be aware of the biological model of IVD and apply an evidence-based, judicious approach to the management of patients afflicted with these disorders.
Footnotes
All authors declare no conflicts of interest and have no disclosures. There is no particular grant funding to cite for this manuscript.
References:
- 1.Rajasekaran S, Naresh Babu J, Arun R, et al. A study of diffusion in human lumbar discs: A serial magnetic resonance imaging stud documenting the influence of the endplate on diffusion in normal and degenerate discs. Spine. 2004;29(23):2654–2667. doi: 10.1097/01.brs.0000148014.15210.64. [DOI] [PubMed] [Google Scholar]
- 2.Urban J, Roberts S. Degeneration of the intervertebral disc. Arthritis Res Ther. 2003;5(3):120–130. doi: 10.1186/ar629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore RJ. The vertebral endplate: disc degeneration, disc regeneration. Eur Spine J. 2006;15(3S):S333–S337. doi: 10.1007/s00586-006-0170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore RJ. The vertebral endplate: what do we know? Eur Spine J. 2000;9:92–96. doi: 10.1007/s005860050217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez AG, Slichter CK, Acosta FL, Rodriguez-Soto AE, Burghardt AJ, Majumdar S, Lotz JC. Human disc nucleus properties and vertebral endplate permeability. Spine (Phila Pa 1976) 2011;36(7):512–520. doi: 10.1097/BRS.0b013e3181f72b94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Del Grande F, Maus TP. Imaging the intervertebral disk: Age-related changes, herniations and radicular pain. Radiol Clin North Am. 2012;50:629–649. doi: 10.1016/j.rcl.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Freemont AJ, Peacock TE, Goupille P, Hoyland JA, O’Brien J, Jayson MI. Nerve ingrowth into diseased intervertebral disc in chronic back pain. Lancet. 1997 Jul 19;350:178–181. doi: 10.1016/s0140-6736(97)02135-1. [DOI] [PubMed] [Google Scholar]
- 8.Ghosh P, Brown S. The biology of the intervertebral disc. Vol. 1. Boca Raton, Fl: CRC Press; 1988. [Google Scholar]
- 9.Erwin WM. The enigma that is the nucleus pulposus cell: the search goes on. Arthritis Res Ther. 2010;12(3):118. doi: 10.1186/ar3001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erwin WM, Islam D, Eftekarpour E, Inman RD, Karim MZ, Fehlings MG. Intervertebral disc-derived stem cells: implications for regenerative medicine and neural repair. Spine (Phila Pa 1976) 2013;38(3):211–216. doi: 10.1097/BRS.0b013e318266a80d. [DOI] [PubMed] [Google Scholar]
- 11.Brown S, Melrose J, Caterson B, Roughley P, Eisenstein S, Roberts S. A comparative evaluation of the small leucine-rich proteoglycans of pathological human intervertebral discs. Eur Spine J. 2012;21(Suppl 2):154–159. doi: 10.1007/s00586-012-2179-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.An HS, Masuda K. Relevance of in vitro and in vivo models for intervertebral disc degeneration. J Bone Joint Surg Am. 2006;88(Suppl 2):88–94. doi: 10.2106/JBJS.E.01272. [DOI] [PubMed] [Google Scholar]
- 13.Erwin WM, Inman RD. Notochord cells regulate intervertebral disc chondrocyte proteoglycan production and cell proliferation. Spine (Phila Pa 1976) 2006;31(10):1094–1099. doi: 10.1097/01.brs.0000216593.97157.dd. [DOI] [PubMed] [Google Scholar]
- 14.Erwin WM, Ashman K, O’Donnel P, Inman RD. Nucleus pulposus notochord cells secrete connective tissue growth factor and up-regulate proteoglycan expression by intervertebral disc chondrocytes. Arthritis Rheum. 2006;54(12):3859–3867. doi: 10.1002/art.22258. [DOI] [PubMed] [Google Scholar]
- 15.Erwin WM, Las Heras F, Islam D, Fehlings MG, Inman RD. The regenerative capacity of the notochordal cell: tissue constructs generated in vitro under hypoxic conditions. J Neurosurg Spine. 2009;10(6):513–521. doi: 10.3171/2009.2.SPINE08578. [DOI] [PubMed] [Google Scholar]
- 16.Erwin WM, Islam D, Inman RD, Fehlings MG, Tsui FW. Notochordal cells protect nucleus pulposus cells from degradation and apoptosis: implications for the mechanisms of intervertebral disc degeneration. Arthritis Res Ther. 2011;13(6):R215. doi: 10.1186/ar3548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan SC, Gantenbein-Ritter B. Intervertebral disc regeneration or repair with biomaterials and stem cell therapy – feasible or fiction? Swiss Med Wkly. 2012;142:w13598. doi: 10.4414/smw.2012.13598. [DOI] [PubMed] [Google Scholar]
- 18.Risbud MV, Guttapalli A, Tsai TT, Lee JY, Danielson KG, Vaccaro AR, Albert TJ, Gazit Z, Gazit D, Shapiro IM. Evidence for skeletal progenitor cells in the degenerate human intervertebral disc. Spine (Phila Pa 1976) 2007;32(23):2537–44. doi: 10.1097/BRS.0b013e318158dea6. [DOI] [PubMed] [Google Scholar]
- 19.Lotz JC, Ulrich JA. Innervation, inflammation, and hypermobility may characterize pathologic disc degeneration: review of animal model data. J Bone Joint Surg Am. 2006;88(Supl 2):76–82. doi: 10.2106/JBJS.E.01448. [DOI] [PubMed] [Google Scholar]
- 20.Indahl A, Kaigle AM, Reikeras O, Holm SH. Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine (Phila Pa 1976) 1997;22(24):2834–40. doi: 10.1097/00007632-199712150-00006. [DOI] [PubMed] [Google Scholar]
- 21.Indahl A, Kaigle AM, Reikeras O, Holm SH. Electromyographic response of the porcine multifidus musculature after nerve stimulation. Spine (Phila Pa 1976) 1995;20(24):2652–2658. doi: 10.1097/00007632-199512150-00006. [DOI] [PubMed] [Google Scholar]
- 22.Stefanakis M, Key S, Adams MA. Healing of painful intervertebral discs: implications for physiotherapy. Part 1 – the basic science of intervertebral discs healing. Physical Therapy Reviews. 2012;17(4):234–240. [Google Scholar]
- 23.Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine (Phila Pa 1976) 2006;31(18):2151–2161. doi: 10.1097/01.brs.0000231761.73859.2c. [DOI] [PubMed] [Google Scholar]
- 24.Roughley PJ. Biology of intervertebral disc aging and degeneration: involvement of the extracellular matrix. Spine (Phila Pa 1976) 2004;29(23):2691–2699. doi: 10.1097/01.brs.0000146101.53784.b1. [DOI] [PubMed] [Google Scholar]
- 25.Urban JP, Smith S, Fairbank JC. Nutrition of the intervertebral disc. Spine (Phila Pa 1976) 2004;29(23):2700–2709. doi: 10.1097/01.brs.0000146499.97948.52. [DOI] [PubMed] [Google Scholar]
- 26.Urban JP. The role of the physiochemical environment in determining disc cell behaviour. Biochem Soc Trans. 2002;30(pt6):858–64. doi: 10.1042/bst0300858. [DOI] [PubMed] [Google Scholar]
- 27.Yoon ST, Patel NM. Molecular therapy of the intervertebral disc. Eur Spine J. 2006;3(Suppl):S379–388. doi: 10.1007/s00586-006-0155-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bibby SR, Jones D, Lee RB, Yu J, Uran JP. The Pathophysiology of the intervertebral disc. Joint Bone Spine. 2001;68(6):537–542. doi: 10.1016/s1297-319x(01)00332-3. [DOI] [PubMed] [Google Scholar]
- 29.Keppler CK, Ponnappan RK, Tannoury CA, Risbud MV, Anderson DG. The molecular basis of intervertebral disc degeneration. The Spine Journal. 2013;13(3):318–330. doi: 10.1016/j.spinee.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Pattapa G, Li Z, Peroglio M, Wismer N, Alini M, Grad S. Diversity of intervertebral disc cells: phenotype and function. J Anat. 2012;221(6):480–496. doi: 10.1111/j.1469-7580.2012.01521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rajasekaran S, Venkatadass K, Naresh Babu J, Ganesh K, Shetty AP. Pharmacological enhancement of disc diffusion and differentiation of healthy, ageing and degenerated discs. Eur Spine J. 2008;17(5):626–643. doi: 10.1007/s00586-008-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singh K, Masuda K, Thonar EJ, An HS, Cs-Szabo G. Age-related changes in the extracellular matrix of nucleus pulposus and annulus fibrosus of human intervertebral disc. Spine Phila Pa 1976. 2009;34(1):10–16. doi: 10.1097/BRS.0b013e31818e5ddd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilchrist CL, Darling EM, Chen J, Setton LA. Extracellular matrix ligand and stiffness modulate immature nucleus pulposus cell – cell interactions. PLoS ONE. 2011;6(11):1–9. doi: 10.1371/journal.pone.0027170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang BL, Yang BB, Erwin M, Ang LC, Finkelstein J, Yee A. Versican G3 domain enhances cellular adhesion and proliferation of bovine intervertebral disc cells cultured in vitro. Life Sciences. 2003;73(26):3399–3413. doi: 10.1016/j.lfs.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 35.Schnake KJ, Putzier M, Haas NP, Kandziora F. Mechanical concepts for disc regeneration. Eur Spine J. 2006;15(Suppl 3):S354–S360. doi: 10.1007/s00586-006-0176-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Antoniou J, Steffen T, Nelson F, Winterbottom N, Hollander AP, Poole RA, Aebi M, Alini M. The human lumbar intervertebral disc: evidence for changes in the biosynthesis and denaturation of the extracellular matrix and growth, maturation, ageing and degeneration. J Clin Invest. 1996;98(4):996–1003. doi: 10.1172/JCI118884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adams MA, Dolan P. Intervertebral disc degeneration: evidence for two distinct phenotypes. J Anat. 2012;221(6):497–506. doi: 10.1111/j.1469-7580.2012.01551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suri P, Hunter DJ, Jouve C, Hartigan C, Limke J, Pena E, Swaim B, Li LIng, Rainville J. Inciting events associated with lumbar disc herniation. The Spine Journal. 2010;10(5):388–395. doi: 10.1016/j.spinee.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin MD, Boxwell CM, Malone DG. Pathophysiology of lumbar disc degeneration: a review of the literature. Neurosurgical Focus. 2002;13(2):1–6. doi: 10.3171/foc.2002.13.2.2. [DOI] [PubMed] [Google Scholar]
- 40.Feng H, Danfelter M, Stromqvist B, Heinegard D. Extracellular matrix in disc degeneration. J Bone Joint Surg Am. 2006;88(S2):25–29. doi: 10.2106/JBJS.E.01341. [DOI] [PubMed] [Google Scholar]
- 41.Walker MH, Anderson DG. Molecular basis of intervertebral disc degeneration. The Spine Journal. 2004;4(6):S158–S166. doi: 10.1016/j.spinee.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Brisby H. Pathology and possible mechanisms of nervous system response to disc degeneration. J Bone Joint Surg Am. 2006;88:68–71. doi: 10.2106/JBJS.E.01282. [DOI] [PubMed] [Google Scholar]
- 43.Smith LJ, Fazzalari NL. The elastic fibre network of the human lumbar annulus fibrosus: architecture, mechanical function and potential role in the progression of intervertebral disc degeneration. Eur Spine J. 2009;18(4):439–448. doi: 10.1007/s00586-009-0918-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guiot BH, Fessler RG. Molecular biology of degenerative disc disease. Neurosurgery. 2000;47(5):1034–1040. doi: 10.1097/00006123-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Del Grande F, Maus TP, Carrino JA. Imaging the intervertebral disk: age-related changes, herniations, and radicular pain. Radiol Clin North Am. 2012;50(4):629–649. doi: 10.1016/j.rcl.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 46.Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 1995;20(11):1307–1314. doi: 10.1097/00007632-199506000-00022. [DOI] [PubMed] [Google Scholar]
- 47.Edgar MA. The nerve supply of the lumbar intervertebral disc. J Bone Joint Surg Br. 2007;89(9):1135–1139. doi: 10.1302/0301-620X.89B9.18939. [DOI] [PubMed] [Google Scholar]
- 48.Yamashita T, Minaki Y, Oota I, Yokogushi K, Ishii S. Mechanosensitive afferent units in the lumbar intervertebral disc and adjacent muscle. Spine (Phila Pa 1976) 1993;18(15):2252–2256. doi: 10.1097/00007632-199311000-00018. [DOI] [PubMed] [Google Scholar]
- 49.Chou R, Qaseem A, Snow V, Casey D, Cross T, Jr, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the american college of physicians and the american pain society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 50.Standaert CJ, Friedly J, Erwin MW, Lee MJ, Rechtine G, Henrikson NB, Norvell DC. Comparative effectiveness of exercise, acupuncture and spinal manipulation for low back pain. Spine. 2011;36(21S):S120–S130. doi: 10.1097/BRS.0b013e31822ef878. [DOI] [PubMed] [Google Scholar]
- 51.Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. The Spine Journal. 2004;4(3):335–356. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 52.Barr KP, Griggs M, Cadby T. Lumbar stabilization: core concepts and current literature, Part 1. Am J Phys Med Rehabil. 2005;84(6):473–480. doi: 10.1097/01.phm.0000163709.70471.42. [DOI] [PubMed] [Google Scholar]
- 53.Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an education booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339:1021–1029. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 54.Freemont AJ, Watkins A, Le Maitre C, Jeziorska M, Hoyland JA. Current understanding of cellular and molecular events in intervertebral disc degeneration: implications for therapy. J Pathol. 2002;196:374–379. doi: 10.1002/path.1050. [DOI] [PubMed] [Google Scholar]
- 55.Burke JG, Watson RW, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM. Intervertebral discs which cause low back pain secrete high levels of proinflamatory mediators. J Bone Joint Surg Br. 2002;84(2):196–201. doi: 10.1302/0301-620x.84b2.12511. [DOI] [PubMed] [Google Scholar]
- 56.Shamji M, Setton LA, Wingrove J, So Stephen, Chen Jun, Jing Liufang, Bullock R, Isaacs RE, Brown C, Richardson WJ. Proinflammatory cytokine expression profile in degenerated and herniated human intervertebral disc tissues. Arthritis Rheum. 2010;62(7):1974–1982. doi: 10.1002/art.27444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brinckmann P, Porter RW. A laboratory model of lumbar disc protrusion. Fissure and fragment. Spine (Phila Pa 1976) 1994;19(2):228–235. doi: 10.1097/00007632-199401001-00019. [DOI] [PubMed] [Google Scholar]
- 58.Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. The Spine Journal. 2008;8:213–225. doi: 10.1016/j.spinee.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 59.Kawchuk GN, Carrasco A, Beecher G, Goertzen D, Prasad N. Identification of spinal tissues loaded by manual therapy: a robot-based serial dissection technique applied in porcine motion segments. Spine (Phila Pa 1976) 2010;35(22):1983–1990. doi: 10.1097/BRS.0b013e3181ddd0a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Oliphant D. Safety of spinal manipulation in the treatment of lumbar disk herniation: a systematic review and risk assessment. J Manipulative Physiol Ther. 2004;27(3):197–210. doi: 10.1016/j.jmpt.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 61.Jagbandhansingh MP. Most common causes of chiropractic malpractice lawsuits. J Manipulative Physiol Ther. 1997;20(1):60–64. [PubMed] [Google Scholar]