Abstract
Background:
Male factor has been considered as a 50% of infertility causes. One of the reasons for poor semen quality is oxidative stress. Saffron and vitamin E as antioxidant agent can be involved in free radical scavenging and improvement of semen quality.
Materials and Methods:
We divided 30 adult male Wistar rats into saffron (n = 10), vitamin E (n = 10) and control (n = 10) groups randomly. Saffron (100 mg/kg/day), vitamin E (100 mg/kg/day), and distilled water (0.5 ml/day) were fed by gavage to the animals for 60 consecutive days in aforementioned groups. After cervical dislocation, both testes and left epididymis of each animal were removed and the cauda epididymal spermatozoa were aspirated for analysis of sperm parameters. Sperm membrane integrity was assessed by hypo-osmotic swelling test (HOST). In different groups, seminiferous tubule histological assessments were done after Hematoxylin -Eosin staining.
Results:
The mean percentage of HOST positive sperm was increased in vitamin E and saffron groups as compared to control group. As we can see there was a significant difference among control and experimental groups (P < 0.001); also a significant difference was obtained between vitamin E and saffron groups (P = 0.002). The evaluation of seminiferous tubules has shown no significant differences among groups.
Conclusions:
The present data suggest that saffron had superior antioxidant properties which can improve sperm parameters and membrane integrity so it can lead to develop fertility potential.
Keywords: Antioxidants, cell membrane integrity, infertility, spermatogenesis
INTRODUCTION
Oxidative stress (OS), a harmful condition especially for sperm, results from an imbalance between the production of reactive oxygen species (ROS) and their efficient removal by available antioxidant systems, which can lead to increased rate of cellular damage.[1] Because of high rates of metabolism and cell replication in the testis, oxidative stress can be especially damage in seminiferous tubules. Although spermatogonia are protected by blood-testis barrier, spermatogonial degeneration can occur by exposure to heat and radiation, deficiencies of hormones, immunodeficiency, and toxic chemicals.[2] It showed that chemicals can cause to destruction of seminiferous basement membranes.[3] It also has been reported that human spermatozoa are capable of spontaneous lipid peroxidation and generating reactive oxygen species.[4] Double bonds polyunsaturated fatty acid molecules in the sperm plasma membrane make sperm vulnerable to free radicals attack. This offense can lead to decrease in sperm membrane integrity and damage to chromatin, proteins, and the entire cellular components. Chromatin condensation and antioxidant system are two effective strategies which equips sperm against oxidative stress. Antioxidants protect the sperm cellular content by neutralizing unpaired electron of free radicals.[5]
Vitamin E (a-tocopherol), a significant antioxidant necessary for the maintenance of mammalian spermatogenesis,[6] is a powerful antioxidant resides on the cell membrane and plays an important role to protect the cell by breaking oxidative chain.[7] It has been shown to suppress lipid peroxidation in testicular microsomes and mitochondria.[6,8] Vitamin E is present in principally high amounts in Sertoli cells and pachytene spermatocytes. Deficiency of this vitamin can lead to oxidative stress in the testes that disturbs spermatogenesis.[6]
Applying medicinal herbs has traditionally been noted from ancient. Recently, due to the undesirable side effects of chemical drugs, more emphasis has been placed on the usage of traditional medicine, particularly plant therapy. Crocus sativus L. commonly known as saffron is a perennial stem less herb of the Iridaceae family which is principally grown in Iran. Previous studies have shown that saffron, as a powerful antioxidant contains vitamins especially riboflavin and thiamine, prevents damages to the chromosomes and modulates lipid peroxidation.[9] Saffron was applied in large number of research for various purposes such as antioxidant effect,[10] sexual potential stimulant,[11] genetic protection effect,[12] positive effect on folliculogenesis,[13] sperm parameter improvement.[14]
We designed this study in order to examine the influence of saffron (Crocus sativus L.) as an antioxidant and vitamin E as a positive control on rat sperm parameters, membrane integrity, and spermatogenesis status.
MATERIALS AND METHODS
Experimental animals
This study was carried out on 30 mature (12 weeks old) male Wistar rats (180-200 g) procured from Pasteur Institute, Tehran, Iran. All animal procedures were approved by Isfahan University of medical sciences ethical committee. Animals were housed in colony cages; each cage contains five rats. All rats kept at 18-24°C temperature, under 12 hours light and 12 hours dark conditions. Laboratory pellet chow and water were always available. Acclimatization of Animals was done for 10 days before experiment. Rats were randomly assigned into three following groups: saffron, vitamin E, and control (10 rats in each group). Rats received 100 mg/kg/day saffron, 100 mg/kg/day vitamin E, and 0.5 ml/day distilled water via gavage, in aforementioned groups. After 60 days (according to spermatogenesis period in rats) all animals were euthanized by chloroform anesthetization and then cervical dislocation.
Saffron and vitamin E
Saffron purchased from Ghaen – Khorasan – Iran. One gram saffron was grounded and soaked in 20 mL warmed distilled water and then stirred for at least two hours. The solution was stored at 4°C for further use. Vitamin E purchased from Sigma Chemical Co., St Louis, Mo.w
Epididymal sperm preparation
Left epididymis of each rat was removed immediately after dissection. The distal end of the cauda epididymis was separated and placed in 1 mL of pre-warm normal saline (37°C). The tissue was cut by several incisions; sperm were allowed to swim out into the dish by gentle shaking. The sperm suspension was put in incubator for 10 minutes.
Sperm parameters
The sperm count and motility was assessed using Neubauer's chamber (LABART, Germany) and phase-contrast microscope (Nikon TE2000-U, Japan) at magnification ×200. One ml of suspension was added to 9 ml normal saline. An aliquot of the fresh sperm suspension was put into the Neubauer's chamber.[15] Sperm motility was determined and data was expressed as percentage of motile and non-motile spermatozoa.
In order to identify normal and abnormal sperm cell morphology, phase-contrast microscope was used at ×400. Briefly, cauda epididymis sperm suspension was diluted 1:10 with 10% normal saline; 200 spermatozoa per each animal sample were classified as one of the following: (1) Total abnormality, (2) abnormal heads (include headless, flattened head and pin head), (3) abnormal neck (bend neck), and (4) abnormal tail (bent tail).
Seminiferous tubules properties
The testes in different groups were removed, weighed by digital scale (A and D company) with an accuracy of 0.001 g and then fixed in Bouin's fluid for 24 hours. The tissue was processed for paraffin embedding and 5 μm thick paraffin sections were stained with hematoxylin and eosin (H and E). The sections were analyzed by light microscope for the seminiferous tubules outer and lumen diameters, germinal epithelial height, as well as spermatogonia and primary spermatocyte counting in similar sections [Figure 1].
Figure 1.

Photographs of testis histology in control (a), vitamin E (b), and saffron (c) groups
Sperm cell membrane integrity
To assess rat sperm plasma membrane integrity, the hypo-osmotic swelling test (HOST) was used in accordance with a previously described technique.[15] The hypo-osmotic solution (150 mOsm/L) was prepared by dissolving 7.35 g of sodium citrate (C6H5Na3O7.2H2O) and 13.51 g fructose in 1000 ml of distilled water. An aliquot of 0.1 ml cauda epididymal sperm suspension was mixed with 1 ml hypo-osmotic solution and incubated at 37°C for an hour. Two hundred sperm per each sample were counted in different fields at ×400 under phase contrast microscope and HOST positive sperms with coiled tails were determined [Figures 2 and 3].[15]
Figure 2.

Photographs of HOS test in control (a), vitamin E (b), and saffron (c) groups
Figure 3.
The mean percentage of HOST + sperm in different groups. *P < 0.05, ***P < 0.001, compared with control group. a: as compared with saffron group
Statistical analysis
The SPSS 17.0 software was applied for data analyzing. All data are expressed as mean ± standard error of the mean (mean ± SE); Data were considered statistically significant when P < 0.05. Data were compared with One-Way ANOVA followed by Tukey's post hoc test for multiple comparisons.
RESULTS
Sperm parameters
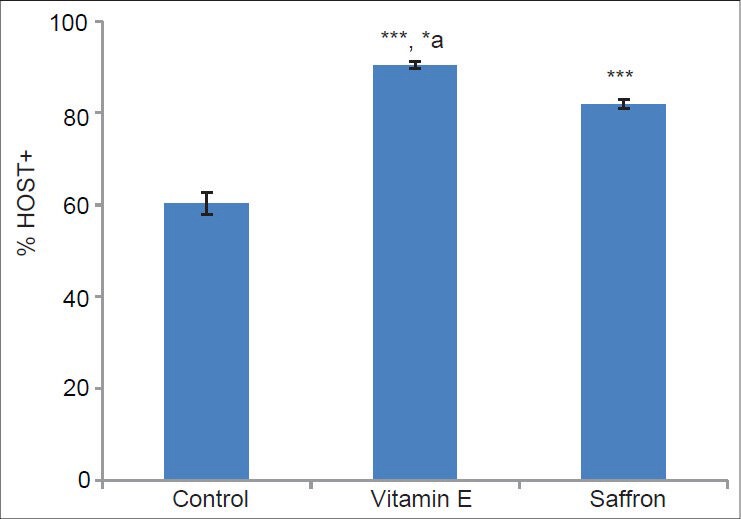
Treatment of rats with vitamin E and saffron had no significant increase the mean percentage of sperm concentration when compared with control group (P = 0.40 and P = 0.88 respectively), while the mean percentages of motile sperm in vitamin E and saffron groups had significant difference in comparison with control group (P < 0.001); also a significant difference in motile sperm was seen between saffron and vitamin E groups (P = 0.007). On the other hand, the mean percentage of abnormal morphology was significantly decreased in treated groups when compared with control group (P < 0.001). Also subset morphological abnormalities in saffron and vitamin E groups had significant difference in comparison with control group (P < 0.001) [Table 1].
Table 1.
The mean percentage of rat sperm parameters in different groups
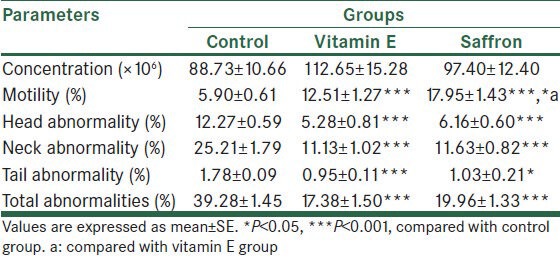
Seminiferous tubules properties
The means percentages of testes weight were 1.07 ± 0.05, 1.27 ± 0.00, and 1.24 ± 0.05 in control, vitamin E and saffron groups respectively. Our results showed that there was no significant difference in testes weight among control and experimental groups (P > 0.05). Outer and lumen diameters as well as germinal epithelial height of seminiferous tubules were measured and no significant difference were seen in the mean percentage of outer, lumen, and germinal epithelial diameters of seminiferous tubules among control and treatment groups (P > 0.05) [Table 2]. Similarly, the mean percentage of spermatogonia and primary spermatocytes count did not have any significant difference among control and experimental groups (P > 0.05) [Table 2, Figure 1].
Table 2.
The mean percentage of various parameters related to Semniferous tubule properties in control, vitamin E, and saffron groups
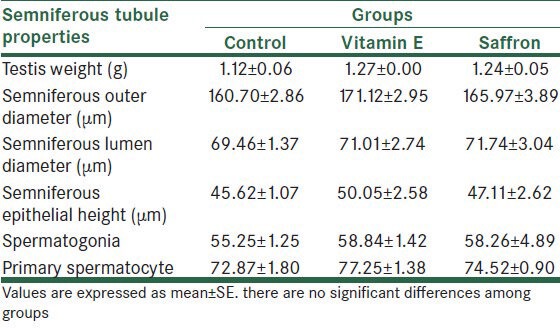
Sperm membrane integrity
The evaluation of sperm membrane integrity with HOS test showed that the mean percentage of sperm HOST+ (with coiled tail) increased in vitamin E and saffron groups when compared with control group (P < 0.001). Also the mean percentage of HOST + sperm increased in vitamin E group related to saffron group (P = 0.002), [Figures 2 and 3].
DISCUSSION
Based on this study, vitamin E and saffron consuming have statistically relevance with enhancement of sperm parameters and membrane integrity, which may lead to increase male reproductive potential.
Almost 15% of couples trying to conceive are clinically infertile and male factor is considered as a 50% of those cases.[16] About 45% of male infertility cases have one of the following problems: varicocele, cryptorchidism, testicular torsion, and endocrinopathy, which all are associated with excessive production of testicular ROS.[16] ROS are oxygen-based molecules that due to the unpaired electron in the electron layer are highly reactive. ROS are largely generated as a result of redox reactions within the mitochondria, the catalytic reactions of the steroidogenic cytochrome P-450 enzymes, and steroidogenesis; but under pathologic condition it can be produced in large amounts by macrophages, neutrophils, and other cell types like spermatozoa.[16,17] Sperm is equipped with two effective mechanisms, sperm chromatin condensation and antioxidant system. During spermiogenesis, histones are replaced by protamines. This rearrangement has made chromatin highly resistant against agents such as detergents, acids, DNase, and proteases.[18]
On the other hand, sperm are protected against oxidative stress by three different antioxidant protection systems: endogenous antioxidants, dietary antioxidants, and metal-binding proteins.[19,20,21,22,23] Endogenous antioxidants comprise enzymatic and non-enzymatic antioxidants. Enzymatic antioxidants include superoxide dismutase (SOD), catalase, glutathione peroxidase (GPX), and glutathione reductase (GRD). Non-enzymatic antioxidants contain ascorbate, vitamin E, vitamin A, glutathione, pyruvate, albumin, ubiquitol, taurine, and hypotaurine.[19,21] Dietary antioxidants (dietary supplements) are usually present in the form of vitamin C, vitamin E, beta-carotenes, carotenoids, and flavonoids.[23] Metal-binding proteins include albumin, ceruloplasmin, metallothionein, transferrin, ferritin, and myoglobin.[22] When excessive ROS is produced, antioxidant system is incapable to counteract it which leads to condition called oxidative stress. All cellular components are the potential target of oxidative stress.[1,5,24]
On the other hand, approximately 25% of male infertility patients with idiopathic cause have abnormal semen analyses.[25] Our results showed that saffron can improve rat sperm parameters (especially motility); but sperm concentration didn’t have statistically influenced. In agreement, it has been demonstrated that applying 50 mg saffron three times a week for three months caused to significant increase in normal human sperm morphology and motility (P < 0.001), but did not have significantly change in the sperm concentration.[14] It also has been shown that crocin especially at 1 mM ameliorated motility in red deer cryopreserved frozen thawed sperm, but it had no effect on lipid peroxidation.[26] It seems that saffron exerts these effects based on its antioxidant properties. The antioxidant activity of saffron is due to its ingredients (safranal, crocin, crocetin, and dimethyl crocetin); each of these agents has individual antioxidant characteristic; however, the synergistic effect of them gives saffron a significant antioxidant potential.[27] Conversely, in another study it was showed that applying saffron (60 mg/day) did not have any positive effect on sperm parameters (density, morphology and motility) in human infertile subject with idiopathic oligoasthenoteratozoospermia compared with placebo group. Also saffron did not significantly improve total seminal plasma antioxidant capacity of these patients in compare with control group.[28] Dissimilarity with our results could be due to administration of different dose.
Vitamin E, as an endogenous and dietary antioxidants (dietary supplements), associating with normal function of male reproductive system, can protect sperm and its cellular structure against free radicals.[29] The effect of Vitamin E on human breeding soundness and preservation of mammalian spermatogenesis is so clear that is introduced as an “anti-sterility vitamin”.[29] Vitamin E is a powerful lipophilic antioxidant resides on the cell membrane which can play an important role to protect the cell by breaking oxidative chain.[7]
Our results revealed that vitamin E can increase sperm motility and decrease abnormal morphology, but cannot affect significantly sperm concentration. Similar to our results, it was reported that administration of vitamin E 300 mg in patient with asthenospermia caused to significant increase in sperm motility.[30] Another study has shown that antioxidant therapy with 600 mg N-acetylcysteine (NAC) and vitamins–minerals caused to significant increase in sperm concentration of patient with oligospermia.[31] Also oral administration of vitamin E (400 mg) and selenium (225 mg) caused to significant increase in sperm motility and concentration of infertile men.[32] Moreover, Momeni and his colleagues administered vitamin E alone and with para-nonylphenol (p-NP) in rats. They reported that vitamin E ameliorated sperm viability in vitamin E and p-NP groups compared with control group. As well as sperm count, sperm with progressive motility, and non-motile sperm were improved in p-NP with vitamin E group compared with p-NP group.[33] In contrast, no significant changes were made in human sperm concentration, motility, and morphology after three months treatment with 600 mg vitamin E.[34] Perhaps this dissimilarity could be due to administration different doses.
However, current sperm selection method for using in ART are still based on conventional semen parameters especially sperm morphology and motility which may not be related to chromatin integrity.[35] Customary parameters used for evaluation of sperm are limited applications because they only help to assess the structural integrity of the cell.[36] Sperm comprises of several sub-morphological compartments with different functions, all of which must be intact for successful fertilization.[37] In fact sperm cell membrane, is composed of large amounts of double bonds polyunsaturated fatty acids, is the main potential purposes of the free radicals attack. In normal condition this structure gives sperm membrane fluidity and flexibility, on the other hand, presence of fatty acids make cell vulnerable to lipid peroxidation. During lipid peroxidation, free radicals attack to fatty acid chains to form lipid free radicals, which may react with molecular oxygen and generate the lipid peroxyl radical. Peroxyl radicals also can react with fatty acid chain, so reaction is continued.[5,38] Lipid peroxidation reduces membrane integrity, causing increased cell permeability to electrolytes which is harmful to cell's energy forming mechanism. Protease and phospholipase activation occur due to increased intracellular calcium that can lead to further damage to proteins and lipids.[20] The hypo-osmotic swelling test selects sperm with functionally membrane integrity.[39] HOST can determine viable sperm, based on fluid transportation across intact cell membrane under hypo-osmotic conditions leads to expansion of the cell, especially in the tail, which can be readily observed with a phase contrast microscope. HOST is quick and simple, and requires minimal equipment.[15]
Our results indicate that saffron and vitamin E can ameliorate sperm membrane integrity (P < 0.001); however, the results of vitamin E was better. In other words, In the presence of vitamin E sperm with coiled tail significantly increased compared to attendance of saffron (P < 0.05). In accordance it has been shown that supplemental antioxidants (zinc, cobalt, and selenium) in ram lambs cause to significant increases in motility, live sperm, and intact membranes indicated by the HOST.[40] Miciński et al. (2011) showed that sperm morphology was positively correlated with sperm motility and HOST results.[41]
Spermatogenesis is a complex process in which spermatogonial stem cells (SSCs) divide and differentiate ultimately to form spermatozoa, a haploid germ cell. This process is performed throughout the most adult mammal's life continuously.[42] SSCs are at the basis of male fertility by their ability to balance self-renewing and differentiating divisions. This balance maintains the stem cell population and supply the proliferative demand to produce millions of sperm each day.[42] Due to excessive production of ROS in the pathologic status, testicular testosterone could be extremely reduced which can affect spermatogenesis.[17] SSCs are well protected by blood-testis barrier, a natural shield, nevertheless SSCs and their progeny are vulnerable to radiation (X-ray), alcohol, and some chemicals.[42] It seems that antioxidants can maintain spermatogenesis from possible damage by neutralizing free radicals. Although Modaresi and his colleagues (2008) showed that the applying saffron 100 mg/kg/48h in mice cause to increase in the number of primary spermatocytes;[43] our results showed that seminiferous tubules properties had not significantly changed in the treatment groups related to control groups.
CONCLUSION
According to this experiment, vitamin E and saffron are efficient on rat reproductive system. These outcomes may be due to their antioxidant functions. As respects saffron comprises various active constituents, further studies are needed to define their mechanism of action and effective dosage in human. However, the efficiency of saffron and vitamin E on spermatogenesis had been investigated; our results revealed no significant changes in seminiferous tubules diameters, spermatogonia and primary spermatocyte counting. Nevertheless, we acknowledge the need for further studies on the effect of antioxidants such as saffron and vitamin E on spermatogenesis and testis histology.
ACKNOWLEDGMENT
This study was supported by Isfahan University of Medical Sciences (Grant No. 391243).
Footnotes
Source of Support: This study was supported by Isfahan University of Medical Sciences (Grant No. 391243).
Conflict of Interest: None declared.
REFERENCES
- 1.Geva E, Lessing JB, Lerner-Geva L, Amit A. Free radicals, antioxidants and human spermatozoa: Clinical implications. Hum Reprod. 1998;13:1422–4. doi: 10.1093/oxfordjournals.humrep.a019709. [DOI] [PubMed] [Google Scholar]
- 2.Richburg JH, Boekelheide K. Mono-(2-ethylhexyl) phthalate rapidly alters both Sertoli cell vimentin filaments and germ cell apoptosis in young rat testes. Toxicol Appl Pharmacol. 1996;137:42–50. doi: 10.1006/taap.1996.0055. [DOI] [PubMed] [Google Scholar]
- 3.Yang HS, Han DK, Kim JR, Sim JC. Effects of a-tocopherol on cadmium-induced toxicity in rat testis and spermatogenesis. J Korean Med Sci. 2006;21:445–51. doi: 10.3346/jkms.2006.21.3.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alvarez JG, Touchstone JC, Blasco L, Storey BT. Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa Superoxide dismutase as major enzyme protectant against oxygen toxicity. J Androl. 1987;8:338–48. doi: 10.1002/j.1939-4640.1987.tb00973.x. [DOI] [PubMed] [Google Scholar]
- 5.Bucak MN, Sarıözkan S, Tuncer PB, Sakin F, Ateşşahin A, Kulaksız R, et al. The effect of antioxidants on post-thawed Angora goat (Capra hircus ancryrensis) sperm parameters, lipid peroxidation and antioxidant activities. Small Rumin Res. 2010;89:24–30. doi: 10.1016/j.cryobiol.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Aitken RJ, Roman SD. Antioxidant systems and oxidative stress in the testes. Oxid Med Cell Longev. 2008;1:15–24. doi: 10.4161/oxim.1.1.6843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bansal AK, Bilaspuri GS. Antioxidant effect of vitamin E on motility, viability and lipid peroxidation of cattle spermatozoa under oxidative stress. Anim Sci Pap Rep. 2009;27:5–14. [Google Scholar]
- 8.Gavazza MB, Catala A. The effect of a-tocopherol on lipid peroxidation of microsomes and mitochondria from rat testis. Prostaglandins Leukot Essent Fatty Acids. 2006;74:247–54. doi: 10.1016/j.plefa.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Premkumar K, Abraham SK, Santhiya ST, Ramesh A. Protective effects of saffron (Crocus sativus Linn.) on genotoxins-induced oxidative stress in Swiss albino mice. Phytother Res. 2003;17:614–7. doi: 10.1002/ptr.1209. [DOI] [PubMed] [Google Scholar]
- 10.Papandreou MA, Tsachaki M, Efthimiopoulos S, Cordopatis P, Lamari FN, Margarity M. Memory enhancing effects of saffron in aged mice are correlated with antioxidant protection. Behav Brain Res. 2011;219:197–204. doi: 10.1016/j.bbr.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Mansoori P, Akhondzadeh S, Raisi F, Ghaeli P, Jamshidi AH, Nasehi AA, et al. A randomized, double-blind, placebo-controlled study of safety of the adjunctive saffron on sexual dysfunction induced by a selective serotonin reuptake inhibitor. J Med Plants. 2011;10:121–30. [Google Scholar]
- 12.Premkumar K, Thirunavukkarasu C, Abraham S, Santhiya S, Ramesh A. Protective effect of saffron (Crocus sativus L.) aqueous extract against genetic damage induced by anti-tumor agents in mice. Hum Exp Toxicol. 2006;25:79–84. doi: 10.1191/0960327106ht589oa. [DOI] [PubMed] [Google Scholar]
- 13.Mokhtari M, Sharifi E, Daneshi A. Effects of Hydro-alcoholic extract of red dried stigmas of crocus sativus L. Flowers (saffron) on the levels of pituitary-ovary hormones and folliculogenesis in Rats. Int J Fertil Steril. 2010;3:185–90. [Google Scholar]
- 14.Heidary M, Vahhabi S, Reza Nejadi J, Delfan B, Birjandi M, Kaviani H, et al. Effect of saffron on semen parameters of infertile men. Urol J. 2008;5:255–9. [PubMed] [Google Scholar]
- 15.Jeyendran RS, Van der Ven HH, Perez-Pelaez M, Crabo BG, Zaneveld LJ. Development of an assay to assess the functional integrity of the human sperm membrane and its relationship to other semen characteristics. J Reprod Fertil. 1984;70:219–28. doi: 10.1530/jrf.0.0700219. [DOI] [PubMed] [Google Scholar]
- 16.Turner TT, Lysiak JJ. Oxidative stress: A common factor in testicular dysfunction. J Androl. 2008;29:488–98. doi: 10.2164/jandrol.108.005132. [DOI] [PubMed] [Google Scholar]
- 17.Hanukoglu I. Antioxidant protective mechanisms against reactive oxygen species (ROS) generated by mitochondrial P450 systems in steroidogenic cells. Drug Metab Rev. 2006;38:171–96. doi: 10.1080/03602530600570040. [DOI] [PubMed] [Google Scholar]
- 18.Mahi CA, Yanagimachi R. Induction of nuclear decondensation of mammalian spermatozoa in vitro. J Reprod Fertil. 1975;44:293–6. doi: 10.1530/jrf.0.0440293. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal A NK, Allamaneni SS, Said TM. Role of antioxidants in treatment of male infertility: An overview of the literature. Reprod Bio Med Online. 2004;8:616–27. doi: 10.1016/s1472-6483(10)61641-0. [DOI] [PubMed] [Google Scholar]
- 20.Halliwell B. Free radicals, antioxidants, and human disease: Curiosity, cause, or consequence? Lancet. 1994;344:721–4. doi: 10.1016/s0140-6736(94)92211-x. [DOI] [PubMed] [Google Scholar]
- 21.Sikka SC. Oxidative stress and role of antioxidants in normal and abnormal sperm function. Front Biosci. 1996;1:78–86. doi: 10.2741/a146. [DOI] [PubMed] [Google Scholar]
- 22.Makker K, Sharma R. Oxidative stress and male infertility. Indian J Med Res. 2009;129:357–67. [PubMed] [Google Scholar]
- 23.Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2005;3:1–21. doi: 10.1186/1477-7827-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: An update. Am J Reprod Immunol. 2007;59:2–11. doi: 10.1111/j.1600-0897.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- 25.Sigman M, Jarow J. Male Infertility. In: Wein AJ, editor. Campbell-Walsh Urology. 9th ed. Philadelphia Pa: Sanders Elsevier; 2007. pp. 609–53. [Google Scholar]
- 26.Dominguez-Rebolledo AE, Fernandez-Santos MR, Bisbal A, Ros-Santaella JL, Ramon M, Carmona M, et al. Improving the effect of incubation and oxidative stress on thawed spermatozoa from red deer by using different antioxidant treatments. Reprod Fertil Dev. 2010;22:856–70. doi: 10.1071/RD09197. [DOI] [PubMed] [Google Scholar]
- 27.Kumar V, Bhat Z, Kumar D, Khan N, Chashoo I, Shah M. Pharmacological profile of crocus sativus-a comprehensive review. Pharmacologyonline. 2011;3:799–811. [Google Scholar]
- 28.Safarinejad MR, Shafiei N, Safarinejad S. A prospective double-blind randomized placebo-controlled study of the effect of saffron (Crocus sativus Linn.) on semen parameters and seminal plasma antioxidant capacity in infertile men with idiopathic oligoasthenoteratozoospermia. Phytother Res. 2011;25:508–16. doi: 10.1002/ptr.3294. [DOI] [PubMed] [Google Scholar]
- 29.Uzunhisarcikli M, Kalender Y, Dirican K, Kalender S, Ogutcu A, Buyukkomurcu F. Acute, subacute and subchronic administration of methyl parathion-induced testicular damage in male rats and protective role of vitamins C and E. Pestic Biochem Physiol. 2007;87:115–22. [Google Scholar]
- 30.Suleiman SA, Ali ME, Zaki ZM, el-Malik EM, Nasr MA. Lipid peroxidation and human sperm motility: Protective role of vitamin E. J Androl. 1996;17:530–7. [PubMed] [Google Scholar]
- 31.Paradiso Galatioto G, Gravina GL, Angelozzi G, Sacchetti A, Innominato PF, Pace G, et al. May antioxidant therapy improve sperm parameters of men with persistent oligospermia after retrograde embolization for varicocele? World J Urol. 2008;26:97–102. doi: 10.1007/s00345-007-0218-z. [DOI] [PubMed] [Google Scholar]
- 32.Keskes-Ammar L, Feki-Chakroun N, Rebai T, Sahnoun Z, Ghozzi H, Hammami S, et al. Sperm oxidative stress and the effect of an oral vitamin E and selenium supplement on semen quality in infertile men. Arch Androl. 2003;49:83–94. doi: 10.1080/01485010390129269. [DOI] [PubMed] [Google Scholar]
- 33.Momeni HR, Soleimani Mehranjani M, Abnosi MH, Mahmoodi M. Effects of vitamin E on sperm parameters and reproductive hormones in developing rats treated with para-nonylphenol. Iran J Reprod Med. 2009;7:111–6. [Google Scholar]
- 34.Kessopoulou E, Powers H, Sharma K, Pearson M, Russell J, Cooke I, et al. A double-blind randomized placebo cross-over controlled trial using the antioxidant vitamin E to treat reactive oxygen species associated male infertility. Fertil Steril. 1995;64:825–31. doi: 10.1016/s0015-0282(16)57861-3. [DOI] [PubMed] [Google Scholar]
- 35.Razavi S, Nasr-Esfahani M, Deemeh M, Shayesteh M, Tavalaee M. Evaluation of zeta and HA-binding methods for selection of spermatozoa with normal morphology, protamine content and DNA integrity. Andrologia. 2010;42:13–9. doi: 10.1111/j.1439-0272.2009.00948.x. [DOI] [PubMed] [Google Scholar]
- 36.Neild D, Chaves G, Flores M, Mora N, Beconi M, Agüero A. Hypo-osmotic test in equine spermatozoa. Theriogenology. 1999;51:721–7. doi: 10.1016/s0093-691x(99)00021-7. [DOI] [PubMed] [Google Scholar]
- 37.Amann R, Graham J. Equine Reproduction. Philadelphia: Lea and Febiger; 1993. Spermatozoal function; pp. 715–45. [Google Scholar]
- 38.Agarwal A, Prabakaran SA. Mechanism, measurement and prevention of oxidative stress in male reproductive physiology. Indian J Exp Biol. 2005;43:963–74. [PubMed] [Google Scholar]
- 39.World Health Organization. 4th ed. Cambridge: Cambridge University Press; 1999. WHO Laboratory Manual for the examination of human semen and Sperm-cervical mucus interaction; p. 128. [Google Scholar]
- 40.Kendall NR, McMullen S, Green A, Rodway RG. The effect of a zinc, cobalt and selenium soluble glass bolus on trace element status and semen quality of ram lambs. Anim Reprod Sci. 2000;62:277–83. doi: 10.1016/s0378-4320(00)00120-2. [DOI] [PubMed] [Google Scholar]
- 41.Miciński P, Pawlicki K, Wielgus E, Bochenek M, Gogol P, Ficek B. Total reactive antioxidant potential and DNA fragmentation index as fertility sperm parameters. Reprod Biol. 2011;11:135–44. doi: 10.1016/s1642-431x(12)60050-3. [DOI] [PubMed] [Google Scholar]
- 42.Zhou Q, Griswold MD. StemBook. Cambridge (MA): Harvard Stem Cell Institute; 2008. [Last accessed on 2008 Jul 14]. Regulation of spermatogonia. Available from: http://www.ncbi.nlm.nih.gov/books/NBK27035/ [PubMed] [Google Scholar]
- 43.Modaresi M, Mesripour M, Asadi Morghmaleki M, Hamedanian M. The effect of saffron extract on testis tissue. Iran J Med Aromat Plants. 2008:237–43. [Google Scholar]


