Abstract
Aim:
Was to describe the knowledge, attitude, and actual practices of mothers in a rural area in Egypt regarding breastfeeding, complementary feeding and weaning and to explore the effect of educational background and age on these views.
Materials and Methods:
A community-based cross-sectional study was conducted on 307 rural mothers who have a youngest child aged 2 years or less. Mothers were selected using systematic random sampling.
Results:
All the studied mothers knew that breastfeeding is the best nutritional source for the baby. The majority of the mothers had good knowledge about the advantages of breastfeeding for child. As regards weaning, majority (92.5%) of the mothers defined weaning as breastfeeding cessation. Most of the mothers (94.8%) agreed that breastfeeding protect child from infection, 96.1% agreed that it is the healthiest for infant, 76.5% agreed that breast milk lead to loss of figure, and 83.4% agreed that breastfeeding should be avoided during mother's illness. About 84% initiated breastfeeding immediately after delivery, and 42.7% of the studied mothers offered pre-lacteal feeds to baby before lactation. About thirty quarters (74.2%) of mothers fed colostrum. Exclusive breast-feeding was found to be associated with mother's education (P < 0.0001) but not with mother's age at birth, mother's occupation, or place of birth.
Conclusion:
There is a need for health care system interventions, family interventions, and public health education campaigns to promote optimal BF practices, especially in less educated women.
Keywords: Attitude, breastfeeding, Egypt, knowledge, practice, rural
Introduction
Breastfeeding is the best way of providing ideal food for healthy growth and development of infants, and its advantages range from physiological to psychological for both mother and infants.[1] It is well-known that breastfeeding influences a child's health positively and improves nutritional status.[2,3,4] A meta-analysis from three developing countries showed that infants who were not breastfed had a 6-fold greater risk of dying from infectious diseases within the first 2 months of life than those who were breastfed.[5] Six months of exclusive breastfeeding and continued breastfeeding in first year of life could also prevent 1.3 million child deaths worldwide according to systematic reviews from the Bellagio Child Survival Study Group.[6] In addition, incorrect infant feeding practices pose significant risk for malnutrition among children under the age of 5.[7]
The American Academy of Pediatrics recognizes breastfeeding and human milk as the “normative standards for infant feeding.” Given the documented health benefits, the Academy recommends exclusive breastfeeding for 6 months, followed by continued breastfeeding for at least 12 months as complementary foods are introduced.[8] Weaning is the term usually used to describe the process of cessation of breastfeeding after a period of successful breastfeeding. This usually involves addition of food to infant's diet and/or replacement of breast milk in infant's diet with another type of milk (formula or whole milk). Maternal physiology, infant nutritional needs, infant development, especially the development of biting and chewing, and cultural issues all play a role in the timing of weaning.[9]
The prevalence of breastfeeding differs from one country to another and from one society to another, this of course is due to cultural and religious believes.[10] Delayed breastfeeding initiation, colostrum deprivation, supplementary feeding of breast milk substitutes, early introduction of complementary feeding, and incorrect weaning from breast milk are commonly found practices in communities around the world.[7,11,12,13,14]
This study was conducted to describe the knowledge, attitude, and actual practices of mothers in rural area regarding breastfeeding, complementary feeding and weaning and to explore the effect of educational background and age on these views.
Materials and Methods
A community-based cross-sectional study was conducted in a rural area, El-Minia governorate. By a multistage random sample, El-Minia governorate was found to be divided into 9 districts, from which El-Minia district was chosen randomly; then, El-Minia district was found to be divided into 40 villages, from which a village (Bany Ahmed) was chosen randomly. The study sample consisted of 307 women who have a youngest child aged 2 years or less. Mothers were selected using systematic random sampling. During visit to houses, if there was no child of 2 years or less, next house satisfying this criterion was included. The study was conducted during the period from April 2013 to August 2013. Verbal consent was obtained after the participants had been informed about the study objectives.
Data were collected by using designed well-structured questionnaire completed during face-to- face interviews with the mothers. Data collected included information regarding participants' demographics, knowledge, attitudes, and practices towards breastfeeding and weaning. This questionnaire also had been tested on a small number of eligible mothers as a pilot study to test the reliability of the questions and the time needed to conduct an interview with a mother. Then, proper corrections and adjustment had been fulfilled.
Statistical methods
The Statistical Package for Social Science (SPSS) for Windows (version 11.0) for statistical analysis was used. Quantitative data were presented by mean and standard deviation, while qualitative data were presented by frequency distribution. Chi-square test was used to compare between more than one proportion. A statistically significant level was considered when P value was less than 0.05.
Results
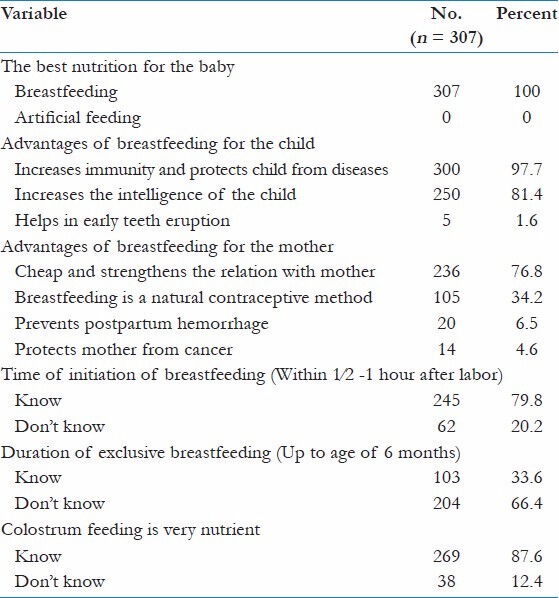
The mean age of the subjects was 28.4 ± 5.9; 44.3% of the studied mothers were able to read and write, and 93.2% were unemployed. As shown in Table 1, all the studied mothers knew that breastfeeding is the best nutritional source for baby. The majority of the mothers had good knowledge about the advantages of breastfeeding for child, 97.9% and 81.4% of the mothers knew that breast milk protects child from diseases as well as increases the intelligence of child, respectively. About 77% of the mothers knew that breastfeeding strengthens the relation between mother and her baby. Minor percentage of the participant mothers stated that breastfeeding prevents postpartum hemorrhage and protects mothers against cancer; (6.5%) and (4.6%), respectively. Nearly 80% of the mothers were aware that the time of initiation of breastfeeding should be within1∕2 hour after labor. About one-third (33.6%) of the mothers knew the proper duration of exclusive breastfeeding. The majority (87.6%) of the participants knew that colostrum feeding is very nutrient for baby.
Table 1.
Knowledge of the studied mothers about breastfeeding, rural area, El-Minia, 2013
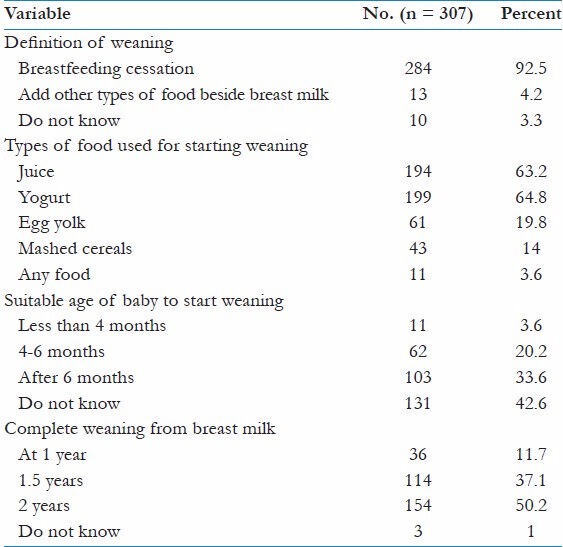
As regards weaning, majority (92.5%) of the mothers defined weaning as breastfeeding cessation. On the other hand, good percentage of the respondents knew that weaning should be started by addition of juices (63.2%) and soft food as yogurt (64.8%). About one-third (33.6%) of the participants knew that 6 months is the suitable age for starting weaning. Unfortunately, 42.6% did not know the suitable age to start weaning. Nearly half (50.2%) of the mothers reported that baby must be weaned completely from breast milk at the age of 2 years and 37.1% said after one and half years [Table 2].
Table 2.
Knowledge of the studied mothers about weaning, rural area, El-Minia, 2013
Most of the mothers (94.8%) agreed that breastfeeding protects child from infection, 96.1% agreed that it is healthiest for infant, 76.5% agreed that breast milk lead to loss of figure, and 83.4% agreed that breastfeeding should be avoided during mother's illness [Table 3]. Table 4 presents the percentages of mothers regarding practice of breastfeeding; 83.7% initiated breastfeeding immediately after delivery, and 42.7% of the studied mothers offered pre-lacteal feeds to the baby before lactation. About thirty quarters (74.2%) of mothers fed colostrum. Majority (95.8%) of the participant fed their child on demand, and 82.7% of them fed their child from both sides at a time. About 32% of mothers breastfed their infants exclusively for 6 months and 71.7% night-fed their infant.
Table 3.
General beliefs of mothers, rural area, El-Minia, 2013
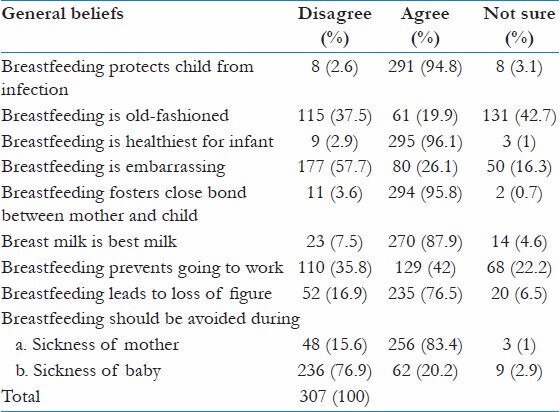
Table 4.
Mothers' practice of breastfeeding, rural area, El-Minia, 2013
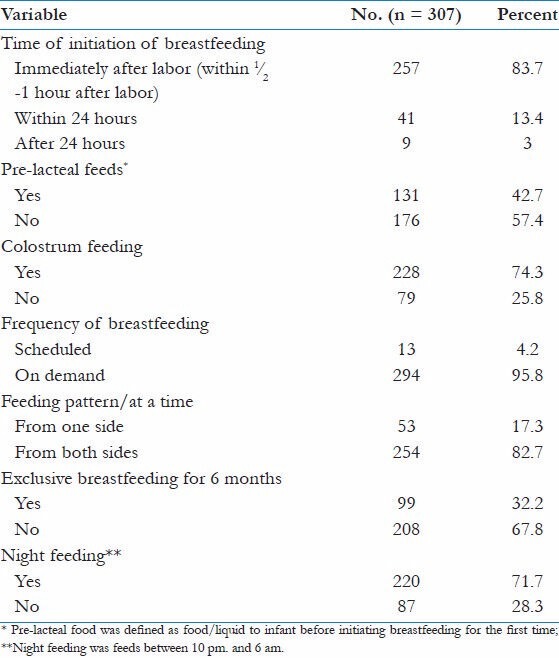
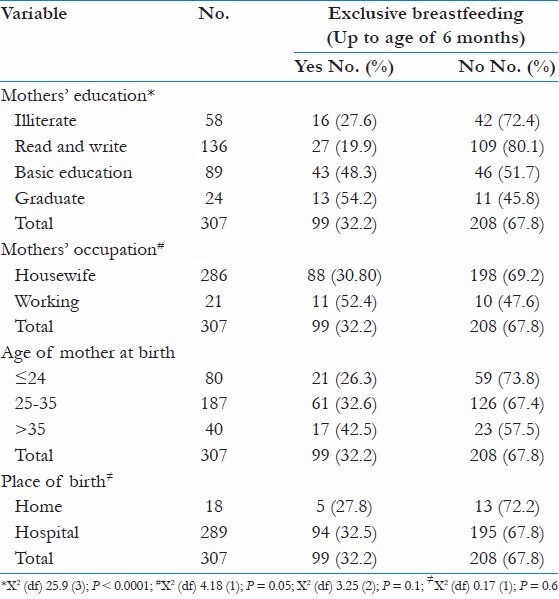
The table 5 showed that out of 307 children, 99 (32.2%) children received exclusive breast-feeding. Exclusive breast-feeding was found to be associated with mother's education (P < 0.0001) but not with mother's age at birth, mother's occupation, or place of birth.
Table 5.
Exclusive breastfeeding in relation to background characteristics of the mother
Discussion
Knowledge about breastfeeding
Several studies over the world have shown that breastfeeding is the universal practice. It seems that mothers don't even consider alternative to this.[15,16,17] In the present study also, all the mothers knew that breastfeeding is the best nutritional source for baby. In a study conducted on Egyptian mothers in Assiut City, about 79% of the participants knew that breast milk promoted bonding between mothers and child and protects child from diseases (Safaa et al., 2012) in comparison to 76.8% and 97.7% of mothers in the present study knew that respectively.[18] It was found that nearly 80% of the mothers were aware that the time of initiation of breastfeeding should be within1∕2 hour after labor and 87.6% of the participants knew that colostrum feeding is very nutrient for baby, but these figures were much higher than those reported by Chaudhary et al. (2011) who found that only 10% and 25% of mothers knew they had to start breastfeeding within1∕2 - 1 hour after birth and knew the benefits of colostrum, and this difference could be explained by valuable effort of health professionals who provide advice and support to mothers during antenatal care visits.[19]
Knowledge about weaning
The current study showed that 92.5% of the mothers defined weaning as breastfeeding cessation and 4.2% defined weaning correctly as introduction of assistant food with breastfeeding; these findings were much lower than that reported by Safaa et al. (2012) who found that less than half of the mothers defined weaning correctly.[18] Yogurt and juice were considered suitable as main diet for weaned infants by 64.8% and 63.2% of women. However, Walkers et al. (2006) who studied mothers' views on feeding infants around the time of weaning found that cow's milk was considered suitable as the main drink for weaned infants.[20] About 33.6% of the participants knew that the suitable age for starting weaning is after 6 month compared to 44.6% as reported by Kishore (2008).[21]
In the current study, 42.6% did not know the suitable age to start weaning. Nearly half (50.2%) of the mothers reported that baby must be weaned completely from breast milk at the age of 2 years, and 37.1% said after one and half years; these findings approximate what reported by Safaa et al. (2012).[18]
The findings of the present study showed that most of the mothers agreed that breastfeeding protects child from infection and agreed that it is healthiest and best for infant, and 83.4% of mothers believed that breastfeeding should be avoided during mother's illness. Similar findings were observed by Woldegebriel (2002) who found that almost all mothers considered human milk as the best milk for good child growth compared to cow's milk and/or formula milk. A higher proportion of mothers considered breast milk alone sufficient enough to feed a baby up to the age of 6 months. Three quarters of mothers preferred not to breastfeed when mother gets sick and may lead to loss of figure. These are potentially harmful beliefs, which could lead to the dangerous practice of abrupt cessation. These harmful beliefs should be well addressed and minimized through continuous health education.[22]
Mothers' practice of breastfeeding
This study showed that 83.7% of the mothers initiated breastfeeding immediately after delivery, which was much higher than what was reported by Shiv et al. (2012), which found that only 20.9% of mothers start breastfeeding within 1 hour after delivery.[23] About 32% of mothers breastfed their infants exclusively for 6 months, which is in agreement with Yeggamal and Chitra (2005) who found that 35% of the studied rural mothers breastfeed their infants exclusively for 6 months. Only 17.3% of women feed their child from one side until whole breast is emptied out. This way, the baby gets hind milk, which is required for brain development.[24] This was similar to Chaudhary et al. (2011) who reported that 85% of mothers were feeding on both sides for 10 minutes each, thinking that feeding on one side is not enough for baby and some thought their breast size would become unequal.[19]
The use of colostrum and avoidance of pre-lacteal foods are cornerstones in early infant nutrition and may be pre-requisites for the establishment of future exclusive breastfeeding. In this study, in practice, nearly 74% of infants had received colostrum. Out of 307 mothers, 42.7% gave pre-lacteal feed, which was greater than what found in a study conducted on Saudi mothers whom been admitted for delivery at maternity hospitals in Riyadh. Pre-lactic feeding was practiced by 10.5% of mothers.[25]
Prolactin is secreted after feed to produce next feed. As secretion of prolactin is more at night, suckling at night is encouraged. In the current study, 71.7% of the mothers night-fed their infant, this was lower than that observed by Chaudhary et al. (2011) who studied knowledge and practice of mothers regarding breast feeding in Nepal and found that 90% mothers were practicing night feed.[19]
In this study, a significant relation between maternal education and exclusive breastfeeding was detected. This was in coherence with Webb et al. (2009) who examined the associations between maternal academic skills and indicators for the initiation of exclusive breastfeeding and timely introduction of complementary foods; mothers in highest category of academic skills had greater odds of initiating exclusive breastfeeding.[26]
Conclusion and Recommendations
Based on the findings of the present study, it was concluded that: Rural women had satisfactory knowledge about the advantages of breastfeeding for child and mother. However, some attitudes and practices of the mothers were suboptimal. This might be due to a low level of education. Hence, it is recommended to develop successful infant-feeding interventions aimed at promoting overall infant health, which can benefit from knowledge of these BF patterns. Our findings also support the need for health care system interventions, family interventions, and public health education campaigns to promote optimal BF practices, especially in less educated women. There is need for improving strategies for maternal care during the antenatal and postnatal periods. Training needs could be extended to staff at private clinics and to traditional birth attendants. This study also recommends further study on attitudes and practices of mothers on breastfeeding covering large sample in community level.
Acknowledgements
We are very much grateful to all participants of study for their kind cooperation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Batal M, Boulghourjin C, Abdullah A, Afifi R. Breast-feeding and feeding practices of infants in a developing country: A national survey in Lebanon. Public Health Nutr. 2005;9:313–9. doi: 10.1079/phn2006860. [DOI] [PubMed] [Google Scholar]
- 2.Horta BL, Bahl R, Martines JC, Victora CG. Evidence on the long-term effects of breastfeeding: Systematic reviews and meta-analyses1. [Last accessed on 17 July 2013]. Available from: http:// whqlibdoc.who.int/publications/2007/9789241595230_eng.pdf .
- 3.Van Rossum CT, Büchner FL, Hoekstra J. Quantification of health effects of breastfeeding: Review of the literature and model simulation: RIVM report 350040001/2005. Bilthoven: RIVM; 2006. [Google Scholar]
- 4.Arenz S, Rückerl R, Koletzko B, von Kries R. Breastfeeding and childhood obesity - A systematic review. Int J Obes Relat Metab Disord. 2004;28:1247–56. doi: 10.1038/sj.ijo.0802758. [DOI] [PubMed] [Google Scholar]
- 5.WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: A pooled analysis [abstract] Lancet. 2000;355:451–5. [PubMed] [Google Scholar]
- 6.Jones G, Stekete RW, Black RE, Bhutta ZA, Morris SS. Bellagio Child Survival Study Group: How many child deaths can we prevent this year.? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 7.Kumar D, Goel NK, Mittal PC, Misra P. Influence of infant-feeding practice on nutritional status of under-five children. Indian J Paediatr. 2006;73:417–22. doi: 10.1007/BF02758565. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics Section of Breastfeeding. Policy statement: Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–41. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 9.Gibney MJ, Elia M, Ljungqvist O, Dowsett J. Ch. 1. 2nd ed. UK: Blackwell; 2006. Clinical Nutrition; p. 2. [Google Scholar]
- 10.Li R, Zhao Z, Mokdad A, Barker L, Grummer- Strawn L. Prevalence of breastfeeding in the United States: The 2001 National Immunization Survey. Pediatrics. 2003;111:1198–201. [PubMed] [Google Scholar]
- 11.Waiswa P, Peterson S, Tomson G, Pariyo GW. Poor newborn care practices- a population based survey in eastern Uganda. BMC Pregnancy Childbirth. 2010;10:9. doi: 10.1186/1471-2393-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cruz Agudo Y, Jones AD, Berti PR, Larrea Macías S. Breastfeeding, complementary feeding practices and childhood malnutrition in the Bolivien Andes. Arch Latinoam Nutr. 2010;60:7–14. [PubMed] [Google Scholar]
- 13.Dibley MJ, Senarath U, Agho KE. Infant and young child feeding indicators across nine East and Southeast Asian countries: An analysis of National Survey Data 2000-2005. Public Health Nutr. 2010;13:1296–303. doi: 10.1017/S1368980010000844. [DOI] [PubMed] [Google Scholar]
- 14.Kimani-Murage EW, Madise NJ, Fotso JC, Kyobutungi C, Mutua MK, Gitau TM, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi, Kenya. BMC Public Health. 2011;11:396. doi: 10.1186/1471-2458-11-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghosh S. A Practical Guide. Delhi: Jaypee Brothers Medical Publishers; 1997. Nutrition and Child Care; pp. 52–3. [Google Scholar]
- 16.Saka AG, Musayeva Erlem M, Ceylan A, Koeturk T. Breast feeding pattern, belief and attitude among Kurdish mothers in Diyarbakir Turky. Acta Pediatr. 2005;94:1303–9. doi: 10.1111/j.1651-2227.2005.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 17.Khasawneta M, Khadu Y, Amarin Z, Alkafeste A. Knowledge, attitude and practices of breastfeeding in the North Jordan. Int Breast Feed J. 2006;23:1–17. doi: 10.1186/1746-4358-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohamed SA, Mohamed AG, Mohamed EM, Khalek EM. Knowledge and practices of working mother about breastfeeding and weaning in Assiut city, Egypt. Life Sci J. 2012;9:803–8. [Google Scholar]
- 19.Chaudhary RN, Shah T, Raja S. Knowledge and practice of mothers regarding breast feeding: A hospital based study. Knowl Pract Breast Feed. 2011;9:194–200. [Google Scholar]
- 20.Walker RB, Conn JA, Davies MJ, Moore VM. Mothers' views on feeding infants around the time of weaning. Public Health Nutr. 2006;9:707–13. doi: 10.1079/phn2005915. [DOI] [PubMed] [Google Scholar]
- 21.Kishore K. Knowledge, Attitude and Practices of weaning among mothers in Gulbarga, MD thesis; Department of Pediatrics, MR Medical College, Gulbarga, Ranjiv Gandhi University of Health Sciences; Karnataka, Bangalore. 2008. pp. 1–71. [Google Scholar]
- 22.Woldegebriel A. Mothers' knowledge and belief on breast feeding. Ethiop Med J. 2002;40:365–74. [PubMed] [Google Scholar]
- 23.Bhardwaj SL, Rathore MS, Paliwal A. A study of breast feeding and neonatal care practices in some ethnic communities in periurban slums at Jaipur, Rajasthan. Anthropologist. 2012;14:459–65. [Google Scholar]
- 24.Yeggamal C, Chitra K. Nutritional state of in-fants of employed and unemployed mothers. Indian J Nutr Diet. 2005;42:47. [Google Scholar]
- 25.Al-Shoshan AA. Factors affecting mother's choices and decisions related to breast feeding practices and weaning habits. Pak J Nutr. 2007;6:318–22. [Google Scholar]
- 26.Webb AL, Sellen DW, Ramakrishnan U, Martorell R. Maternal years of schooling but not academic skills is independently associated with infant-feeding practices in a cohort of rural Guatemalan women. J Hum Lact. 2009;25:297–306. doi: 10.1177/0890334408330449. [DOI] [PMC free article] [PubMed] [Google Scholar]


