Illustration
No objective guidelines exist regarding handling of turbid blood units in developing countries. Therefore, use or discard of such units is decided as per local protocols which are mostly subjective and vary over time. Some of such turbid units are removed by blood centers at the time of preparation when ‘milky appearance’ is very gross, while some are returned by treating doctor at the time of transfusion. Overall, the frequency of lipemic donations ranges between 0.31 and 0.35%,[1] although sporadic reports have highlighted that the frequency might be much higher, up to 13%. Nonetheless, a significant numbers of such blood and plasma units are thus discarded each year.[2]
We came across a highly turbid plasma unit, prepared from a whole blood donation by a 37-year-old first time male donor. Unit was segregated from routine processing as it did not pass the ‘label should be visible’ test used at our center [Figure 1]. Medical history of the donor was reviewed and found to be insignificant. Donor had a weight of 70 kg and a blood pressure of 129/90 mmHg before donation. Serum lipid profile on the donated sample showed a very high triglyceride level of 3,168 mg/dl; cholesterol 358 mg/dl, high density lipoprotein (HDL) 23 mg/dl, and very low density lipoprotein (VLDL) 634 mg/dl. Despite repeated calls donor did not return for further evaluation. As, triglyceride levels were higher than those recommended by the equipment manufacturer for infectious marker (IM) testing (Vitros ECi by Ortho Clinical Diagnostics Inc. USA; enhanced chemilumniscence technique with highest concentration of triglyceride as 3000 mg/dl as acceptable), sample [Figure 2] as well as unit had to be discarded. Also, spot test available with our center (Tridot by J. Mitra and Co., Okhla, New Delhi, India), declared interference/cross reactivity with lipemic serum and thus were not used for IM testing.
Figure 1.

Turbid plasma bag (left) compared to normal plasma unit with visible label
Figure 2.
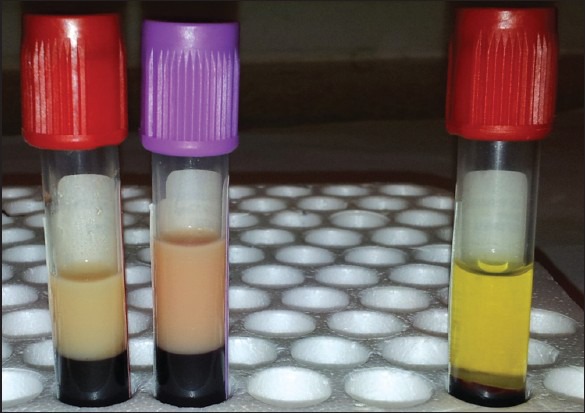
Turbid blood sample from same unit (left) compared to normal blood sample
As shown by Peffer et al., simply having a meal before donation[3] may yield such a turbid unit. On the other hand, highly unfavorable cardiovascular profile[4] and elevated lipid levels may be the cause of such units, requiring further counseling of the donor. Additionally, as highlighted by Vassallo and Stearns, false-negative results on such turbid samples[5] may compromise the blood transfusion safety. Effect on transfusion recipients of such turbid units has not yet been studied in detail and is a gray area with regards to transfusion safety. Bashir and colleagues recently showed that use of such turbid plasma may increase the hemolysis if used for resuspension of red cells for exchange transfusion in neonates.[6]
Thus, the blood donors, the blood center, as well as the transfusion recipient; all are impacted by such turbid donations. Therefore, there is an imminent need to have studies on large sample size with an objective of providing guidelines for blood centres for testing as well as use of these turbid donations for blood transfusion purpose.
Footnotes
Source of Support: Nil
Conflicting Interest: None declared
References
- 1.Lippi G, Franchini M. Lipaemic donations: Truth and consequences. Transfus Apher Sci. 2012 doi: 10.1016/j.transci.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Morish M, Ayob Y, Maim N, Salman H, Muhamad NA, Yusoff NM. Quality indicators for discarding blood in the National Blood Center, Kuala Lumpur. Asian J Transfus Sci. 2012;6:19–23. doi: 10.4103/0973-6247.95045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peffer K, de Kort WL, Slot E, Doggen CJ. Turbid plasma donations in whole blood donors: Fat chance? Transfusion. 2011;51:1179–87. doi: 10.1111/j.1537-2995.2011.03079.x. [DOI] [PubMed] [Google Scholar]
- 4.Bedi R, Basu S, Kaur P, Chattopadhya A. Visual inspection of blood units, a necessary practice at blood centers. Transfusion. 2005;45:459. doi: 10.1111/j.0041-1132.2005.04403.x. [DOI] [PubMed] [Google Scholar]
- 5.Vassallo R, Stearns FM. Lipemic plasma: A renaissance. Transfusion. 2011;51:1136–9. doi: 10.1111/j.1537-2995.2011.03142.x. [DOI] [PubMed] [Google Scholar]
- 6.Bashir S, Wiltshire M, Cardigan R, Thomas S. Lipaemic plasma induces haemolysis in resuspended red cell concentrate. Vox Sang. 2012;104:218–24. doi: 10.1111/j.1423-0410.2012.01660.x. [DOI] [PubMed] [Google Scholar]


