Abstract
Background:
The development of anti-red blood cell antibodies (both allo-and autoantibodies) remains a major problem in thalassemia major patients. We studied the frequency of red blood cell (RBC) alloimmunization and autoimmunization among thalassemia patients who received regular transfusions at our center and analyzed the factors, which may be responsible for development of these antibodies.
Materials and Methods:
The study was carried out on 319 multiply transfused patients with β-thalassemia major registered with thalassemia clinic at our institute. Clinical and transfusion records of all the patients were examined for age of patients, age at initiation of transfusion therapy, total number of blood units transfused, transfusion interval, status of splenectomy or other interventions. Alloantibody screening and identification was done using three cell and 11 cell panel (Diapanel, Bio-rad, Switzerland) respectively. To detect autoantibodies, autocontrol was carried out using polyspecific coombs (IgG + C3d) gel cards.
Results:
Eighteen patients out of total 319 patients (5.64%) developed alloantibodies and 90 (28.2%) developed autoantibodies. Nine out of 18 patients with alloantibodies also had autoantibodies. Age at first transfusion was significantly higher in alloimmunized than non-immunized patients (P = 0.042). Out of 23 alloantibodies, 52.17% belonged to Rh blood group system (Anti-E = 17%, Anti D = 13%, Anti-C = 13%, Anti-Cw = 9%), 35% belonged to Kell blood group system, 9% of Kidd and 4% of Xg blood group system.
Conclusion:
Alloimmunization was detected in 5.64% of multitransfused thalassemia patients. Rh and Kell blood group system antibodies accounted for more than 80% of alloantibodies. This study re-emphasizes the need for RBC antigen typing before first transfusion and issue of antigen matched blood (at least for Rh and Kell antigen). Early institution of transfusion therapy after diagnosis is another means of decreasing alloimmunization.
Keywords: Alloimmunization, autoimmunization, thalassemia major, transfusion
Introduction
Thalassemia is a congenital hemolytic disorder, caused by a partial or complete defect in α or β globin chain synthesis. Thalassemia is considered as the most common genetic disorder world-wide with a particularly high frequency in a broad belt, extending from the Mediterranean basin through the Middle East (Iran), India and Southeast Asia.[1] In the absence of stem cell transplantation, the disease is treated by life-long red blood cell (RBC) transfusion[2] to keep the hemoglobin (Hb) level between 9 and 11.5 g/dL. The development of anti-RBC antibodies (both allo-and autoantibodies) remains a major problem. The development of alloantibodies and/or autoantibodies against RBC antigens complicate RBC crossmatching, shortens in vivo survival of transfused cells, delays provision of safe transfusions and may accelerate tissue iron loading.[3,4] The literature reports various frequencies of alloimmunization depending on the homogeneity of the donor - recipient population, RBC phenotype matching policy and age at transfusion initiation. Reported alloimmunization rates ranged from 4% to 50% in thalassemia and were lower in more homogenous populations.[2,5,6,7] Some alloantibodies are hemolytic and may cause, though not invariably, hemolytic transfusion reactions, others are clinically insignificant. Erythrocyte autoantibodies appear less frequently, but they can result in clinical hemolysis and in difficulty in cross-matching blood. Patients with autoantibodies may have a higher transfusion rate and often require immunosuppressive drugs, splenectomy, or alternative treatments.[8,9] Approaches for prevention of alloimmunization are under debate. They range from the provision of RBCs matched for all the major antigens associated with clinically significant antibodies to blood matched only for antibodies that have already been made. Reasons for controversy regarding following the best approach lay in the fact that many alloantibodies are not harmful and expensive prevention methods may therefore benefit only some patients.[10,11,12] In addition, donor feasibility and the cost of RBC matching affects the approach of individual medical centers. There is limited data on the RBC phenotypes and the extent of alloimmunization among Asians. We studied the frequency of RBC alloimmunization and autoimmunization among thalassemia patients who received regular transfusions at our center and analyzed the factors, which may be responsible for development of these antibodies.
Materials and Methods
The study was carried out on 319 multiply transfused patients with β-thalassemia major registered with thalassemia clinic at our institute. Study was conducted from October 2009 to April 2010. Informed consent was obtained from patients or their parents. Clinical and transfusion records of all the patients were examined for age of patients, age at diagnosis and initiation of transfusion therapy, total number of blood units transfused, transfusion interval, status of splenectomy or other interventions.
Transfusion protocol
All thalassemics were transfused according to institutional transfusion policy to keep target Hb level 9-11.5 g/dl with a transfusion interval of 2-4 weeks. All patients were transfused with ABO and Rh(D) matched, crossmatch compatible blood. In case patient was detected to have alloantibodies, antigen matched crossmatch compatible blood was issued to the patient.
Antibody detection
A volume of 2 ml blood was drawn into an ethylene diamine tetraacetate containing tube, centrifuged at 3000 ×g for 3 min to obtain plasma (for crossmatch and antibody screening) and red cells (for detection of autoantibodies) on micro-column agglutination system (Bio-rad, Switzerland). Alloantibody screening was performed using 3 cell screening panel (Diacell, Bio-rad, Switzerland). All alloantibody screening positive samples were investigated to identify the antibody specificity. Antibody specificity detection was performed using a commercial 11 cell identification panel (Diapanel, Bio-rad, Cressier sur Morat, Switzerland). Autoantibodies were detected by incubating patient's own cell with patient's plasma at 37°C for 15 min and then centrifuging for 10 min on gel card containing polyspecific antihuman globulin (anti IgG + C3d).
Statistical analysis
Analysis was conducted using SPSS for Windows (version 15.0; SPSS Inc., Chicago, IL, USA). Discrete categorical data were presented as n (%). Continuous data were given as mean standard deviation. Mann-Whitney U-test was used for statistical analysis of continuous variables. For categorical data, comparisons were made by Pearson Chi-square test or Fisher's exact test as appropriate. All statistical tests were two-sided and performed at a significance level of α = 0.05.
Results
The study included a total of 319 (235 male and 84 female) thalassemia major patients. The age of the patients ranged from 1.5 to 27 years with a mean age of 15.18 years. Eighteen patients out of total 319 patients (5.64%) developed alloantibodies and 90 (28.2%) developed autoantibodies. Nine out of 18 patients with alloantibodies also had autoantibodies. Difference between mean age among alloimmunized and non-alloimmunized was not statistically significant. Mean age of patients developing autoantibodies was 18.35 years, which is significantly higher (P = 0.001) than the patients without the presence of autoantibodies (13.93 years). There was no statistically significant gender difference for the development of allo and autoantibodies. Age at first transfusion was significantly higher in alloimmunized (23.28 months) than non-immunized patients (14.43 months) (P = 0.042). Total transfusions received by patients were not correlating with development of alloantibodies, but development of autoantibodies was statistically significant (P = 0.01) with increased numbers of transfusion [Table 1].
Table 1.
Frequency of alloantibodies and autoantibodies in patient's population in relation to mean age of patient, age at fi rst transfusion and total number of transfusions
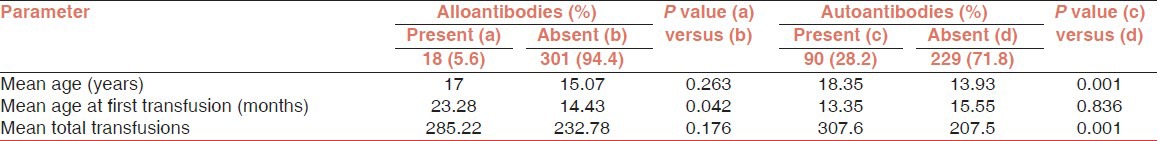
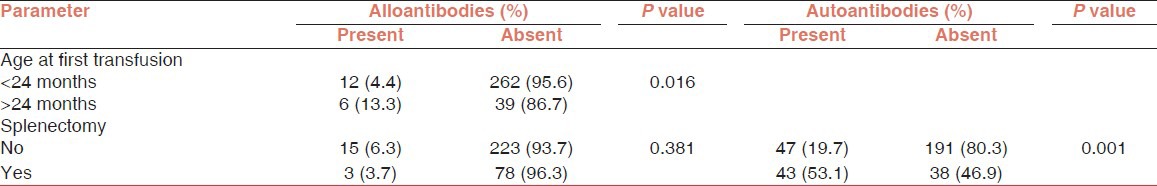
It was observed that patients who received their first transfusion before 24 months of age had significantly lower prevalence of alloantibodies (P = 0.016).
Of the 319 patients, 90 (28.2%) developed autoantibodies as determined by positive autocontrol on gel card (IgG + C3d). Patients who had undergone splenectomy had significantly higher prevalence of autoantibodies [Table 2]. Specificity of these antibodies as IgG or C3d was not determined in the study however reaction strength of these autoantibodies varied from weak (wk) to 2+ in most of the cases and these antibodies were not interfering with compatibility testing in most cases.
Table 2.
Frequency of alloantibodies and autoantibodies in patient's population in relation to age at fi rst transfusion (less than or more than 24 months) and status of splenectomy
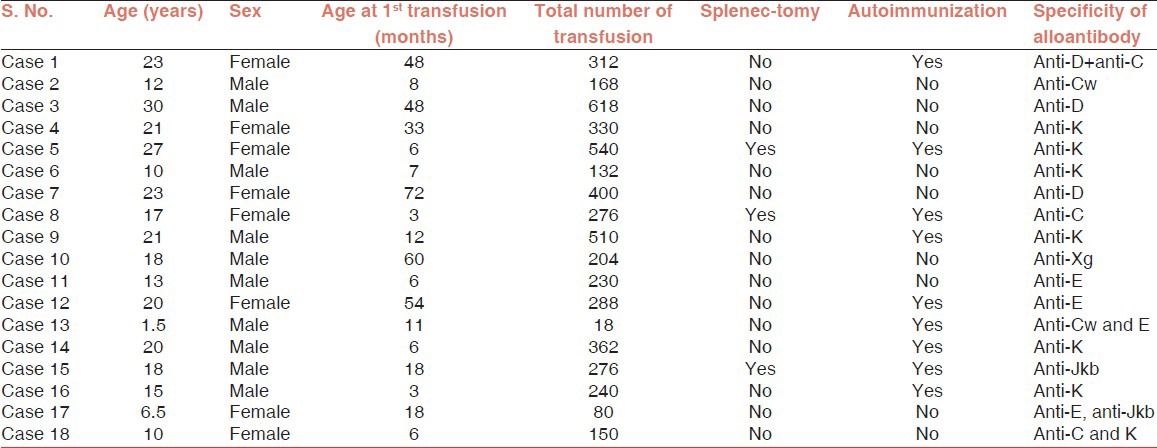
Eighteen patients out of total 319 patients (5.64%) developed alloantibodies. A total of 23 alloantibodies were identified in patient population [Figure 1]. Out of 23 alloantibodies, 52.17% belonged to Rh blood group system (Anti-E = 17%, Anti D = 13%, Anti-C = 13%, Anti-Cw = 9%), 35% belonged to Kell blood group system, 9% of Kidd and 4% of Xg blood group system. Fourteen patients (78%) developed single antibody while 4 (22%) patients developed dual alloantibody. All patients who developed dual antibodies were having at least one antibody belonging to Rh blood group system. Data of patients developing alloantibodies is as shown in Table 3.
Figure 1.
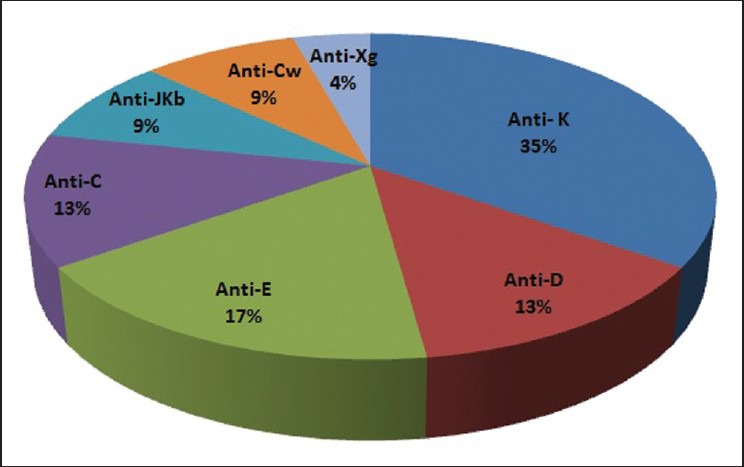
Distribution of alloantibodies in alloimmunised patients
Table 3.
Details of patients who developed alloantibodies
Discussion
Alloimmunization to red cell antigens is an immune response usually stimulated by the transfusion of blood products and is one of the complications of RBC transfusions. Other than RBC alloimmunization, immunologic complications of repeated RBC transfusions include: Difficulties obtaining compatible blood, development of autoantibodies, acute or delayed hemolytic transfusion reactions and hemolytic disease of the newborn.[13]
The factors for alloimmunization are complex and involve at least three main contributing elements: (1) the RBC antigenic difference between the blood donor and the recipient; (2) the recipient's immune status; (3) the immunomodulatory effect of the allogeneic blood transfusions on the recipient's immune system.[6] Overall rate of alloimmunization was 5.64% in our study.
The previous studies have reported quite variable rate of alloimmunization ranging from 3.1% to 37% in patients of different ethnic origin [Table 4]. A low rate of alloimmunization may be expected when there is homogeneity of RBC antigens between the blood donors and recipients.[6] At our center, most of our patients and blood donor population is from Chandigarh and adjoining area of states of Punjab and Haryana. This homogeneity between the patient and blood donors population may be the reason of low rate of alloimmunization in our study.
Table 4.
Alloimmunization rates in thalassemia patient in India and world

In our study, rate of alloimmunization was lower in patients who received their first transfusion at <2 years of age (P = 0.016). It has been previously shown that alloimmunization risk was significantly lower in hemoglobinopathy patients who started transfusion therapy at a very young age (<3 years) compared with those who started later in life, where an immature immune system and some form of the acquired immune tolerance to allogeneic RBC antigens is held responsible for the reduced alloimmunization risk.[3,14,22,23]
We did not find any association of gender (male/female) with rate of alloimmunization. In literature, the studies of Ameen et al.,[16] El Danasoury et al.[24] and Hendrickson et al.[25] showed that gender was not a significant factor in the development of alloimmunization. However, Reisner et al.[26] reported a significant association between alloimmunization and gender, as they found alloimmunization to be associated more with female patients while on the other hand Saied et al.[27] found more association in male patients.
The relationship between the number of units transfused and alloimmunization is unknown in thalassemia.[28] However, some of the studies reported that alloimmunization is more likely in patients who receive more units of blood.[12,22] Schonewille et al.,[29] Saied et al.[27] and Ahmed et al.[30] found no significant association between alloantibodies and autoantibodies formation and the number of transfused packed RBCs.
In our study, there was no significant difference between patients developing alloimmunization (P = 0.117) with respect to the number of transfusions, but development of autoantibodies was significantly higher in patients receiving more number of transfusions (P = 0.001).
In the present study, the most frequently detected alloantibodies belonged to Rh blood group system (52.17%). Individually, most frequent alloantibodies were anti-Kell (35%) and anti-E (17%).
These findings were in accordance with most of the reported studies, which found that anti-Kell, anti-E and anti-D being the most frequent antibodies in these patients.[1,2,6,16,19,27,30] However, no anti-Kell antibodies were reported by Pradhan et al.,[15] (Mumbai, India) in their study on thalassemia patients.
In the present study, 90 (28.2%) patients developed autoantibodies. Previously Singer et al.[6] and Ameen et al.[16] reported 25% and 11% rate of autoimmunization in thalassemia patients respectively. It is known that splenectomized patients are more prone to autoimmunization.[6,31] In our study, out of 90 auto positive patients 43 (53.1%) had undergone splenectomy (P = 0.001). Possible explanation for this is that lymphocytosis associated with blood transfusion is also associated with elevated levels of serum immunoglobulins, immune complexes and cells expressing surface immunoglobulins,[31,32,33] suggesting the possible role of absence of spleen and autoantibody formation. In our study, these antibodies were not interfering with compatibility testing in most cases and were not associated with increased destruction of RBCs in these patients. The clinical importance of autoantibodies in multi-transfused patients is debatable. Although some reports found the existence of warm autoantibodies to be associated with clinically significant hemolysis[34] others did not find this to be always the case.[35]
Conclusion
Alloimmunization was detected in 5.64% of multitransfused thalassemia patients. Rh and Kell blood group system antibodies accounted for more than 80% of alloantibodies. This study re-emphasizes the need for RBC antigen typing before first transfusion and issue of antigen matched blood (at least for Rh and Kell antigen). Early institution of transfusion therapy after diagnosis is another means of decreasing alloimmunization. Regular antibody screening for already alloimmunized patients to check for the disappearance of old antibodies or development of new alloantibody. These measures will help in decreasing the incidence of RBC alloimmunization and delayed hemolytic transfusion reactions in these patients.
Footnotes
Source of Support: Nil
Conflicting Interest: None declared
References
- 1.Sadeghian MH, Keramati MR, Badiei Z, Ravarian M, Ayatollahi H, Rafatpanah H, et al. Alloimmunization among transfusion-dependent thalassemia patients. Asian J Transfus Sci. 2009;3:95–8. doi: 10.4103/0973-6247.53884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang LY, Liang DC, Liu HC, Chang FC, Wang CL, Chan YS, et al. Alloimmunization among patients with transfusion-dependent thalassemia in Taiwan. Transfus Med. 2006;16:200–3. doi: 10.1111/j.1365-3148.2006.00656.x. [DOI] [PubMed] [Google Scholar]
- 3.Charache S. Problems in transfusion therapy. N Engl J Med. 1990;322:1666–8. doi: 10.1056/NEJM199006073222309. [DOI] [PubMed] [Google Scholar]
- 4.Higgins JM, Sloan SR. Stochastic modeling of human RBC alloimmunization: Evidence for a distinct population of immunologic responders. Blood. 2008;112:2546–53. doi: 10.1182/blood-2008-03-146415. [DOI] [PubMed] [Google Scholar]
- 5.Sirchia G, Zanella A, Parravicini A, Morelati F, Rebulla P, Masera G. Red cell alloantibodies in thalassemia major. Results of an Italian cooperative study. Transfusion. 1985;25:110–2. doi: 10.1046/j.1537-2995.1985.25285169198.x. [DOI] [PubMed] [Google Scholar]
- 6.Singer ST, Wu V, Mignacca R, Kuypers FA, Morel P, Vichinsky EP. Alloimmunization and erythrocyte autoimmunization in transfusion-dependent thalassemia patients of predominantly Asian descent. Blood. 2000;96:3369–73. [PubMed] [Google Scholar]
- 7.Pahuja S, Pujani M, Gupta SK, Chandra J, Jain M. Alloimmunization and red cell autoimmunization in multitransfused thalassemics of Indian origin. Hematology. 2010;15:174–7. doi: 10.1179/102453309X12583347114013. [DOI] [PubMed] [Google Scholar]
- 8.Kruatrachue M, Sirisinha S, Pacharee P, Chandarayingyong D, Wasi P. An association between thalassaemia and autoimmune haemolytic anaemia (AIHA) Scand J Haematol. 1980;25:259–63. doi: 10.1111/j.1600-0609.1981.tb01398.x. [DOI] [PubMed] [Google Scholar]
- 9.Argiolu F, Diana G, Arnone M, Batzella MG, Piras P, Cao A. High-dose intravenous immunoglobulin in the management of autoimmune hemolytic anemia complicating thalassemia major. Acta Haematol. 1990;83:65–8. doi: 10.1159/000205170. [DOI] [PubMed] [Google Scholar]
- 10.Ness PM, Shirey RS, Thoman SK, Buck SA. The differentiation of delayed serologic and delayed hemolytic transfusion reactions: Incidence, long-term serologic findings, and clinical significance. Transfusion. 1990;30:688–93. doi: 10.1046/j.1537-2995.1990.30891020325.x. [DOI] [PubMed] [Google Scholar]
- 11.Ness PM. To match or not to match: The question for chronically transfused patients with sickle cell anemia. Transfusion. 1994;34:558–60. doi: 10.1046/j.1537-2995.1994.34794330007.x. [DOI] [PubMed] [Google Scholar]
- 12.Fluit CR, Kunst VA, Drenthe-Schonk AM. Incidence of red cell antibodies after multiple blood transfusion. Transfusion. 1990;30:532–5. doi: 10.1046/j.1537-2995.1990.30690333485.x. [DOI] [PubMed] [Google Scholar]
- 13.Moreira Júnior G, Bordin JO, Kuroda A, Kerbauy J. Red blood cell alloimmunization in sickle cell disease: The influence of racial and antigenic pattern differences between donors and recipients in Brazil. Am J Hematol. 1996;52:197–200. doi: 10.1002/(SICI)1096-8652(199607)52:3<197::AID-AJH11>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 14.Spanos T, Karageorga M, Ladis V, Peristeri J, Hatziliami A, Kattamis C. Red cell alloantibodies in patients with thalassemia. Vox Sang. 1990;58:50–5. doi: 10.1111/j.1423-0410.1990.tb02055.x. [DOI] [PubMed] [Google Scholar]
- 15.Pradhan V, Badakere S, Vasantha K, Korgaonkar S, Panjwani S, Jajoo N. Antibodies to red cells in beta thalassemia major patients recieving multiple transfusions: A short report. Indian J Hematol Blood Transfus. 2001;19:100–1. [Google Scholar]
- 16.Ameen R, Al-Shemmari S, Al-Humood S, Chowdhury RI, Al-Eyaadi O, Al-Bashir A. RBC alloimmunization and autoimmunization among transfusion-dependent Arab thalassemia patients. Transfusion. 2003;43:1604–10. doi: 10.1046/j.1537-2995.2003.00549.x. [DOI] [PubMed] [Google Scholar]
- 17.Karimi M, Nikrooz P, Kashef S, Jamalian N, Davatolhagh Z. RBC alloimmunization in blood transfusion-dependent beta-thalassemia patients in southern Iran. Int J Lab Hematol. 2007;29:321–6. doi: 10.1111/j.1365-2257.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 18.Bhatti FA, Salamat N, Nadeem A, Shabbir N. Red cell immunization in beta thalassaemia major. J Coll Physicians Surg Pak. 2004;14:657–60. [PubMed] [Google Scholar]
- 19.Noor Haslina MN, Ariffin N, Illuni Hayati I, Rosline H. Red cell immunization in multiply transfused Malay thalassemic patients. Southeast Asian J Trop Med Public Health. 2006;37:1015–20. [PubMed] [Google Scholar]
- 20.Gupta R, Singh DK, Singh B, Rusia U. Alloimmunization to red cells in thalassemics: Emerging problem and future strategies. Transfus Apher Sci. 2011;45:167–70. doi: 10.1016/j.transci.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Chao YH, Wu KH, Lu JJ, Shih MC, Peng CT, Chang CW. Red blood cell alloimmunisation among Chinese patients with β-thalassaemia major in Taiwan. Blood Transfus. 2013;11:71–4. doi: 10.2450/2012.0153-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosse WF, Gallagher D, Kinney TR, Castro O, Dosik H, Moohr J, et al. Transfusion and alloimmunization in sickle cell disease. The Cooperative Study of Sickle Cell Disease. Blood. 1990;76:1431–7. [PubMed] [Google Scholar]
- 23.Poole J, Daniels G. Blood group antibodies and their significance in transfusion medicine. Transfus Med Rev. 2007;21:58–71. doi: 10.1016/j.tmrv.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 24.El Danasoury AS, Eissa DG, Abdo RM, Elalfy MS. Red blood cell alloimmunization in transfusion-dependent Egyptian patients with thalassemia in a limited donor exposure program. Transfusion. 2012;52:43–7. doi: 10.1111/j.1537-2995.2011.03234.x. [DOI] [PubMed] [Google Scholar]
- 25.Hendrickson JE, Desmarets M, Deshpande SS, Chadwick TE, Hillyer CD, Roback JD, et al. Recipient inflammation affects the frequency and magnitude of immunization to transfused red blood cells. Transfusion. 2006;46:1526–36. doi: 10.1111/j.1537-2995.2006.00946.x. [DOI] [PubMed] [Google Scholar]
- 26.Reisner EG, Kostyu DD, Phillips G, Walker C, Dawson DV. Alloantibody responses in multiply transfused sickle cell patients. Tissue Antigens. 1987;30:161–6. doi: 10.1111/j.1399-0039.1987.tb01615.x. [DOI] [PubMed] [Google Scholar]
- 27.Saied DA, Kaddah AM, Badr Eldin RM, Mohaseb SS. Alloimmunization and erythrocyte autoimmunization in transfusion-dependent Egyptian thalassemic patients. J Pediatr Hematol Oncol. 2011;33:409–14. doi: 10.1097/MPH.0b013e3182208154. [DOI] [PubMed] [Google Scholar]
- 28.Shamsian BS, Arzanian MT, Shamshiri AR, Alavi S, Khojasteh O. Frequency of red cell alloimmunization in patients with b-major thalassemia in an Iranian referral hospital. Iran J Pediatr. 2008;18:149–53. [Google Scholar]
- 29.Schonewille H, van de Watering LM, Loomans DS, Brand A. Red blood cell alloantibodies after transfusion: Factors influencing incidence and specificity. Transfusion. 2006;46:250–6. doi: 10.1111/j.1537-2995.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 30.Ahmed AM, Hasan NS, Ragab SH, Habib SA, Emara NA, Aly AA. Red cell alloimmunization and autoantibodies in Egyptian transfusion-dependent thalassaemia patients. Arch Med Sci. 2010;6:592–8. doi: 10.5114/aoms.2010.14473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hodge G, Lloyd JV, Hodge S, Story C, Han P. Functional lymphocyte immunophenotypes observed in thalassaemia and haemophilia patients receiving current blood product preparations. Br J Haematol. 1999;105:817–25. doi: 10.1046/j.1365-2141.1999.01385.x. [DOI] [PubMed] [Google Scholar]
- 32.Smit Sibinga CT. Immune effects of blood transfusion. Curr Opin Hematol. 1999;6:442–5. doi: 10.1097/00062752-199911000-00016. [DOI] [PubMed] [Google Scholar]
- 33.Ghio M, Contini P, Mazzei C, Brenci S, Barberis G, Filaci G, et al. Soluble HLA class I, HLA class II, and Fas ligand in blood components: A possible key to explain the immunomodulatory effects of allogeneic blood transfusions. Blood. 1999;93:1770–7. [PubMed] [Google Scholar]
- 34.Aygun B, Padmanabhan S, Paley C, Chandrasekaran V. Clinical significance of RBC alloantibodies and autoantibodies in sickle cell patients who received transfusions. Transfusion. 2002;42:37–43. doi: 10.1046/j.1537-2995.2002.00007.x. [DOI] [PubMed] [Google Scholar]
- 35.Castellino SM, Combs MR, Zimmerman SA, Issitt PD, Ware RE. Erythrocyte autoantibodies in paediatric patients with sickle cell disease receiving transfusion therapy: Frequency, characteristics and significance. Br J Haematol. 1999;104:189–94. doi: 10.1046/j.1365-2141.1999.01127.x. [DOI] [PubMed] [Google Scholar]


