Abstract
Importance
Young adults have high levels of behavioral health needs but often lack health insurance. Recent health reforms have increased coverage, but it is unclear how use of hospital-based care changed after expanding insurance.
Objective
To evaluate the association between health insurance coverage expansions and use of hospital-based care among young adults with behavioral health diagnoses.
Design
Quasi-experimental analyses of hospital inpatient and emergency department use from 2003–2009 based on hospital discharge data, comparing differential changes in service use among young adults with behavioral health diagnoses in Massachusetts versus other states before and after Massachusetts’ 2006 health reform.
Setting
Hospital inpatient departments in the U.S. and emergency departments in Massachusetts and Maryland.
Participants
Population-based sample of inpatient admissions (n=12,821,746 across 7 years) nationwide and emergency department visits (n=6,756,303 across 7 years) from Maryland and Massachusetts for 12 to 25 year olds.
Main Outcomes and Measures
Inpatient admission rates per 1000 population for primary diagnosis of any behavioral health disorder, by diagnosis; emergency department visit rates per 1000 population by behavioral health diagnosis; and insurance coverage for discharges.
Results
After 2006, uninsurance among 19 to 25 year olds in Massachusetts fell from 26% to 10% (16 percentage points; 95% CI, 13–20). Young adults experienced relative declines in inpatient admission rates of 2.0 per 1000 for primary diagnoses of any behavioral health disorder (95% CI, 0.88–3.1), 0.38 for depression (95% CI, 0.18–0.58), and 1.3 for substance use disorder (95% CI, 0.68–1.8). The rise in emergency department visits with any behavioral health diagnosis after 2006 was lower among young adults in Massachusetts compared to Maryland (16.5 per 1000; 95% CI, 11.4–21.6). Among young adults in Massachusetts, the percent of behavioral health discharges that were uninsured fell by 5.0 (95% CI, 3.0–7.2) percentage points in inpatient settings and 5.0 (95% CI, 1.7–7.8) percentage points in emergency departments, relative to other states.
Conclusions and Relevance
Expanded health insurance coverage for young adults was not associated with large increases in hospital-based care for behavioral health, but it increased financial protection to young adults with behavioral health diagnoses, and to the hospitals that care for them.
The coverage and financing of health care services for individuals with mental illness and substance use disorders are changing rapidly in the U.S. The 2008 Federal parity legislation requires that insurance benefit design and management for mental health and substance abuse treatment match those for medical and surgical services. The 2010 Patient Protection and Affordable Care Act (PPACA), with coverage provisions mirroring Massachusetts’ 2006 health reform,1 expands health insurance coverage to populations with high behavioral health needs through Medicaid expansions,2,3 establishes health insurance exchanges to ease purchase of individual and small group health insurance, and requires that insurers permit dependent children to remain on parental insurance policies to age 26. Furthermore, PPACA requires health plans offered through new insurance exchanges to cover mental health and substance abuse treatment, and other PPACA reforms integrate care across settings for behavioral health treatment.4
Most behavioral health disorders, 75%, emerge by age 24,5 and the odds of having a 12-month DSM IV disorder are higher for individuals age 18 to 29 than any other adult age group.6 Despite the long-term mortality, disability, and labor market consequences of these disorders,7,8 young adults lack health insurance coverage more often than other age groups.9 The lack of coverage is particularly important for young adults in foster care, child Supplemental Security Income recipients, and Medicaid recipients, for whom the 18th birthday coincides with a loss of benefits.10,11
In outpatient settings, demand for behavioral health treatment is more responsive to insurance coverage and patient cost sharing than other health care services, suggesting that hospital-based services may rise in response to increased insurance coverage.12,13 Alternatively, hospital-based services may fall with increased insurance coverage either because outpatient care use substitutes for inpatient care, or due to utilization management of managed behavioral health organizations responsible for new enrollees.14 Little is known about behavioral health service use when young adults acquire coverage.
In this paper, we study the experience of the Massachusetts health reform to examine inpatient hospital admissions and emergency department visits for young adults aged 19 to 25 diagnosed with behavioral health disorders. To understand how utilization of hospital-based care, and insurance coverage for such care changed following health insurance coverage expansion, we compared inpatient admissions before and after 2006 in Massachusetts to the rest of the US. We further compared these differences among the 19 to 25 year olds to differences among adolescents aged 12 to 18 in Massachusetts, for whom insurance coverage changed less after health reform.15 To examine changes in emergency department (ED) visits, we use a similar approach, focusing on the universe of ED visits in Massachusetts and Maryland. We estimated the net effect of opposing influences of insurance coverage on hospital-based behavioral health services against a null hypothesis that service use would not change after coverage expanded.
METHODS
Study Population
To analyze hospital-based care for behavioral health disorders, we assembled four sources of hospital discharge records from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.16 The 2003–2009 Nationwide Inpatient Samples (NIS) provided records of inpatient admissions from annual random samples of 20% of U.S. hospitals. With sample weights, the data represent U.S. inpatient admissions. Second, we used the universe of discharge records from Massachusetts (State Inpatient Database), and thus we excluded Massachusetts from NIS estimates. Finally, for ED visits, we used the two State Emergency Department Datasets from Massachusetts and Maryland. National data on ED visits do not exist before 2006. Of the subset of states with ED data before 2006, we chose Maryland because it was most similar to Massachusetts in size, geography, pre-reform uninsurance rates among young adults, and like Massachusetts, Maryland has more mental health providers than average.17,18 To focus on the set of discharges most likely affected by coverage expansions, we present results from non-birth discharges only (eTable 1), although estimated effects are similar without this exclusion.
From 12,921,828 non-birth inpatient admission records among 12 to 25 year olds, we excluded records missing information on sex (n=58,352), diagnosis (n=6,179), or payment source (n=38,431), leaving 12,818,866 admissions for any diagnosis. From 6,893,810 non-birth ED visit records among 12 to 25 year olds, we excluded observations missing information on sex (n=711), diagnosis (n=7,266) or payment source (n=81,426), leaving a total of 6,804,407 ED visits for any diagnosis.
To calculate population-based estimates of health insurance rates by single year of age, state of residence, and calendar year, we analyzed the Bureau of Labor Statistics’ 2004–2010 Current Population Survey Annual Social and Economic Supplements (CPS). Consent was waived for our study of secondary data, reviewed and deemed exempt by Dartmouth College’s Committee for the Protection of Human Subjects.
Study Variables
We classified CPS respondents reporting no health insurance coverage at any time in the prior calendar year as uninsured.
Inpatient outcomes included admission rates for: any reason, any primary diagnosis for behavioral health, and separately for primary diagnoses of depression, psychoses/schizophrenia, substance use disorders, and all other behavioral health disorders (eTable 1). We expressed admissions as rates per 1000 population in a given age, sex, “state” (Massachusetts vs. other), and year cell. Because the NIS samples different hospitals within each state in every year, we pooled “other” states to mitigate the effects of annual entry or exit of sample hospitals. Numerators were based on total admissions in a given cell, for each outcome. Denominators were computed from Census Bureau population estimates19 to form rates for each of the 392 cells defined by 14 single years of age (12–25) × 7 years × 2 sexes × 2 “states.”
Other outcomes, also measured for each age, year, sex, and state cell, included mean length of hospital stay in days, share of admissions with comorbid diagnoses of depression, psychoses, or substance use disorders (excluding admissions for primary diagnoses of depression, psychoses, or substance use disorders, respectively), and share of admissions by insurance status. Insurance status is based on payment source, including: uninsured (“self-pay”), Medicaid, private, or Commonwealth Care, subsidized coverage from Massachusetts’ health insurance exchange.
Outcomes for ED visits were similar, but reflect the presence of any behavioral health diagnosis since no primary diagnosis is available. We created six mutually exclusive diagnosis categories: depression only, psychosis only, substance use disorder only, substance use disorder and any mental illness, more than one mental illness, and all other behavioral health (eTable1), where “only” indicates the absence of other behavioral health diagnoses for that visit. Available in Massachusetts only, we calculated the share of visits leading to inpatient admission.
Statistical Analysis
Our analysis estimates the effects of expanding insurance on hospital-based care for young adults with behavioral health diagnoses, using a difference-in-difference-in-difference study design, common in related studies.20,21 We estimate changes in inpatient admissions and ED visits before and after the health reform while controlling for overall trends in hospital-based services for young adults with behavioral health diagnoses during the same period and controlling for existing trends in hospital-based services for behavioral health diagnoses in Massachusetts.
For each outcome, we estimated the following linear regression model separately for each diagnosis category:
E(Yikts) = β0 + β1 MAs + agei + yeart + femalek+ β2(age19to25i × aftert) + β3(age19to25i × MAs) + β4(aftert × MAs) + β5(age 19 to 25i × aftert × MAs),
where Yikts=admissions or visits per 1000 population for age i sex k, year t, and state s, agei is a set of 13 indicator variables, yeart is a set of 6 indicator variables. We created three two way interaction terms between the variables MAs (= 1 in Massachusetts, and 0 otherwise) aftert, (= 1 in years 2007–2009 and 0 otherwise), and “age 19 to 25i” (= 1 for age 19–25 rates and 0 otherwise) along with the triple interaction between the three variables. The coefficient, β5, yields our estimate of interest, the differential change in admissions per 1000 for 19 to 25 year olds relative to 12 to 18 year olds in Massachusetts versus other states after health reform. Negative estimates of β5 indicate that admissions or ED visits for 19 to 25 year olds in Massachusetts fell relative to other age groups and states after health reform, or in cases of rising utilization, increased less relative to other groups. We report the estimated coefficient, β5, and 95% confidence intervals based on robust Huber-White estimated standard errors. P-values are based on 2-sided tests of statistical significance, defined as P<.05. Analyses were conducted using SAS 9.3 and Stata 11.2.
Results
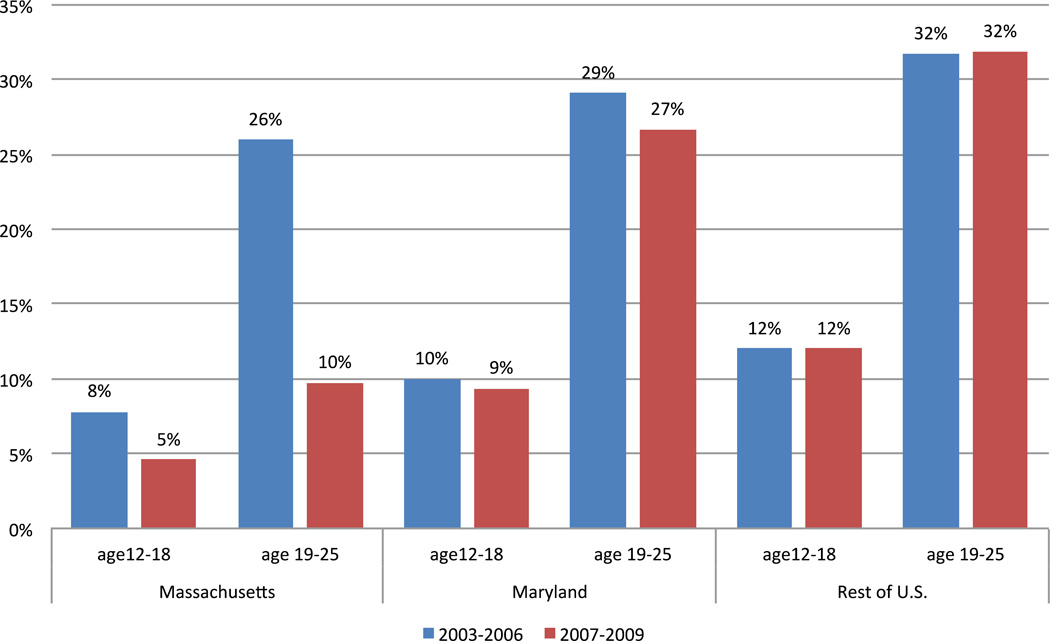
Figure 1 confirms prior evidence15 that the Massachusetts health reform led to a dramatic decline in uninsurance rates for young adults in Massachusetts compared to other states and age groups. Among 19 to 25 year olds in Massachusetts, uninsurance rates fell from 26% to 10% (16 percentage points; 95% CI, 13–20) after health reform.
Figure 1.
Percent of Population Uninsured
Primary behavioral health diagnoses accounted for 49,889 non-birth inpatient admissions for 19 to 25 year olds in Massachusetts over our study period, or 28% of inpatient admissions in this age group, compared with 16% for the rest of the US (Table 1). Notably, the number of inpatient admissions fell over time for total admissions and admissions with primary behavioral health diagnoses. Finally, as inpatient admissions with primary diagnoses of behavioral health disorders fell after 2006, there was a statistically insignificant increase in the share of admissions with secondary diagnoses of psychoses, depression, or substance use disorders.
Table 1.
Inpatient admission characteristics
| Inpatient admissions | Age 19 to 25 Massachusetts |
Rest of U.S. | Age 12 to 18 Massachusetts |
Rest of U.S. | ||||
|---|---|---|---|---|---|---|---|---|
| 2003–06 | 2007–09 | 2003–06 | 2007–09 | 2003–06 | 2007–09 | 2003–06 | 2007–09 | |
| # by primary diagnosis | ||||||||
| All diagnosesa | 99,809 | 77,481 | 4,328,324 | 3,294,235 | 63,464 | 49,087 | 2,893,370 | 2,015,977 |
| Any behavioral health | 28,341 | 20,548 | 651,087 | 554,432 | 12,559 | 10,288 | 489,763 | 378,904 |
| Depression | 3,638 | 2,770 | 126,296 | 102,725 | 2,221 | 1,974 | 117,352 | 82,635 |
| Psychoses | 5,669 | 5,789 | 193,462 | 181,833 | 2,653 | 3,571 | 84,553 | 101,513 |
| Substance use disorder | 11,306 | 6,600 | 109,434 | 97,584 | 1,101 | 551 | 29,220 | 20,925 |
| Other behavioral health | 7,728 | 5,389 | 221,894 | 172,290 | 6,584 | 4,192 | 258,638 | 173,831 |
| Admission rateb (SD) for: | ||||||||
| All diagnosesa | 41 (3.8) | 40 (4.2) | 38 (11) | 38 (9.1) | 25 (6.1) | 26 (5.8) | 25 (6.9) | 23 (5.9) |
| Any behavioral health | 12 (2.6) | 11 (1.8) | 5.8 (1.1) | 6.3 (0.8) | 5.1 (2.1) | 5.5 (1.8) | 4.2 (1.5) | 4.3 (1.3) |
| Depression | 1.5 (0.4) | 1.4 (0.3) | 1.6 (.47) | 1.2 (0.3) | 1.5 (.96) | 1.5 (.82) | 1.0 (0.6) | 0.9 (0.5) |
| Psychoses | 2.3 (0.9) | 1.7 (0.6) | 1.7 (.62) | 2.1 (0.6) | 1.1 (.43) | 1.9 (.55) | 0.7 (0.3) | 1.1 (0.4) |
| Substance use disorder | 4.7 (1.9) | 3.4 (1.3) | 1.0 (.34) | 1.1 (0.3) | 0.4 (.63) | 0.3 (.39) | 0.3 (.23) | 0.2 (0.2) |
| Other behavioral health | 3.2 (0.5) | 2.8 (.36) | 2.0 (0.4) | 2.0 (0.3) | 2.0 (.67) | 1.8 (.49) | 2.2 (0.8) | 2.0 (0.6) |
| Mean length of stay (days) | 4.6 | 4.4 | 4.2 | 4.3 | 5.5 | 5.2 | 4.3 | 4.5 |
| % of admissions paid by | ||||||||
| Medicaid | 26 | 30 | 33 | 33 | 25 | 28 | 36 | 38 |
| Private insurancec | 42 | 45 | 39 | 37 | 69 | 68 | 54 | 52 |
| Commcarec | 0.02 | 4.1 | - | - | 0.03 | 0.2 | - | - |
| Other | 8.7 | 9.3 | 10 | 11 | 2.3 | 2.3 | 5.2 | 5.1 |
| Uninsured | 23 | 12 | 18 | 19 | 4.0 | 1.7 | 5.4 | 5.3 |
| % female | 53 | 53 | 60 | 58 | 52 | 51 | 52 | 52 |
| % of admissions with any | ||||||||
| Psychoses | 3.6 | 5.9 | 2.6 | 4.2 | 3.3 | 5.0 | 2.0 | 3.6 |
| Depression | 8.0 | 9.2 | 5.7 | 6.6 | 5.7 | 5.2 | 4.7 | 4.8 |
| Substance Use Disorder | 21 | 26 | 21 | 25 | 7.6 | 8.6 | 8.4 | 11 |
- Excludes birth admissions
– Rate = # per 1000 population.
– “Private” excludes Commonwealth care, subsidized coverage through Massachusetts’ Insurance Exchange.
Total ED visits fell in both age groups in Massachusetts and Maryland (Table 2). In contrast, visits with any behavioral health diagnosis on the record rose in absolute terms and per 1000 population. For example, among 19 to 25 year olds, visits increased from 53 to 68 per 1000 in Massachusetts, and from 65 to 99 per 1000 in Maryland. Much of this growth was among visits with diagnoses of substance use disorder, which grew from 22 to 32 per 1000 in Massachusetts and from 38 to 64 per 1000 population in Maryland. Finally, comparing 19 to 25 year olds to 12 to 18 year olds in Massachusetts, the rise in share of visits leading to admission was similar (2.0% and 2.5% among 19 to 25 year olds and 3.3% to 3.9% for 12 to 18 year olds, respectively).
Table 2.
Emergency department visit characteristics
| Age 19 to 25 | Age 12 to 18 | |||||||
|---|---|---|---|---|---|---|---|---|
| Massachusetts | Maryland | Massachusetts | Maryland | |||||
| Emergency Department | 2003–06 | 2007–09 | 2003–06 | 2007–09 | 2003–06 | 2007–09 | 2003–06 | 2007–09 |
| Visits with diagnosis of | ||||||||
| Any diagnoses (total) | 1,279,539 | 998,671 | 967,409 | 845,371 | 819,934 | 642,564 | 674,864 | 527,951 |
| Any behavioral health | 129,056 | 132,230 | 131,592 | 157,917 | 80,734 | 76,301 | 78,028 | 69,907 |
| Depression (only) | 12,320 | 11,101 | 9,432 | 8,083 | 11,984 | 10,393 | 8,680 | 6,848 |
| Psychoses (only) | 5,809 | 6,746 | 4,945 | 6,366 | 3,349 | 4,891 | 3,785 | 5,006 |
| Substance use disorder (only) | 54,844 | 62,494 | 78,215 | 102,141 | 17,631 | 16,553 | 19,399 | 19,582 |
| 2 or more mental disorders | 8,970 | 8,330 | 5,059 | 5,120 | 10,718 | 10,469 | 10,057 | 8,585 |
| Co-occuring SUD and mental | 15,144 | 16,417 | 14,579 | 18,663 | 5,736 | 5,938 | 7,637 | 7,073 |
| Other behavioral health | 31,969 | 27,142 | 19,362 | 17,544 | 31,316 | 28,057 | 28,470 | 22,813 |
| Visit rate per 1000a (SD) for: | ||||||||
| Any diagnoses (total) | 522 (55) | 513 (67) | 478 (101) | 531(136) | 328 (79) | 343 (77) | 300 (76) | 316 (85) |
| Any behavioral health | 53 (6.9) | 68 (5.4) | 65 (15) | 99 (14) | 33 (12) | 41 (15) | 35 (12) | 42 (16) |
| Depression onlyb | 5.0 (1.4) | 5.7 (1.5) | 4.7 (2.0) | 5.1 (2.2) | 4.8 (2.7) | 5.6 (3.1) | 3.9 (2.2) | 4.1 (2.3) |
| Psychoses onlyb | 2.4 (0.9) | 3.5 (0.5) | 2.4 (1.0) | 4.0 (0.7) | 1.3 (0.6) | 2.6 (0.7) | 1.7 (0.8) | 3.0 (1.0) |
| Substance use disorder onlyb | 23 (4.9) | 32 (3.5) | 38 (12) | 64 (8.2) | 7.1 (6.4) | 8.4 (8.6) | 8.7 (9.6) | 11 (13) |
| 2 or more mental disorders | 3.7 (0.8) | 4.3 (0.9) | 2.5 (0.5) | 3.2 (0.7) | 4.3 (1.7) | 5.7 (1.8) | 4.4 (1.2) | 5.2 (1.2) |
| Co-occuring SUD and mentalc | 6.3 (1.6) | 8.5 (1.6) | 7.2 (1.7) | 12 (1.6) | 2.3 (1.7) | 3.1 (2.4) | 3.4 (2.2) | 4.2 (2.9) |
| Other behavioral health | 13 (2.3) | 14 (2.5) | 9.6 (2.2) | 11 (3.0) | 13 (2.6) | 15 (2.9) | 13 (2.5) | 14 (2.8) |
| % admitted to hospitald | 2.02 | 2.46 | d | d | 3.25 | 3.89 | d | d |
| % admissions paid by | ||||||||
| Medicaid | 20 | 28 | 17 | 22 | 27 | 34 | 32 | 37 |
| Private insurancee | 41 | 40 | 38 | 35 | 63 | 59 | 52 | 48 |
| Commcaree | 0.01 | 4.0 | e | e | 0 | 0.17 | e | e |
| Other | 8.1 | 8.1 | 6.5 | 6.2 | 2.2 | 1.8 | 3.3 | 3.5 |
| Uninsured | 31 | 19 | 39 | 37 | 8.3 | 4.8 | 13 | 12 |
| % female | 54 | 56 | 59 | 61 | 50 | 50 | 52 | 53 |
– Rate = # per 1000 population.
– For visits with diagnoses of depression, substance use disorder, or psychosis, “only” indicates that no other behavioral health diagnosis was recorded for that visit. Other physical diagnoses may be present.
– SUD is Substance Use Disorder.
– d not available for Maryland
– “Private” excludes Commcare, subsidized coverage through the Massachusetts Connector
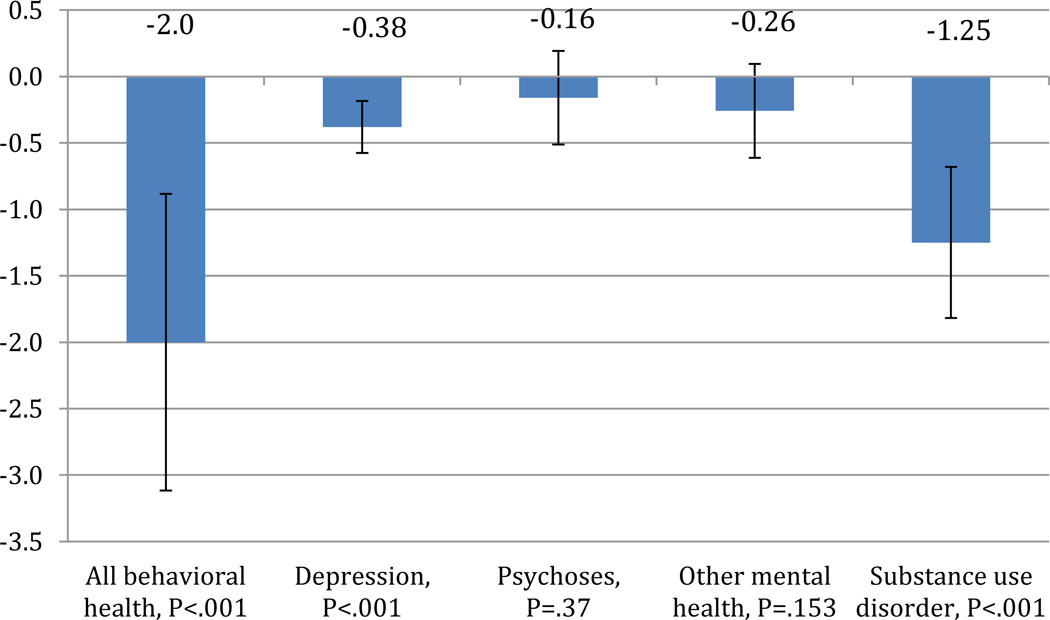
Figure 2 displays the differential change in inpatient admissions per 1000 for 19 to 25 year olds after Massachusetts’ health reform from our regression analyses. Across all behavioral health diagnoses, relative declines in admission rates were 2.0 per 1000 (95% C.I., 0.95–3.2). Comparing young adults in Massachusetts to adolescents and to other states, the relative declines in admissions for primary diagnoses of substance use disorders, 1.3 per 1000 (95% C.I., 0.68–1.8), were greater than the declines in the other specific behavioral health categories. Relative declines in depression admissions among young adults in Massachusetts were also statistically significant, (0.38 admissions per 1000, 95% C.I. 0.18–0.58). Admissions for other behavioral health diagnoses were unchanged, an insignificant fall of 0.27 per 1000 (95% CI, fall of 0.62 to rise of 0.08).
Figure 2.
Change in Behavioral Health Admissions per 1000 among 19–25 Year Olds in Massachusetts vs. Rest of US, Before and After Health Reform
Figure shows adjusted estimate and 95% Confidence Interval of the change in inpatient admissions per 1000 population, for 19–25 year olds in Massachusetts 2003–06 to 2007–09, relative to the rest of the US, netting out changes in admissions for 12–18 year olds in Massachusetts and the rest of the US. SUD is substance use disorder.
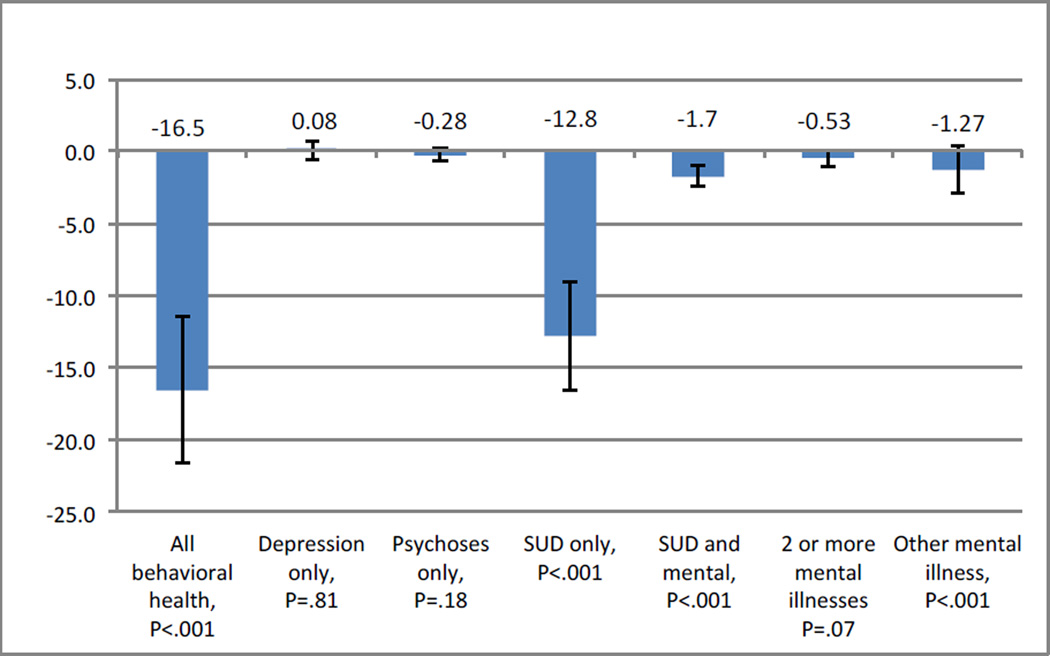
Differential changes in ED visits after Massachusetts health reform are presented in Figure 3. Although ED visits for behavioral health diagnoses grew after 2006, they grew much less among young adults in Massachusetts compared to Maryland, by 16.5 per 1000 (95% CI, 11.4–21.6). Substance use disorder visits grew by 12.8 fewer visits per 1000 (95% C.I. 9.0–16.6) relative to other groups, and accounted for most of the relative declines in visits with behavioral health diagnoses. Relative to other ages and to Maryland, visits for young adults in Massachusetts diagnosed with substance use disorders and at least one mental illness fell by 1.7 per 1000 (95% C.I., 0.91–2.6). Among young adults in Massachusetts, the percent of behavioral health discharges that were uninsured fell by 5.0 (95% CI, 3.0–7.2) percentage points in inpatient settings and 5.0 (95% CI, 1.7–7.8) percentage points in emergency departments, relative to other states.
Figure 3.
Change in Emergency Department Visits with Behavioral Health Diagnoses: Visits per 1000 among 19–25 Year Olds in Massachusetts vs. Rest of US, Before and After Health Reform
Figure shows adjusted estimate and 95% Confidence Interval of the change in emergency department visits per 1000 population, for 19–25 year olds in Massachusetts 2003–06 to 2007–09, relative to Maryland, netting out changes in ED visits for 12–18 year olds in Massachusetts and Maryland. SUD is substance use disorder. For visits with Depression, SUD, or psychosis, “only” indicates that no other behavioral health diagnosis was recorded for that visit. Other physical diagnoses may be present.
Finally, in inpatient settings, young adults in Massachusetts did not experience significant changes in length of stay for overall admissions (+0.22; 95% C.I., −0.17–0.38), but length of stay rose in relative terms for behavioral health admissions (+1.86; 95% C.I., 0.77–2.9). The largest increases were in admissions with primary behavioral health diagnoses other than depression, psychosis, or substance use disorder (+1.86; 95% C.I., 0.52–3.2). Changes for other specific behavioral diagnoses were not statistically significant.
COMMENT
Recent calls for increased access to mental health services have raised concern that increases in coverage will fuel unsustainable increases in utilization and spending. We examined the effects of Massachusetts’ health reform, which dramatically increased health insurance coverage, on hospitalbased utilization. We focused on young adults aged 19–25, a group with relatively high behavioral health needs and low rates of insurance coverage prior to reform, and the target of policies to expand coverage among young adults.22 Increased insurance coverage post-reform coincided with significant relative declines in inpatient admissions and emergency department visits for behavioral health overall. This change was due largely due to lower rates of encounters for individuals with diagnoses of substance use disorders in Massachusetts relative to other states.
The finding that declines were largest for substance use disorders is unsurprising given that these diagnoses were the single most common type of behavioral health diagnosis in hospital-based settings. Thus, one would expect effects to be larger in absolute value for substance use disorders. Furthermore, because many effective substance abuse treatments can be delivered in outpatient settings23–26 care may appropriately move to outpatient settings as insurance coverage expands. This diversion away from inpatient settings may be facilitated by managed behavioral health organizations, charged with managing those benefits, and in some cases, limiting expensive care.14
We also found significant declines in admissions or visits without insurance coverage, in both hospital and ED settings. This change resulted from increased coverage through Commonwealth Care, private coverage, and Medicaid. This signifies much lower out of pocket burden for young adults with a behavioral health crisis, as well as less uncompensated care burdening hospitals.
Prior to this study, research examining the impact of Massachusetts health reform’s coverage expansion on hospital care focused on utilization of services for general medical conditions,20,21 but did not examine patterns of care for behavioral health, conditions that are particularly important for young adults and for which public and private insurance coverage often leaves gaps. An important strength of this study is that we examine the universe of Massachusetts’ hospital admissions allowing for richer analyses than earlier data using a sample of inpatient admissions.20 The declines in hospital-based care found in this study are consistent with less-severely ill young adults using more care in outpatient settings, and consequently avoiding hospital-based care. Health plans have incentives to limit access to inpatient settings as they assume responsibility for the newly-insured population’s behavioral health services. Indeed evidence from managed behavioral health organizations suggests that inpatient utilization declines when behavioral health plans manage these services, but the outcome of such diversion depends on whether patients are diverted to suitable alternative care.14
The results presented here should be interpreted with several limitations in mind. First, we do not observe outpatient treatment for mental illness or substance abuse for individuals in the study. Thus, we cannot infer whether reduced use of hospital based care for mental illness and substance use disorders represents lower rates of morbidity in the population,27 effective care in outpatient settings,23–26 or restrictions on use of hospital-based settings.14 However, it is unlikely that reduced inpatient use represents worse behavioral health after increasing health insurance, or limits on care associated with insurance expansion. Because changes within Massachusetts were larger for 19–25 year olds compared with 12–18 year olds, it is unlikely that Massachusetts’ policies or practices besides health reform explain our findings.
Second, Massachusetts’ mental health system was more expansive with 32.4 Psychiatrists per capita18 compared to 14.5 for the U.S.17 Finally, high rates of hospitalization for behavioral health in Massachusetts compared to other states limit our ability to generalize findings to areas of the country where hospital-based care is less common. The decline in the use of hospital-based mental health services found here may not be generalizable to the lean mental health system found in the rest of the U.S., although it is encouraging that a system more likely to use hospital based care did not increase inpatient admissions and ED visits when coverage increased.
It is important to consider these results within the context of the Massachusetts behavioral health care landscape and reforms more broadly. Massachusetts’ health reform required insurance plans to cover dependents up to age 26 on parental policies, just as PPACA has required since September of 2010. The remaining coverage related provisions in PPACA will not take effect until 2014. Furthermore, Massachusetts’ health reform allowed for low cost ‘Young Adult Plans’ for 18–26 year olds without access to employer sponsored coverage.28 Finally, in addition to PPACA, the federal parity law, implemented in 2010–2011, is likely to improve care for individuals with behavioral health conditions. Although Massachusetts had a state mental health parity law prior to reform, this law was less extensive.
As developmental neuroscience indicates, brain development continues into early adulthood. Similarly, the onsets of major mental illnesses are very high in this period.29 Thus, providing high quality preventive and treatment services to this age group is an important goal.30 These data offer a snapshot of one aspect of policies to improve access to behavioral health treatment, expanded insurance coverage. It is reassuring that use of expensive emergency and inpatient treatments did not rise with greater insurance coverage, a result that stands in contrast to a recent analysis describing the aggregate rise in behavioral health spending over recent years.31 Further studies should examine patterns of care across inpatient and outpatient settings, particularly as data emerge since implementation of Federal parity laws. The increase in visits for substance use disorders is noteworthy and speaks to the need for effective treatment and preventive services. Expanded health insurance coverage for young adults is not associated with large increases in hospital-based care for behavioral health, but it increased financial protection to young adults with behavioral health diagnoses, and to the hospitals that care for them.
Supplementary Material
ACKNOWLEDGMENT
This research was supported by the following NIH grants from the National Institute of Drug Abuse: K24DA019855, DA030391, and DA026414. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; nor in the decision to submit the manuscript for publication. Dr. Meara had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All analyses were completed by Ms. Zaha, Dr. Golberstein, and Dr. Meara.
Contributor Information
Ellen Meara, Email: ellen.r.meara@dartmouth.edu, Associate Professor, The Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine, 35 Centerra Parkway, Lebanon, NH 03766, Phone: 603-653-0899 Fax: 603-653-0820; National Bureau of Economic Research, Cambridge, MA.
Ezra Golberstein, Email: egolberstein@umn.edu, Assistant Professor of Health Policy and Management, University of Minnesota School of Public Health.
Rebecca Zaha, Email: rebecca.zaha@dartmouth.edu, Epidemiologic Research Analyst, The Dartmouth Institute for Health Policy and Clinical Practice Geisel School of Medicine.
Shelly F. Greenfield, Email: sgreenfield@mclean.harvard.edu, Chief Academic Officer, McLean Hospital; Professor of Psychiatry, Harvard Medical School.
William R. Beardslee, Email: william.beardslee@childrens.harvard.edu, Director, Baer Prevention Initiatives, Department of Psychiatry, Boston Children's Hospital; Gardner-Monks Professor of Child Psychiatry, Harvard Medical School.
Susan H. Busch, Email: susan.busch@yale.edu, Associate Professor, Department of Health Policy and Management, Yale School of Public Health.
REFERENCES
- 1.Gruber J. Massachusetts Points the Way to Successful Heatlh Care Reform. J Policy Anal Manage. 2011;30(1):184–192. [Google Scholar]
- 2.Busch SH, Meara E, Huskamp HA, Barry CL. Characteristics of Adults With Substance Use Disorders Expected to Be Eligible for Medicaid Under the ACA. Psychiatr Serv. 2013 Mar 1;64(6):520–526. doi: 10.1176/appi.ps.201200011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garfield RL, Zuvekas SH, Lave JR, Donohue JM. The impact of national health care reform on adults with severe mental disorders. Am J Psychiatry. 2011 May;168(5):486–494. doi: 10.1176/appi.ajp.2010.10060792. [DOI] [PubMed] [Google Scholar]
- 4.Barry CL, Huskamp HA. Moving beyond parity--mental health and addiction care under the ACA. N Engl J Med. 2011 Sep 15;365(11):973–975. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Chiu WT, Colpe L, et al. The prevalence and correlates of serious mental illness (SMI) in the National Comorbidity Survey Replication (NCS-R) In: Manderscheid RW, Berry JT, editors. Mental Health, United States, 2004. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. pp. 134–148. [Google Scholar]
- 7.Druss RG. The psychology of illness : in sickness and in health. 1st ed. Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- 8.Ettner S, Frank R, Kessler R. Impact of Psychiatric Disorder on Labor Market Outcomes. Ind Labor Relat Rev. 1997;51(1):64–81. [Google Scholar]
- 9.Kaiser Family Foundation. How Will Health Reform Impact Young Adults? 2010 [Google Scholar]
- 10.Levine P, McKnight R, Heep S. How Effective are Public Policies to Increase Health Insurance Coverage among Young Adults? Am Econ J Econ Policy. 2011;3(1):129–156. [Google Scholar]
- 11.US Social Security Administration. Benefits for Children with Disabilities. 2013 [Google Scholar]
- 12.Frank RG, McGuire TG. Economics and mental health. In: Culyer A, Newhouse J, editors. Handbook of Health Economics. Vol 1. New York: Elsevier; 2000. pp. 893–954. [Google Scholar]
- 13.Keeler EB, Manning WG, Wells KB. The demand for episodes of mental health services. J Health Econ. 1988 Dec;7(4):369–392. doi: 10.1016/0167-6296(88)90021-5. [DOI] [PubMed] [Google Scholar]
- 14.Frank RG, Garfield RL. Managed behavioral health care carve-outs: past performance and future prospects. Annu Rev Public Health. 2007;28:303–320. doi: 10.1146/annurev.publhealth.28.021406.144029. [DOI] [PubMed] [Google Scholar]
- 15.Kenney GM, Long SK, Luque A. Health reform in Massachusetts cut the uninsurance rate among children in half. Health Aff (Millwood) 2010 Jun;29(6):1242–1247. doi: 10.1377/hlthaff.2010.0314. [DOI] [PubMed] [Google Scholar]
- 16.HCUP Databases, editor. Rockville, MD: Agency for Healthcare Research and Quality; 2003–2009. Healthcare Cost and Utilization Project (HCUP) http://www.hcup-us.ahrq.gov/databases.jsp; [PubMed] [Google Scholar]
- 17.OECD. OECD.StatExtracts: Health Care Resources, Physicians by Category. In: OECD, editor. Paris, France: 2011. [Google Scholar]
- 18.Thomson Healthcare. Ranking America's Mental Health: An Analysis of Depression Across the States. Washington, D.C: Mental Health America; 2007. [Google Scholar]
- 19.US Census Bureau. State Intercensal Estimates (2000–2010) 2012 [Google Scholar]
- 20.Kolstad JT, Kowalski AE. The Impact of Health Care Reform on Hospital and Preventive Care: Evidence from Massachusetts. J Public Econ. 2012 Dec 1;96(11–12):909–929. doi: 10.1016/j.jpubeco.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller S. The effect of the Massachusetts reform on health care utilization. Inquiry. 2012 Winter;49(4):317–326. doi: 10.5034/inquiryjrnl_49.04.05. [DOI] [PubMed] [Google Scholar]
- 22.Long SK, Yemane A, Stockley K. Disentangling the Effects of Health Reform in Massachusetts: How Important Are the Special Provisions for Young Adults? Am Econ Rev. 2010;100(May 2010):297–302. doi: 10.1257/aer.100.2.297. [DOI] [PubMed] [Google Scholar]
- 23.Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcohol Clin Exp Res. 1998 Sep;22(6):1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- 24.Fiellin DA, Pantalon MV, Chawarski MC, et al. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med. 2006 Jul 27;355(4):365–374. doi: 10.1056/NEJMoa055255. [DOI] [PubMed] [Google Scholar]
- 25.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997 Apr 2;277(13):1039–1045. [PubMed] [Google Scholar]
- 26.Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year Follow-up Outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychol Addict Behav. 1998;11(4):291–298. [Google Scholar]
- 27.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013 May 2;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Massachuseetts Health Insurance Connector Authority T. Report to the Massachusetts Legislature Implementation of the Health Care Reform Law, Chapter 58 2006–2008. Boston: Massachusetts; 2008. [Google Scholar]
- 29.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 30.National Research Council and Institute of Medicine. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, D.C: Committee on Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions; 2009. [Google Scholar]
- 31.Health Care Cost Institute. The impact of the Mental Health Parity and Addiction Equity Act on Inpatient Admissions. Washington, D.C: 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.