Abstract
Background
Controversy remains regarding the role of pyloric drainage procedures following esophagectomy with gastric conduit reconstruction. We aimed to compare the effect of pyloric drainage strategies upon subsequent risk of complications suggestive of conduit distention, including aspiration and anastomotic leak.
Methods
A retrospective study was conducted reviewing patients undergoing esophagectomy between 1/2007 – 4/2012. Prospectively collected data included baseline comorbidities, operative details, hospital course, and complications. Statistical comparisons were performed using ANOVA for continuous variables and X2 testing for categorical variables.
Results
There were 361 esophagectomies performed during the study period, 68 were excluded from analysis (for prior esophagogastric surgery and/or benign disease). Among 293 esophagectomies included, emptying procedures were performed as follows: 44 (15%) no drainage procedure, 197 (67%) pyloromyotomy/pyloroplasty, 8 (3%) dilation alone, 44 (15%) dilation + onabotulinumtoxinA. Aspiration occurred more frequently when no pyloric intervention was performed (5/44 [11.4%] versus 6/249 [2.4%], P = 0.030). The incidence of anastomotic leak (18 [6.1%]) and gastric outlet obstruction (5 [1.7%]) were statistically similar among groups. Subgroup analysis demonstrated persistence of these findings when limiting the comparison to transthoracic esophagectomies. Major complications directly related to pyloroplasty/pyloromyotomy occurred in 2 (0.6%) patients, including 1 (0.3%) mortality.
Conclusions
These data suggest that omission of pyloric intervention at the index operation results in more frequent aspiration events. The combination of dilation plus onabotulinumtoxinA provided for a similar complication profile compared to surgical drainage. Future prospective comparisons are needed to evaluate these short-term effects of pyloric intervention as well as long-term sequelae such as dumping syndrome and bile reflux.
Keywords: esophageal surgery; surgery, complications; esophageal cancer
Introduction
For patients with potentially curable disease, surgical resection plays a significant role in the treatment of esophageal cancer. While several technical approaches exist for performing esophagectomy, all are associated with significant morbidity and mortality, in the ranges of 50-60% and 5-18%, respectively.1,2 Regardless of the surgical approach, pull-up with gastric conduit remains the most common reconstruction. While vagal-sparing esophagectomy has been described for patients with benign disease or early-staged malignancy,3-5 this technique is not ideal for locally advanced cancers. For most patients, bilateral vagotomies are inherent in the conduction of the operation, rendering these individuals susceptible to problems related to impaired gastric emptying and contributing to the burden of postoperative morbidity attributed to esophagectomy with gastric conduit reconstruction.
The association of bilateral vagotomy with delayed gastric emptying and gastric outlet obstruction originates from early publications documenting the physiologic effects of vagotomies performed in the surgical treatment of peptic ulcer disease.6 Significantly delayed gastric emptying is generally believed to occur in approximately 15% of patients who undergo esophagectomy with gastric pull-up, with reports of this problem ranging from 4 to 50%.7-13 Delayed gastric emptying after esophagectomy has been associated with increased aspiration, prolonged hospital stay, and decreased patient satisfaction.14,15
Proponents of pyloric drainage argue that procedures such as pyloroplasty or pyloromyotomy can prevent gastric outlet obstruction, thereby lowering the risk of aspiration events, with resultant decrease in postoperative morbidity and mortality.12 However, while two large meta-analyses supported pyloric drainage on the basis of decreased gastric outlet obstruction and improved gastric emptying, overall complication rates and operative mortality were unaffected by pyloric drainage.13,16,17 Further, increasing reports of minimally invasive esophagectomies have shown that, when conducted by experienced surgeons, these procedures have comparable outcomes to open procedures, despite rare inclusion of pyloric drainage.16,18,19
As potential downfalls of pyloromyotomy/pyloroplasty have been weighed against the proposed benefits of improved gastric drainage, additional tools for improving pyloric drainage have entered the thoracic surgeon’s armamentarium. A number of authors have suggested that endoscopic balloon dilatation and botulinum toxin may effectively reduce gastric outlet obstruction and, further, may allow avoidance of risks specifically inherent to pyloroplasty/pyloromyotomy.9,12,15,20-23
In our institution, several methods of addressing pyloric drainage have been employed, including omission of pyloric drainage in a portion of patients. In this study, we sought to assess the impact of current pyloric drainage techniques upon subsequent risk of aspiration and anastomotic leak. Further, we aimed to compare outcomes among these techniques, with the ultimate goal of identifying an optimal management strategy with regard to the issue of pyloric drainage at the time of esophagectomy. In particular, with recent increase in our use of botulinum and its anecdotally favorable complication profile, we sought to specifically demonstrate non-inferiority of botulinum versus surgical drainage with regard to potential complications related to delayed gastric emptying.
Patients and Methods
Following Institutional Review Board approval, a retrospective review was conducted of prospectively gathered data for all patients who underwent esophagectomy at a single institution between January 2007 and April 2012. Patients were excluded if esophagectomies were performed for benign disease or if they had undergone previous esophagogastric surgery. Data were retrieved from the Society of Thoracic Surgeons database maintained by the surgical division and supplemented with clinical information from patient medical records and the Social Security Death Index.
Patients underwent various pyloric drainage procedures according to surgeon preference. Pyloromyotomy and pyloroplasty were performed in adherence to routine operative technique. Manual pyloric dilatation, when used in isolation, was applied by digitally stretching the pylorus and everting it between the thumb and forefinger. OnabotulinumtoxinA (Botox; Allergan, Inc., Irvine, CA) was injected as 200 mg in 8 mL, delivered in equal parts circumferentially into the pylorus, and accompanied by either digital pyloric dilation or endoscopic balloon dilation. Endoscopic dilatation, when employed in the postoperative setting, was performed with fiberoptic esophagoscopy and using standard manufactured esophagogastroduodenoscopy pneumatic balloons.
Aspiration was deemed to have occurred if it was witnessed at the bedside (vomiting or regurgitation noted to precede coughing, gagging, and/or acute decompensation in respiratory status) or evident on contrast esophagography. Pneumonia diagnosis was based on strict criteria as defined by STS guidelines, as were all other postoperative outcome definitions, when applicable.24 Anastomotic leakage was defined by presence of contrast extravasation on esophagography or visualization of an anastomotic breakdown on endoscopy. Presence of gastric outlet obstruction, delayed gastric emptying, and dumping syndrome were based on patient reported symptoms upon follow-up. We did not routinely perform radiographic studies to objectively assess the degree of delayed gastric emptying.
Clinical data were analyzed using SPSS (SPSS 21.0 for Windows; SPSS Inc., Chicago, IL). Descriptive statistics were expressed as mean ± standard error, and comparisons were made with paired, two-tailed t-tests and single-factor Analysis of Variance (ANOVA) tests for means of normally distributed continuous variables. Categorical data were expressed as counts and percentages, with Fisher’s exact test and chi-squared testing used to analyze differences, with α=0.05 considered significant.
Results
Patients
361 esophagectomies were performed during the study period, with 293 patients meeting inclusion criteria. Mean age was 61.8 +/− 0.6 years, and 248 (84.6%) were male. For 44 (15.0%) patients, no pyloric intervention was performed at the index operation. Among the remainder, pyloromyotomy was performed in 161 (54.9%), pyloroplasty in 36 (12.3%), digital dilatation in 8 (2.7%), and botulinum toxin in 44 (15.0%). Pyloric drainage strategy trends over time are shown in Fig 1. Demographics and comorbidities, as shown in Table 1, were not significantly different among groups as stratified by pyloric drainage strategy.
Figure 1. Pyloric drainage procedure trends over time.
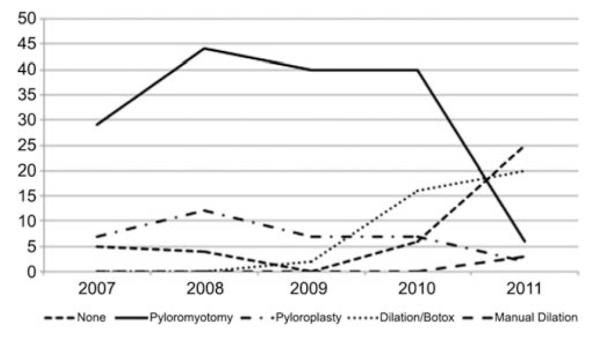
As we have learned from our experiences, beginning approximately 2010, our use of pyloromyotomy and pyloroplasty has diminished, while employment of botulinum toxin injection continues to rise.
Table 1.
Patient demographics/comorbidities
| No intervention |
Pyloroplasty /
pyloromyotomy |
Dilation |
Dilation +
botulinum toxin |
Total | P-value | |
|---|---|---|---|---|---|---|
| N | 44 | 197 | 8 | 44 | 293 | |
| Age (years) | 61.1 +/− 1.4 | 61.4 +/− 0.7 | 59.8 +/− 3.7 | 64.7 +/− 1.4 | 61.8 +/− 0.6 | 0.174 |
| Male | 38 (86.4%) | 162 (82.2%) | 7 (87.5%) | 41 (93.2%) | 248 (84.6%) | 0.321 |
| BMI | 27.6 +/−0.8 | 27.7 +/− 0.4 | 28.6 +/− 2.1 | 28.9 +/− 0.7 | 27.9 +/− 0.3 | 0.514 |
| Current smoker | 7 (15.9%) | 42 (21.3%) | 1 (12.5%) | 4 (9.1%) | 54 (18.4%) | 0.582 |
| Previous smoker | 24 (54.5%) | 102 (51.8%) | 4 (50.0%) | 24 (54.5%) | 154 (52.6%) | |
| Pack-year smoking | 30.0 +/− 5.6 | 32.6 +/− 2.2 | 22.3 +/− 7.3 | 25.3 +/− 4.3 | 30.8 +/− 1.8 | 0.453 |
| COPD | 3 (6.8%) | 24 (12.2%) | 1 (12.5%) | 4 (9.1%) | 32 (10.9%) | 0.74 |
| GERD | 24 (54.5%) | 108 (54.8%) | 5 (62.5%) | 23 (52.3%) | 160 (54.6%) | 0.96 |
| Barrett’s | 8 (18.2%) | 36 (18.3%) | 2 (25.0%) | 9 (20.5%) | 55 (18.8%) | 0.962 |
| HTN | 22 (50.0%) | 104 (52.8%) | 3 (37.5%) | 30 (68.2%) | 159 (54.3%) | 0.184 |
| DM | 10 (22.7%) | 30 (15.2%) | 1 (12.5%) | 10 (22.7%) | 51 (17.4%) | 0.472 |
| CAD | 8 (18.2%) | 24 (12.2%) | 3 (37.5%) | 10 (22.7%) | 45 (15.4%) | 0.084 |
| Preop chemo | 25 (57%) | 96 (49%) | 6 (75%) | 23 (52%) | 150 (51.2%) | 0.412 |
| Preop XRT | 23 (52%) | 101 (51%) | 6 (75%) | 21 (48%) | 151 (51.5%) | 0.565 |
BMI = body mass index; COPD = chronic obstructive pulmonary disease; GERD = gastroesophageal reflux disease; HTN = hypertension; DM = diabetes mellitus; CAD = coronary artery disease; Preop chemo = preoperative chemotherapy; Preop XRT = preoperative radiation therapy
Operative procedures
Esophagectomies were performed by 6 surgeons, with 164 (56.0%) transthoracic and 129 (44.0%) transhiatal approaches. Considerable variability in operative time was present among all techniques (Table 2). Patients who underwent dilation with botulinum injection had significantly longer operations than those individuals in the other groups. These were predominantly Ivor Lewis esophagectomies, which, in general, took more time than transhiatal esophagectomies. Operative time tended to vary most by surgeon, and did not vary significantly by pyloric drainage strategy within same-surgeon groups. 289 (98.6%) of the patients included in this study underwent gastric pull-up as the conduit used for reconstruction, with a tubularized stomach (rather than whole stomach) employed in all 289 of these individuals. All tubularized stomachs were created with the goal of a 4-5 cm wide conduit. There were no significant differences in type of conduit used, type of anastomosis performed, ASA class, or need for intraoperative transfusion among the groups as defined by pyloric drainage.
Table 2.
Operative and hospitalization resource utilization
| No intervention |
Pyloroplasty /
pyloromyotomy |
Dilation |
Dilation +
botulinum toxin |
Total | P-value | |
|---|---|---|---|---|---|---|
| N | 44 | 197 | 8 | 44 | 293 | |
| Operative time, hh:mm |
3:44 +/− 9:38 | 4:55 +/− 0:07 | 2:55 +/− 0:07 | 6:23 +/− 0:15 | 4:54 +/− 0:06 | <0.001 |
| ICU LOS, days | 2.18 +/− 0.5 | 4.16 +/− 0.4 | 3.00 +/− 1.5 | 5.14 +/− 2.03 | 3.98 +/− 0.4 | 0.279 |
| Hospital LOS, days | 12.7 +/− 1.0 | 13.6 +/− 0.6 | 15.3 +/− 3.0 | 16.5 +/− 2.62 | 13.9 +/− 0.6 | 0.284 |
ICU = Intensive Care Unit; LOS = Length of Stay
Postoperative course
The average lengths of ICU and overall hospital stay did not differ among groups, and are shown in Table 2. There were 102 (34.8%) patients that returned to the operating room prior to discharge; overall likelihood of returning to the OR was not dependent upon pyloric drainage procedure (P = 0.278).
Delayed gastric emptying was documented for only 5 (1.7%) patients, and it did not differ among pyloric drainage strategies. However, differences were seen among complications potentially related to poor gastric emptying. Need for postoperative pyloric dilation during the index hospitalization was significantly reduced by the inclusion of any pyloric drainage technique during the esophagectomy (7 [15.9%] versus 8 [3.2%], P = 0.008). Likewise, risk of aspiration was also reduced when any pyloric drainage strategy was employed (5 [11.4%] versus 6 [2.4%], P = 0.030). When performing ANOVA to assess differences in these outcomes among all pyloric drainage strategies, these findings persist (Table 3, Fig. 2). Further, there were no significant differences seen when comparing complications of the various pyloric drainage strategies compared head-to-head.
Table 3.
30-day complications
| No intervention |
Pyloroplasty /
pyloromyotomy |
Dilation |
Dilation +
botulinum toxin |
Total | P-value | |
|---|---|---|---|---|---|---|
| N | 44 | 197 | 8 | 44 | 293 | |
| Aspiration | 5 (11.4%) | 4 (2.0%) | 0 | 2 (4.5%) | 11 (3.8%) | 0.029 |
| Pneumonia | 3 (6.8%) | 26 (13.2%) | 0 | 6 (13.6%) | 35 (11.9%) | 0.458 |
| Anastomotic leak requiring medical treatment only |
2 (4.5%) | 1 (0.5%) | 0 | 2 (4.5%) | 5 (1.7%) | 0.109 |
| Anastomotic leak requiring operative intervention |
1 (2.3%) | 8 (4.1%) | 1 (12.5%) | 3 (6.8%) | 13 (4.4%) | 0.500 |
| Postoperative pyloric dilation before discharge |
7 (15.9%) | 5 (2.5%) | 0 | 3 (6.8%) | 15 (5.1%) | 0.003 |
Figure 2. Postoperative complication development by drainage procedure type.
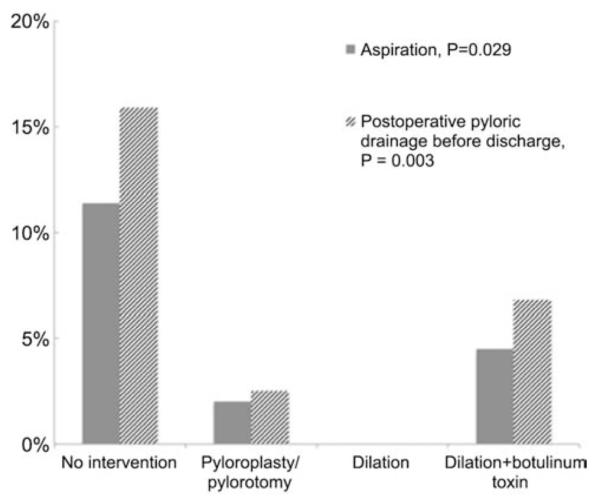
Patients who did not undergo any pyloric drainage intervention were at increased risk of aspiration as well as need for pyloric drainage procedure prior to discharge from index hospitalization.
Of significant interest, early during the study period, two severe complications were observed directly related to pyloric drainage procedures. In one patient who had undergone induction therapy followed by Ivor Lewis esophagectomy, during his pyloromyotomy, the mucosa was inadvertently entered. The myotomy was converted to a pyloroplasty, and a routine esophagram on post-operative day (POD) 7 demonstrated a leak from the site of the pyloroplasty, which persisted, ultimately requiring stent placement across the pylorus on POD 17 and further re-explorations. The patient’s post-operative course continued to be complicated, and he ultimately succumbed on POD 68. In a second patient, who underwent pyloromyotomy, re-exploration was required on POD 1 when bilious drainage was noted from the midline abdominal incision. Operative findings included a pinpoint hole at the pyloromyotomy. This patient was also converted to a pyloroplasty. Thus, major complications directly related to pyloroplasty/pyloromyotomy occurred in 2 (0.6%) serious complications, including 1 (0.3%) mortality.
Long-term outcomes
Late postoperative data were available for 272 (92.8%) from the 0 to 6 month time period, 157 (53.6%) from 6 to 12 months, and 140 (47.8%) past 12 months. Neither the inclusion of a pyloric drainage procedure nor the specific type of drainage performed significantly impacted the need for subsequent dilation of the pylorus during the follow-up period (Table 4). Likewise, the prevalence of symptoms of dumping syndrome and bile reflux at each time point were similar among all groups, with no significant differences found in our analyses.
Table 4.
Long-term outcomes
| No intervention |
Pyloroplasty /
pyloromyotomy |
Dilation |
Dilation +
botulinum toxin |
Total | P-value | |
|---|---|---|---|---|---|---|
| N | 44 | 197 | 8 | 44 | 293 | |
| Pyloric dilation required |
5 (11%) | 23 (12%) | 2 (5%) | 8 (18%) | 38 (13.0%) | 0.479 |
| Dumping 0 - 6M | 5/39 (13%) | 26/187 (14%) | 1/7 (14%) | 5/39 (13%) | 37/272 (13.6%) | 0.996 |
| Dumping 6 - 12M | 1/18 (6%) | 19/111 (17%) | 1/1 (100%) | 5/27 (19%) | 26/167(15.6%) | 0.082 |
| Dumping > 12M | 0/14 | 23/111 (21%) | 0/0 | 2/15 (13%) | 25/140 (17.9%) | 0.144 |
Comment
In this study, patients who did not receive pyloric drainage procedures at the time of esophagectomy were prone to increased risk of aspiration during the postoperative period and were more likely to need pyloric dilation prior to discharge from the hospital. We did not demonstrate any clear benefit of one pyloric drainage strategy over others in prevention of gastric outlet obstruction-related complications. However, of significant importance, major complications directly related to pyloroplasty/pyloromyotomy occurred, including 1 (0.3%) mortality. Therefore, innovative strategies of providing pyloric drainage while minimizing procedural risk are highly desirable, rendering options such as botulinum toxin injection a potentially acceptable alternative.
Our study did not show any reduction in pneumonia, length of stay, or respiratory failure following pyloric drainage procedures. These outcomes measures, while markers of gastric emptying, all have multifactorial origins, and our study may have been underpowered to demonstrate such differences. While there may be potential benefits from pyloric drainage, the conundrum of balancing risk versus benefit remains. Proponents of pyloric drainage have emphasized the low morbidity of the procedure.2 However, as seen here, significant adverse events, although rare, may occur following pyloroplasty/pyloromyotomy.25 Zieren and colleagues described 1 mortality and 1 severe stricture formation secondary to surgical pyloric drainage, accounting for 3.8% of their study group.26
In addition to such infrequent, serious complications of pyloric drainage, less severe side effects may occur with a greater prevalence. Patients undergoing pyloric drainage may make a tradeoff, exchanging poor gastric motility for bile reflux and dumping syndrome.25,27,28 Wang et al found patients with pyloroplasty to experience greater incidences of both of these undesirable outcomes (Table 5).28
Table 5.
Previous investigations
| Author | Year | Methodology | N | Outcomes significantly impacted by pyloric intervention | Outcomes unaffected by pyloric drainage |
|---|---|---|---|---|---|
| Wang | 1992 | Retrospective review |
368 | Bile reflux: 55.6% pyloroplasty vs 8.6% no pyloroplasty Dumping syndrome: 33.3% pyloroplasty vs 6.9% no pyloroplasty |
|
| Urschel | 2002 | Meta-analysis | 553 | Early postoperative gastric outlet obstruction: decreased with pyloric drainage vs no drainage (P = 0.046) |
No differences in respiratory complications, failure to thrive, anastomotic leaks, or long-term gastric emptying |
| Khan | 2007 | Meta-analysis | 1063 | Gastric motility: faster with pyloric drainage Gastric outlet obstruction: less frequent with pyloric drainage |
No differences in anastomotic leak rate, pulmonary complications, or operative mortality |
| Gaur | 2013 | Meta-analysis | 668 | Pyloric drainage associated with non-significant trend for delayed gastric emptying and bile reflux, no impact on dumping, leaks, pulmonary complications, hospital stay, and overall morbidity |
|
| Lanuti | 2007 | Retrospective review |
242 | Pyloric dilation improved gastric outlet obstruction in 96.7% | Pyloromyotomy vs no pyloromyotomy with no difference in gastric outlet obstruction, pneumonia, respiratory failure, or length of stay |
| Kim | 2008 | Prospective observational |
257 | Pyloric dilation improved symptoms of delayed gastric emptying in 100% Pyloric dilation resulted in increased rates of gastric emptying on radio-isotope imaging in 67% |
|
| Lanuti | 2011 | Retrospective review |
436 | Pyloric dilation 95% successful in patients with delayed gastric emptying |
|
| Kent | 2007 | Prospective pilot study |
15 | After botulinum injection, 0 patients developed delayed gastric emptying or aspiration pneumonia |
|
| Cerfolio | 2009 | Retrospective review |
221 | Delayed gastric emptying: 93% pyloromyotomy, 96% pyloroplasty, 96% no drainage procedure, 59% botulinum injection (P=0.002) Biliary reflux at follow-up (mean 40 months) lowest in botulinum group (P = 0.024) Hospital stay and operative times shorter for botulinum injection (P = 0.015 and 0.037, respectively |
With such mixed results, the utility of pyloric drainage has been an area of particular interest to esophageal surgeons. Meta-analyses performed by Urschel and Khan both suggested a reduced rate of early postoperative gastric outlet obstruction among patients who underwent pyloric drainage procedures; however, patients experienced no consequent improvement in other related outcomes13,17 (Table 5). In 2013, another meta-analysis aimed to readdress the issues, evaluating outcomes from studies performed within the last decade.11,22,29,30 Each of the studies considered in this publication suggested that pyloric drainage was unnecessary and could be omitted. Reasons for the shift in paradigm may be related to an evolution over time with regard to the type of gastric conduit used, as it has been shown that use of whole stomach pull-ups has a greater tendency toward gastric outlet obstruction and delayed gastric emptying.31 Results of this review conflicted with those of the two aforementioned meta-analyses, concluding that with the modern use of gastric tubes, pyloric drainage strategies may be obsolete16 (Table 5).
New techniques, such as endoscopic balloon dilation and botulinum toxin injection have been touted for a number of potential strengths. Analyzing results of 242 esophagectomies, Lanuti failed to demonstrate any clinical benefits of pyloromyotomy over no drainage; however, in this study, pyloric dilation proved successful in managing symptoms of gastric outlet obstruction (Table 5).22 Similarly, Kim used balloon dilatation to successfully ameliorate all 21 (8%) patients who sustained symptoms of delayed gastric emptying.9 More recently, Lanuti evaluated 436 esophagectomy patients, among whom a portion underwent pyloric dilation with controlled radial expansion balloon dilators, demonstrating a 95% success rate.23
A number of practicing surgeons have begun injecting botulinum toxin into the pylorus, achieving the early benefits of a gastric outlet procedure while avoiding potential complications.15,21 Kent performed a pilot study of botulinum in association with minimally invasive esophagectomy, demonstrating its utility in preventing delayed gastric emptying and aspiration pneumonia.21 In a larger retrospective study, Cerfolio reports outcomes of postoperative gastric emptying, aspiration, and swallowing symptoms, with findings strongly suggesting beneficial outcomes of botulinum compared to other drainage strategies (Table 5).20 Subsequently, Martin reported botulinum toxin to be an effective means of avoiding delayed gastric emptying in 96% of patients.15
In this study, we describe the use of botulinum toxin injection as an alternative to pyloroplasty and pyloromyotomy, which, in part, is attractive due to the decreased risk of leak from the pylorus. Other strategies have been described in attempts to minimize risk of pyloric disruption, such as the circular stapled pyloroplasty.32,33 While this technique has been shown to reduce risks of leak as well as conduit shortening when compared to standard pyloroplasty, there are further advantages that are unique to botulinum injection. Each of the invasive surgical strategies for pyloric drainage, regardless of specific risk of perforation, tends to have permanent effects. However, physiologic studies have suggested that foregut function following esophagectomy improves with time, regardless of the anastomotic level or the inclusion of pyloric drainage procedures.16,34-36 Consequently, the transient nature of the botulinum injection offers additional benefits that may not be attainable by simply altering the technical approach to pyloroplasty.
We acknowledge that this study is subject to several limitations. These data were retrospectively retrieved from a prospective database, rather than obtained via randomization. Choice of gastric emptying strategy was decided by surgeon preference, and there may some inherent selection bias in terms of the different practices and experiences of the surgeons in the group. In addition, in considering need for pyloric dilation as an outcome of interest, we recognize the lack of objective criteria in determining requirement for intervention. Reasons for pyloric dilation included slow progression of contrast through the pylorus on esophagography and/or symptoms of delayed gastric emptying. It is conceivable that, for patients already undergoing endoscopy for alternative reasons, there may have been a lower threshold to proceed with concurrent pyloric dilation. Additionally, we acknowledge that our stringent definition of aspiration, requiring either a witnessed event or radiographic evidence, has the potential to miss some episodes. We presume that this likelihood is similar for all groups regardless of pyloric drainage strategy. Finally, we acknowledge that this study may be underpowered to detect differences among various drainage strategies for the defined postoperative outcomes, and we aim to conduct large scale prospective studies in the future.
In this study, we aimed to investigate the ongoing utility of pyloric drainage for patients undergoing esophagectomy for cancer with tubularized gastric reconstruction. We further sought to compare benefits and risk profiles of various pyloric drainage strategies. This study carries several strengths, in that it is a large review of prospectively gathered data obtained in the modern era. We found that inclusion of pyloric drainage procedures helped reduce risk of aspiration and need for pyloric dilatation prior to discharge. All pyloric drainage strategies were essentially similarly effective; however, we found botulinum injection to result in comparable benefits with minimal inherent risk, as compared to pyloroplasty/pyloromyotomy. Botulinum toxin injection serves as a promising adjunct to esophageal surgery, and future trials investigating perioperative outcomes, long-term follow-up, and quality of life metrics are warranted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation: Southern Thoracic Surgical Association Meeting; November 1, 2013. Scottsdale, Arizona.
References
- 1.Metzger R, Bollschweiler E, Vallbohmer D, Maish M, DeMeester TR, Holscher AH. High volume centers for esophagectomy: what is the number needed to achieve low postoperative mortality? Dis Esophagus. 2004;17:310–4. doi: 10.1111/j.1442-2050.2004.00431.x. [DOI] [PubMed] [Google Scholar]
- 2.Raymond D. Complications of Esophagectomy. Surg Clin N Am. 2012;92:1299–313. doi: 10.1016/j.suc.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Banki F, Mason RJ, DeMeester SR, et al. Vagal-sparing esophagectomy: a more physiologic alternative. Ann Surg. 2002;236:324–35. doi: 10.1097/00000658-200209000-00009. discussion 35-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peyre CG, DeMeester TR. Vagal-sparing esophagectomy. Adv Surg. 2008;42:109–16. doi: 10.1016/j.yasu.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 5.DeMeester SR. Vagal-sparing esophagectomy: is it a useful addition? Ann Thorac Surg. 2010;89:S2156–8. doi: 10.1016/j.athoracsur.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 6.Dragstedt LR, Camp EH. Follow-up of gastric vagotomy alone in the treatment of peptic ulcer. Gastroenterology. 1948;11:460–5. [PubMed] [Google Scholar]
- 7.Bonavina L. Comments on the publication “Effect of pyloric drainage procedures on gastric passage and bile reflux after esophagectomy with gastric conduit reconstruction by Palmes et al.”. Arch Surg. 2007;393:117–8. doi: 10.1007/s00423-007-0242-x. [DOI] [PubMed] [Google Scholar]
- 8.Holscher AH, Schneider PM, Gutschow C, Schroder W. Laparoscopic ischemic conditioning of the stomach for esophageal replacement. Ann Surg. 2007;245:241–6. doi: 10.1097/01.sla.0000245847.40779.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim J-H, Lee H-S, Kim MS, Lee JM, Kim SK, Zo JI. Balloon dilatation of the pylorus for delayed gastric emptying after esophagectomy. Eur J Cardiohthor Surg. 2008;33:1105–11. doi: 10.1016/j.ejcts.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Lee HS, Kim MS, Lee JM, Kim SK, Kang KW, Zo JI. Intrathoracic gastric emptying of solid food after esophagectomy for esophageal cancer. Ann Thorac Surg. 2005;80:443–7. doi: 10.1016/j.athoracsur.2005.02.049. [DOI] [PubMed] [Google Scholar]
- 11.Palmes D, Weilinghoff M, Colombo-Benkmann M, Senninger N, Bruewer M. Effect of pyloric drainage procedures on gastric passage and bile reflux after esophagectomy with gastric conduit reconstruction. Arch Surg. 2007;392:135–41. doi: 10.1007/s00423-006-0119-4. [DOI] [PubMed] [Google Scholar]
- 12.Swanson EW, Swanson SJ, Swanson RS. Endoscopic pyloric balloon dilatation obviates the need for pyloroplasty at esophagectomy. Surg Endosc. 2012;26:2023–8. doi: 10.1007/s00464-012-2151-5. [DOI] [PubMed] [Google Scholar]
- 13.Urschel JD, Blewett CJ, Young JEM, Miller JD, Bennett WF. Pyloric drainage (pyloroplasty) or no drainage in gastric reconstruction after esophagectomy: a meta-analysis of randomized controlled trials. Dig Surg. 2002;19:160–4. doi: 10.1159/000064206. [DOI] [PubMed] [Google Scholar]
- 14.Aly A, Jamieson GG. Reflux after oesophagectomy. Br J Surg. 2004;91:137–41. doi: 10.1002/bjs.4508. [DOI] [PubMed] [Google Scholar]
- 15.Martin JT, Federico JA, McKelvey AA, Kent MS, Fabian T. Prevention of Delayed Gastric Emptying After Esophagectomy: A Single Center's Experience With Botulinum Toxin. Ann Thorac Surg. 2009;87:1708–14. doi: 10.1016/j.athoracsur.2009.01.075. [DOI] [PubMed] [Google Scholar]
- 16.Gaur P, Swanson SJ. Should we continue to drain the pylorus in patients undergoing an esophagectomy? Dis Esophagus. 2013 doi: 10.1111/dote.12035. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.Khan OA, Manners J, Rengarajan A, Dunning J. Does pyloroplasty following esophagectomy improve early clinical outcomes? Interact Cardiovasc Thorac Surg. 2007;6:247–50. doi: 10.1510/icvts.2006.149500. [DOI] [PubMed] [Google Scholar]
- 18.Ben-David K, Sarosi GA, Cendan JC, Howard D, Rossidis G, Hochwald SN. Decreasing morbidity and mortality in 100 consecutive minimally invasive esophagectomies. Surg Endosc. 2012;26:162–7. doi: 10.1007/s00464-011-1846-3. [DOI] [PubMed] [Google Scholar]
- 19.Luketich JD, Pennathur A, Awais O, et al. Outcomes After Minimally Invasive Esophagectomy. Annals of Surgery. 2012;256:95–103. doi: 10.1097/SLA.0b013e3182590603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerfolio RJ, Bryant AS, Canon CL, Dhawan R, Eloubeidi MA. Is botulinum toxin injection of the pylorus during Ivor–Lewis esophagogastrectomy the optimal drainage strategy? J Thorac Cardiovasc Surg. 2009;137:565–72. doi: 10.1016/j.jtcvs.2008.08.049. [DOI] [PubMed] [Google Scholar]
- 21.Kent MS, Pennathur A, Fabian T, et al. A pilot study of botulinum toxin injection for the treatment of delayed gastric emptying following esophagectomy. Surg Endosc. 2007;21:754–7. doi: 10.1007/s00464-007-9225-9. [DOI] [PubMed] [Google Scholar]
- 22.Lanuti M, de Delva PE, Wright CD, et al. Post-esophagectomy gastric outlet obstruction: role of pyloromyotomy and management with endoscopic pyloric dilatation. Eur J Cardiohthor Surg. 2007;31:149–53. doi: 10.1016/j.ejcts.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 23.Lanuti M, DeDelva P, Morse CR, et al. Management of Delayed Gastric Emptying After Esophagectomy With Endoscopic Balloon Dilatation of the Pylorus. Ann Thorac Surg. 2011;91:1019–24. doi: 10.1016/j.athoracsur.2010.12.055. [DOI] [PubMed] [Google Scholar]
- 24.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Lerut TT, Coosemans WW, De Leyn PP, Van Raemdonck DD. Gastroplasty: yes or no to gastric drainage procedure. Dis Esophagus. 2001;14:173–7. doi: 10.1046/j.1442-2050.2001.00207.x. [DOI] [PubMed] [Google Scholar]
- 26.Zieren HU, Muller JM, Jacobi CA, Pichlmaier H. [Should a pyloroplasty be carried out in stomach transposition after subtotal esophagectomy with esophago-gastric anastomosis at the neck? A prospective randomized study] Chirurg. 1995;66:319–25. [PubMed] [Google Scholar]
- 27.Bonavina L, Anselmino M, Ruol A, Borsato N, Peracchia A. [Functional evaluation of the intrathoracic stomach after esophagectomy for esophageal cancer] Minerva Chir. 1991;46:247–51. [PubMed] [Google Scholar]
- 28.Wang LS, Huang MH, Huang BS, Chien KY. Gastric substitution for resectable carcinoma of the esophagus: an analysis of 368 cases. Ann Thorac Surg. 1992;53:289–94. doi: 10.1016/0003-4975(92)91335-7. [DOI] [PubMed] [Google Scholar]
- 29.Mehran R, Rice D, El-Zein R, et al. Minimally invasive esophagectomy versus open esophagectomy, a symptom assessment study. Dis Esophagus. 2011;24:147–52. doi: 10.1111/j.1442-2050.2010.01113.x. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen NT, Dholakia C, Nguyen XM, Reavis K. Outcomes of minimally invasive esophagectomy without pyloroplasty: analysis of 109 cases. Am Surg. 2010;76:1135–8. [PubMed] [Google Scholar]
- 31.Bemelman WA, Taat CW, Slors JF, van Lanschot JJ, Obertop H. Delayed postoperative emptying after esophageal resection is dependent on the size of the gastric substitute. J Am Coll Surg. 1995;180:461–4. [PubMed] [Google Scholar]
- 32.Oezcelik A, DeMeester SR, Hindoyan K, et al. Circular stapled pyloroplasty: a fast and effective technique for pyloric disruption during esophagectomy with gastric pull-up. Dis Esophagus. 2011;24:423–9. doi: 10.1111/j.1442-2050.2010.01169.x. [DOI] [PubMed] [Google Scholar]
- 33.Oezcelik A, DeMeester SR. Circular stapled pyloroplasty during esophagectomy with gastric pull-up. Semin Thorac Cardiovasc Surg. 2010;22:341–4. doi: 10.1053/j.semtcvs.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Collard JM, Romagnoli R, Otte JB, Kestens PJ. The denervated stomach as an esophageal substitute is a contractile organ. Annals of Surgery. 1998;227:33–9. doi: 10.1097/00000658-199801000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johansson J, Sloth M, Bajc M, Walther B. Radioisotope evaluation of the esophageal remnant and the gastric conduit after gastric pull-up esophagectomy. Surgery. 1999;125:297–303. [PubMed] [Google Scholar]
- 36.Schaaf M, Johar A, Lagergren P, et al. Surgical Prevention of Reflux after Esophagectomy for Cancer. Annals of Surgical Oncology. 2013 doi: 10.1245/s10434-013-3041-3. Epub 6 June 2013. [DOI] [PubMed] [Google Scholar]


