Abstract
Background
Our aim was to investigate the pattern of self reported symptoms and utilisation of health care services in Norway.
Design and Methods
With data from the cross-sectional Tromsø Study (2007-8), we estimated population proportions reporting symptoms and use of seven different health services. By logistic regression we estimated differences according to age and gender.
Results
In this study 12,982 persons aged 30-87 years participated, constituting 65.7% of those invited. More than 900/1000 reported symptoms or health problems in a year as well as in a month, and 214/1000 and 816/1000 visited a general practitioner once or more in a month and a year, respectively. The corresponding figures were 91/1000 and 421/1000 for specialist outpatient visits, and 14/1000 and 116/1000 for hospitalisations. Physiotherapists were visited by 210/1000, chiropractors by 76/1000, complementary and alternative medical providers by 127/1000, and dentists by 692/1000 in a year. Women used most health care services more than men, but genders used hospitalisations and chiropractors equally. Utilisation of all services increased with age, except chiropractors, dentists and complementary and alternative medical providers.
Conclusions
Almost the entire population reported health related problems during the previous year, and most residents visited a general practitioner. Yet there were high rates of inpatient and outpatient specialist utilisation. We suggest that wide use of general practitioners may not necessarily keep patients out of specialist care and hospitals.
Acknowledgments
the authors would like to thank Tor Anvik for a significant contribution in developing the idea for the study, Tom Wilsgård for useful discussions about the statistical analyses and Jarl-Stian Olsen for graphic design of the figures. They would also thank the people of Tromsø and The Tromsø Study for giving data to this study. Northern Norway Regional Health Authority and The University of Tromsø funded this research.
Key words: cross-sectional study, health care utilisation, general practitioner, specialist, hospitalisation
Significance for public health
Proper planning and development of health care services is important in any society’s effort to prevent and cure disease and promote health. A population-based perspective is mandatory in this endeavour. Data from a large population survey made it possible for us to analyse self- reported symptoms and disease, and self reported utilisation of seven health care services both in primary and secondary care. We found that almost the entire population reported symptoms or health related problems during the previous year. Although 816/1000 visited a general practitioner, 421/1000 received specialist outpatient care and 116/1000 were hospitalised. We suggest that wide use of general practitioners may not necessarily keep patients out of specialist care and hospitals. Our paper should be of interest to public health professionals and policymakers involved in planning and development of health care services.
Introduction
In 1961 White published The Ecology of Medical Care, estimating self-reported illness, injuries and health care behaviour in a population.1 Presented as cubes, showing the proportion of people using different health care settings in an average month, these patient-centred and population-based estimates have provided a framework for thinking about the organisation and utilisation of health care. Expanded and updated studies with monthly rates for a broad range of health care services were later undertaken in the USA2-4 and Asia,5,6 but until now not in Europe. Annual rates for health care services utilisation are available in many countries, but seldom studied in relation to monthly rates.
The Norwegian health care system has a high share of public financing and universal health insurance for every citizen. Specialist services, consisting of hospitals and outpatient specialist clinics, are mainly owned by the state and operated by regional health enterprises. Emergency admissions account for more than 60% of all hospitalisations.7,8 Access to specialist care is as a rule achieved by referral from general practitioners (GPs) or GP based municipality emergency clinics (the gatekeeper role). Primary health care, including GPs, physiotherapists and chiropractors, is run by the municipalities. The patient-list system was introduced in 2001, offering all residents a GP as their regular doctor. GPs report more competition, greater responsibility and higher expectations from patients in this context, and less consciousness of the gatekeeper role.9 GP and specialist outpatient visits are co-paid by a small fee by adults, but hospital admissions are free. Dentists and complementary and alternative medical providers (CAM) are usually organized outside the above-mentioned system and most often fully paid by adult patients.
Norway is considered one of the best countries to live in with high scores on population health parameters.10 Health care services, and GPs in particular, are well regarded in the population.11 Nevertheless, patient-assessed health services quality scores were only average or less in most areas according to Commonwealth Fund’s international comparisons of 11 western countries.12 The poorest scores were found along the themes general view and quality of health services, medical errors, information sharing, communication, and coordination between different health services. Norway scored better than average on access to a regular doctor and access to out-of-hours service.12 Despite shortcomings, we would assume that a universal health insurance, an established usual source of care, general practitioners with a good reputation, and a high user-assessed access to a regular doctor would give a high utilisation of GP visits, and a correspondingly low utilisation of inpatient and outpatient specialist care.4,13
With data from the comprehensive Tromsø Study we aimed to investigate the pattern of health care utilisation among adults aged 30 years and over, focusing on the prevalence of self-reported symptoms and utilisation of health care services, and differences according to age and gender.
Design and Methods
Tromsø is the largest municipality in Northern Norway, with 65,286 inhabitants (January 2008). The municipality is roughly equivalent to Norway as a whole for key parameters like unemployment, income per capita, proportion of disability pensioners, number of primary care physicians per 10,000 residents, and the proportion living in urban areas.14 Tromsø hosts the University Hospital of Northern Norway, which is also a local hospital for Tromsø and surrounding areas.
Population based health surveys have been conducted in Tromsø since 1974. The cross sectional sixth Tromsø Study (Tromsø 6) was conducted from October 2007 to December 2008, and consisted of comprehensive questionnaires, clinical examination and laboratory tests. Four groups were invited; every resident aged 40-42 or 60-87 years (n=12,578), a 10% random sample of individuals aged 30-39 (n=1056), a 40% random sample of people aged 43-59 (n= 5787) and subjects who had attended the follow-up visit of the fourth Tromsø Study, if not already included in the previous groups (n=341).
Our data were collected from two questionnaires; the first mailed with the invitation about two weeks ahead of suggested appointment time, and the second handed out at attendance. Both questionnaires and further details about enrolment methods, attendees and non-attendees are available at the Tromsø Study website,15 and elsewhere.16
The study includes 16 outcome variables, one for symptoms and seven for utilisation of different health care services in a year, and similar variables for a month. All outcome variables were dichotomous, with yes and no as possible answers. For each health care setting the respondents were asked whether they had used the service the previous year, and if so, how many times.15 For our purpose, we merged the four specialist outpatient categories (psychologist or psychiatrist, somatic specialist outside hospital, hospital psychiatric outpatient clinic, and hospital somatic outpatient clinic) into one category. We used the reported number of annual visits to estimate the proportion participating in the different types of health care in a month. The value was set to zero if the respondent reported no use during the previous year. Otherwise, missing values were substituted with the average number of visits for each health care service by gender and age group. We then divided the estimated number of annual visits by 12, followed by generating a dichotomous variable for monthly use for each service, based on the assumption that zero indicated no use, and one or more indicated use. Numbers between zero and one were included in a calculation of the sample proportion of monthly use.
Respondents reporting symptoms or health problems, occasional or regular medication, or bad or very bad health were counted as having had symptoms during the given period. The following symptoms, health problems and medications were included in the symptom variable: illness or injury in general, much or very much fear, anxiousness, dizziness, insomnia or depression, inability to wash, dress or perform usual activities, dyspnoea, much more than usual unable to cope with difficulties, memory problems with consequences for daily life, periodic daily cough, headache, nausea, reflux, diarrhoea, constipation, bloating, or musculoskeletal, abdominal or other chronic pain, use of painkillers, antihypertensives, lipid lowering drugs, heart disease medication, diuretics, osteoporosis medication, insulin, diabetes tablets, thyroxin, sleeping pills, tranquilisers, or antidepressants.
Descriptive analysis was performed to describe sample characteristics and to estimate the proportion per 1000 who had symptoms or received health care from different sources in the previous month and year. To permit inferences for the Norwegian population, proportions were adjusted for gender and age in 10 year age groups by the use of weights, equivalent to the method of direct standardization. To illustrate patterns of utilisation, we calculated the ratios of annual/monthly rates for the different health services. A low ratio implies a tendency for repeated visits by each participant. We performed multivariate logistic regression analyses to estimate the likelihood of reporting symptoms or participating in care during a year attributable to the independent variables age and gender. The largest groups were reference categories. All analyses were done in Stata version 12.0. The Tromsø Study and the protocol for this particular project were approved by The Regional Committee of Research Ethics.
Results
Sample characteristics are presented in Table 1. All together 12,982 persons aged 30-87 years participated, 65.7% of those invited, and 33.8% of the total population in this age group in Tromsø. Compared to men more women participated, and more women lived in lower income and single person households. Those with high education, high middle income, good health, and those living with a spouse made up the largest groups in both genders (Table 1).
Table 1.
Sample distribution according to age, household income, education, living with a spouse and self-rated health, for total sample and by gender
| Total sample n=12,982 | Males n=6053 | Females n=6929 | ||||
|---|---|---|---|---|---|---|
| n* | %° | n* | %° | n* | %° | |
| Age | ||||||
| 30-39 | 509 | 3.9 | 212 | 3.5 | 297 | 4.3 |
| 40-49 | 3574 | 27.5 | 1662 | 27.5 | 1912 | 27.6 |
| 50-59 | 2436 | 18.8 | 1147 | 18.9 | 1289 | 18.6 |
| 60-69 | 4103 | 31.6 | 1995 | 33.0 | 2108 | 30.4 |
| 70-79 | 1829 | 14.1 | 841 | 13.9 | 988 | 14.3 |
| 80-87 | 531 | 4.1 | 196 | 3.2 | 335 | 4.8 |
| Living with a spouse# | ||||||
| No | 3127 | 24.9 | 1063 | 17.9 | 2064 | 31.2 |
| Yes | 9432 | 75.1 | 4869 | 82.1 | 4563 | 68.8 |
| Income§ | ||||||
| Low | 1456 | 12.2 | 468 | 8.1 | 988 | 16.0 |
| Low middle | 3191 | 26.7 | 1402 | 24.2 | 1789 | 29.0 |
| High middle | 4220 | 35.2 | 2247 | 38.8 | 1973 | 31.9 |
| High | 3101 | 25.9 | 1671 | 28.9 | 1430 | 23.1 |
| Education^ | ||||||
| Low | 3673 | 28.7 | 1494 | 25.0 | 2179 | 31.9 |
| Middle | 4289 | 33.5 | 2119 | 35.5 | 2170 | 31.8 |
| High | 4837 | 37.8 | 2362 | 39.5 | 2475 | 36.3 |
| Self-rated health | ||||||
| Bad$ | 699 | 5.4 | 286 | 4.8 | 413 | 6.0 |
| Fair | 3699 | 28.8 | 1693 | 28.2 | 2006 | 29.3 |
| Good | 6593 | 51.2 | 3206 | 53.3 | 3387 | 49.4 |
| Excellent | 1873 | 14.6 | 824 | 13.7 | 1049 | 15.3 |
*Summarized numbers may vary for the different variables due to missing values
°row percentage
#living with a spouse or cohabitant
§household total gross income (low: <200,000 NOK, low middle: 201-400,000 NOK, high middle: 401-700,000 NOK, and high: >700,000 NOK)
^highest completed education (low: primary and part of secondary school, middle: high school, high: college or university)
$the bad and very bad categories from the questionnaire are merged.
In line with the tradition initiated by White, we used ecology cubes to present the proportion of the population who used the different health services once or more in an average month (Figure 1) and year (Figure 2). Almost the entire population reported symptoms or health problems in a year as well as in a month. The highest annual/monthly rate ratio was found for hospitalisation (8.3) and the lowest for physiotherapy (1.5). The ratio was 6.0 for dentist, 4.6 for specialist outpatient clinic, 3.8 for GP and 2.3 for CAM and chiropractor.
Figure 1.
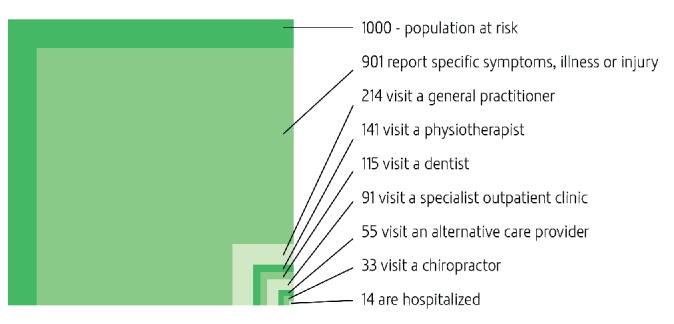
Monthly prevalence estimates of self-reported symptoms and illnesses, and use of different health care services for persons 30 years and over.
Figure 2.
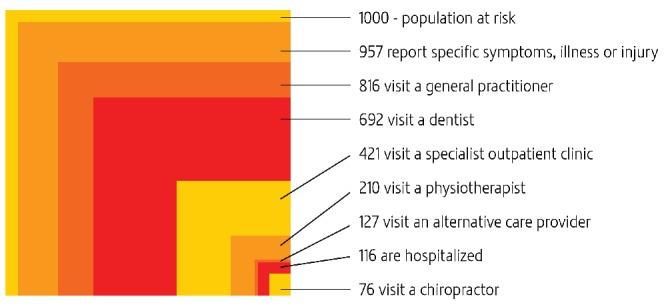
Annual prevalence estimates of self-reported symptoms and illnesses, and use of different health care services for persons 30 years and over.
Table 2 shows how annual symptoms and health care participation rates vary by age for each gender. As a general trend, annual symptoms and disease, use of GP, physiotherapist, specialist outpatient clinic and hospitalisation increased with age, whereas use of chiropractors and CAM decreased with age in both genders. Dentist utilisation peaked in the age group 50-59 years.
Table 2.
Annual prevalence rates of symptoms and disease, visits to general practitioner, specialist outpatient clinic, hospital admissions, visits to physiotherapist, chiropractor, complementary and alternative provider, and dentist, by gender and age.
| Males by age | Symptoms and disease n/N rate/1000 (95% CI) | General practitioner n/N rate/1000 (95% CI) | Specialist outpatient clinic n/N rate/1000 (95% CI) | Hospital admission n/N rate/1000 (95% CI) | Physiotherapist n/N rate/1000 (95% CI) | Chiropractor n/N rate/1000 (95% CI) | CAM n/N rate/1000 (95% CI) | Dentist n/N rate/1000 (95% CI) |
|---|---|---|---|---|---|---|---|---|
| 30-39 | 191/212 901 (860-941) |
152/210 724 (663-785) |
62/206 301 (238-364) |
10/210 48 (19-77) |
21/207 101 (60-143) |
17/206 83 (45-120) |
19/202 94 (53-135) |
117/209 560 (492-628) |
| 40-49 | 1541/1662 927 (915-940) |
1127/1651 683 (660-705) |
490/1612 304 (281-326) |
118/1653 71 (59-84) |
270/1634 165 (147-183) |
145/1629 89 (75-103) |
132/1607 82 (69-96) |
1164/1646 707 (685-729) |
| 50-59 | 1085/1147 946 (933-959) |
870/1136 766 (741-791) |
427/1106 386 (357-415) |
115/1135 101 (84-119) |
212/1109 191 (168-214) |
85/1096 78 (62-93) |
88/1079 82 (65-98) |
853/1124 759 (734-784) |
| 60-69 | 1899/1995 952 (942-961) |
1633/1983 823 (807-840) |
836/1893 442 (419-464) |
261/1964 133 (118-148) |
361/1913 189 (171-206) |
150/1884 80 (67-92) |
136/1841 74 (62-86) |
1412/1953 723 (703-743) |
| 70-79 | 818/841 973 (962-984) |
768/833 922 (904-940) |
400/771 519 (483-554) |
164/824 199 (172-226) |
150/786 191 (163-218) |
38/779 49 (34-64) |
46/769 60 (43-77) |
481/809 595 (561-628) |
| 80-87 | 188/196 959 (931-987) |
177/193 917 (878-956) |
80/159 503 (425-582) |
38/192 198 (141-255) |
39/170 229 (166-293) |
9/168 54 (19-88) |
7/157 45 (12-77) |
83/178 466 (392-540) |
| All ages | 5722/6053 945 (940-951) |
4727/6006 787 (777-797) |
2295/5747 399 (387-412) |
706/5978 118 (110-126) |
1053/5819 181 (171-191) |
444/5762 77 (70-84) |
428/5655 76 (69-83) |
4110/5919 694 (683-706) |
| Females by age | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) | n/N rate/1000 (95% CI) |
| 30-39 | 288/297 970 (950-989) |
253/296 855 (814-895) |
126/278 453 (394-512) |
46/296 155 (114-197) |
60/287 209 (162-256) |
24/285 84 (52-117) |
57/282 202 (155-249) |
184/290 634 (579-690) |
| 40-49 | 1862/1912 974 (967-981) |
1560/1895 823 (806-840) |
810/1832 442 (419-465) |
189/1894 100 (86-113) |
415/1864 223 (204-242) |
158/1833 86 (73-99) |
317/1801 176 (158-194) |
1410/1889 746 (727-766) |
| 50-59 | 1258/1289 976 (968-984) |
1065/1276 835 (814-855) |
575/1226 469 (441-497) |
92/1271 72 (58-87) |
350/1242 282 (257-307) |
105/1206 87 (71-103) |
219/1200 183 (161-204) |
1068/1265 844 (824-864) |
| 60-69 | 2078/2108 986 (981-991) |
1809/2081 869 (855-884) |
907/1935 469 (446-491) |
263/2066 127 (113-142) |
524/1977 265 (246-285) |
104/1934 54 (44-64) |
267/1899 141 (125-156) |
1532/2035 753 (734-772) |
| 70-79 | 968/988 980 (971-989) |
904/970 932 (916-948) |
430/845 509 (475-543) |
145/944 154 (131-177) |
277/899 308 (278-338) |
43/865 50 (35-64) |
101/836 121 (99-143) |
591/931 635 (604-666) |
| 80-87 | 333/335 994 (986-1002) |
306/326 939 (912-965) |
149/274 544 (484-603) |
85/320 266 (217-314) |
91/283 322 (267-376) |
8/268 30 (9-50) |
34/264 129 (88-169) |
151/284 532 (473-590) |
| All ages | 6787/6929 980 (976-983) |
5897/6844 862 (853-870) |
2997/6390 469 (457-481) |
820/6791 121 (113-128) |
1717/6552 262 (251-273) |
442/6391 69 (63-75) |
995/6282 158 (149-167) |
4936/6694 737 (727-748) |
CAM, complementary and alternative medical provider; n/N, proportion number/total number; CI, confidence interval.
In multivariate logistic regressions, men were less likely than women to report symptoms and disease. Similarly, utilisation of health care services was lower among men than women, except for hospital admissions and chiropractors (Table 3).
Table 3.
Multivariate logistic regressions of symptoms and use of health care services during the last year, according to gender and age
| Symptoms and disease | General practitioner | Specialist outpatient clinic | Hospital admission | Physiotherapist | Chiropractor | CAM | Dentist | |
|---|---|---|---|---|---|---|---|---|
| OR 95% CI | OR 95% CI | OR 95% CI | OR 95% CI | OR 95% CI | OR 95% CI | OR 95% CI | OR 95% CI | |
| Gender | ||||||||
| Male | 0.36 | 0.59 | 0.75 | 0.99 | 0.62 | 1.12 | 0.44 | 0.79 |
| 0.29-0.44 | 0.54-0.65 | 0.70-0.81 | 0.89-1.10 | 0.57-0.68 | 0.98-1.29 | 0.39-0.49 | 0.73-0.85 | |
| Female* | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Age | ||||||||
| 30-39 | 0.47 | 0.69 | 0.74 | 0.83 | 0.64 | 1.29 | 1.46 | 0.53 |
| 0.31-0.71 | 0.55-0.88 | 0.61-0.90 | 0.62-1.11 | 0.50-0.82 | 0.91-1.82 | 1.12-1.92 | 0.44-0.64 | |
| 40-49 | 0.62 | 0.56 | 0.72 | 0.63 | 0.82 | 1.35 | 1.24 | 0.94 |
| 0.49-0.78 | 0.49-0.62 | 0.65-0.79 | 0.55-0.74 | 0.73-0.91 | 1.13-1.61 | 1.07-1.43 | 0.85-1.05 | |
| 50-59 | 0.78 | 0.72 | 0.90 | 0.63 | 1.06 | 1.26 | 1.28 | 1.45 |
| 0.60-1.03 | 0.63-0.83 | 0.81-0.99 | 0.53-0.75 | 0.94-1.19 | 1.04-1.54 | 1.09-1.50 | 1.28-1.64 | |
| 60-69* | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 70-79 | 1.28 | 2.29 | 1.26 | 1.42 | 1.14 | 0.73 | 0.82 | 0.56 |
| 0.90-1.83 | 1.88-2.79 | 1.12-1.41 | 1.22-1.65 | 1.00-1.30 | 0.56-0.94 | 0.67-1.01 | 0.50-0.64 | |
| 80-87 | 1.47 | 2.29 | 1.30 | 2.11 | 1.30 | 0.58 | 0.81 | 0.35 |
| 0.77-2.82 | 1.61-3.25 | 1.06-1.58 | 1.69-2.64 | 1.04-1.61 | 0.35-0.95 | 0.58-1.14 | 0.29-0.43 | |
CAM, complementary and alternative medical provider; OR, odds ratio; CI, confidence interval
*reference category.
Discussion
To the best of our knowledge, our study represents the first attempt to map the ecology of health care, both in the context of a Scandinavian society, as well as in Europe. Nearly the entire study population reported health related problems during the previous month and year, and the vast majority received health care, mostly in primary care services.
Although several studies of health care utilisation have been conducted with partly the same methodology (Table 4), comparisons are difficult due to sample composition, cross-national differences in organisation, distribution, and access to health care as well as cultural aspects. Nevertheless, our findings are intriguing both in the light of previous studies, and ongoing debates on health care reforms and the interaction between primary and specialist health care services.11,17
Table 4.
Estimated proportion per 1000 in different populations at different times reporting symptoms or using health care services once or more during an average month.
| Place (time of data collection) | Age | Symptoms or illness | General practitioner | First line physician | Specialist outpatient clinic | Admitted to hospital | Dentist | CAM |
|---|---|---|---|---|---|---|---|---|
| UK and US (1928-59)1 |
16 and over | 750 | - | 250 | - | 9 | - | - |
| US (1996)2 |
All ages | 800 | 113 | 217 | 21 | 8 | - | 65 |
| US (1996)3 |
18 and over | - | - | 235 | 26 | 10 | 73 | - |
| Hong Kong (2002)5 |
All ages | 567 | - | 372 | 68 | 7 | - | 54* |
| Japan (2003)6 |
All ages | 862 | 232 | 307 | 88 | 7 | - | 49 |
| Present study Norway (2007-8) | 30-87 | 901 | 214 | - | 91 | 14 | 115 | 55 |
CAM, complementary and alternative medical provider
*traditional Chinese medical practitioner.
More respondents reported symptoms or illness during a month and a year than in any other ecology study (Table 4). This is not likely to reflect a higher morbidity than in other populations,10 but may be due to sample age and the construction of this variable, focusing a broad range of specific symptoms and medications. The high rates may also indicate a great interest in, and awareness of, health issues in the population.
We found a lower monthly rate of visits to physicians who provide services directly to patients each month than in the US, Japan and Hong Kong, despite the higher age in our sample (Table 4). This is surprising due to the national health insurance coverage and access for all to a primary care doctor, and suggests that good access does not necessarily lead to higher utilisation. The annual rate, however, is relatively high compared to the averages of western countries as reported by the Organisation for Economic Cooperation and Development (OECD).18 The high annual/monthly rate ratio indicates a wide outreach in the population, but less repeated visits by each individual during the year.
The use of physiotherapy, chiropractors and CAM seem to be roughly in line with other developed countries,19,20 which suggests that there is no obvious substitution effect between the different services with direct access.
Monthly specialist outpatient utilisation rates are quite similar to Japan and Hong Kong, but much higher than the US rates (Table 4). Wide between-country variation has been found for annual rates too, and our rate is a little lower than the OECD averages of western countries.21 This probably reflects the large variation in specialist outpatient clinics roles in different health care systems. However, as monthly visit rates were found to be low for GPs and high for specialist outpatient clinics compared to other western countries, one might ask whether there is a substitution effect. This could indicate a lower GP awareness of the gatekeeper role. 9
We found the highest monthly hospitalisation rate, twice as high as in the Asian studies (Table 4). Likewise, the proportion admitted to hospital in a year was well above the average of western OECD countries.18 Our sample age composition might have contributed, but is unlikely to explain it all. Rates above the OECD average are found by others as well.22,23 Hospitalisations are particularly interesting since they are expensive and often represent major events in people’s lives. Rates are suggested to vary by access to primary care and continuity of care (inversely), access to hospital care and number of hospital beds (directly),24-27 economic conditions in the community28 and treatment available in outpatient and inpatient care.29 Studies from the US and England have shown that reductions in hospitalisations are associated with high proportions of primary care physicians relative to specialists.30,31 In Norway the proportion of primary care physicians was 29% in 2007,32 which is considered low.33
Barbara Starfield has set forth the hypothesis that a qualitatively well functioning primary care system prevents hospital admissions.34 Under the assumption that Norway has a well-functioning primary care, the combination of a high hospitalisation rate and a high annual rate of GP visits in our study is surprising. However, Norwegian health care services might not be as well-functioning as we like to believe. Despite good access, shortcomings related to lack of communication and coordination between different levels of care has been reported.12 Our findings do not allow any firm conclusions about the quality of health care services, nor the validity of Starfield’s hypothesis. Both may be sensitive to content, organisation and volume of health care services. In addition, it is well documented that health care consumption is supply-sensitive, and that demand both for primary and hospital care is influenced by the current offer.17,30,31 The reform on integrated care in Norway suggests strengthening primary health care by more GPs, aiming among other things at halting the growth in specialist care expenditure.11 As a single action, this may not necessarily reduce hospitalisations.
The present study has some limitations. Despite a high response rate, our sample may not be entirely representative of the general population. It is well known that women, married/cohabitants, higher socio-economic groups and healthier persons are more likely to participate in population surveys.35 However, the direction of a possible bias caused by these factors is not obvious, and might vary for different health services.18 In Tromsø 6, attendees were older, and the proportions of married/cohabitants and women were higher than in non-attendees,15,16 probably leading to higher estimates of health care utilisation. On the other hand, the potential for recall bias might lead to lower estimates, especially for minor events and distant past.36 All in all, we do not think that our main conclusions are threatened by these possible biases. Furthermore, the outcome measures were limited to use or not use of health services, and neither the volume of use nor the need for care was measured. Also, the method used does not establish causal relationships. Particular strengths of this study are the large sample size and the comprehensive coverage of symptoms and health problems in the questionnaires.
This study has provided necessary overall information on patterns of health care utilisation across age and gender, by describing both monthly and annual utilisation rates for seven health care services in a Scandinavian context. We have shown that Norway has high rate of inpatient specialist utilisation compared to most other countries, despite a high annual contact rate between GPs and the population. Our data suggests that wide use of GP services may not necessarily keep patients out of specialist care and hospitals. This could have implications for policymakers and public health professionals involved in health care planning and health care reforms. The complex interaction between health care services needs more attention in future research and development of health policy.
References
- 1.White KL, Williams TF, Greenberg BG.The ecology of medical care. N Engl J Med 1961;265:885-92 [DOI] [PubMed] [Google Scholar]
- 2.Green LA, Fryer GE, Yawn B P, Lanier D, Dovey SM.The ecology of medical care revisited. N Engl J Med 2001;26:2021-25 [DOI] [PubMed] [Google Scholar]
- 3.Dovey SM, Weitzman M, Fryer GE, et al. The ecology of medical care for children in the United States. Pediatrics 2003;111:1024-29 [DOI] [PubMed] [Google Scholar]
- 4.Fryer GE, Green LA, Dovey SM, et al. Variation in the Ecology of Medical Care. Ann Fam Med 2003;2:81-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung GM, Wong IOL, Chan WS, et al. The ecology of health care in Hong Kong. Soc Sci Med 2005;61:577-90 [DOI] [PubMed] [Google Scholar]
- 6.Fukui T, Rhaman M, Takahashi O, et al. The Ecology of Medical Care in Japan. JMAJ 2005;4:163-67 [Google Scholar]
- 7.Eikeland G, Garåsen H, Jacobsen G.[Are there alternatives to emergency admissions?]. [Article in Norwegian]. Tidsskr Nor Lægeforen 2005;125:2355-7 [PubMed] [Google Scholar]
- 8.Statistics Norway. More women than men to hospital. Accessed on: 2 June2012. Available from: http://www.ssb.no/pasient/ [Google Scholar]
- 9.Carlsen B, Norheim OF.Introduction of the patient-list system in general practice. Changes in Norwegian physician’s perception of their gatekeeper role. Scand J Prim Health Care 2003;21:209-13 [DOI] [PubMed] [Google Scholar]
- 10.Organisation for European Economic Co-operation (OECD). Health Data 2011. How Does Norway Compare. Accessed on: 13 March2012. Available from: http://www.oecd.org/dataoecd/43/23/40905066.pdf [Google Scholar]
- 11.Norwegian Ministry of Health Care Services. Reform on integrated care. Proper treatment – at the right place and time. Report No. 47 to the Storting2009 [Google Scholar]
- 12.Holmboe O, Iversen HH, Sjetne IS, Skudal KE.The 2011 Commonwealth Fund survey among sicker adults: Results from a comparative survey in 11 countries. The Norwegian Knowledge Centre for the Health Services 2011. Accessed on: 2 June 2012. Available from: http://www.kunnskapssenteret.no/Publikasjoner/Commonwealth+Fund-unders%C3%B8kelsen+i+2011+blant+utvalgte+pasientgrupper%3A+Resultater+fra+en+komparativ+unders%C3%B8kelse+i+11+land*.13747.cms?threep-agenor=1. [Google Scholar]
- 13.Suominen-Taipale AL, Koskinen S, Martelin T, et al. Differences in older adults’ use of primary and specialist care services in two Nordic countries. Eur J Public Health 2004;14:375-80 [DOI] [PubMed] [Google Scholar]
- 14.Municipality of Tromsø. Facts about Tromsø Municipality. Accessed on: 29 February2012. Available from: http://www.tromso.kommune.no/fakta-om-tromsoe-kommune.241052.no.html [Google Scholar]
- 15.The Tromsø Study website. Accessed on: 2 June2012. Available from: http://en.uit.no/ansatte/organisasjon/artikkel?p_document_id=104991&p_dimension_id=88111&p_menu=42374 [Google Scholar]
- 16.Jakobsen BK, Eggen AL, Matiesen E, et al. Cohort profile: The Tromsø Study. Int J Epidemiol 2011 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wennberg JE, Fisher ES, Skinner JS.Geography and the debate over Medicare reform. Health Affairs 2002. Web exclusive. Accessed on: 15 June2012. Available from: http://content.healthaffairs.org/cgi/content/full/ hlthaff.w2.96v1/DC1. [DOI] [PubMed] [Google Scholar]
- 18.Van Doorslaer E, Masseria C.OECD Health Equity Research Group. Income-Related Inequality in the Use of Medical Care in 21 OECD Countries. Towards high-performing health systems: Policy studies. Paris: OECD; 2004. Accessed on: 11 April 2012. Available from: http://www.oecd.org/dataoecd/14/0/31743034.pdf [Google Scholar]
- 19.Reijneveld SA, Stronks K.The validity of self-reported use of health care across socioeconomic strata: a comparison of survey and registration data. Int J Epidemiol 2001;30:1407-14 [DOI] [PubMed] [Google Scholar]
- 20.Lawrence DJ, Mecker WC.Chiropractic and CAM utilisation: adescriptive review. Chiropr Osteopat 2007;15:2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Doorslaer E, Masseria C, Koolman X.The OECD Health Equity Research Group. Inequalities in access to medical care by income in developed countries. CMAJ 2006;174:177-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Statistics Norway. Living Conditions Survey Norway 2008. Accessed on: 2 June2012. Available from: http://statbank.ssb.no/statistikkbanken/Default_FR.asp?PXSid=0&nvl=true&PLanguage=0&tilside=selectvarval/define.asp&Tabellid=04217 [Google Scholar]
- 23.Godager G, Iversen T.[Users’ experiences of general practitioner scheme 2001-2008. Trends in use, availability and satisfaction]. [Article in Norwegian]. University of Oslo, Helseøkonomisk forskningsprogram. Skriftserie2010:1 [Google Scholar]
- 24.Saha S, Solotaroff R, Oster A, Bindman A.Are preventable hospitalizations sensitive to changes in access to primary care? The case of the Oregon health plan. Med Care 2007;45:712-19 [DOI] [PubMed] [Google Scholar]
- 25.Bindman A, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA 1995;274:305-11 [PubMed] [Google Scholar]
- 26.Menec VH, Sirski M, Attawar D, Katz A.Does continuity of care with a family physician reduce hospitalizations among older adults? J Health Serv Res policy 2006;11:196-201 [DOI] [PubMed] [Google Scholar]
- 27.Wilson DM, Truman CD.Does the availability of hospital beds affect utilization patterns? The case of end-of-life care. Health Serv Manage Res 2001;14:229-39 [DOI] [PubMed] [Google Scholar]
- 28.Ricketts TC, Randolph R, Howard HA, et al. Hospitalization rates as indicators of access to primary care. Health Place 2001;7:27-38 [DOI] [PubMed] [Google Scholar]
- 29.Mosterd A, Reitsma JB, Grobbee DE.Angiotensin converting enzyme inhibition and hospitalisation for heart failure in the Netherlands, 1980 to 1999: the end of an epidemic? Heart 2002; 87:75-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kravet SJ, Shore AD, Miller R, et al. Health care utilization and the proportion of primary care physicians. Am J Med 2008;121:142-8 [DOI] [PubMed] [Google Scholar]
- 31.Gulliford MC.Avilability of primary care doctors and population health in England: is there an association? J Public Health Med 2002;24:252-4 [DOI] [PubMed] [Google Scholar]
- 32.Statistics Norway. Growth in the number of medical doctors. Accessed on: 29 February2012. Available from: http://www.ssb.no/samfunnsspeilet/utg/201102/09/ [Google Scholar]
- 33.Starfield B.Is primary care essential? Lancet 1994;344:1129-33 [DOI] [PubMed] [Google Scholar]
- 34.Starfield B, Shi L, Macinko J.Contribution of primary care to health systems and health. Milbank Q 2005;3:457-502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galea S, Tracy M.Participation rates in epidemiological studies. Ann Epidemiol 2007;17:643-53 [DOI] [PubMed] [Google Scholar]
- 36.Roberts RO, Bergstralh EJ, Schmidt L, Jacobsen SJ.Comparison of self-reported and medical record health care utilization measures. J Clin Epidemiol 1996;9:989-95 [DOI] [PubMed] [Google Scholar]


