Abstract
The aim of this research was to conduct a thorough review on the literature of tuberculosis in Canada and the Province of Quebec. To achieve this aim, an exhaustive literature review of tuberculosis in the Province of Quebec was undertaken. Data was collected with the goal of creating an epidemiological and public health evidence base to forecast the spread of tuberculosis. A keyword search strategy was used to find relevant articles from the peer-reviewed literature using the electronic search engine PubMed and a search of other relevant federal and provincial government databases. Twenty-nine peer-reviewed publications and twenty government reports containing information about the incidence or prevalence of tuberculosis in the Province of Quebec were included in the analysis. An analysis of the data revealed that while tuberculosis rates have been decreasing in both Canada and Quebec with an overall incidence below 3 per 100,000 of population in 2007, among immigrants and the Inuit communities in Quebec, the incidence and prevalence of the disease still remains high and reached 18 per 100,000 and 100 per 100,000, respectively in 2007. In general, while tuberculosis does not pose a significant burden to the general population, it does continue to affect certain sub-groups disproportionately, including select immigrants and Inuit communities in Quebec. Efforts to ensure that cost-effective healthcare interventions are delivered in a timely fashion should be pursued to reduce the associated morbidity and mortality of tuberculosis in the Province of Quebec.
Acknowledgments
Funding for this research was provided to Medmetrics Inc., by McGill University, Montreal, Quebec, Génome Québec and the Ministère de Développement Economique, Innovation et Exportation du Gouvernement du Québec.
The authors also wish to thank Drs. John White and Marcel Behr, both of McGill University and Dr Suneil Malik of the Infectious Disease Program in the Office of Biotechnology, Genomics and Population Health at the Public Health Agency of Canada for comments and suggestions on earlier drafts of this manuscript.
Key words: tuberculosis, Canada, Quebec, epidemiology, prevalence
Significance for public health
This article provides a timely review of the burden imposed by tuberculosis in the Canadian Province of Quebec. It reviews the existing literature on the epidemiology of tuberculosis in Quebec using both government and literature sources. In so doing, this article provides public health policy makers with an invaluable and updated review of the current prevalence of tuberculosis amongst at risk population groups in the Province of Quebec. Such information should be extremely helpful to planning current and future health intervention strategies designed to control and reduce the burden of illness posed by tuberculosis and to plan cost-effective and appropriate treatment and management options in an optimal manner.
Introduction
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis which typically affects the lungs. Globally, the prevalence of TB has reached epidemic levels, particularly in the developing world. Canada, by contrast, has one of the lowest incidences of TB in the world.1 In fact, TB rates have been falling in Canada since the 1970s.2 TB rates in the Province of Quebec have been lower than the Canadian average since 1986, but remain higher amongst certain populations, notably the Inuit and immigrants. This paper aims to highlight the epidemiological trends of TB in the Province of Quebec, particularly in regards to these two groups.
Throughout Canada and Quebec, TB is regarded as a reportable communicable disease and so official records provide a best estimate of the number of persons with tuberculosis in Canada and Quebec. Active TB requires immediate medical attention although M. tuberculosis infection can persist in a latent form. While treatment is often effective, drug resistant strains are known to occur.3 Co-infection with other diseases such as HIV further complicates the treatment of the disease and can increase the mortality and cost of treatment.4 There are many other risk factors for developing active TB from latent infection,5 including immunosuppressant conditions such as HIV and factors related to poverty such as alcoholism, drug abuse, and malnutrition. Proximity and contact with infected persons also greatly increases the risk of infection.5
The incidence of TB is over ten times greater in the Province of Quebec among immigrants compared to Canadian-born residents. The highest prevalence rates are among recent immigrants from countries with a high incidence of TB, notably Haiti, India, China, Vietnam, the Philippines and The Democratic Republic of Congo.6 Canada has among the highest migrant populations in the world.7 The cost of treatment of TB in Canada is a financial burden, averaging over $47,000 dollars per case annually.8 Active TB requires isolation and in rare cases intensive care, especially among multiple drug resistant cases, which while rare are potentially very costly to the healthcare system.
The rate among aboriginal populations is higher compared to non-Indigenous Canadian-born citizens. In Quebec, the greatest incidences are among the Inuit, where the incidence rates can approach 50 times that of the general population.2 While rates may be higher among non-Inuit Aboriginal Canadians than the non-Aboriginal population, the epidemiological trends within that group are not discussed due to the small number of cases, typically less than five per year.2 Other risk factors such as an increased genetic susceptibility,9 a changing diet away from vitamin D rich traditional diet towards a more Western diet, the increased prevalence of diabetes10-12 and smoking13-16 all potential contribute to high rates of TB amongst Quebec’s Inuit population, especially those on reserves versus off reserves. Nevertheless, while incidences are high, the low absolute numbers of Quebec’s Inuit population mean that there are often less than 10 cases per year. In Nunavik (the region in Northern Quebec home to many Inuit) communities, however, the lack of appropriate diagnostic medical facilities requires flying infected individuals to the nearest hospital, greatly increasing the cost of diagnosis and treatment. This paper aims to document the current epidemiological trends of tuberculosis in the Province of Quebec, with the goal of informing decision-makers about the cost-effectiveness of intervention strategies to reduce morbidity and mortality associated with tuberculosis in at risk populations.
Research methodology
A systematic literature review of tuberculosis epidemiology research in the Province of Quebec and Canada was performed. The primary electronic database service used was PubMed, a service provided by the National Institute of Health in the USA that is the primary interface for searching the MEDLINE database. The following keyword searches were used to find documents in PubMed: tuberculosis Quebec epidemiology, aboriginal tuberculosis Canada, aboriginal tuberculosis Quebec, Inuit tuberculosis Quebec, immigrant tuberculosis Canada, immigrant tuberculosis Quebec and incidence tuberculosis Quebec. The terms incidence and prevalence yielded redundant results.
Only literature that explicitly described the incidence or prevalence of tuberculosis cases occurring in the Province of Quebec was included for analysis. Twenty-nine of 226 peer-reviewed publications were deemed relevant and used as a basis for statistical analysis. These papers are summarised in Table 1. In addition, to the PubMed and Medline electronic search engines, The Cochrane database was searched with similar terms, but yielded nothing of use. In addition to the peer-reviewed literature, a fruitful source of data on the epidemiology of tuberculosis was to be found in reports compiled by the governments of Canada and the Province of Quebec. The most useful sources of epidemiologic information on the incidence and prevalence of tuberculosis in the Province of Quebec are also summarised in Table 1.
Table 1.
Summary of relevant literature.
| Document | Year | Cases | Years | Demographic | Additional notes of interest |
|---|---|---|---|---|---|
| Nguyen et al.1 | 2003 | 46 | 1990-2000 | Nunavik Inuit | |
| Menzies and Oxlade3 | 2006 | 1574 | 2004 | Canada | Cost of TB in Canada |
| Brassard4 | 1999 | 1500 | 1979-1996 | Quebec | |
| Rivest et al.17 | 1998 | 798 | 1992-1995 | Montreal | Complement official |
| Enarson and Grzybowski18 | 1986 | 28,000 | 1970-1981 | Canadian natives | |
| Gaudette and Ellit19 | 2003 | 2082 | 1984-1988 | Canada | TB in Canada |
| Frappier et al.20 | 1971 | 6000 | 1956-1961 | Quebec under 29 | Effect of vaccination |
| Ashikari and Menzies21 | 1995 | 782 | 1987-1991 | Montreal | |
| Menzies et al.22 | 1997 | 88 | 1987-1991 | Montreal children | |
| Dasgupta et al.23 | 2000 | 27 | 1996-1997 | Montreal | Cost analysis |
| Smeja24 | 2000 | 1274 | 1993-1998 | Quebec | Aboriginal TST |
| Kulaga et al.25 | 2002 | 303 | 1997-1998 | Montreal | |
| Dion et al.26 | 2002 | 112 | 1999-2000 | Montreal | Health preferences |
| Kulaga et al.27 | 2004 | 216 | 1996-1998 | Montreal | No evidence of founder effect for TB |
| Dion et al.28 | 2004 | 112 | 1999-2000 | Montreal | Preference among TB patients |
| Richards29 | 2005 | 322 | 1999-2000 | Montreal | TB surveillance new immigrant |
| Menzies30 | 2005 | 104 | 2002 | Montreal | Latent TB |
| Decarie et al.31 | 2005 | 66 | 2005 | Laurentians | |
| Harris et al.32 | 2006 | 3416 | 1997-1998 | Canada | Analysis of HIV co-infection in Canada |
| Lavigne et al.33 | 2006 | 320 | 1998-2000 | Montreal | Smoking |
| Haase34 | 2007 | 900 | 1996-2000 | Montreal | Spatial analysis within Montreal |
| Fortin et al.35 | 2007 | 670 | 1998-2003 | Montreal | Prevalence of positive TST test |
| Reed et al.36 | 2008 | 798 | 2001-2007 | Montreal immigrants | Tracks strain by country |
| Lacroix et al.37 | 2008 | 115 | 1998-2007 | Monteregie | |
| Carter et al.38 | 2009 | 1543 | 1996-2004 | Montreal | Overlaps with other data |
| Aspler et al.39 | 2010 | 420 | 2007 | Canada | |
| Brassard and Remis40 | 2004 | 262 | 1988-1998 | Montreal | Drug users |
| Smith et al.41 | 2011 | 9145 | 1998-2003 | Quebec | Latent TB in general population |
| Wanyeki et al.42 | 2006 | 595 | 1996-2000 | Montreal | Dwellings and crowding |
| Government agencies | References | No. of reports | Title |
|---|---|---|---|
| Santé et Services Sociaux Quebec | Ministre de la Santé et Services Sociaux, Quebec2, 6 | 3 | Epidemiologie de la tuberculose au Quebec |
| Health Canada | Public Health Agency of Canada8 | 14 | Tuberculosis in Canada |
| Institut National de Santé Quebec | Institut National de Santé Publique du Québec47 | 3 | La resistance aux antituberculose au Quebec |
The agencies that provide such reports include: i) Health Canada; ii) The Public Health Agency of Canada (PHAC); iii) Ministère de la Santé et des Services Sociaux (MSSS); and iv) Institut National de Santé Publique du Québec (INSPQ). The website of each organisation is searchable, and the keywords tuberculosis and tuberculose were used to locate official documents within each agency. A total of 20 reports from 1996 through 2009 were included for analysis.
The MSSS provided epidemiological reports of TB in the Province of Quebec for 2000-20032 and 2004-2007.6 These reports give incidences of TB in the Province of Quebec for various demographic groups and regions and were the primary source of data in this study. Health Canada, through PHAC, releases a yearly report on TB epidemiology in Canada.8 Reports are available online from 1996 to 2009. These were used to provide additional information about TB in Canada and the Province of Quebec that were not covered by the MSSS documents.
Several databases were used to gather demographic information about the overall population including; the Quebec Census,43 Quebec Demographics Database,44 Circumpolar Socioeconomic Database45 and Nunavik Statistics Program.46 Demographic data beyond that were provided by individual papers based on these sources. As this was a systematic literature review of existing published literature, no ethical approval was required to complete this research project.
Overall quantitative findings
The number of cases and incidence of TB in the Province of Quebec in 2009 is summarised in Table 2. The data for this table are compiled from the 2009 Health Canada report on tuberculosis.8 As can be seen, the incidence of TB in the Province of Quebec has been decreasing (Pearson’s coefficient: -0.96, P<0.01) since the 1980s and was below 3 cases per 100,000 in 2007 (Figure 1). This includes the general population as well as immigrants (Pearson’s coefficient: -0.81, P<0.01) (Figure 2).While the incidence was low overall in the Province of Quebec, it was over 14 per 100,000 among immigrants in 2007 (Figure 2).8 The percentage of TB cases that occurred amongst immigrants rose steadily in Canada from 1985 to 2005 (Figure 2), recently exceeding 50% and accounted for 62% of all cases in 2008.8 The increase in the proportion of cases in Quebec that occur in immigrants, approximately 0.7 percent per year, is statistically significant (Pearson’s coefficient: 0.70, P<0.01). Montreal is home to a large immigrant population and its proportion of immigrant cases is higher than the rest of the province: Rivest et al.17 reported that from 1992 to 1995, 77.9% of cases in Montreal were among immigrants and that the incidence of TB in various immigrant groups reflects that in their home countries. The Rivest paper also provides a table of the incidence of TB in Montreal for immigrants from various regions, which is not reported in the official document. While the proportion of TB cases among immigrants has been increasing, the total number of cases has been decreasing.
Table 2.
Summary of the incidence of tuberculosis in Canada and Quebec in 2009.
| Group | Canada cases | Quebec cases | Canada incidence per 100,000 | Quebec incidence per 100,000 |
|---|---|---|---|---|
| Canadian non-indigenous | 237 | 45 | 1 | 0.7 |
| Immigrants | 1003 | 131 | 13.3 | 12.2 |
| Inuit | 89 | 14 | 155.8 | 118.1 |
| Aboriginal Canadians (non-Inuit) | 228 | 5 | 27.4 | 6.3 |
| Other | 42 | 0 | <1 | 0 |
| Total | 1599 | 195 | 4.7 | 2.5 |
Figure 1.
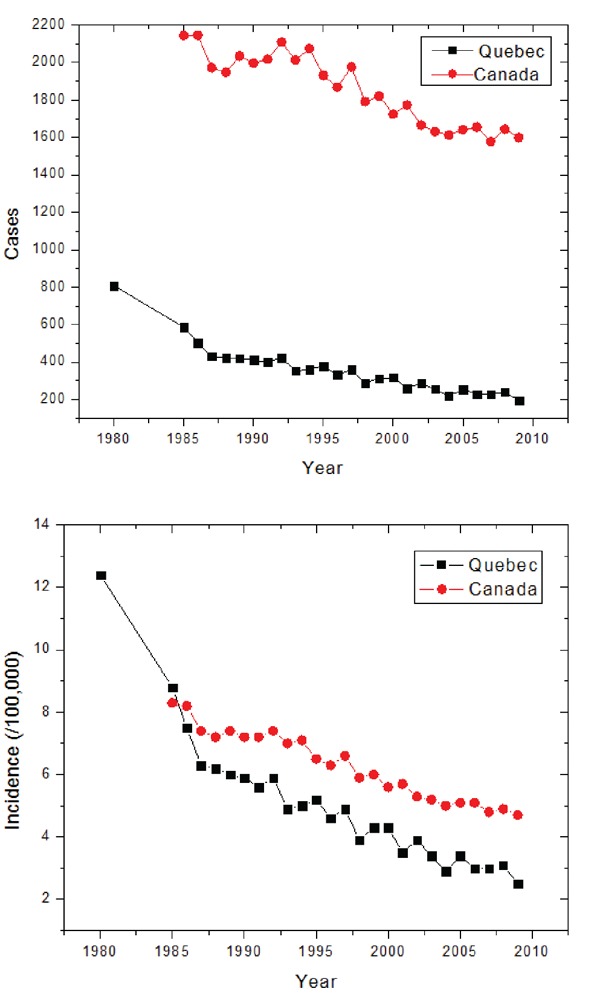
Number of cases and incidence of TB in Canada and Quebec 1980-2009. Sources: Ministre de la Santé et Services Sociaux, Quebec2, 6 and Public Health Agency of Canada.8
Figure 2.
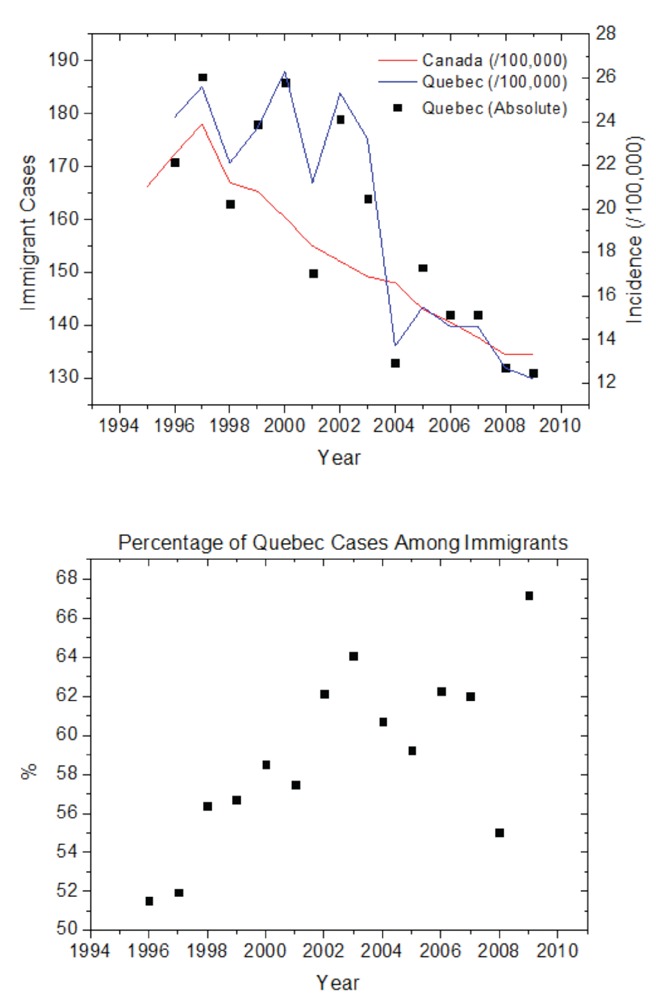
Number of TB cases among immigrants in Quebec and Canada, 1995-2009, and percentage of immigrant cases. Sources: Ministre de la Santé et Services Sociaux, Quebec2 and Public Health Agency of Canada.8
In addition to an increased incidence among immigrants, the Inuit community in the Province of Quebec also experiences a high rate of tuberculosis. In 2007, the incidence among Inuit in the Province of Quebec was over 100 per 100,000. While rates are decreasing over time among other groups, examining epidemiological data (Figure 3) suggests tuberculosis rates may be increasing among Inuit nationwide (Pearson’s coefficient: 0.67, P<0.01) but there is no clear trend in Quebec (Pearson’s coefficient: 0.55, P>0.02). While government data is available from the mid 1990s, historical data may be used to examine the epidemiology of TB among the Inuit in Canada in prior decades. In the 1970s the mean incidence among the Inuit was 168 per 100,000,18 while during the period from 1995 to 2005 the mean incidence was 65 per 100,000.8 Enarson reports a reduction in incidence of 16% per year among the Inuit in the early 1970s, but the trend slowed towards the end of the decade.18 Nguyen et al.1 reports a fluctuating incidence of TB in Nunavut throughout the 1990s. It is ascertained that the fluctuating rates observed from 1996 to 2009 are not a new trend.
Figure 3.
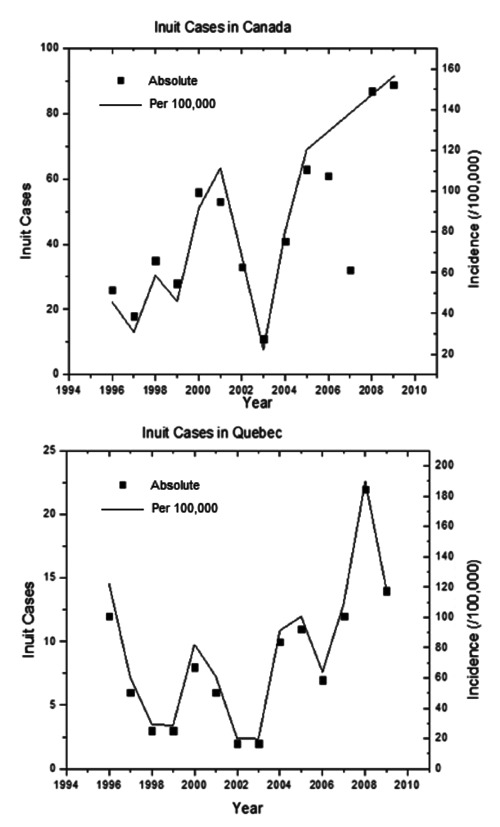
Number of TB cases among Inuit in Canada and Quebec, 1995-2009. Sources: Ministre de la Santé et Services Sociaux, Quebec2 and Public Health Agency of Canada.8
Among non-indigenous Canadians, TB rates generally increase with age with the highest rates among those older than 65 (Figure 4). Among immigrants, a bimodal distribution is seen with respect to age, with most cases occurring in young adults and a second peak in incidence among the elderly. Rivest et al.17 observed the same age distribution trends. The peak among young adult immigrants is not necessarily due to an increased susceptibility to TB in that group, but rather that new immigrants are mostly in that age group43 and many immigrants are diagnosed within two years of their arrival.6 The age distribution of Inuit cases in Quebec was bimodal, similar to that observed in immigrant cases. This is reported both by the SSSQ reports2, 6 in the 2000s and by Nguyen et al. in the 1990s.1 This may be explained by the fact that population of Nunavik45 is considerably younger compared to that of the Province of Quebec.43
Figure 4.
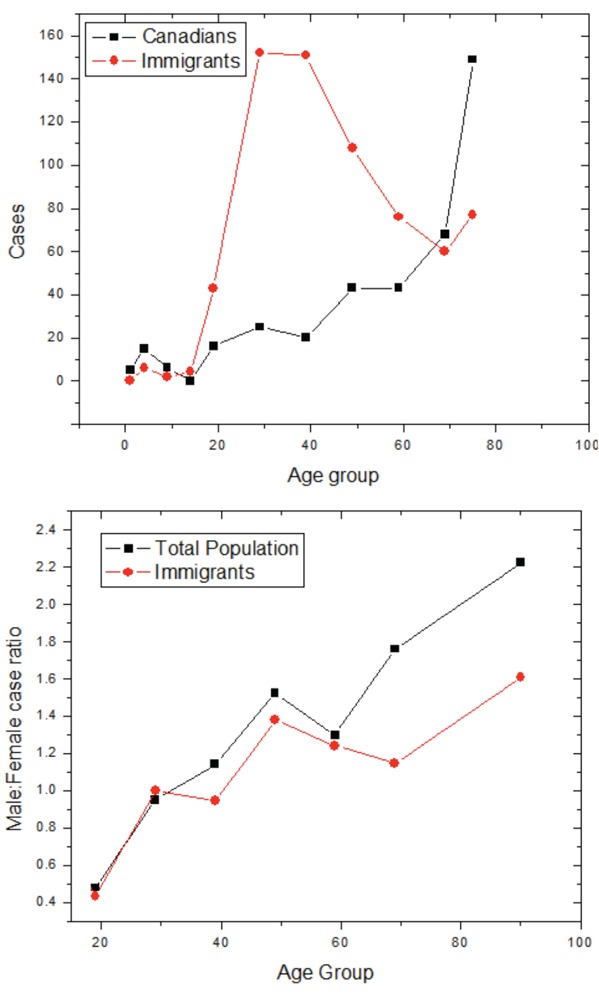
Distribution of cases with respect to age, and the ratio of male to female cases with respect to age.
In general, the rate of TB with respect to age increases more strongly among men than women. While there is significant variation among children due to the small numbers, a trend can be seen among adults. The relative incidence between sexes among children varies from year to year due to the small number of cases. Among adults the ratio of male to female cases increases with age (Figure 4). The difference in the oldest age bracket is statistically significant (P<0.005). The greater rate among older men compared to older women has also been observed by Holmes et al.,48 who have advanced two hypotheses for this trend: that adult men spend more time outside the house than women, or that female cases are under-reported due to differences in skin test efficacy. There does not appear to be a great difference between Canadian and immigrant sex trends, although the immigrant population tends to display more gender parity.
Discussion
The results presented paint a clear picture: while Quebec generally has low and falling tuberculosis rates, two groups suffer higher rates of the disease: immigrants and the Inuit. These trends, however, are not unique to Quebec or to Canada.
Canada is one of several countries with a low rate of TB that has a greater incidence rate among indigenous and immigrant populations. Watkins et al.49 examined tuberculosis epidemiology among immigrants in Canada and Australia and found that immigrant groups in both countries suffer rates that mirror those of their home countries, similar to the conclusions of Rivest et al. in Quebec.17 French et al.50 found that in the United Kingdom, 67% of TB cases were among immigrants, with an incidence rate of 88 per 100,000, much greater than among immigrants in Canada or in the Province of Quebec (typically 20 per 100,000; Figure 2). In comparison to the UK, the immigrant proportion of cases in Quebec in 2001-2003, the years of French et al.’s study, was 61%.2 Talbot et al.51 in the United States found that between 29 and 40 percent of cases in the mid 1990s were among immigrants, with rates of 32.9 per 100,000, higher than Canada’s rate during that same time period.
Other industrialized nations with an indigenous population also have greater rates of tuberculosis in those populations. The rate among aboriginal populations in Australia is 6.6 per 100,000, lower than among the Inuit in Quebec but seven times greater than the non-native population.52 In the United States the rate of TB among Native Americans is 6 per 100,000, 5.4 times greater than among the white population, while in New Zealand the Maori experienced a TB rate that was 6.9 times greater than the non-indigenous population.52 In all these countries, the rates are several times lower than among the Province of Quebec’s Inuit population. The increased tuberculosis rates are a manifestation of a greater problem of poor indigenous health in well-developed countries, which Durie53 claims is due to genetic vulnerability, socioeconomic disadvantage, resource alienation, and political oppression. While this may explain the global trend, it does not explain why the situation is so much worse among the Inuit compared to other indigenous groups worldwide.
One may be interested in the causative factors behind the observed correlations. One such factor is co-infection with HIV, a disease more common in immigrants. Co-infection of HIV and TB is reported by Brassard et al.4 They report that 5.2% of people with AIDS in the Province of Quebec have had TB and 5.8% of those with active TB are HIV positive. They conclude that immigrants from HIV-stricken countries are significantly more likely to develop TB and that AIDS contributes significantly to the number of TB cases in the Province of Quebec. This is consistent with the fact that the most common country of origin for immigrants with TB in Quebec is Haiti,2 which has the third highest rate of HIV outside Africa.54 Another factor is poverty and socioeconomic status. In British Colombia, it was observed that one’s socioeconomic stratum was an important risk factor for the incidence of TB.5 Poverty is known to be an issue among indigenous peoples in Canada. In addition, there is evidence that tuberculosis epidemiology is linked to vitamin D deficiency55 and thus it may be possible to reduce the incidence of the disease in at-risk populations with a supplementation program. Vitamin D deficiency may help explain the disparity between men and women in Quebec: Selvaraj et al.56 found evidence that tuberculosis susceptibility is related to a mutation of the vitamin D receptor in men but not women. Among other factors, the increased rate of tuberculosis among the Quebec Inuit may be due to vitamin D insufficiency, due to both the greater latitude of their communities and due to nutritional insufficiencies.57 This may be a factor explaining why tuberculosis rates are so much greater in Quebec Inuit than other Indigenous populations, such as Australian aborigines, who experience more sunlight.
This paper was motivated by questioning the economic benefit of preventative measures against tuberculosis. To gauge these benefits, the financial burden of treating the disease must be understood. The costs of tuberculosis care in Canada are discussed by Menzies in a report for the Public Health Agency of Canada (PHAC).3 The average cost per active case in Canada is $ 47,290 (2004 dollars). Excluding expenditures such as research funding, the cost of treating an active case is $ 19,906, while latent TB costs $ 845 per case. Half of patients are hospitalised, costing nearly a thousand dollars per day. The drugs used to treat active TB range in cost from CDN $ 500 to CDN $ 1000 dollars, but rare cases of multiply resistant TB require drugs costing over CDN $ 50,000 dollars. However, costs in the northern territories were much higher than the national average, due to the higher incidences and wide geographic dispersion. Many northern communities lack medical facilities and staff, and suspected TB patients and their families must be flown to a hospital. Nunavik has similar human geography as Nunavut, with the population distributed between several small villages, only one with a hospital. Rates are similar between Nunavik and Nunavut. While the cost of treatment in Quebec is $ 35,000 per TB case, it is over twice as high in Nunavut. Due to their similarities, the cost per case may be similarly high in Nunavik although it was not explicitly reported. The increased rate of tuberculosis among the Inuit in Quebec may present an economic burden if not checked.
Conclusions
Peer reviewed and government documents were used to collate data about the epidemiology of TB in the Province of Quebec. Overall, the incidence of TB is much higher among immigrants than the general population. The rates among the total population as well as among immigrants were found to be decreasing over time. The Inuit suffer a much higher rate than either immigrants or the general population, but this fluctuates from year to year with no significant trend being observed. Several factors including HIV, poverty, and vitamin D deficiency were investigated, as well as the potential economic burden of the disease.
References
- 1.Nguyen D, Proulx J-F, Westley J, Thibert L, et al. Tuberculosis in the Inuit community of Quebec, Canada. Am. J. Respir. Crit. Care Med. 2003:168:1353-7 [DOI] [PubMed] [Google Scholar]
- 2.Ministre de la Santé et des Services sociaux du Quebec. Epidémiologie de la tuberculose au Quebec de 2000-2003. 2005 [Google Scholar]
- 3.Menzies D, Oxlade O.Costs for tuberculosis care in Canada. 2006 Report for the Public Health Agency of Canada. Accessed on: 14 June2011. Available from: http://www.phac-aspc.gc.ca/tbpclatb/costtb/pdf/cost_tb_e.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brassard P.Yield of tuberculin screening among injection drug users. Int J Tuberc Lung D 2004;8:988-93 [PubMed] [Google Scholar]
- 5.Moran-Mendoza O.Risk factors for developing tuberculosis: a 12-year follow-up of contacts of tuberculosis cases. Int J Tuberc Lung D 2010:14:1112-9 [PubMed] [Google Scholar]
- 6.Ministre de la Santé et des Services sociaux du Quebec. Epidémiologie de la tuberculose au Quebec de 2004-2009. 2005 [Google Scholar]
- 7.Central Intelligence Agency. World Factbook: Country comparison of net immigration rate. Accessed on: 14 June 2011. Available from: https://www.cia.gov/library/publications/the-world-factbook/rankorder/2112rank.html?countryName=Canada&countryCode=ca®ionCode=na&rank=15#ca [Google Scholar]
- 8.Public Health Agency of Canada. Tuberculosis in Canada. Accessed on: 14 June2011. Available from: http://www.phac-aspc.gc.ca/tbpclatb/pubs/tbcan09pre/index-eng.php [Google Scholar]
- 9.Greenwood CM, Fujiwara TM, Boothroyd LJ, et al. Linkage of tuberculosis to chromosome 2q35 loci, including NRAMP1, in a large aboriginal Canadian family. Am J Hum Genet 2000;7:405-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeon CY, Murray MB.Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 Observational studies. PLoS Med 2008;5:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung CC, Lam TH, Chan WM, et al. Diabetic control and risk of tuberculosis: a cohort study. Am J Epidemiol 2008;167:1486-94 [DOI] [PubMed] [Google Scholar]
- 12.Restrepo BI, Fisher-Hoc SP, Smith B, et al. Short report: mycobaterial clearance from sputum is delayed during the first phase of treatment in patients with diabetes. Am J Trop Med Hyg 2008;79:541-4 [PMC free article] [PubMed] [Google Scholar]
- 13.Lin HH, Ezzati M, Murray M.Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med 2007;4:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bates MN, Khalakdina A, Pai M, et al. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Arch Intern Med 2007;167:335-42 [DOI] [PubMed] [Google Scholar]
- 15.Slama K, Chiang CY, Enarson DA, et al. Tobacco and tuberculosis: a systematic review and meta-analysis. Int J Tuberc Lung D 2007;11:1049-61 [PubMed] [Google Scholar]
- 16.Lin HH, Murray M, Cohen T, et al. Effects of smoking and solid-fuel use on COPD, lung cancer, and tuberculosis in China: a time-based, multiple risk factor, modelling study. Lancet 2008;372:1473-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rivest P, Tannenbaum T, Bedard L.Epidemiology of tuberculosis in Montreal. Can Med Assoc J 1998;58:605-9 [PMC free article] [PubMed] [Google Scholar]
- 18.Enarson DA, Grzybowski S.Incidence of active tuberculosis in the native population of Canada. Can Med Assoc J 1986;134:1149-52 [PMC free article] [PubMed] [Google Scholar]
- 19.Gaudette L, Ellis E.Tuberculosis in Canada: a focal disease requiring distinct control strategies for different risk groups. Tubercle Lung Dis 1993;74:244-53 [DOI] [PubMed] [Google Scholar]
- 20.Frappier A, Cantin M, Davignon L, et al. Bcg vaccination and pulmonary tuberculosis in Quebec. Can Med Assoc J 1971;105:707-10 [PMC free article] [PubMed] [Google Scholar]
- 21.Adhikari N, Menzies R.Community-based tuberculin screening in Montreal: a cost-outcome description. Am J Public Health 1995;85:786-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menzies D, Hochan C, Vissandjee B.Impact of immigration on tuberculosis infection among Canadian-born schoolchildren and young adults in Montreal. Am J Respir Crit Care 1997;156:1915-21 [DOI] [PubMed] [Google Scholar]
- 23.Dasgupta K, Schwartzman K, Marchand R, et al. Comparison of cost-effectiveness of tuberculosis screening of close contacts and foreign-born populations. Am J Respir Crit Care 2000;162:2079-86 [DOI] [PubMed] [Google Scholar]
- 24.Smeja C.Tuberculosis infection in an aboriginal (First nations) population of Canada. Int J Tuberc Lung D 2000;4:925-30 [PubMed] [Google Scholar]
- 25.Kulaga S, Behr M, Musana K, et al. Molecular epidemiology of tuberculosis in Montreal. Can Med Assoc J 2002;167:353-4 [PMC free article] [PubMed] [Google Scholar]
- 26.Dion M-J, Tousignant P, Bourbeau J, et al. Measurement of health preferences among patients with tuberculous infection and disease. Med Decis Making 2002;22:S102-14 [DOI] [PubMed] [Google Scholar]
- 27.Kulaga S, Behr MA, Nguyen D, et al. Diversity of mycobacterium tuberculosis isolates in an immigrant population: Evidence against a founder effect. Am J Epidemiol 2004;159:507-13 [DOI] [PubMed] [Google Scholar]
- 28.Dion M-J, Tousignant P, Bourbeau J, et al. Feasibility and reliability of health-related quality of life measurements among tuberculosis patients. Qual Life Res 2004;13:653-65 [DOI] [PubMed] [Google Scholar]
- 29.Richards B.Tuberculosis surveillance among new immigrants in Montreal. Int J Tuberc Lung D 2005;9:858-64 [PubMed] [Google Scholar]
- 30.Menzies D.In closely monitored patients, adherence in the first month predicts completion of therapy for latent tuberculosis infection. Int J Tuberc Lung D 2005;9:1343-8 [PubMed] [Google Scholar]
- 31.Decarie D, Grenier J, Allard A.Outbreak of tuberculosis in the Laurentian region, 2005. [Article in English, French].. Can Commun Dis Rep 2006;32:226-9 [PubMed] [Google Scholar]
- 32.Harris T, Panaro L, Phypers M, et al. HIV testing among Canadian tuberculosis cases from 1997 to 1998. Can J Infect Dis Med Microbiol 2006;17:165-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lavigne M, Rocher I, Steensma C, Brassard P.The impact of smoking on adherence to treatment for latent tuberculosis infection. BMC Public Health 2006;6:1-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haase I.Use of geographic and genotyping tools to characterize tuberculosis transmission in Montreal. Int J Tuberc Lung D 2007;11:632-8 [PubMed] [Google Scholar]
- 35.Fortin K, Carceller A, Robert A, et al. Prevalence of positive tuberculin skin tests in foreign-born children. J Paediatr Child H 2007;43:768-72 [DOI] [PubMed] [Google Scholar]
- 36.Reed MB, Pichler VK, McIntosh F, et al. Major mycobacterium tuberculosis lineages associate with patient country of origin. J. Clin. Microbiol 2009;7:1119-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lacroix C, Martin P, Turcotte S, et al. The delay in diagnosis of tuberculosis in the Monteregie region of Quebec, Canada. McGill J Med 2008;11: 124-31 [PMC free article] [PubMed] [Google Scholar]
- 38.Carter A, Zwerling A, Olson S, et al. Tuberculosis and the city. Health Place 2009;15:807-13 [DOI] [PubMed] [Google Scholar]
- 39.Aspler A, Long R, Trajman A, et al. Impact of treatment completion, intolerance and adverse events on health system costs in a randomised trial of 4 months rifampin or 9 months isoniazid for latent TB. Thorax 2010;65:582-7 [DOI] [PubMed] [Google Scholar]
- 40.Brassard P, Remis RS.Incidence of tuberculosis among reported Aids cases in Quebec from 1979 to 1996. Can Med Assoc J 1999;160:1838-42 [PMC free article] [PubMed] [Google Scholar]
- 41.Smith BM, Schwartzman K, Bartlett G, Menzies D.Adverse events associated with treatment of latent tuberculosis in the general population. Can Med Assoc J 2011;183:E173-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wanyeki I, Olson S, Brassard P, et al. Dwellings, crowding, and tuberculosis in Montreal. Soc Sci Med 2006;63:501-11 [DOI] [PubMed] [Google Scholar]
- 43.Institut de la Statistique Quebec. 2001 Quebec Census. Accessed on: 14 June 2011. Available from:http://www.stat.gouv.qc.ca/regions/index_2006_an.htm [Google Scholar]
- 44.Institut de la Statistique Quebec. Quebec demographics. Accessed on: 14 June2011. Available from: http://www.stat.gouv.qc.ca/donstat/societe/demographie/index_an.htm [Google Scholar]
- 45.Arcticstat Socioeconomic Circumpolar Database. Nunavik aboriginal population profile. 2006. Accessed on: 14 June2011. Available from: http://www.arcticstat.org/Statistics.aspx/Region/%5BCanada%5DNunavik/Indicator/Population/ [Google Scholar]
- 46.University of Laval. Nunavik statistics institute. Accessed on: 14 June2011. Available from: http://www.nunivaat.org/statistics.aspx [Google Scholar]
- 47.Institut National de Santé Publique du Québec. La résistance aux antituberculeaux au Québec - 2009. Accessed on: 14 June2011. Available from: http://www.inspq.qc.ca/pdf/publications/1085_Antituberculeux2009.pdf [Google Scholar]
- 48.Holmes CB, Hausler H, Nunn P.A review of sex differences in the epidemiology of tuberculosis. Int J Tuberc Lung D 1998;2:96-104 [PubMed] [Google Scholar]
- 49.Watkins RE, Plant AJ, Gushulak BD.Tuberculosis rates among migrants in Australia and Canada. Int J Tuberc Lung D 2002;6:641-4 [PubMed] [Google Scholar]
- 50.French C.Tuberculosis in non-UK born persons, England and Wales, 2001-2003. Int J Tuberc Lung D 2007;11:577-84 [PubMed] [Google Scholar]
- 51.Talbot EA, Moore M, McCray E, Binkin NJ.Tuberculosis among foreign-born persons in the United States, 1993-1998. JAMA 2000;284:2894-900 [DOI] [PubMed] [Google Scholar]
- 52.Robertus LM, Konstantinos A, Hayman NE, Paterson DL.Tuberculosis in the Australian indigenous population: history, current situation and future challenges. Aust NZ J Publ Heal 2011;35:6-9 [DOI] [PubMed] [Google Scholar]
- 53.Durie M.The health of indigenous peoples. BMJ 2003;326:510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Central Intelligence Agency. World Factbook: HIV/AIDS Adult Prevalence Rate. 2009. Accessed on: 29 April2011. Available from: https://www.cia.gov/library/publications/the-world-factbook/rankorder/2155rank.html [Google Scholar]
- 55.Ho-Pham L, Nguyen N, Nguyen T, et al. Association between vitamin D insufficiency and tuberculosis in a Vietnamese population. BMC Infect Dis 2010;10:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Selvaraj P, Chandra G, Sunil MK, et al. Association of vitamin D receptor gene variants of BsmI, ApaI and FokI polymorphisms with susceptibility or resistance to pulmonary tuberculosis. Curr Sci India 2003;84:1564-8 [Google Scholar]
- 57.El Hayek J, Egeland G, Weiler H.Vitamin D status of Inuit preschoolers reflects season and vitamin D intake. J Nutr 2010; 140:1839-45 [DOI] [PubMed] [Google Scholar]


