Abstract
While the benefits of collaboration have become widely accepted and the practice of collaboration is growing within the public health system, a paucity of research exists that examines factors and mechanisms related to effective collaboration between public health and their partner organizations. The purpose of this paper is to address this gap by exploring the structural and organizational characteristics of public health collaboratives. Design and Methods. Using both social network analysis and traditional statistical methods, we conduct an exploratory secondary data analysis of 11 public health collaboratives chosen from across the United States. All collaboratives are part of the PARTNER (www.partnertool.net) database. We analyze data to identify relational patterns by exploring the structure (the way that organizations connect and exchange relationships), in relation to perceptions of value and trust, explanations for varying reports of success, and factors related to outcomes. We describe the characteristics of the collaboratives, types of resource contributions, outcomes of the collaboratives, perceptions of success, and reasons for success. We found high variation and significant differences within and between these collaboratives including perceptions of success. There were significant relationships among various factors such as resource contributions, reasons cited for success, and trust and value perceived by organizations. We find that although the unique structure of each collaborative makes it challenging to identify a specific set of factors to determine when a collaborative will be successful, the organizational characteristics and interorganizational dynamics do appear to impact outcomes. We recommend a quality improvement process that suggests matching assessment to goals and developing action steps for performance improvement.
Acknowledgements
the authors would like to thank the Robert Wood Johnson Foundation’s Public Health Program for funding for this research.
Key words: partnerships, public health systems, collaboration, effectiveness
Significance for public health
While the benefits of collaboration have become widely accepted, and the practice of collaboration is growing within the public health system, the ability to measure, document, and strategize to affect practice has been weak. However, the need for evaluation and analysis in these areas is strong because collaboration has the potential to improve the processes of healthcare which can create better outcomes, but also reduce the cost of delivering services by eliminating waste, unnecessary work, and rework. In the case of collaboration, it is important to recognize that both the resources (inputs) and activities carried out (processes) must be addressed together to ensure or improve the quality of care. Once these dimensions are addressed, then practice and policy can be affected through strategic planning, involving the workforce that makes up the bulk of leadership within public health collaboratives (PHCs).
Introduction
In the United States, the Ten Essential Services of Public Health were designed in 1994 as a framework for the National Public Health Performance Standards Program of the Center for Disease Control and Prevention.1 Notably, they included the goal of mobilizing community partnerships and action to identify and solve health problems. At the local level, this meant clearly stating the importance of identifying relevant stakeholders and involving them in the process, building coalitions to strengthen human and material resources, and facilitating partnerships among groups and associations, some who may be atypical partners (e.g. organizations outside of public health, for example public safety, business, and schools).2,3 With these guiding responsibilities, public health departments are working toward strengthening their network of partners through interorganizational networks in order to better coordinate health services and resources leading not only to less duplication but more substantially, increased cohesion and improved adoption of interventions and programme implementation.4
More recently, collaboration across sectors continues to be formalized. For example, the Public Health Accreditation Board (PHAB), the governance body that provides guidance to Public Health Departments (PHDs) in preparation to meet the evolving set of standards and measures for voluntary accreditation, published the revised Proposed State/Local Standards and Measures documents,5 emphasizing collaboration as a core competency. The fourth domain addressed in these standards is Engage the Public Health System and the Community in Identifying and Addressing Health Problems. They emphasize taking inventory of partnerships and demonstrating their relevance to demonstrate improved capacity.
The increased practice of collaboration echoes what is emphasized in the literature. For example, relations that involve the exchange of resources and knowledge among sectors are the norm and certainly the latest trend in successful social service models.6-11 Networks of community organizations working for a common purpose are thought to increase community capacity to meet social needs.10,12 The benefits of interorganizational community networks include: i) bringing diverse groups and resources together; and ii) addressing issues that no group can resolve by itself.13 Blau and Rabrenovic14 found that interorganizational linkages are more important than bureaucratic hierarchies for controlling and coordinating work…linkages are used to integrate programs within a community, coordinate client services, obtain resources, and deal with governmental agencies (p. 328). However, despite these published benefits of collaboration, it is important to note that in addition to the anticipated benefits, collaborations are often characterized by a high-level of dissatisfaction with their actual outcomes relative to expectations, and correspondingly, a high rate of failure (p. 326).15 This is in large part due to the challenges of collaborating such as transaction costs, potential conflict, and lack of accountability.
This mix of accountability, evidence in research, and experience in practice has in turn led to the rise of public health collaboratives (also referred to as coalitions) as a strategy for addressing the most pressing public health problems in communities. This paper is an exploratory analysis of eleven public health collaboratives.
While the benefits of collaboration have become widely accepted,16,17 and the practice of collaboration is growing within the public health system, the ability to measure, document, and strategize to affect practice has been weak.18,19 However, the need for evaluation and analysis in these areas is strong because collaboration has the potential to improve the processes of healthcare which can create better outcomes, but also reduce the cost of delivering services by eliminating waste, unnecessary work, and rework.20 In the case of collaboration, it is important to recognize that both the resources (inputs) and activities carried out (processes) must be addressed together to ensure or improve the quality of care.20 Once these dimensions are addressed, then practice and policy can be affected through strategic planning, involving the workforce that makes up the bulk of leadership within public health collaboratives (PHCs).
Research questions
Analysis to understand and explain the process of collaboration requires an understanding of the relationships among a number of factors (e.g. in a dynamic system with nested levels of interaction.17,21 For example, Mays and Scutchfield6 note that Public health activities in the United States are delivered through multiple public and private organizations that vary widely in their resources, missions, and operations…without strong coordination mechanisms, these delivery arrangements may perpetuate large gaps, inequities, and inefficiencies in public health activities (p. 1). The diversity of these multiple organizations and the varying context that each community contributes to the functioning of these collaboratives creates a level of complexity within public health systems that cannot be evaluated with a single case study or anecdotal analysis.22,23 Rather, analysis across a wider range of collaboratives is required to identify determinants of effectiveness in public health collaboration. While the practice of collaboration in public health is on the rise and accepted as an essential practice in the field, the study of collaboration has not kept up. Understanding the process of collaboration, differences among practice, and factors of success is important to ensure that collaboration is conducted with evidence to back up the process. In this paper, we conduct an exploratory analysis of 11 public health collaboratives across the United States. We analyze network data to identify relational patterns by exploring the network structure (the way that organizations connect and exchange relationships). We then take a closer look at the relationships between members in these collaboratives to determine how certain organizational characteristics are associated with outcomes of these relationships such as how frequently partners interact and their perceptions of partners’ trust and value to the network. Specifically, we address the following two research questions:
RQ1: What are network characteristics of public health collaboratives?
RQ2: What are the relationships between network members’ characteristics and quality of connections (e.g. trust, value, and frequency of interactions) among members of collaboratives?
Design and Methods
Data collection
This study was an exploratory, secondary data analysis of 11 public health collaboratives chosen from the PARTNER (Program to Analyze, Record, and Track Networks to Enhance Relationships - www.partnertool.net) database. PARTNER is a social network analysis tool used by public health agencies across the country to assess and evaluate their efforts to collaborate with other organizations/agencies across the public health system. These efforts include but are not limited to partnerships for shared programming and/or funding, implementation of interventions and programmes, knowledge sharing, and community capacity building with a diverse range of other organizations/agencies. At the heart of these collaborations is the exchange of resources such as in-kind service, health expertise and non-health expertise, funding, data, education, and programmatic services shared to accomplish mutual goals related to public health practice. PARTNER is an online survey and analysis tool designed to measure and monitor collaboration among people and/or organizations. The online PARTNER survey collects data on individual organizational characteristics such as type of organization, length of time participating in the partnership, what resource contributions the organization provides to the collaborative, what outcomes the collaborative focuses on, the perceived level of success for accomplishing collaborative goals, and reasons for successful collaborations. The survey also contains relational questions that ask organizations to identify other organizations in the collaborative that they work with and then asks subsequent questions about how frequently they interact with that organization, the quality of those interactions, and perceptions of trust and organizational value for each partner organization (using three measures of trust and three measures of value).24 These survey items are listed in table 1.
Table 1.
Partner survey questions.
| Demographic questions (organizational description) |
|---|
| Job title, length of time as a member of the collaborative, types of activities engaged in, outcomes of the collaborative, resources contributed to the collaborative. |
| Perception of success |
| How successful has your collaborative been at reaching its goals? |
| Not Successful, Somewhat Successful, Successful, Very Successful, Completely Successful |
| Outcome questions |
| Collaborative outcomes; factors contributing to successful outcomes. |
| Relational questions |
| Please list all organizations/ divisions/ agencies/ programs with whom you have a relationship with to meet the goals of your collaborative. |
| Once each respondent selected their organizational partners, they were asked to answer the following questions: |
|
This project was reviewed by the Colorado Multiple Institution Internal Review Board and was deemed exempt and approved for analysis as a secondary data set.
Sample
The 11 collaboratives used for this study are a purposeful sample, selected from the PARTNER database for their common characteristics. Collaboratives that were most comparable along a set of criteria were selected. These selection criteria were based on the following: i) mission (we chose collaboratives that were focused on addressing a set of identified public health needs in their communities (for example, oral health, early childhood intervention, maternal health, health disparities, and general community health); ii) organizations as the unit of analysis in their data (no individuals were represented in the data); iii) use of the same PARTNER survey questions (or questions that were easily coded to match the PARTNER survey questions); iv) State or local public health department as members of the collaborative. Less than half of these collaboratives had some kind of funding. All collaboratives opted to participate in the PARTNER survey. The 11 public health collaboratives ranged in size from having 16 to 433 member organizations totaling 868 organizations. Of those, 262 responded to the surveys which resulted in 3738 dyadic ties between organizations who were members of the collaboratives. Data were collected between July 2010 and February 2011 in the United States. Response rates for each network dataset (11 in total) ranged from 45% to 100%, with a mean response rate of 76%. While we analyzed each data set at the whole network (collaborative) level in our descriptive social network analysis, we used a different approach in our inferential analysis to account for the variation in response rates. Specifically, because some of the response rates were low enough to cause uncertainty of whether a full representation of the network was attained,25 we opted to aggregate the data into one dataset consisting of attribute data for the respondent organizations and reported dyadic relationships. Each dyad (N=3738) consisted of two organizations and the measure of interaction between them. In this way, we are able to take a closer look at the way that organizations work together with partners they identify as having a relationship with, rather than comparing across the 11 collaboratives.
Analysis
To address the research questions posed above, we analyzed the data at three levels (Figure 1). First, we described some of the organizational level characteristics of members of public health collaboratives. Then, we describe the 11 collaboratives at the whole network level in terms of their network characteristics using Social Network Analysis (SNA)14 and descriptive statistics. SNA is a methodology used to gather and analyze data to explain the degree to which network actors connect to one another and the structural makeup of collaborative relationships.26 We present network maps of the 11 collaboratives and report on whole network characteristics including reciprocity, centralization, and transitivity.27 Finally, we examined the data at the dyad level (to analyze relationships between each pair of organizations) using Hierarchical Linear Modeling (HLM) and regressions to examine the relationships between network members’ characteristics (organization type, members’ perceptions of outcome achieved, and members’ perception for factors contributing to success) and quality of connections (trust, value, and frequency of interactions). We used HLM to account for the nested features of these data (dyads nested within organizations), specifically to examine how variables measured at one level affect relationships at another.28 HLM accounts for the dependent nature of nested data using multilevel models to estimate variation on one-on-one organizational relationship (dyad level) outcomes using a restricted maximum likelihood approach. Using this method, the interactions that occur across levels are taken into account and can be estimated.
Figure 1.
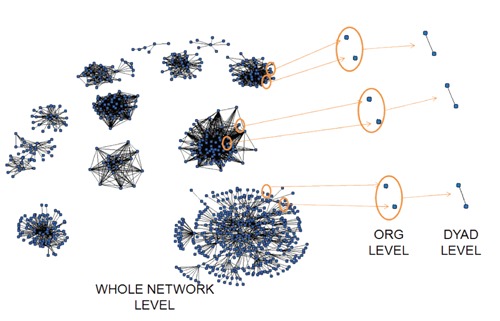
Three levels of analysis (Whole Network, Organizational, Dyad).
Results
We used SNA and descriptive statistics to answer research Question 1, What are network characteristics of PH collaboratives?
Organizational characteristics of members of the eleven collaboratives
Organizations represented in these collaboratives include public health, businesses, dental services, educational institutions, faith-based organizations, government organizations, funders, hospitals, law enforcement, non-profit community and advocacy organizations, primary care, health clinics, hospices, professional organizations, health insurance organizations, among others. The role and number of public health departments and specifically how they were embedded in each collaborative structure varied among the 11 groups. The survey asked respondents to rate these organizational partners in terms of levels of trust and value to the collaborative. Overall, funders, primary care/health clinics, hospitals, and public health were rated highest on these two measures by respondents (Figure 2). While public health organizations do not rank highest on value, they have the highest ranking for trust (they were rated as most trusted by their partners). Moreover, independent sample t-tests indicate there is a significant difference between public health and non-public health organizations (total trust, t=3.538, P=0.001).
Figure 2.
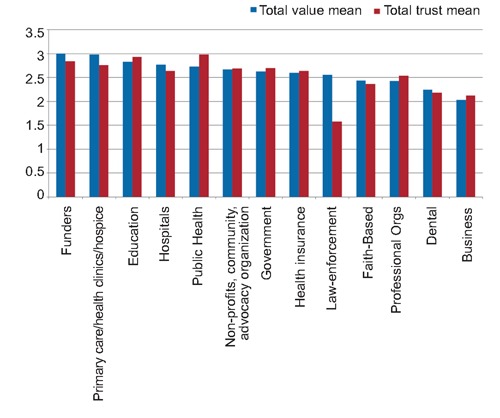
Organizational rankings on trust and value.
When asked what types of resources each respondent organization (N=262) contributes to their public health collaborative, the following were reported: community connections (n=189), specific health expertise (n=171), information/feedback (n=166), volunteers (n=116), facilitation (n=106), data sets (n=94), expertise other than health expertise (n=84), paid staff (n=82), in-kind resources (n=74), decision making (n=50), and funding (n=26). Respondents also reported which outcomes were achieved due to the work of the collaborative. The most commonly mentioned outcome was public awareness, followed by increased knowledge sharing, increased resource sharing, community support, increased services, reduction of health disparities, new sources of data, new policies, and finally education. Of these outcomes reported, respondents identified the most important outcomes as increased services to clients (n=66, 24.9%).
Whole network analysis to describe the network characteristics of the eleven collaboratives
Figure 3 presents network images of all eleven collaboratives to demonstrate the variation in how these types of networks are structured. In these images, nodes are connected when a formal working relationship exists between the organizations and interaction occurs at least once a year. All collaboratives had unique network structures (Figure 3), meaning some were very dense (they had many relationships between the partners) (collaborative 10), while others were less dense (collaborative 9), some included public health organizations (indicated as large nodes) as the centralized members of the network (collaborative 4), others were more clustered by these sector differences (collaborative 10), and still others had structures that consisted of several distinct components (collaborative 4). No two collaboratives had very similar structures.
Figure 3.
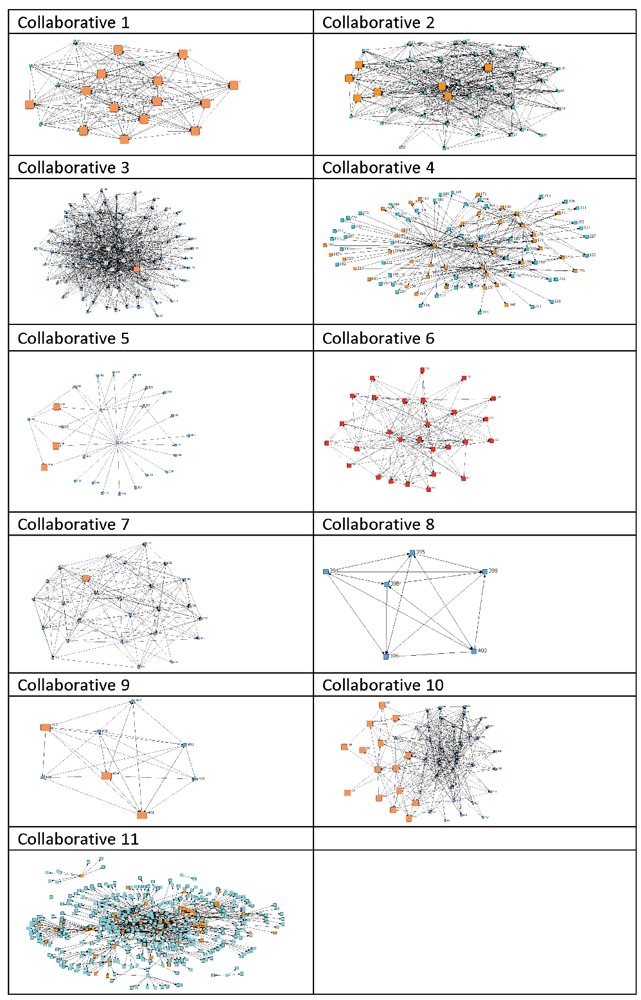
Comparison of three network maps (large orange nodes indicate Public Health Organizations).
We used three social network analysis metrics to describe the network characteristics of these collaboratives. These included reciprocity, transitivity, and centralization. Reciprocity is a measure that tells us what percentage of relationships are reciprocated between organizations. Transitivity is a measure that tells us about the level of information flow in a collaborative. Centralization is a measure that indicates how many organizations play central positions (the lower the number the fewer the number of organizations that are central).27 Across the 11 collaboratives we saw varying levels of all three of these scores. However, we did identify a pattern (Figure 4) that indicates that when reciprocity is high or low within a collaborative, transitivity mimics that behaviour. In other words, in these 11 collaboratives, when there is a higher instance of reciprocal relationships in a network there is also a tendency to see greater information flow. On the other hand, when reciprocity is low, information flow (transitivity) is also low. Centralization did not seem to follow any kind of similar pattern among these collaboratives. We also compared the collaboratives at the whole network level in terms of how the respondents reported levels of success. Respondents were asked to answer the question How successful has your collaborative been at reaching its goals? While the top responses included successful (37% of respondents) and somewhat successful (36% of respondents), the variability of these responses within collaboratives was high (20% reported their collaboratives as being very successful, 4% reported completely successful and 3% reported not successful). The responses lacked consensus from respondents in any one collaborative to demonstrate agreement about whether their collaboratives are successful and to what degree.
Figure 4.
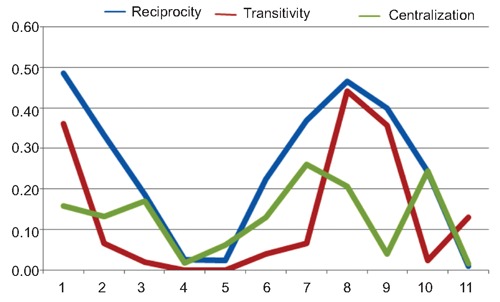
Comparison across the 11 collaboratives in terms of reciprocity, transitivity, and centralization.
Dyad level analysis
HLM was used at the dyadic level to answer research Question 2: What are the relationships between network members’ characteristics and quality of connections (trust, value, and frequency of interactions) among members of collaboratives? We tested three different types of HLM models to explore whether or not certain organizational characteristics (including an organization’s type, their perceptions of success, and reported outcomes) related to three variables that describe the quality of the dyad relationships among members. These include how an organization perceived other members’ i) overall value an organization brings to the collaborative (index score of power and influence, level of involvement, and resource contribution); ii) trustworthiness of the organization (index score of reliability, mission congruence, openness to discussion); and iii) how often organizations interact with that member organization (measured as frequency of interaction on a likert scale). We examined independent variables that measured organizational type, perceptions of outcomes achieved, and reasons for success in the collaborative. We found some variables significantly related to the variation in our three outcome variables (table 2). For organizations identifying increased services as one of their collaborative’s outcomes, a higher frequency of interaction was predicted. Organizations identifying lower frequency of interaction were businesses, dental, faith-based, funders, law enforcement, and public health. Higher trust and value scores were significantly related to organizations identifying exchange of knowledge information as a reason for success in the collaborative. Businesses, government, funders, hospitals, law enforcement, non-profits, primary care, and public health organizations reported lower trust scores for their partner organizations. Finally, funders, non-profits, public health, and professional organizations reported significantly lower value scores for their fellow collaborative partners.
Table 2.
HLM results of outcomes, success, reasons for success and organization type on frequency of interaction, trust, and value (significant results only reported).
| Predictor variables | Frequency of interaction | Trust coefficient | Value coefficient |
|---|---|---|---|
| Level 2 predictors | |||
| Outcomes | |||
| Increased services | 0.216 | - | - |
| Reasons for success | |||
| Exchanging knowledge | - | 0.402 | ** |
| information | |||
| Organization type | |||
| Business | -0.362 | -0.886 | - |
| Dental | -0.362 | - | - |
| Faith based | -0.632 | - | - |
| Government | - | -0.269 | - |
| Funder | -0.800 | -0.778 | -0.867 |
| Hospital | - | -0.591 | - |
| Law enforcement | -1.408 | -1.001 | - |
| Non-profit | - | -0.229 | -0.245 |
| Public health | -0.335 | -0.216 | -0.245 |
| Professional | - | - | -0.673 |
Coefficients were significant (P<0.05). There was only minimal model change between the unconditional model and the model with predictor variables; this means there was very little model improvement and therefore, the predictor variables do not explain our understanding of the outcome variables to a large degree.
Finally, we used traditional regression models at the organizational level to explore the second research question in more depth. Specifically, we looked at why some organizations are perceived as more valuable or trusted than others. Using a stepwise regression approach for resource contributions as our independent variables, we found that a few types of resources contributed by member organizations were significantly related to trust and value. Those organizations providing specific health expertise (β=0.250, P<0.001) and paid staff (β=0.250, P<0.001) received higher trust scores and those providing in-kind resources (β= -0.217, P<0.001) were associated with lower level of trust. Organizations providing paid staff (β=0.287, P<0.001) were also more highly valued.
Discussion
This exploratory analysis of 11 public health collaboratives has provided some insight into the demographics, network characteristics, and factors related to quality of relationships among members of PHCs. These findings inform what we know about the structure of public health collaboratives and how some organizational characteristics are related to relationships between members of collaboratives. From these analyses, we have identified the following summative points.
Public health collaboratives are unique in structure, although patterns of characteristics are evident. Overall, we found a high degree of variation among these 11 public health collaborative structures. These results demonstrate the uniqueness among public health collaboratives in terms of who is a member, their frequency of interaction, and the role that each organization plays in the network. Specifically, we were not able to identify a common role that public health agencies play in each collaborative. Some are central to the network, others are evenly embedded throughout the network, and still some find a role on the periphery of the network. Time (not measured) may play a role in these findings. It is not uncommon for a public health department to play a central role early in a collaborative’s formation, often as a facilitator/funder/convener, but as the collaborative matures, this role becomes shared by other members.24
The findings that transitivity and reciprocity mimic one another in a collaborative indicate that better information flow can occur when members form reciprocal relationships. It is not uncommon that a small set of members take the responsibility for attending meetings, leading subcommittees, and working outside meeting times. When more members participate in these kinds of activities, greater opportunities for reciprocity emerges. Increased reciprocal exchanges in turn will lead to more closed triples (any three members and the relationships between them - the measure of transitivity) and in turn better overall information flow throughout the collaboratives. Differences among organization types in the network are a key factor in how these partners value and trust one another. The many types of organizations that participate in public health collaboratives bring both benefits and a degree of complexity to these collaboratives that make working together a challenge. Mays and Scutchfield,17 refer to this characteristic as breadth and link this to an opportunity for more and diverse resources. What we learned from this analysis is that different types of organizational partners perceive the trust and value of their partners in unique ways. Funders are perceived as the most valuable in this data set. This is not surprising given that funding is a key factor in the initiation and sustainability of public health collaboratives.17,29 While the difference was not significant, it was surprising that public health agencies were not perceived as one of the top three valued organizations, given their prominent and trusted role in public health collaboratives. However, while other organizations might be perceived for their value more frequently, public health is ranked as the most trusted. This is a sign of the important role that public health agencies play in facilitation roles30 and explain why public health agencies are often identified by members as key players in these types of collaboratives.24 Differences in perceptions of partners’ value and trust of one another can inform practice, specifically when collaboratives are identifying potential roles and functions of members. While it may be surprising that some organizations can be highly valued but not trusted (or viceversa), it could simply mean that organizations play different roles in these collaboratives and it may not be necessary that they play both of these roles simultaneously. The implications of this guide public health collaboratives in strategic thinking about how to leverage organizations with both kinds of characteristics (for example, identifying organizations that are trusted but not perceived as having as much value to fill roles where trust is a key factor for success; or for example, identifying valuable members such as politicians and funders who do not regularly attend meetings (something that often breeds trust) but play important roles in the work of the collaborative (such as making policy change or implementation of programmes). Network members’ characteristics play an important role in social exchanges. Certain resource contributions, a network member’s perception of outcomes achieved, and identified reasons for success play a role in the quality of partner interactions (the frequency of interaction and levels of trust and value among members). First, a network member’s resource contributions seem to influence how they are valued and trusted. The amount and type of resource that members contribute appears to be a factor in how much members trust one another. Organizations providing paid staff and specific health expertise were more trusted in these public health collaboratives, while organizations providing in-kind services received lower trust rankings. It is questionable whether organizations increase their trust levels when they commit paid staff and expertise, or that organizations that have more trust with other members are willing to commit these kinds of expertise. In other words, are members willing to commit more than in-kind resources when greater levels of trust exist in the collaborative? In these data, only increased services was associated with frequency of interaction. Other outcomes reported by the respondents were not associated with frequency of interaction. This finding is counter to the process that is most common within public health collaboratives; that is, that meeting regularly with more partners will result in more outcomes.31 The lack of evidence that meeting more often leads to better outcomes informs future research questions to determine how collaboratives can achieve outcomes and demonstrate success in ways other than adding new members, meeting more frequently, and demonstrating more activity. A focus on demonstrating the quality of interactions among members is the next step in understanding how working together in these processes can lead to more and better outcomes.
Conclusions
One of the difficult aspects of understanding factors to effective collaboration is the variance among the missions, process, and outcomes of each collaborative. While it would be ideal to identify a specific set of factors that will determine when a collaborative will be successful, we found in this study that the unique structure of each collaborative makes this a challenging exercise. The implications of these findings indicate that the research linking collaboration to outcomes must take into consideration the complex system of factors that influence outcomes. This includes the complex organizational and governance structures, variations in goals and processes, and the challenge of measuring outcomes that can be attributed to collaborative activities. Evaluators and researchers should use caution when generalizing about what an ideal collaborative structure looks like and why those factors might lead to successful outcomes, given the complex nature of the nested features of the inputs and outputs that can be considered. The practical implications for taking a systems approach to studying collaboration are evident. While getting a sense of factors that lead to success will inform collaborative practices, it is as important that each collaborative articulate its goals, take account of whether the process they are engaged in gets them closer to that goal, and then develop action steps that help them meet those goals.32 To engage in this, a quality improvement process should be implemented that includes planning (setting goals), implementing collaborative activities, collecting data on the collaborative process, and analyzing whether the process is meeting the goals. Future work on the evaluation and analysis of collaboratives should take into account differences among collaboratives, specifically the community context (e.g. geography, types of collaborative leadership, funding, governance structures, missions, etc.) as a way to identify factors related to effective collaboration.
This relatively small, exploratory study of public health collaboratives is a modest start to understanding the broad and largely unchartered landscape of public health and community collaboration. From this study, we have articulated a number of future research questions to contribute to our understanding of how working together collaboratively can lead to more and better outcomes. First, further study of how different sectors involved in community collaboratives and their variability in perception of the goals, governance structures, and resource availability (defined as breadth by Mays and Scutchfield17) can provide guidance on how to manage the diversity that comes with bringing together organizations from many sectors. Second, these data showed some evidence that there exists a large degree of variability in member’s perceptions of whether their collaboratives have been successful and which factors contribute to success. While we expected to find more consensus within each collaborative of the perceptions of success, we consistently found more disagreement among respondents than agreement. In other words, members of a collaborative vary widely in how they report their perceptions of whether the collaborative has achieved success or not. This leads us to question how members of public health collaboratives are defining success. It appears now that definitions of success include stark differences and a lack of consensus by members regarding whether the work of the collaborative has achieved that success. An important question that needs further examination is How can collaboratives measure their success if perceptions of goal attainment vary so greatly among members? The data from this analysis indicates that exchanging information and knowledge, sharing resources, bringing together diverse stakeholders and informal relationships created were among those reasons most frequently reported as factors associated with successful outcomes, giving us some indication of what leads to success. On the other hand, respondents who reported more outcomes also reported lower levels of success, indicating that perhaps having too many or disparate goals could have an impact on perceived effectiveness of the work. These data represent a small sample of collaboratives selected from the PARNTER dataset. Since this sample was pulled, the PARTNER dataset has grown to include over one hundred similar datasets. Future research includes analysis to answer these and other research questions with a dataset containing a larger number of PHCs. This study allowed us to identify future models to analyze as we explore ways for public health departments to improve their work toward strengthening their network of partners in order to address population health outcomes.
References
- 1.CDC. National Public Health Performance Standards Program. [Google Scholar]
- 2.Lasker RD.Broadening Participation in community problem solving: a multidisciplinary model to support collaborative practice and research. J Urban Health 2003;80:14-47; discussion 48-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zahner SJ.Local public health system partnerships. Public Health Rep 2005;120:76-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valente TW, Chou CP, Pentz MA.Community coalition networks as systems: effects of network change on adoption of evidence-based prevention. Am J Public Health 2007;97:880-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.PHAB. Public Health Accreditation Board. Available from: http://www.phaboard.org [Google Scholar]
- 6.Gulati R, Singh H.The architecture of cooperation: managing coordination costs and appropriation concerns in strategic alliances. Admin Sci Quart 1998:781-814 [Google Scholar]
- 7.Isett KR, Provan KG.The evolution of dyadic interorganizational relationships in a network of publicly funded nonprofit agencies. J Publ Adm Res Theor 2005;15:149-65 [Google Scholar]
- 8.Kapucu N.Interorganizational coordination in dynamic context: networks in emergency response management. Connections 2005;26:33-48 [Google Scholar]
- 9.Mandell MP.Getting results through collaboration: networks and network structures for public policy and management. Quorum Books, 2001 [Google Scholar]
- 10.Monge P, Heiss BM, Margolin DB.Communication network evolution in organizational communities. Commun Theor 2008;18:449-77 [Google Scholar]
- 11.Westley F, Vredenburg H.Interorganizational collaboration and the preservation of global biodiversity. Organ Sci 1997:381-403 [Google Scholar]
- 12.Parker B, Selsky JW.Interface dynamics in cause-based partnerships: an exploration of emergent culture. Nonprof Volunt Sec Q 2004;33:458-88 [Google Scholar]
- 13.Witte JM, Reinicke W, Benner T.Networked governance: developing a research agenda. Available from: http://isanet.ccit.arizona.edu/noarchive/Reinicke-Benner-Witte%20ISA%202002.pdf [Google Scholar]
- 14.Blau JR, Rabrenovic G.Interorganizational relations of nonprofit organizations: an exploratory study. Sociol Forum 1991;6:327-47 [Google Scholar]
- 15.Madhok A, Tallman SB.Resources, transactions and rents: managing value through interfirm collaborative relationships. Organ Sci 1998:326-39 [Google Scholar]
- 16.Singer HH, Kegler MC.Assessing interorganizational networks as a dimension of community capacity: illustrations from a community intervention to prevent lead poisoning. Health Educ Behav 2004;31:808-21 [DOI] [PubMed] [Google Scholar]
- 17.Mays GP, Scutchfield FD.Improving public health system performance through multiorganizational partnerships. Prev Chronic Dis 2010;7:A116. [PMC free article] [PubMed] [Google Scholar]
- 18.Mays G, Smith S, Ingram R, et al. Public health delivery systems: evidence, uncertainty, and emerging research needs. Am J Prev Med 2009;36:256-65 [DOI] [PubMed] [Google Scholar]
- 19.Raynor J.What makes an effective coalition? Evidence-based indicators of success. Available from: http://www.mcf.org/resources/evidence-based-indicators-of-coalition-success [Google Scholar]
- 20.QAP. Quality Assurance Project. Accessed on: 16 September2010. Available from: http://www.qaproject.org/methods/resmeasure.html [Google Scholar]
- 21.Luke DA, Harris JK.Network analysis in public health: history, methods, and applications. Annu Rev Public Health 2007;28:69-93 [DOI] [PubMed] [Google Scholar]
- 22.Harris JK, Clements B.Using social network analysis to understand Missouri’s system of public health emergency planners. Public Health Rep. 2007;122:488-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wholey D, Gregg W, Moscovice I.Public health systems: a social network perspective. Health Serv Res 2009;44:1842-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Varda DM, Chandra A, Stern S, Lurie L.Core dimensions of connectivity in public health collaboratives. J Public Health Manag Pract 2008;14:E1-7 [DOI] [PubMed] [Google Scholar]
- 25.Rothenberg RB.Commentary: sampling in social networks. Connections 1995;18:104-10 [Google Scholar]
- 26.Scott J.Social network analysis: a handbook. London, Sage Publications, 1991 [Google Scholar]
- 27.Wasserman S, Faust K.Social network analysis: methods and applications. Cambridge University Press, New York, 1994 [Google Scholar]
- 28.Raudenbush S, Bryk A.Hierarchical Linear models: applications and data analysis methods, 2nd Ed Newbury Park, Sage Publications, 2002 [Google Scholar]
- 29.Huxham C, Vangen S.Managing to collaborate: the theory and practice of collaborative advantage. London, Routledge, 2005 [Google Scholar]
- 30.Taylor-Robinson DC, Lloyd-Williams F, Orton L, et al. Barriers to partnership working in public health: a qualitative study. PloS ONE 2012;7:e29536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varda DM.Data-driven management strategies in public health collaboratives. J Public Health Manag Pract 2011;17:122-32 [DOI] [PubMed] [Google Scholar]
- 32.Varda D, Shoup JA, Miller S.A systematic review of collaboration and network research in the public affairs literature: implications for public health practice and research. Am J Public Health 2012; 102:564-71 [DOI] [PMC free article] [PubMed] [Google Scholar]


