Abstract
Qatar has a high burden of chronic diseases including obesity, cardiovascular disease and type 2 diabetes mellitus. Low serum vitamin D levels have been implicated in the development and progression of a range of these chronic conditions. The prevalence of vitamin D insufficiency or deficiency in the general population of Qatar has still not been investigated. The aim of this study was to carry out a systematic review of published studies documenting the prevalence of vitamin D insufficiency or deficiency in the Qatari population. A search strategy was developed for online databases (PubMed, Ovid MEDLINE, Embase and Embase Classic) between 1980 to the last week of August 2012, and bibliographies of the included studies were further searched for additional reports. Search terms used were QATAR and VITAMIN D. Studies reporting the serum levels of vitamin D in several Qatari sub-populations were identified. Weighted-average vitamin D serum levels and prevalence of low vitamin D status (<75 nmol/L) were calculated. Subgroup analysis was carried out by age. The quality of each study was evaluated according to four criteria: national representativeness, representation of males and females, the sample size, and the sampling protocol. A total of 16 relevant publications were identified, and 8 of these (reporting from 7 unique studies) met our inclusion and exclusion criteria with a total number of 1,699 Qatari subjects. The pooled sample size weighted-average vitamin D concentration (±SD) was 45.3±14.3 nmol/L (95% CI: 44.6-46.0; range 29.2-66.9 nmol/L). The weighted-average prevalence of low vitamin D status was 90.4% (95% CI: 90.1-91.0; range 83%-91%). Age was inversely correlated with vitamin D levels and directly with its insufficiency/deficiency prevalence. There have only been a few studies on the prevalence of low vitamin D in Qatar a very high prevalence of vitamin D insufficiency/deficiency in Qatar that increases with age has been suggested. The present report underlines the need to develop a nationally representative study to further evaluate vitamin D status in Qatar. Given the growing evidence of the role of vitamin D in chronic disease, this study could help develop public health strategies for disease prevention in Qatar.
Key words: Qatar, vitamin D, prevalence, prevention, public health, systematic review
Significance for public health
Low serum vitamin D levels have been implicated in the development and progression of a range of chronic conditions. A few studies have evaluated the prevalence of low vitamin D status in Qatar and how this possibly causes chronic disease. The limited information available suggests a high prevalence of vitamin D insufficiency/deficiency in Qatar and reinforces the need to develop a nationally representative study to further evaluate vitamin D status in the Qatari population. Subsequently, the present report could help develop public health strategies for disease prevention in Qatar.
Introduction
It has recently been reported that member states of the Gulf Cooperative Council (GCC, Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates) have a higher burden of chronic diseases [e.g., metabolic syndrome, type 2 diabetes mellitus (T2DM), obesity, and cardiovascular diseases] than most developed countries.1,2 Qatar has one of the highest prevalence rates of obesity among all GCC countries after Kuwait, and is ranked sixth globally; 45.3% of the entire Qatari population is obese.3 Qatar was also reported to have the highest rate of obesity among boys in the Middle East and North African region.2,4 Furthermore, according to recent estimates,1,2,4 Qatar has high prevalence rates of hypertension (32%), metabolic syndrome (27%), hyperglycemia (13%), diabetes and cardiovascular diseases (approx. 240 cases/100,000 for both conditions)5 among other countries in the Middle East, North Africa and the Eastern Mediterranean Region.1,2,4,6,7
The increasing rate of non-communicable diseases in Qatar, as with other GCC states, is believed to be influenced by genetic predisposition8,9 and the rapid socio-economic growth that has led to a more sedentary lifestyle.10,11 Furthermore, several reports have highlighted a growing pattern of an unhealthy diet and micronutrient deficiency as major factors in the increasing incidence of metabolic derangements and, subsequently, metabolic syndrome-related chronic diseases.2,4,11-14 In this context, vitamin D hypovitaminosis has received particular attention.11 The consensus of available information implicates low serum vitamin D levels as a factor influencing the development of a range of chronic conditions, such as metabolic syndrome, insulin resistance, type 2 diabetes mellitus and cardiovascular diseases.15-18 These findings are supported by observations from populations around the world, including the US,19 Europe,20 New Zealand21 and Asia,22 and are thought to be related to the immunomodulatory function of vitamin D.23 Although egg yolks, seafood oil, oily fish, and beef liver, together with fortified food, are the major dietary sources of vitamin D, it is more readily accessible through exposure to sunlight.24 However, several studies show that vitamin D insufficiency can be quite prevalent even in sunny regions of the world.11,25-28 In the sunny Gulf region, numerous reports have demonstrated a high prevalence of low vitamin D status.2,11 In fact, the Gulf region has some of the highest vitamin D insufficiency rates in the world29 and Qatar is thought to have one of the highest vitamin D deficiency/insufficiency rates. The high prevalence of low vitamin D status in the Gulf region is believed to be due to several socio-cultural and other factors, e.g. avoiding the sun during the summer months in order to maintain a fair complexion (particularly among women), the intense heat, the habit of not fortifying dairy products, and incorrect supplementation.2-4,11-14 Genetic predisposition to lower serum vitamin D synthesis and skin pigmentation may also play a role in vitamin D deficiency. For example, it was shown that subjects of Asian origin exhibit lower serum levels of vitamin D compared to their Caucasian counterparts even when they are exposed to the same amount of sunlight.18 In Qatar, as with other GCC states, there is an apparent coincidence of a unique lifestyle, heterogeneous population genetics, low vitamin D intake/exposure, and a high prevalence of obesity, type 2 diabetes mellitus, and cardiovascular and other chronic diseases. To better understand the mechanisms by which these chronic disorders develop, it is essential to examine the etiological role of vitamin D deficiency. Before any relationship can be confirmed, the extent of vitamin D insufficiency or deficiency in Qatar must be accurately evaluated. The present review was undertaken in an attempt to systematically examine the published evidence on the prevalence of vitamin D insufficiency or deficiency in the Qatari population. Defining the magnitude of this health problem will allow effective public health strategies for chronic disease prevention and control to be designed.
Design and methods
Search strategy and inclusion criteria
A search was conducted in PubMed, Ovid MEDLINE, Embase and Embase Classic databases between 1980 to the last week of August 2012 using the search term (MeSH) VITAMIN D and the keyword QATAR. The search retrieved 27 English language studies (Figure 1). After eliminating duplicate listings, and initial screening of the titles and abstracts, a total of 16 peer-reviewed articles were selected and the full articles were retrieved. A bibliography search did not identify any additional studies. Inclusion criteria were limited to studies that reported vitamin D levels in male and female subjects of all age groups and in healthy populations (non-vitamin D deficient and defined as healthy) from available social groups (e.g,. school children, health professionals, athletes, students, etc.).
Figure 1.
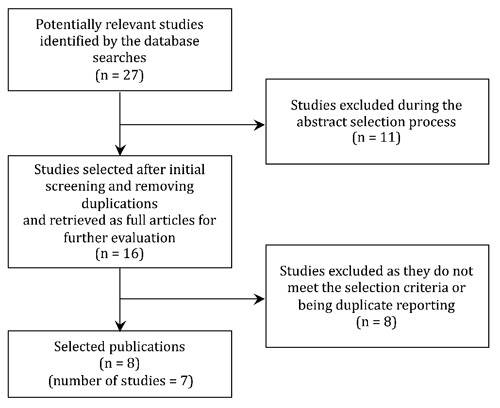
Systematic literature review process. The flow diagram describes the systematic review of literature on vitamin D status in Qatar. The selected 8 reports represent 7 unique studies.
We excluded studies in which vitamin D was reported in subjects with hypovitaminosis D,30,31 hypocalcemia32 or rickets.33 One study, reported in 2 publications with different details, divided the population into vitamin D sufficient (50-200 nmol/L) and deficient (<50 nmol/L) with no mention of the average population levels:34,35 there was also one review article.11 Another study was shown in 2 different reports36,37 and we excluded the earlier publication.36 Eight publications (from 7 unique studies) reported the level of vitamin D in their study populations and satisfied our selection criteria; these were included in the review.37-44 From the studies included, 2 reports were considered as one study42,43 since the same population and findings were presented again (but with additional information) in the more recent report. From these 2 studies,42,43 we examined vitamin D in healthy controls only and excluded information from those children with asthma37 or diabetes.42,43
Inter-reviewer agreement
The abstracts of the selected studies were independently reviewed by 2 readers (AB and BG-B). Differences were resolved through discussion until a consensus was reached. As stated above, only 7 unique studies (from 8 reports) were reviewed according to the selection criteria. Percentage agreement and Cohen’s Kappa (k) statistic45 were calculated and interpreted in accordance with Landis and Koch’s benchmarks46 for assessing the agreement between reviewers as poor (<0), slight (0.0-0.20), fair (0.21-0.40), moderate (0.41-0.60), substantial (0.61-0.80), and excellent (0.81-1.0). The agreement on the inclusion between the two reviewers was 94%, with k=0.88.46
Definition of the vitamin D deficiency
Optimal vitamin D effects on the skeleton and on calcium metabolism are achieved at a serum 25-hydroxyvitamin D [25(OH)D] level of more than 75 nmol/L.24 Vitamin D deficiency is defined as a serum 25(OH)D less than 50 nmol/L; insufficiency is considered at 51-75 nmol/L. For the purposes of this study, and clarity of presentation, we categorised subjects with less than 75 nmol/L as vitamin D insufficient/deficient, though this definition would include those technically deficient in vitamin D. Vitamin D concentrations were converted from the reported ng/mL to nmol/L.
Study subjects and data analysis
A total of 1767 healthy subjects from Qatar (i.e. Qatari nationals and expatriates) were included from the 8 selected reports from 7 studies.37-44 There were 795 males (46.8%) and 904 females (53.2%) and the male-to-female ratio was 1:1.14. There were 68 missing subjects (not reported by gender) from 2 studies: 19 subjects were missing from the study by Bener et al.37 and 46 subjects were missing from the study by El-Manyar et al.44 Therefore, 1699 subjects were evaluated in this study. We determined the weighted-overall average and weighted average age-related vitamin D serum concentrations, and prevalence estimates for vitamin D insufficiency/deficiency and 95% confidence intervals (95% CI) by pooling values from studies meeting the selection criteria and calculating averages weighted by sample size as previously described.47
Assessment of the methodological quality of studies
The methodological quality of each study was evaluated as previously described1 with some modification. Quality of the study was based on four criteria: national representativeness, equal representation of both sexes, robustness of the sample size (at least 400 subjects), and an explicit sampling protocol. For each criterion, each study was given a score (0 or 1, with 1 being high quality). The total score was calculated for each study (score range 0-4). Quality scores of 4, 3, 2 or 1 were considered excellent, good, fair or poor, respectively.
Results
Selected studies and study populations
Eight studies met our inclusion and exclusion criteria. The progression of studies through the search and selection process is illustrated in Figure 1. The selected studies were carried out on different Qatari sub-populations including children (<16 years old), health care professionals, sportsmen and female college students, as well as retrospectively from hospital records (Table 1). The weighted-average age of the studied sub-populations was 27.7±14.3 years (95% CI: 8.7-37.2). The number of subjects examined in each of these studies ranged from 64 to 498 with an almost equal gender representation (overall male-to-female ratio 1:1.14). The samples in these studies were collected between winter 2007 to fall 2010; one study did not state the duration of recruitment.39
Table 1.
Characteristics of the selected studies and study populations.
| Study | Study population | Study design | Duration of recruitment | n | Average age (years±SD)* | M:F (%) | Quality score° |
|---|---|---|---|---|---|---|---|
| Bener et al.42,43# | Children | Case-control | Aug-Dec 2007 | 170 | 9.9±4.2 | 47:53 | 2 |
| Bener et al.37 | Children | Case-control | Oct 2009-July 2010 | 464 | 8.01±4.6 | 55:45 | 3 |
| Mahdy et al.41 | Health care professionals | Cross-sectional | Jan 2007-Jan 2008 | 340 | 37.9§ | 40:60 | 2 |
| El-Menyar et al.44 | Hospital record | Retrospective | Jan 2008-Nov 2009 | 498 | 49±13 | 44:56 | 3 |
| Hamilton et al.40 | Sportsmen | Cross-sectional | April-Oct 2008 | 92 | 21.3±6.9 | 100:0 | 1 |
| Shrief and Rizk38 | College girls | Cross-sectional | Spring-fall 2010 | 71 | 23^ | 0:100 | 1 |
| Racinais et al.39 | School girls | Cross-sectional | NS | 64 | 11.7±1.5 | 0:100 | 0 |
*Values represent mean±standard deviation (SD).
°Quality score was calculated as described in Materials and Methods.
#The same study reported in two publications, with additional information in the more recent report.
§SD was not mentioned in the original report.
^Median age as calculated from the reported age range. NS, not stated in the original report.
None of the selected studies were drawn from a nationally- or geographically-representative sample. Therefore, none scored the full 4 points assigned for quality assessment. Two studies scored 3 out of 4 quality points and were considered to be of a good quality since they reported an almost equal gender representation, large sample size (>400 subjects), and an explicit sampling methodology. Two studies were of fair quality while the remaining 3 reports were considered poor (Table 1). Despite their scoring, the 3 poor reports were included in the present study to avoid any selection bias and to ensure a comprehensive evaluation of the prevalence of vitamin D insufficiency in Qatar.
Vitamin D levels and deficiency prevalence
The pooled sample size weighted-average level of vitamin D in the Qatari sub-populations studied was 45.3±14.3 nmol/L (95% CI: 44.6-46.0) (Table 2). This estimate was generated from 4 studies with a sample size of 1,472 subjects. Three studies did not report the average vitamin D serum levels in the study population.38-40 The weighted-average prevalence of vitamin D insufficiency/deficiency (<75 nmol/L) was 90.4% (95% CI: 90.1-91.0), an estimate that was calculated from the 7 selected studies (n=1,699). In general, the vitamin D serum levels ranged from 29.2 to 66.9 nmol/L and the prevalence of vitamin D deficiency in the sub-populations studied ranged between 83% and 91% if the 3 studies with low quality score were excluded.
Table 2.
Average vitamin D serum levels and deficiency/insufficiency in the Qatari population at different age groups.
| Age group | Study | Study | Average serum vitamin D levels | Prevalence of vitamin D <75nmol/L | |
|---|---|---|---|---|---|
| Years* | n | n | (nmol/L) | (%) | |
| <16 | 698 | Bener et al.42,43# | 170 | 46.2±23.0 | 85 |
| Bener et al.37 | 464 | 66.9±24.7 | 83 | ||
| Racinais et al.39 | 64 | NS | 100 | ||
| Weighted average§ | (60.6-62.2) | (85.9-86.4) | |||
| 61.4±10.0 | 86.2±2.4 | ||||
| 16-30 | 163 | Hamilton et al.40 | 92 | NS | 100 |
| Shrief and Rizk38 | 71 | NS | 97 | ||
| Weighted average | ^ | 93.9±5.3 | |||
| (93.5-94.3) | |||||
| >30 | 838 | Mahdy et al.41 | 340 | 29.2 | 97 |
| El-Menyar et al.44 | 498 | 35.9±27.5 | 91 | ||
| Weighted average | 33.2±3.4 | 93.4±3.1 | |||
| (31.9-32.5) | (93.1-93.6) | ||||
| O verall° | 1699 | Weighted overall average | 45.3±14.3$ | 90.4±7.2** | |
| (44.6-46.0) | (90.1-90.8) | ||||
*Stratifying vitamin D level by age was carried out from the average age of the study population (Table 1). Stratifying vitamin D level by gender from the selected reports was not possible given the way in which the data were in the original studies.
°Overall represents the entire age range from <16 to >30 years.
#The same study reported in two publications, with additional information in the more recent report.
§Data represent weighted average±standard deviation (SD). Numbers in parentheses are 95% confidence intervals (CI) for weighted average.
^Data in three of the selected studies (ref. ns. 38-40) did not allow this value to be generated.
$Calculated from 1472 subjects extracted from 4 of the selected studies in which the relevant information was available (ref. ns. 37, 41-44).
**Calculated from the 7 selected studies (n=1699). NS, values not stated in the original report.
Vitamin D in different age groups
The selected studies spanned three main age groups: under 16 years of age (3 studies from 4 reports),37,39,42,43 16-30 years of age (2 studies) 38,40 and over 30 years of age (2 studies).41,44 We estimated the weighted-average vitamin D serum concentration and prevalence of insufficiency/deficiency in each of these age groups (Table 2). Age group was inversely correlated with vitamin D serum concentration (Spearman’s correlation coefficient r=approx. 0.803; 95% CI: 0.79-0.82) and directly with the prevalence of vitamin D insufficiency/deficiency (r=0.26; 95% CI: 0.22-0.30). Vitamin D concentration was approximately 50% lower in the oldest age group compared to the youngest. This was accompanied by an increased prevalence of insufficiency/deficiency (86.2%-93.4%) in the youngest and oldest groups, respectively.
Discussion
There are few published reports on vitamin D status in Qatar. However, given the limited number of studies available, and despite the heterogeneity of the characteristics (subject age, social group, study design and study quality) of studies included in this review (Table 1), there was an overall consensus on the presence of low vitamin serum levels and high prevalence of its insufficiency/deficiency in Qatar. Approximately 90% of the population had 25(OH)D levels below the optimal level (weighted-average level 45.3±14.3 nmol/L) (Table 2). As advocated by the National Academy of Sciences Institute of Medicine (IOM), the optimal level of serum vitamin D is over 75 nmol/L with levels around 50-75 nmol/L considered insufficient.24 None of the studies found were geographically- or demographically-representative so an accurate estimate of national vitamin D insufficiency/deficiency for Qatar can not be made. However, based on the evidence generated from this systematic review, about 90% of the Qatari population may have insufficient levels of serum vitamin D. This estimate is similar, if not higher, than that reported from other Arab and Gulf countries.2,11,29 Prevalence among adolescent Saudi girls and women indicates the severity of the insufficiency with up to 80% presenting with vitamin D levels below 25 nmol/L48 (Table 3). A similar prevalence of vitamin D deficiency was also reported in UAE women.49,50 Furthermore, in Saudi Arabian subjects with back pain, 83% had vitamin D levels below 22.5 nmol/L.51 Similar severe deficiency was also reported from Kuwait.52 As stated above, this high prevalence of low vitamin D status is thought to be linked to socio-cultural factors, the habit of not fortifying dairy products, and poor vitamin D supplementation.2,4,11-14
Table 3.
Prevalence of vitamin D insufficiency/deficiency in some Arab and Western countries and in Qatar.
| Country | Study group | Prevalence of low vitamin D (%) |
|---|---|---|
| Qatar | Population (this study) | 90 |
| Jordan | Adult females | 37 |
| Morocco | Adult females | 91 |
| Lebanon | Adolescent females | 32 |
| Adolescent males | 12 | |
| Saudi Arabia | Adolescent females | 80 |
| Tunisia | Adult females | 48 |
| USA | Population | 31 |
| Canada | Population | 70 |
The rates of vitamin D insufficiency/deficiency reported in Qatar and many GCC states, and in many population groups within nations at high latitude (i.e. in the northern hemisphere in countries with little sun exposure) are markedly higher than in many Western countries. In Canada, for example, approximately 70% of the population is vitamin D insufficient.53 However, in the United States, approximately 60% of the population were found to have sufficient levels of vitamin D whereas 25% were at risk of vitamin D insufficiency and 8% were deficient54 (Table 3). Ethnic minority groups (originally from Arab countries) living in northern Europe, the USA and Australia have also shown a high prevalence of low vitamin D status.55 For example, over 80% of the Moroccan women immigrants in the Netherlands had less than 25 nmol/L of 25(OH)D, rates that are similar to those reported in veiled women in Australia.55 Comparison between the frequencies of vitamin D deficiency in Qatar can also be made with those reported in the home countries of major population sub-groups present in Qatar. For example, a large proportion of the expatriates in Qatar are from southern and eastern Asia. Analysis of vitamin D in women of reproductive and post-menopausal ages from southern India showed that the frequency of deficiency can reach 76% and 70% in these two groups, respectively.56 These frequencies are still lower than those reported in the Qatari population but higher than those from the USA and Canada (Table 3).
Several studies16,23,57-61 showed an inverse association between serum 25(OH)D and a wide array of chronic diseases, such as cancer, autoimmune disorders, atherosclerosis, and cardiovascular diseases. Furthermore, an inverse relationship was recently reported between vitamin D serum levels and a number of chronic disease-predisposing conditions such as metabolic syndrome,18 insulin resistance,62 cardiometabolic diseases,63 and obesity.64 This suggests that vitamin D insufficiency/deficiency may play a role at the early stages of the natural history of many chronic diseases.23 Vitamin D deficiency may, therefore, explain, at least partially, the increased incidence of hypertension, metabolic syndrome, hyperglycemia, obesity, diabetes and cardiovascular diseases in Qatar. Indeed, other host-related (e.g. genetic profile), environmental (e.g. sedentary lifestyle and diet), and social and economic (e.g. religion and economic growth) factors may work together to contribute to the increased rates of chronic disease not only in Qatar, but also in other countries with similar ancestral and socio-economic profiles.1,2,4,6,7,11
Age was inversely associated with vitamin D serum levels and directly with the prevalence of its deficiency in the sub-populations studied (Table 2). This observation is supported by various reports demonstrating lower vitamin D serum concentrations with increased age, as well as higher insufficiency/deficiency rates in the oldest age group compared to the youngest. For example, in healthy Saudi men in the over 50 years age group, 12% were deficient (compared to 10% in the younger age group) and 25% had insufficient 25(OH)D levels (compared to 18% in the younger men).65 Furthermore, in the United States, a recent study from the National Health and Nutrition Examination Survey (NHANES) reported that the prevalence of vitamin D deficiency is lower younger people whereas serum 25(OH)D is higher.54 Similarly, in the Canadian Health Measure Survey (CHMS) population, children aged 6-11 years were most likely to be above the adequacy cut-off values compared to the older adults.66 According to CHMS data, younger age groups were found to be more likely to consume vitamin D fortified dairy products (e.g. milk) compared to the older age groups. In addition, the increased obesity rates in adult population may be partially responsible for this age-related difference in vitamin D levels. Low plasma 25(OH)D concentrations are known to be common in obese subjects and a negative relationship with body fat distribution has been recently reported.67 This is thought to be due to the sequestration of vitamin D, as a fat-soluble micronutrient, in the adipose tissue in obese individuals.23,67 Furthermore, vitamin D deficiency may play a role in the development of asthma, rickets in children, and osteomalacia in adults. Rickets is currently largely found in some low-income countries in Africa, Asia or the Middle East,68 as well as in subjects with the pseudo-vitamin D deficiency rickets genetic disorders.69
Osteomalacia (a bone-thinning disorder) occurs exclusively in adults and is thought to contribute to chronic musculoskeletal pain.68,69 Individuals with this bone disorder benefit from vitamin D supplements with calcium. Although there is some evidence to suggest a link between vitamin D and asthma, particularly in children,36,37 the beneficial effect of supplements is still a question for debate70 and further research is warranted to confirm the etiological role of vitamin D in asthma.
The present study has some limitations and any interpretation of results should bear this in mind. Our findings are based on only a small number of studies (only 8 reports from 7 unique studies). These studies are not of exceptional quality, different study designs had been adopted, and diverse Qatari sub-populations had been studied with a wide age range. Furthermore, none of the selected studies were drawn from a nationally- or geographically-representative sample.
However, it is the first systematic review of the levels of vitamin D and the extent of its insufficiency/deficiency in Qataris. Furthermore, while the evidence base is limited, this review is the first to report that, in Qatar, such vitamin D insufficiency/deficiency is associated with age. The present report illustrates a gap in the knowledge on vitamin D in Qatar and reinforces the need for a nationally representative study to assess vitamin D status and its association with a range of chronic diseases known to occur at high incidence rates in Qatar. In Qatar, vitamin D should be introduced into public health intervention strategies for chronic disease prevention, and changes in lifestyle and diet should be promoted.
Current practices for the prevention of diseases related to vitamin D insufficiency (e.g., type 2 diabetes mellitus, cardiovascular diseases and osteomalacia) in the general population include changes in lifestyle and diet, and exercise. Vitamin D supplements may help prevent and control these conditions through its anti-oxidant, anti-inflammatory and immunomodulatory properties.23,58 Therefore, it is reasonable to suggest that the two preventive approaches (i.e. vitamin D supplements and changes in lifestyle) may be combined into a single public health programme to enhance the success and effectiveness of intervention.57,58 This strategy could be more efficient in reducing the pre-clinical disease status and, subsequently the disease burden, than when a single approach is considered. Furthermore, such a combined strategy can be introduced into general practice settings as well as in a population-based fashion with low expenditure and minimal side effects. This approach should principally target subjects with vitamin D insufficiency when considering the socio-cultural factors contributing to the low vitamin D status, e.g. women, children, and obese or heavyweight subjects.
Acknowledgments
This systematic review was supported by the Public Health Agency of Canada (AB, PA) and the Supreme Council of Health, Qatar (AB, ES, A-AA-T and MHA-T). The authors thank Bibiana Garcia-Bailo (BG-B) for reviewing the abstracts with AB during the initial screening of the studies. Received for publication: 27 September 2012.
References
- 1.Mabry RM, Reeves MM, Eakin EG, et al. Gender differences in prevalence of the metabolic syndrome in Gulf Cooperation Council Countries: A systematic review. Diabet Med 2010:27:593-7 [DOI] [PubMed] [Google Scholar]
- 2.Fahed AC, El-Hage-Sleiman A-KM, Farhat TI, et al. Diet, genetics, and disease: A focus on the Middle East and North Africa Region. J Nutr Metab 2012: doi:10.1155/2012/109037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Anouti F, Thomas J, Abdel-Wareth L, et al. Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermatoendocrinol 2011:3:235-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Musaiger AO, Hassan AS, Obeid O. The Paradox of Nutrition-Related Diseases in the Arab Countries: The Need for Action. Int J Environ Res Public Health 2011:8:3637-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization-WHO. Global Status Report on Non-Communicable Diseases 2010. WHO, Geneva, Switzerland, 2011
- 6.Alhyas L, McKay A, Balasanthiran A, et al. Prevalence of overweight, obesity, hyperglycaemia, hypertension and dyslipidaemia in the Gulf: Systematic review. J R Soc Med Sh Rep 2010:2:55 DOI 10.1258/shorts.2011.011019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng SW, Zaghloul S, Ali HI, et al. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf States. Obes Rev 2011:12:1-13 [DOI] [PubMed] [Google Scholar]
- 8.Nemr R, Salman RA, Jawad LH, et al. Differential contribution of MTHFR C677T variant to the risk of diabetic nephropathy in Lebanese and Bahraini Arabs. Clin Chem Lab Med 2010:48:1091-4 [DOI] [PubMed] [Google Scholar]
- 9.Al-Daghri NM, Al-Attas OS, Alokail MS, et al. Adiponectin gene polymorphisms (T45G and G276T), adiponectin levels and risk for metabolic diseases in an Arab population. Gene 2012:493:142-7 [DOI] [PubMed] [Google Scholar]
- 10.Malik M, Razig SA. The prevalence of the metabolic syndrome among the multiethnic population of the United Arab Emirates: a report of a national survey. Metab Syndr Relat Disord 2008:6:177-86 [DOI] [PubMed] [Google Scholar]
- 11.Fields J, Trivedi NJ, Horton E, et al. Vitamin D in the Persian Gulf: Integrative Physiology and Socioeconomic Factors. Curr Osteoporos Rep 2011:9:243-50 [DOI] [PubMed] [Google Scholar]
- 12.Musaiger OA, Al-Hazzaa HM, Takruri HR, et al. Change in nutrition and lifestyle in the Eastern Mediterranean Region: Health impact. J Nutr Metab 2012. doi:10.1155/2012/436762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Musaiger OA. Nutritional status of infants and young children in the Arabian Gulf Countries. J Trop Pediatr 1996:42:121-4 [DOI] [PubMed] [Google Scholar]
- 14.Musaiger OA. Nutrition situation in the Arabian Gulf Countries. J R Soc Promot Health 1986:105:104-6 [DOI] [PubMed] [Google Scholar]
- 15.Forouhi NG, Luan J, Cooper A, et al. Baseline serum 25-hydroxy vitamin D is predictive of future glycemic status and insulin resistance: the Medical Research Council Ely Prospective Study 1990-2000. Diabetes 2008:57:2619-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pittas AG, Chung M, Trikalinos T, et al. Systematic review: vitamin D and cardiometabolic outcomes. Ann Intern Med 2010:152:307-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holick MF. Vitamin D: a D-Lightful health perspective. Nutr Rev 2008:66: S182-S194 [DOI] [PubMed] [Google Scholar]
- 18.Brenner DR, Arora P, Garcia-Bailo B, et al. Plasma vitamin D and risk of the metabolic syndrome in Canadians. Clin Invest Med 2011:34:E377-E384 [DOI] [PubMed] [Google Scholar]
- 19.Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care 2004:27:2813-8 [DOI] [PubMed] [Google Scholar]
- 20.Hypponen E, Boucher BJ, Berry DJ, et al. 25- hydroxyvitamin D IGF-1, and metabolic syndrome at 45 years of age: a cross-sectional study in the 1958 British Birth Cohort. Diabetes 2008:57:298-305 [DOI] [PubMed] [Google Scholar]
- 21.von Hurst PR, Stonehouse W, Coad J. Vitamin D supplementation reduces insulin resistance in South Asian women living in New Zealand who are insulin resistant and vitamin D deficient - a randomised, placebo-controlled trial. Br J Nutr 103:549-55 [DOI] [PubMed] [Google Scholar]
- 22.Kim MK, 2nd, Kang M, Won OK, et al. The association of serum vitamin D level with presence of metabolic syndrome and hypertension in middle-aged Korean subjects. Clin Endocrinol 2010:73:330-8 [DOI] [PubMed] [Google Scholar]
- 23.Badawi A, Klip A, Haddad P, et al. (2010) Type 2 diabetes mellitus and inflammation: Prospects for biomarkers of risk and nutritional intervention. Diabetes Metab Syndr Obes 2010:26:3:173-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Institute of Medicine (IOM) Food and Nutrition Board Dietary Reference Intakes for Calcium and Vitamin D. National Academy Press, Washington, Washington DC USA, 2011 [PubMed] [Google Scholar]
- 25.Levis S, Gomez A, Jimenez C, et al. Vitamin D deficiency and seasonal variation in an adult South Florida population. J Clin Endocrinol Metab 2005:90:1557-62 [DOI] [PubMed] [Google Scholar]
- 26.Gannage YMH, Chemali R, Yaacoub N, et al. Hypovitaminosis D in a sunny country: relation to lifestyle and bone markers. J Bone Miner Res 2000:15:1856-62 [DOI] [PubMed] [Google Scholar]
- 27.Van der Mei IAF, Ponsonby AL, Engelsen O, et al. The high prevalence of vitamin D insufficiency across Australian populations is only partly explained by season and latitude. Environ Health Persp 2007:115:1132-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mishal AA. Effects of different dress styles on vitamin D levels in healthy young Jordanian women. Osteoporos Int 2001:12:931-5 [DOI] [PubMed] [Google Scholar]
- 29.Lips P. Vitamin D status and nutrition in Europe and Asia. J Steroid Biochem 2007:103:620-5 [DOI] [PubMed] [Google Scholar]
- 30.Soliman AT, El-Dabbagh M, Adel A, et al. Clinical responses to a mega-dose of vitamin D3 in infants and toddlers with vitamin D deficiency rickets. J Trop Pediatrics 2010:56:19-26 [DOI] [PubMed] [Google Scholar]
- 31.Soliman AT, Adel A, Wagdy M, et al. Manifestations of severe vitamin D deficiency in adolescents: effects of intramuscular injection of a megadose of cholecalciferol. J Trop Pediatrics 2011:57:303-6 [DOI] [PubMed] [Google Scholar]
- 32.Toiema FH, Al Ansari K. Nineteen cases of symptomatic neonatal hypocalcemia secondary to vitamin D deficiency: a 2-year study. J Trop Pediatrics 2010:56:108-10 [DOI] [PubMed] [Google Scholar]
- 33.Soliman AT, Al Khalaf F, Alhemaidi N, et al. Linear growth in relation to the circulating concentrations of insulin-like growth factor I parathyroid hormone, and 25-hydroxy vitamin D in children with nutritional rickets before and after treatment: endocrine adaptation to vitamin D deficiency. Metabolism 2008:57:95-102 [DOI] [PubMed] [Google Scholar]
- 34.Bener A, Al-Ali M, Hoffmann GF. Vitamin D deficiency in healthy children in a sunny country: associated factors. Int J Food Sci Nutr 2009:60:60-70 [DOI] [PubMed] [Google Scholar]
- 35.Bener A, Al-Ali M, Hoffmann GF. High prevalence of vitamin D deficiency in young children in a highly sunny humid country: a global health problem. Minerva Pediatr 2011:61:15-22 [PubMed] [Google Scholar]
- 36.Ehlayel MS, Bener A, Sabbah A. Is high prevalence of vitamin D deficiency evidence for asthma and allergy risks? Eur Ann Allergy Clin Immunol 2011:43:81-8 [PubMed] [Google Scholar]
- 37.Bener A, Ehlayel MS, Tulic MK, et al. Vitamin D deficiency as a strong predictor of asthma in children. Int Arch Allergy Imm 2012:157:168-75 [DOI] [PubMed] [Google Scholar]
- 38.Sharif EA, Rizk NM. The prevalence of vitamin D deficiency among female college students at Qatar University. Saudi Med J 2011:32:964-5 [PubMed] [Google Scholar]
- 39.Racinais S, Hamilton B, Li CK, et al. Vitamin D and physical fitness in Qatari girls. Arch Dis Child 2010:95:854-5 [DOI] [PubMed] [Google Scholar]
- 40.Hamilton B, Grantham J, Racinais S, et al. Vitamin D deficiency is endemic in Middle Eastern sportsmen. Pub Health Nutr 2010:13:1528-34 [DOI] [PubMed] [Google Scholar]
- 41.Mahdy S, Al-Emadi SA, Khanjar IA, et al. Vitamin D status in health care professionals in Qatar. Saudi Med J 2010:31:74-77 [PubMed] [Google Scholar]
- 42.Bener A, Alsaied A, Al-Ali M, et al. Impact of lifestyle and dietary habits on hypovitaminosis D in type 1 diabetes mellitus and healthy children from Qatar, a sun-rich country. Annal Nutr Metab 2008:53:215-22 [DOI] [PubMed] [Google Scholar]
- 43.Bener A, Alsaied A, Al-Ali M, et al. High prevalence of vitamin D deficiency in type 1 diabetes mellitus and healthy children. Acta Diabetol 2009:46:183-9 [DOI] [PubMed] [Google Scholar]
- 44.El-Menyar A, Rahil A, Dousa K, et al. Low vitamin D and cardiovascular risk factors in males and females from a sunny, rich country. Open Cardiovasc Med J 2012:6:76-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen A. Comparison of correlated correlations. Stat Med 1989:8:1485-95 [DOI] [PubMed] [Google Scholar]
- 46.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977:33:159-74 [PubMed] [Google Scholar]
- 47.Havemann BD, Henderson CA, El-Serag HB. The association between gastro oesophageal reflux disease and asthma: a systematic review. Gut 2007:56:1654-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mithal A, Wahl DA, Bonjour JP, et al. ; IOF Committee of Scientific Advisors (CSA) Nutrition Working Group 2009. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 2009:20:1807-20 [DOI] [PubMed] [Google Scholar]
- 49.El-Kaissi S, Sherbeeni S. Vitamin D deficiency in the middle east and its health consequences for adults from nutrition and health. In: Holick MF. (ed.) Vitamin D. Springer Science, 2010, pp. 495-503 [Google Scholar]
- 50.Hosseinpanah F, Rombad M, Hossein-nejad A, et al. Association between vitamin D and bone mineral density in Iranian post-menopausal women. J Bone Miner Metab 2008;26:86-92 [DOI] [PubMed] [Google Scholar]
- 51.Faraj S, Khalaf A. Vitamin D deficiency and chronic low back pain in Saudi Arabia. Spine 2003:28:177-9 [DOI] [PubMed] [Google Scholar]
- 52.El Sonbaty MR, Nu A-G. Vitamin D deficiency in veiled Kuwait women. Eur J Clin Nutr 1996:50:315-8 [PubMed] [Google Scholar]
- 53.Schwalfenberg GK, Genuis SJ, Hiltz MN. Addressing vitamin D deficiency in Canada: a public health innovation whose time has come. Public Health 2010:124:350-9 [DOI] [PubMed] [Google Scholar]
- 54.Looker AC, Johnson CL, Lacher DA, et al. Vitamin D status: United States, 2001-2006. National Center for Health Statistics, Centers for Disease Control and Prevention. Data Brief Report n. 59, 2011 [Google Scholar]
- 55.Prentice A. Vitamin D deficiency: a global perspective. Nutr Rev 2008:66: S153-S164 [DOI] [PubMed] [Google Scholar]
- 56.Harinarayan CV, Sachan A, Reddy PA, et al. Vitamin D status and bone mineral density in women of reproductive and post-menopausal age groups: A cross-sectional study from South India. J Assoc Phys India 2011:9:695-701 [PubMed] [Google Scholar]
- 57.Badawi A, Sadoun E, Al-Thani MH. Vitamin D and inflammation in the prevention of type 2 diabetes: Public health relevance. Reviews in Health Care 2012:3:247-59 [Google Scholar]
- 58.Garcia-Bailo B, El-Sohemy A, Haddad P, et al. Vitamins D, C and E in the prevention of type II diabetes mellitus: modulation of inflammation and oxidative stress. Biologics 2011:5:7-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pittas AG, Chung M, Trikalinos T, et al. Systematic review: Vitamin D and cardiometabolic outcomes. Ann Intern Med 2010:152:307-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Botella-Carretero JI, Alvarez-Blasco F, Villafruela JJ, et al. Vitamin D deficiency is associated with the metabolic syndrome in morbid obesity. Clin Nutr 2007:26:573-80 [DOI] [PubMed] [Google Scholar]
- 61.Teegarden D, Donkin SS. Vitamin D: emerging new roles in insulin sensitivity. Nutr Res Rev 2009:22:82-92 [DOI] [PubMed] [Google Scholar]
- 62.Garcia-Bailo B, Badawi A, El-Sohemy A. Vitamin D status and biomarkers of type 2 diabetes risk in an ethnically diverse population. Can J Diabetes 2011:35:432-3 [Google Scholar]
- 63.Brenner DR, Arora P, Garcia-Bailo B, et al. The relationship between metabolic syndrome components and inflammatory markers among non-diabetic Canadian adults. J Diabetes Metab 2012. doi:10.4172/2155-6156.S2-003 [Google Scholar]
- 64.Da Costa LA, Arora P, Garcia-Bailo B, et al. The association between obesity, cardiometabolic disease markers and innate immunity-related inflammation in Canadian adults. Diabetes Metab Syndrome Obesity 2012. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sadat-Ali M, Al Elq A, Al-Turki H, et al. Vitamin D levels in healthy men in eastern Saudi Arabia. Ann Saudi Med 2009:29:378-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Langlois K, Greene-Finestone L, Little J, et al. Vitamin D status of Canadians as measured in the 2007 to 2009 Canadian Health Measures Survey. Health Rep 2010:21:47-55 [PubMed] [Google Scholar]
- 67.Sulistyoningrum DC, Green TJ, Lear SA, et al. Ethnic-specific differences in vitamin D status is associated with adiposity. PLoS One 2012;7:e43159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lerch C, Meissner T, Lerch C. Interventions for the prevention of nutritional rickets in term born children. Cochrane Database of Systematic Reviews 2007:4;CD006164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zargar AH, Mithal A, Wani AI, et al. Pseudovitamin D deficiency rickets - a report from the Indian subcontinent. Postgrad Med J 2000:76:369-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hart PH. Vitamin D supplementation, moderate sun exposure, and control of immune diseases. Discov Med 2012:13:397-404 [PubMed] [Google Scholar]


