Abstract
Objective. To assess student satisfaction and learning of course objectives following the integration of virtual patient cases designed to promote active, patient-centered learning in an advanced therapeutics pharmacy course.
Design. A dynamic virtual patient platform that incorporated a branched-narrative, decision-making teaching model was used in an advanced therapeutics course to supplement lecture content.
Assessment. Presimulation and postsimulation tests were used to assess student learning. The use of virtual patients significantly enhanced student learning for both higher- and lower-level test questions (p<0.001 and p=0.01, respectively). Students agreed or strongly agreed that the virtual patient cases provided an effective way to learn (72%), were enjoyable (69%), and were appropriate in content (80%), and that more should be incorporated (59%).
Conclusion. The use of virtual patients in an advanced therapeutics practicum effectively promoted active, patient-centered learning; engaged students in an interactive and dynamic educational technology; encouraged teamwork; enhanced higher-level student learning; and improved student satisfaction in the course.
Keywords: virtual patients, active learning, simulation
INTRODUCTION
Graduates from colleges and schools of pharmacy are expected to be medication experts, providing patient-centered care with efficiency and effectiveness.1 The Center for the Advancement of Pharmacy Education has specifically addressed, through several domains, that graduates of doctor of pharmacy (PharmD) programs should possess the knowledge, skills, and attitudes upon program completion to provide patient-centered care; use problem-solving skills; collaborate with other health professions; and educate patients and other healthcare providers.1 To prepare graduates, accreditation standards set forth by the Accreditation Council for Pharmacy Education (ACPE) direct pharmacy educators to incorporate innovative, active-learning teaching methods into their curricula to develop students’ critical thinking, problem-solving, and interprofessional skills.2 Standard 11 specifically addresses teaching and learning methods, and advocates for patient simulation immersion experiences through the employment of educational technologies and techniques that support various modes of educational delivery and evaluation.
In support of Standard 11, ACPE has acknowledged that educational technologies replicating pharmacy practice activities and medication delivery to patients using simulated, standardized, and virtual patients provide a learning experience for students in the early pharmacy curriculum that is comparable to direct patient contact.3 In June 2010, the ACPE board approved a policy to allow such simulations to account for up to 20% of the introductory pharmacy practice experience time. As a result, educational technologies such as computer-aided instruction, virtual patients, and mannequin model simulators have become almost omnipresent in pharmacy education.4,5
Virtual patient technology has been used by educators throughout the health sciences to develop required knowledge and skills.4,6-8 Virtual patients simulate real clinical scenarios and allow learners to emulate the roles of healthcare providers by obtaining patient information and making diagnostic and therapeutic decisions.9 Virtual patients offer educators the opportunity to assess students’ decision-making skills regarding course content in a safe, high-fidelity environment, while allowing students to succeed, err, and learn individually.10 Despite these advantages, educational technologies like virtual patients can be underused in the curricula of higher education. Cultural, process, and academic obstacles to implementing such technologies in the classroom can be overwhelming and disabling.11 Specifically, attitudes of an institution towards technology and education must be positive, resources (eg, financial, personnel) must be made available to facilitate adoption, and the technology must satisfy the educational goals of the institution and needs of the students.
Our study assessed the design, development, implementation, and evaluation of a novel approach that used educational technology as an instructional tool and assessment measure in an advanced therapeutics course within a pharmacy curriculum. This teaching method used virtual patients to promote active, patient-centered learning, allowed students repetitive practice of course objectives, improved student self-awareness of course content, and met the curricular outcomes at the University of Pittsburgh School of Pharmacy.
DESIGN
Faculty members of the University of Pittsburgh School of Pharmacy modified the school’s educational and teaching processes by incorporating an active-learning strategy that used teamwork and educational technology to simulate practice experiences. This method provided students with individualized learning opportunities that aligned more closely with the educational outcomes and standards of the profession. The teaching strategy introduced patients to students via simulation during a practicum session, which historically had been a paper-based case discussion. The simulation was designed to reinforce concepts that were discussed during lecture through clinical decision-making, outcome realization of decisions, feedback from faculty members, and repetition of concepts not understood. Goals developed to realize this purpose included the design of complex virtual patient cases to offer students practical application of course content in a safe environment, integration of the cases into an advanced therapeutics course to replace traditional teaching methods, and assessment of student learning and satisfaction with this novel teaching strategy.
Faculty members used vpSim (Decision Simulation LLC, Chadsford, PA), a virtual patient platform developed by the Laboratory for Educational Technology at the University of Pittsburgh. The simulation content was written by 1 author and reviewed by a content expert. Faculty members spent approximately 50 hours developing the simulations, from writing the cases to implementing the program. No information technology support was needed. One author had previous experience with this program and served as the simulation expert. Virtual patient cases were developed through vpSim using a “branched-narrative” model, in which learners are presented with a challenge, given choices, and then provided with a consequence specific to their choice. Pharmacy students made clinical recommendations as healthcare providers for patient problems and then were given patient outcomes and faculty-derived feedback based on their decisions. Branching was relative to the student's decision making. For example, if a student correctly classified a patient, they would move on to design a treatment regimen. However, if students answered incorrectly, they were sent to a learning module and redirected to the same question until they answered correctly. The branched model allowed case writers to direct students down a learning path that was individualized to their knowledge, skill, and decision-making level, while ensuring students covered the prespecified learning objectives.
Simulation content was derived from subject matter in Pulmonology and Rheumatology, a required 2-credit advanced therapeutics course for third-year PharmD students. The course covered diseases related to pulmonology, including but not limited to chronic obstructive pulmonary disorder and asthma. In the course, students learned to design and monitor treatment regimens for patients and provide appropriate patient counseling and healthcare provider education. Lectures provided students with fundamental knowledge needed for each disease state and were typically followed by a practicum session. The structure of the asthma section of the course remained largely intact from previous years, with the exception of the simulation replacing paper-based cases. Course prerequisites included basic science courses (ie, anatomy and physiology, biochemistry), pharmacokinetics, and several therapeutics courses (infectious diseases, cardiovascular disease, and gastroenterology/nutrition). Students were not exposed to virtual patient technology in the classroom prior to the pulmonology/rheumatology course.
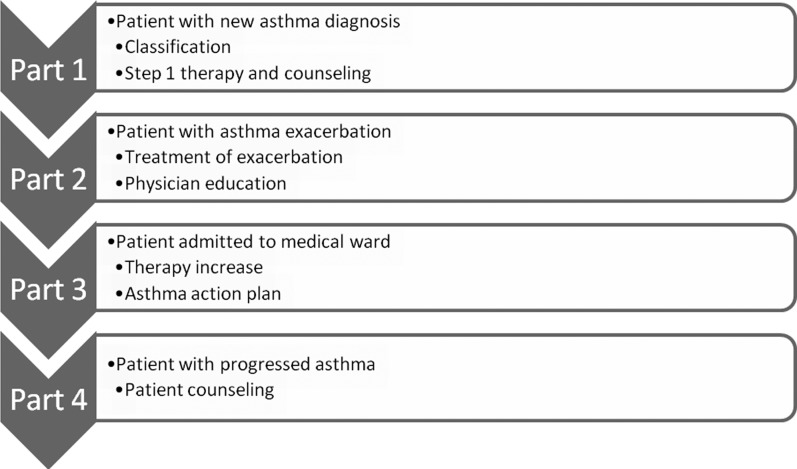
The virtual patient cases were integrated into the asthma practicum session within the pulmonology/rheumatology course. This 1-hour practicum was preceded by two 2-hour lectures and followed by a 1-hour inhaler laboratory session. The students were given 1 hour to complete the simulation, with the remaining time for the assessments and review session. Goals and objectives for the practicum experience are shown in Table 1. The first lecture was focused on the pathophysiology of asthma and its classification. The second lecture centered on the therapeutics of asthma, which included patient counseling points and healthcare provider education. After completing the pretest, each student group had 1 hour to complete the simulation followed by completion of the posttest. The remaining time was used to review key clinical decisions. During the practicum session, the interactive virtual patients were introduced and completion of the cases by students was mandatory for all learners. Following the lectures and the practicum session, students were exposed to a variety of inhalers, spirometers, and further patient counseling points. The cases were left open to allow students to access the virtual patients outside of dedicated class time.
Table 1.
Goals and Learning Objectives for an Asthma Practicum Session in an Advanced Therapeutics Pharmacy Course
The virtual patient cases were built from predefined goals and learning objectives (Table 1) developed through Bloom’s Taxonomy.12 The goals and purpose of the virtual patient cases were explained to the students by the instructor prior to the practicum. In addition, students were presented with an introduction to the virtual patient platform, which further elaborated on faculty objectives for the session.
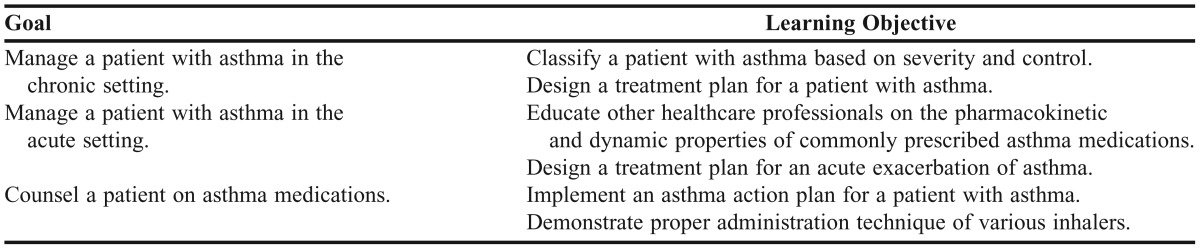
The cases combined several techniques to help the students actively learn. At the onset of the simulation, a newly diagnosed patient with asthma in a community pharmacy was presented. Students began making clinical decisions based on this case presentation. Students gauged the success of their recommendations through observed patient outcomes and feedback provided by faculty members throughout the simulation. Students who answered incorrectly were directed to tutorials to reinforce concepts. Following the tutorial, students were given a “chance of redemption” prior to continuing the case. At the end of each patient case, students were challenged with clinical questions from unrelated patient cases based on the concepts that they encountered. The challenges were meant to test the knowledge of the students and allow them to gauge their progress towards the learning objectives of the case. After completion of the initial challenge, the format of the simulation was repeated with 3 more patient encounters: an exacerbation in the emergency department, escalation of therapy on the medical ward, and further counseling in the community pharmacy (Figure 1). The simulation concluded with a learning summary outlining student decisions throughout the cases and a presentation of the faculty-derived goals and learning objectives for which the students would be held accountable.
Figure 1.
Progression of a patient case using virtual patients in an advanced therapeutics course.
The students traversed the simulation cases as teams of 5 to 6 students. At the completion of the practicum session, the instructor reviewed the simulation with the students. The instructor discussed pivotal clinical decisions made during the cases and provided further insight into the challenge questions. Faculty members were also given an opportunity to show students how an expert might have approached the cases. Finally, contact with the faculty members allowed students to further discern how the understanding of 1 concept (eg, classification of disease) directly affected the students’ decision making (eg, appropriate therapy).
EVALUATION AND ASSESSMENT
Assessment of student learning and perceptions was accomplished through presimulation and postsimulation assessments, and a satisfaction survey. Prior to the simulation, students were given a 6-question pretest. Course faculty members who served as the content experts established face validity of the questions. The content experts achieved consensus on level of difficulty of the questions based on Bloom’s taxonomy of learning activity levels.12 Three of the questions were determined to be higher-level learning (evaluation and application of material), while 3 were determined to be lower-level learning (knowledge based). Immediately following the simulation but prior to the review session, the students were given a posttest designed to be similar but not identical to the pretest in both content and difficulty. All pretest and posttest questions were constructed from predetermined learning objectives provided to the students during the lecture portion of the course and at the beginning of the simulation (Table 1).
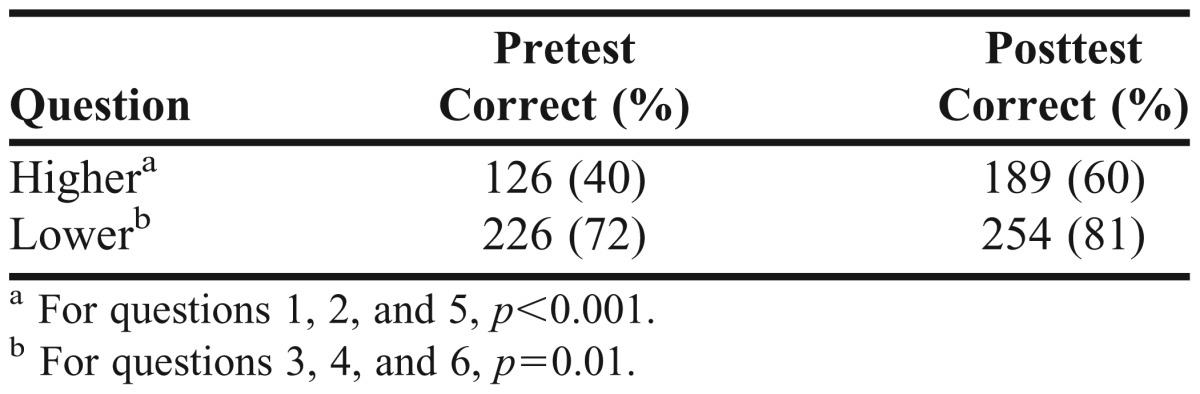
The pretest and posttest results are summarized in Table 2. The simulation session enhanced the students’ learning of both higher- and lower-level domains (p<0.001 and p=0.01, respectively). The proportion of students who correctly answered the higher-level questions increased by 20%, while the proportion of students who answered the lower-level questions increased by 9% (Table 3). The median examination score for all content was 77.7%, while the median examination score for the section on asthma was 84.6%. Faculty members other than those involved in this study constructed examinations from previous years. The scores from previous examinations were not readily available.
Table 2.
Presimulation and Postsimulation Test Scores in an Advanced Therapeutics Pharmacy Course (N = 105)
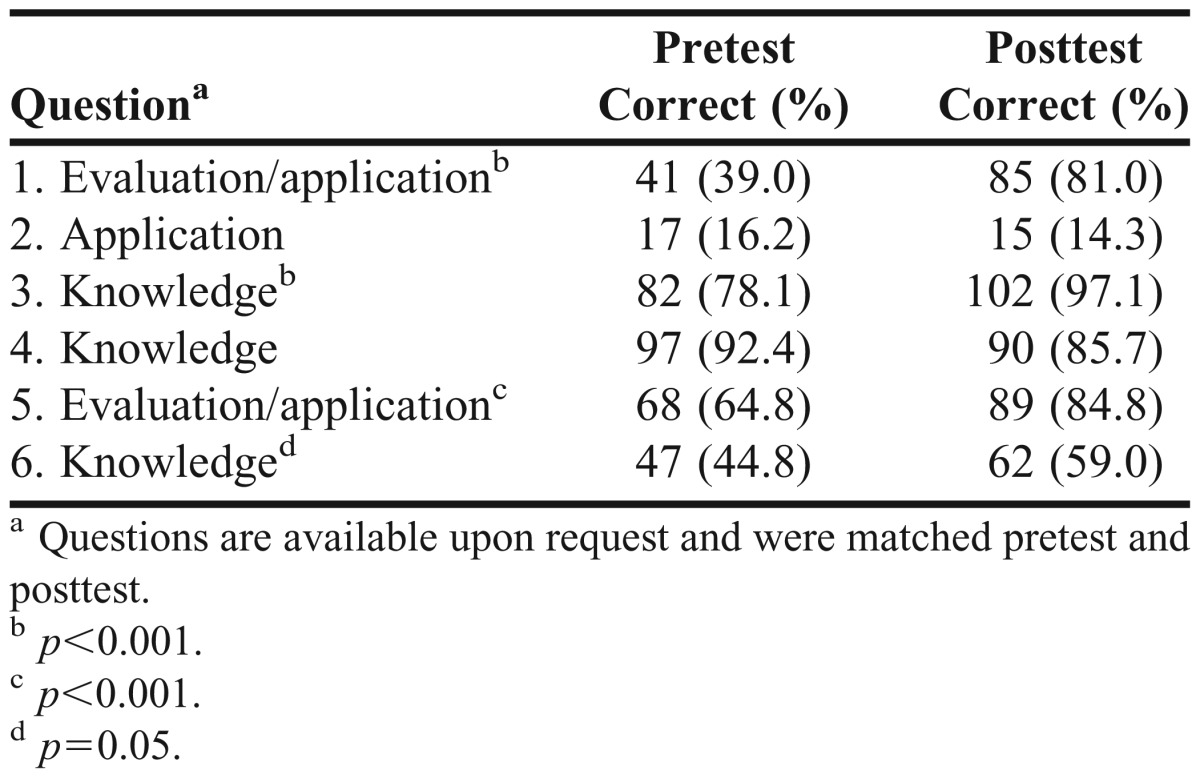
Table 3.
Comparison of Results for Higher-Level and Lower-Level Questions on Presimulation and Postsimulation Test Scores in an Advanced Therapeutics Pharmacy Course (N=315)
Following completion of the course, the students were sent a link to complete a satisfaction survey instrument related to the use of virtual patients as instructional tools in the classroom. The satisfaction survey was developed by the authors and included 5 questions based on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree) and 2 free-response questions (favorite aspect and how to improve the practicum session). At no point did results from the pretest, posttest, or satisfaction survey affect the students’ overall course grade. Students were mandated to complete all simulations and assessments during the practicum but could choose to withdraw assessment results from the research. The investigational review board at the University of Pittsburgh approved this study under an exempt status. Statistical analysis was completed using SPSS Statistics, version 21 (IBM, Armonk, NY). Pretest and posttest scores were analyzed as nominal data using chi-square tests. If the data did not meet criteria for chi-square analysis, the Fisher exact was used.
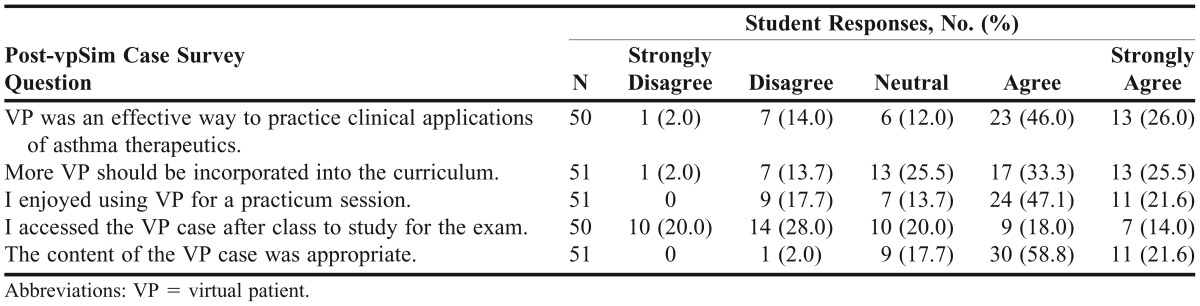
Fifty-one (47%) students completed the satisfaction survey instrument. Seventy-two percent of students agreed or strongly agreed that virtual patients were an effective way to practice clinical applications of asthma, 69% enjoyed using the simulation software, and 59% responded that virtual patient cases should be incorporated into the curriculum (Table 4). Thirty-two percent of students accessed the case to study for the examination.
Table 4.
Student Perceptions of Teaching Methodology That Included Virtual Patient Casework in an Advanced Therapeutics Pharmacy Course
DISCUSSION
Instructors of health professions curricula are challenged to develop innovative, active-learning strategies to graduate medication experts capable of providing patient-centered care through efficiency and effectiveness.1,2 Advances in educational technology have presented educators with a myriad of teaching and learning methods at their disposal to engage students in active learning through realistic, but safe, environments. These technologies can offer students “anytime-anywhere” learning accessibility, on-demand curricular content, and repetitive practice of course objectives.
Through the design, development, and curricular integration of complex, interactive virtual patient cases, instructors developed an innovative, active-learning environment while meeting specific curricular outcomes of the University of Pittsburgh, including critical thinking, development of knowledge and skills, patient assessment, pharmaceutical care plan development and decision making, and life-long learning. The complex cases within the simulation allowed the students to see patients’ disease progression and understand how to appropriately treat them. The virtual patient cases were targeted to higher-level learning as the focus of the cases was critical thinking through problem solving and clinical decision making. The simulations allowed the students to significantly improve upon higher-level learning outcomes, based around evaluation and application of knowledge. The new practicum session promoted active-learning by placing students in scenarios in which they were the healthcare provider making decisions based on patients’ needs. Each question posed to the students during the simulations was focused on patient care, patient counseling, and healthcare provider education. These tasks helped the students understand their roles as medication experts and gave them responsibility to their patients.
The overarching goal of this project was to provide students with a safe, high-fidelity environment to apply critical thinking, problem solving, and teamwork skills through complex clinical decision-making. This goal was realized through the incorporation of virtual patient technology into an advanced therapeutics pharmacy course. The virtual patient cases allowed the students to advance their knowledge and skills related to the management of asthma through practical application and repetition of course content, immediate patient outcomes from clinical decisions, and faculty feedback.
Our primary objective was to assess student satisfaction and learning of course objectives following the integration of this teaching strategy that was designed to promote active, patient-centered learning. Posttest scores were higher with almost every question compared to pretest scores. Scores significantly improved in both higher- and lower-level learning domains (p≤0.01). Additionally, median scores for the asthma portion of the examination were higher than the total median examination scores. Based on postcourse survey results, students enjoyed this teaching strategy, deemed it to be effective, and supported further curricular integration.
The use of virtual patients proved to be an effective strategy at improving higher-level learning among students. This can be attributed to the fact that pharmacy students, like most learners in higher education, are technologically savvy and feel that it enhances their learning.13 They are digital natives, thus more acclimated to learning in a technology-enhanced environment. In addition, active learning replaced passive learning with virtual patients and pharmacy students were provided unlimited repetition opportunities. For educators, the virtual patients allow for cost-effective, lifelike patient simulation scenarios that were easily sustainable. Cost-effectiveness can be realized through several venues including repetitive use of the technology and minimization of facilitators needed for larger class sizes.
Simulations are not without obstacles to implementation and curricular integration. We overcame cultural, process, and academic obstacles that can be experienced when implementing a new technology. Simulations require some resources, including funding for the programming and faculty time. We were fortunate to have access to a virtual patient platform; however, case development time was substantial, with approximately 50 hours dedicated to designing, developing, editing, and implementing the cases. The initial resource-intensive needs of virtual patient simulation are offset with future use, as updating and implementing cases for students is minimal. Therefore, virtual patient simulation is a sustainable resource that other health professions colleges and schools may be able to adopt.
An unexpected finding from our study showed that while students had the opportunity to practice skills outside of the classroom, few took advantage (32%). This study did not look at how virtual patients may change study habits; however, students seemed to be more comfortable using preformed study methods in preparing for the examination rather than the patient simulation.
This study had limitations. Faculty members must be able to use the program from both a design and student standpoint for it to be successful. Change in the students’ routine may be difficult, especially if technology that is included does not operate in a smooth, user-friendly fashion. Although we showed that students overall enjoyed this type of learning, our satisfaction survey instrument response rates were low at 47%. The low response rates were most likely because of the timing of the postcourse survey, which was sent to students during their final examinations week. Also, because of limited data availability, we were unable to compare test scores among students from previous years as a historical control (ie, conventional teaching methodology). Although we did report higher median scores for the asthma section relative to the entire examination, the objective of this study was not long-term retention of knowledge. We chose to limit our evaluation of the instructional tool to a 6 questions pretest and posttest. Six questions were chosen based on providing an equal distribution of higher- and lower-level questions and to fit within the time constraints of the course. Although our class size was large, more questions may have helped to delineate which domain in Bloom’s taxonomy that virtual patient technology improves. One other area to consider in future studies would be how virtual patient simulation may affect the comfort and/or performance of students on advanced pharmacy practice experiences, which may more accurately reflect the retention of the knowledge and skills gained through a virtual patient simulation.
SUMMARY
The incorporation of interactive, dynamic virtual patients into an advanced therapeutics pharmacy course at the University of Pittsburgh School of Pharmacy offered students opportunities for practical repetition of course content in a high-fidelity, safe environment, while promoting students to higher levels of learning. The technology allowed students to experience disease presentation and progression, patient counseling, and healthcare provider education as a team in a condensed active-learning environment. Through this simulation platform, the students were able to practice their assessment, treatment plans, decision making, and plan monitoring of asthma patients. Students thoroughly enjoyed the use of virtual patients and felt it to be an effective way to learn. Through virtual patient simulation, educators are granted a means to assess advanced student critical-thinking skills, while achieving the desired outcomes for the course. The ability of the virtual patient simulation teaching method to be easily updated and/or modified by case authors and its user-friendly interface should allow this technology to be employed at other institutions.
ACKNOWLEDGEMENTS
We gratefully acknowledge the support of the Laboratory for Educational Technology at the University of Pittsburgh.
REFERENCES
- 1.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education 2013 educational outcomes. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed August 2, 2013.
- 3.Accreditation Council for Pharmacy Education. Policies and procedures for ACPE accreditation pf professional degree programs. http://www.acpe-accredit.org/pdf/cs_policiesandprocedures.pdf. Accessed August 2, 2013.
- 4.Benedict NJ, Schonder K. Patient simulation software to augment an advanced pharmaceutics course. Am J Pharm Educ. 2011;75(2):Article 21. doi: 10.5688/ajpe75221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Monoghan MS, Cain JJ, Malone PM. Educational technology use among US colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(5):Article 87. doi: 10.5688/ajpe75587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.AAMC Institute for Improving Medical Education. Effective use of educational technology in medical education. Colloquium on educational technology: recommendations and guidelines for medical educators. March 2007; https://members.aamc.org/eweb/upload/Effective%20Use%20of%20Educational.pdf. Accessed August 12, 2013.
- 7.Orr KK. Integrating virtual patients into a self-care course. Am J Pharm Educ. 2007;71(2):Article 30. doi: 10.5688/aj710230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Triola M, Feldman H, Kalet AL. A randomized trial of teaching clinical skills using virtual and live standardized patients. J Gen Intern Med. 2006;21(5):424–429. doi: 10.1111/j.1525-1497.2006.00421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook D, Triola M. Virtual patients: a critical literature review and proposed next steps. Med Educ. 2009;43(4):303–311. doi: 10.1111/j.1365-2923.2008.03286.x. [DOI] [PubMed] [Google Scholar]
- 10.Tworek J, Coderre S, Wright B, McLaughlin K. Virtual patients: ED-2 Band-Aid or valuable asset in the learning portfolio? Acad Med. 2010;85(1):155–158. doi: 10.1097/ACM.0b013e3181c4f8bf. [DOI] [PubMed] [Google Scholar]
- 11.Greenberg AD. Wainhouse Research White Paper: Blended learning technology: navigating the challenges of large scale adoption. Wainhouse Research; 2012. http://echo360.com/sites/default/files/Adoption%20White%20Paper.pdf. Accessed July 29, 2014.
- 12.Bloom BS. Taxonomy of Educational Objectives. Boston, MA: Allyn and Bacon; 1984. [Google Scholar]
- 13.DiVall MV, Hayney MS, Marsh W, et al. Perceptions of pharmacy students, faculty members, and administrators on the use of technology in the classroom. Am J Pharm Educ. 2013;77(4):Article 75. doi: 10.5688/ajpe77475. [DOI] [PMC free article] [PubMed] [Google Scholar]