Abstract
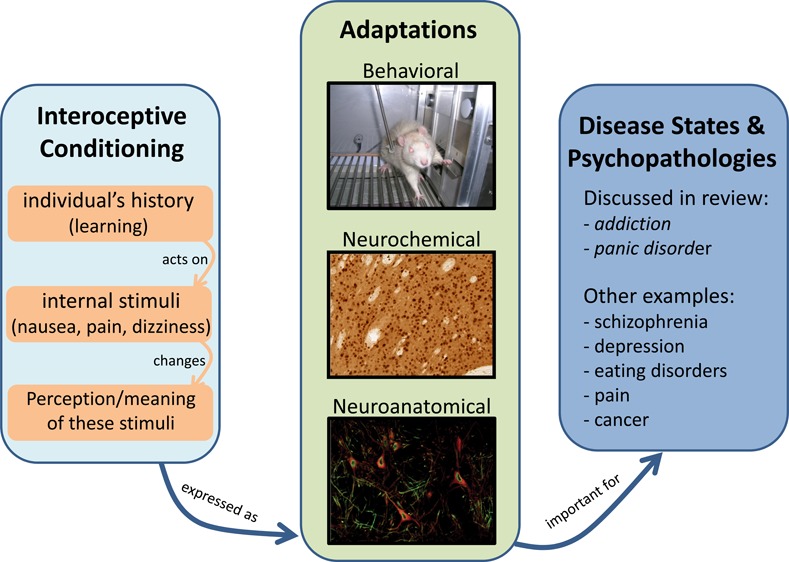
Chemotherapeutic agents nauseate cancer patients. Some individuals with schizophrenia hear voices. Chronic pain can be reduced by analgesics. Nausea, voices, and pain are examples of internal (interoceptive) stimuli closely linked with a disease and/or its treatment. There is evidence that the perception and, hence, role of these internal stimuli can be modified by one’s learning history. There is also increased awareness by researchers and practitioners of the potential import of learning involving internal states to some diseases and psychopathologies. Unfortunately, the science, theory, and practice appear to be trailing behind awareness. In this mini-review, we describe two examples: smoking and panic disorder. While doing so, we discuss the need to develop translationally relevant animal models that will allow investigators to better understand the behavioral and neural mechanisms underlying interoception and learning.
Keywords: Interoceptive conditioning, smoking, nicotine, panic-disorder, psychopathologies, neuropathologies, drug abuse
Pavlov,1 in his seminal work Conditioned Reflexes: An Investigation of the Physiological Activity of the Cerebral Cortex, described how an environmental event (termed conditioned stimulus) can come to acquire control over a behavior that the stimulus previously had not controlled. Specifically, using dogs prepared with a fistula to collect saliva, a dog would be given repeated presentation of an external stimulus such as operation of a metronome, tone, light, or buzzer followed by the availability of food (termed unconditioned stimulus). At the outset, food produced salivation, but presentation of the buzzer does not. Repeated pairing of the buzzer with food eventually led the buzzer to acquire control over salivation. Pavlov1,2 used this powerful model of learning that we now refer to as classical or Pavlovian conditioning to gain insight into the functioning of the nervous system and how it produces complex behaviors, adaptive and maladaptive. Notably, Pavlov did not limit this theorizing to events outside the animal (external or exteroceptive). As a physiologist, he gave great import to the internal environment of the animal. For example, he spent much time researching and writing about short-term and long-term perturbations in the internal environment that may influence conditioning (e.g., illness, sleep deprivation, hunger, drugs, stress, etc.). He further speculated that such internal or interoceptive events contribute to pathologies.1,2
A modern, important, and well-reasoned extension of this theorizing can be found in the work of Paulus and colleagues, in which they argue that interoception is fundamentally involved in hedonic and incentive motivational processes.3 To this end, one can consider that a misinterpretation of an individual’s internal state or dysregulation in interoception processing can contribute to maladaptive behaviors. Accordingly, Paulus and colleagues have posited that populations with depression, anxiety, and drug addiction have altered interoceptive processing.3−6 Additionally, this group provides an empirically based neuroanatomical framework by which to explain how an individual’s internal state can impact motivated behavior. The insular cortex is a central component of this neuroanatomical framework as this brain region plays an important role in the processing of interoception-related information (see refs (7) and (8) for reviews). Further, functional and connectivity neuroimaging studies have led to the identification of subdivisions of the insular cortex: the anterior portion of the insula shows connectivity with frontal, cingulate, parietal, and cerebellar brain regions; the posterior portion of the insula shows connectivity with sensorimotor, temporal, and posterior cingulate brain regions.9−11 Therefore, the anterior insular cortex is hypothesized to modulate awareness of the internal state and has been implicated in integrating emotional salience into motivated behavior. In contrast, the posterior portion is hypothesized to be involved in detecting changes in the internal state (see refs (7), (8), and (11)). In line with Paulus and colleagues’ neuroanatomical framework are the findings from neuroimaging studies that show altered insula response in populations with dysfunction in interoception processing such as those with depression, anxiety and drug addiction (as reviewed by Paulus and colleagues in refs (3), (4), and (6)), lending further support for the importance and integration of internal states in maladaptive behavior.
Along with the internal milieu affecting acquisition and expression of conditioning, Pavlov thought that these internal events were also available to be modified by learning and hence contribute to adaptive and maladaptive behaviors. For example, in the 1927 translation of his book Conditioned Reflexes, Pavlov defined conditioned stimuli as follows:
“...I shall suggest the following modification and amplification of our definition of agencies which can become conditioned, viz. that innumerable individual fluctuations in the external and internal environment of the organism may, each and all of them, singly or collectively, being reflected in definite changes in the cells of the cerebral cortex, acquire the properties of a conditioned stimulus.” (p 43, italics added for emphasis)
The research initially prompted by this theorizing used internal stimuli such as irrigation of fluid into the stomach or electrical stimulation of the brain (see, e.g., refs (12) and (13)). For example, Bykov12 reported a study by Vassilevskaya (p. 252–253) in which a dog had irrigation of 0.2% hydrochloric acid into the stomach (i.e., the internal conditioned stimulus) paired with a mild electric shock to a hind paw. The interoceptive stimulus of acid in the stomach came to control withdrawal of the paw. This conditioned withdrawal response was specific to the acid, as irrigation of water did not evoke paw withdrawal.
The focus of this mini-review is on internal stimuli functioning as conditioned stimuli. Despite the early interest in interoceptive conditioning and the theoretical speculations of its import, programmatic research on the contribution of interoceptive conditioning to health issues has been mixed at best. Albeit mixed, there is at least some evidence that interoceptive conditioning may be involved in such health issues as treatment of cancer,14 cardiovascular disease,15 chronic pain,16 schizophrenia,17 depression,4 eating disorders,18,19 drug addiction,20,21 and panic disorder.22,23 One goal of this mini-review is to highlight the potential importance of interoceptive conditioning processes using two examples, smoking and panic disorder.
These two examples were selected for several reasons. First, there is recent research identifying the potential import of interoceptive conditioning to the development and/or treatment of the pathology. Second, there has been recent work to develop animal models to study the interoceptive events and their modification through learning processes. Finally, there have been recent efforts to delineate the neural mechanisms. In highlighting the role of interoceptive conditioning to smoking and panic disorders, a second goal of this mini-review is to encourage the reader to reflect on their research area and potentially related neuropathologies or disease and ask the question: “What are the internal stimuli likely experienced by the population of interest and are those stimuli available to be modified by experience?” We hope by generating reflection and discussion of this important area of research that further scientific advances will be made as investigators better leverage current animal models, as well as creatively improve these models and develop new animal models to study the neural underpinnings of interoceptive conditioning.
Smoking
As a demonstration, consider the following hypothetical, but not unlikely, example from Jill, a 32 year old smoker that quit 5 days earlier (Box 1).
Box 1.
At a party, an open pack of cigarettes sits on the counter by the ashtray. Jill picks up the pack, taps a cigarette out, and places it between her lips. She turns to her friend Jack and asks for a light. He does so. Jill takes a long draw from the cigarette. The smoke mildly irritates her throat as she pulls it deep into her lungs. A little short of breath, Jill feels a little excited and jittery; like the first cigarette of the day, only more intense. As she finishes the cigarette, a mental fog that has bothered her all week seems to lift. Looking around the room, Jill notes that the party seems to be becoming more enjoyable as she catches herself laughing along with the others.
This seemingly simple scenario is rich with stimuli. Some of the smoking-related cues that have their origin in the external environment (recall the buzzer used by Pavlov1) include the sight of the cigarette and cigarette pack, the ashtray, the smell of the unlit and then lit tobacco, the sight of the smoke, the lighter, Jill’s smoking friends, and so forth. Learning and memory involving these exteroceptive stimuli play an important role in theories of drug addiction in general, and in chronic tobacco use and nicotine dependence specifically (e.g., refs (24−26)). Briefly, many of these exteroceptive stimuli reliably co-occur with the neuropharmacological effects of nicotine and other constituents of tobacco (cf. to food or the unconditioned stimulus in Pavlov’s studies) that contribute to its abuse liability. Across repeating pairings, these exteroceptive stimuli enter into conditioned (learned) associations with these pharmacological effects. This modification through experience results in the exteroceptive stimuli controlling behavioral and neural responses related to drug-seeking, drug-taking, and propensity to relapse.
Notably, there are many internal or interoceptive stimuli in this scenario that are at least as important as the exteroceptive stimuli. Some of the smoking-related interoceptive stimuli include the neuropharmacological effects of nicotine and other active constituents of tobacco, shortness of breath, excited jittery feeling, mental fog, depressed or anhedonic mood, and so forth. As with exteroceptive stimuli, learning involving interoceptive stimuli likely contributes to the development of chronic tobacco use and nicotine dependence, as well as the high relapse rate.27,28 For example, nicotine generates a perceptible and distinct interoceptive stimulus that can acquire control over behavior. In human laboratory studies, participants readily discriminate when intranasal spray contains nicotine or not.29 Participant’s sensitivity to dose was also demonstrated in this study. To do so, the men and women were asked to place a set of poker chips in a placebo or nicotine pile with 25 cents available for each “correctly” placed chip. As the dose of nicotine in the spray decreased, the number of chips in the nicotine pile correspondingly decreased. In a smoker’s environment, this nicotine stimulus co-occurs with many potential reinforcing events (e.g., work breaks, peer acceptance, social interactions, alcohol, etc.). Theories of learning and memory predict that this co-occurrence should alter the behaviors controlled by nicotine and enhance its abuse liability.
Preclinical animal models have confirmed some of these predictions. The discriminated goal-tracking task is one such model used to study interoceptive conditioning with drug stimuli. In one variant of the task, rats receive daily nicotine sessions intermixed with daily saline sessions. On nicotine sessions, there is intermittent access to liquid sucrose. For saline sessions, sucrose is withheld. The nicotine stimulus comes to control anticipatory sucrose-seeking behavior expressed as an increase in the rate of head entries into a dipper receptacle where sucrose has been available in the past.27,30 A recent experiment using a behavioral procedure referred to as reinforcer devaluation provides some of the best evidence to date that presentation of the nicotine stimulus after training activates neurobiological processes related to the sucrose reward.31 In that study, rats were first trained to discriminate nicotine from saline as previously described. Then, sucrose was devalued by repeatedly pairing 15 min access to sucrose in the home cage with illness induced by lithium chloride (LiCl) injections. After three separate daily pairings of sucrose with LiCl, consumption of the sucrose was significantly reduced relative to control values (i.e., conditioned taste aversion32). A subsequent test of the nicotine stimulus revealed that sucrose-seeking was reduced relative to a control that had comparable exposure to LiCl. That control group eliminates an account of decreased responding to the nicotine stimulus based on a nonspecific effect of illness decreasing sucrose-seeking behavior. Thus, the nicotine stimulus appears to activate a neural representation of past associated reward (i.e., sucrose). The sucrose, now associated with illness, has reduced appetitive value and the rat avoids the dipper receptacle even though the nicotine stimulus never co-occurred with LiCl-induced illness. Clearly, learning and memory processes can modulate the behavior controlled by interoceptive stimuli, nicotine in this case.
Some of the neuropharmacological processes involved in interoceptive conditioning with the nicotine stimulus are known. For example, nicotine-evoked responding in the discriminated goal-tracking task is blocked by systemic administration of the central and peripheral nicotinic acetylcholine receptor (nAChR) antagonist mecamylamine; the mostly peripheral nAChR antagonist hexamethonium has no effect.30,33 This outcome indicates the relative import of nAChRs in the central nervous system. Pretreatment with ABT-418, an α4β2-containing nAChR agonist,34 prompts a full “nicotine-like” response in tests designed to briefly assess the similarity between ligands’ interoceptive stimulus effects.35 The smoking cessation aid varenicline (Chantix or Champix), a partial agonist for α4β2-containing nAChRs and an agonist for the α7 nAChRs,36 also prompts nicotine-like responding in these stimulus substitution tests.35 Similarly, pretreatment with the α4β2 antagonist dihydro-β-erythroidine (DHβE37) blocks the sucrose-seeking response controlled by the nicotine stimulus.33 In contrast, the α7 antagonist methyllycaconitine (MLA37) has no effect on responding evoked by the nicotine stimulus.33 In ligand substitution tests, the α7 agonist PHA-54361338 does not evoke sucrose-seeking behavior above placebo controls (unpublished data). Overall, this pattern of findings suggests that α4β2-containing, and not the α7 nAChRs, are important in generating the stimulus effects of nicotine that control acquired appetitive behavior. We refer the reader to Wooters and colleagues39 for more information regarding the nicotine stimulus and the role of other neurotransmitter systems. Also, research investigating the neuroanatomical substrates has just begun. Early indications suggest an important role for the dorsal striatum,40 an area thought to be important for habit learning.41 Although c-Fos activation in the insula was not quantified or reported in that initial publication,40 later examination of brain sections that contained a portion of the posterior insula reveal very little c-Fos activation and was, hence, not quantified. Given the relative import placed on the insula by some theories for the processing of interoception-related information (refs (7) and (8); see the introduction above), future research will need to more programmatically investigate this area.
Note that the above discussion was limited to learning that involved the nicotine stimulus. What about the other interoceptive stimuli mentioned earlier, for example, excited jittery feeling, mental fog, depressed or anhedonic mood? There are animal models available to study some of these internal stimuli. Take as an example deficits in cognition, learning, and memory related to withdrawal from nicotine (i.e., “mental fog” in our story with Jill). Such deficits are considered to be important for relapse back to tobacco use.42,43 There are also a number of animal models available to study different psychological or behavioral constructs such as attention and memory that are thought to be important. The five-choice serial reaction time task (5-CSRTT) has been used to study attentional processes.44,45 A variety of mazes (radial arm-maze, Morris water maze, elevated plus maze) and Pavlovian fear conditioning have been used to study learning and memory processes (e.g., refs (46) and (47)). Hopefully, the discussion to this point has the reader wondering whether the nature of cognitive deficits varies depending on an individual’s past experiences involving the mental fog. Presumably, the extent of experiencing work errors, reprimands from a boss, and so forth can alter the subsequent nicotine withdrawal-induced cognitive deficit stimulus and the behavior this complex interoceptive stimulus controls. The seemingly obvious consequence of an extensive punishment history while in a mental fog would be acquired avoidance behaviors of the interoceptive stimulus. Avoidance would translate into reduced quit attempts and greater likelihood of relapse evoked by the mental fog.
One future challenge for the preclinical investigator is to adapt current animal models, or develop new models, to study such malleability in a way that has good validity for the construct(s) of interest.48 Once such models are developed and refined, another challenge will be to understand the behavioral, neurochemical, and neuroanatomical processes underlying such interoceptive conditioning. This understanding could then be leveraged to develop better therapeutic interventions to enhance quit attempts and decrease relapse rates. Within the example of cognitive deficits during smoking cessation, clinical researchers have examined whether so-called procognitive or vigilance promoting drugs impact success rates. For example, modafinil (Provigil) is prescribed in the United States for the treatment of narcolepsy and excessive sleepiness during waking hours. Modafinil has widespread central nervous system effects. Its therapeutic effects for narcolepsy have been attributed to orexin receptors in hypothalamic areas,49 as well as action at serotonin (5-HT) and adrenoceptors.50,51 Additionally, modafinil binds weakly to the dopamine transporter52 which might account for its ability to increase dopamine in the nucleus accumbens.53 Glutamatergic and GABAergic processes have also been implicated in these effects of modafinil.53,54 In clinical trials with smokers seeking treatment, modafinil did not increase quit rates.55,56 In fact, the early placebo-controlled study had to be stopped as modafinil-treated participants that had relapsed (i.e., nonabstinent individuals) were smoking more each day than nonabstinent placebo controls; modafinil also increased reported symptoms of withdrawal and negative mood.56
The negative outcome of these smoking cessation studies with modafinil does not necessarily indicate that cognitive deficits are unimportant. The convergent evidence suggests quite the contrary (see ref (42) for a recent review). For us, this example suggests that a deeper understanding of the nature of the multifaceted interoceptive stimulus that the field categorizes as cognitive deficits is needed. That is, what the field calls “cognitive deficits” must be deconstructed into what are believed to be its component constructs. Does it include short-term memory, spatial memory, working memory, and so forth? Even these constructs can be further broken down. Once operationalized, the task is to ask if it is possible that experience could affect any or all of the elements of the internal state of interest and then design studies to test this possibility. This discussion, of course, applies to the many other likely interoceptive stimuli contributing to tobacco use and nicotine dependence, as well as to other psychopathologies and disease states.
Panic Disorder
In contrast to smoking, the field of panic disorders has explicitly incorporated the notion of interoceptive conditioning into its conceptual framework, as well as in treatment approaches. A key feature of panic disorder is the experience of recurrent panic attacks that can occur at any time. During a panic attack, an individual such as the hypothetical Walter in the following vignette (Box 2) may experience an array of physical symptoms.
Box 2.
Walter experienced his first panic attack in his early 20s. He was waiting to get off a crowded airplane after a long flight. As Walter was standing in the crowd, he felt the plane getting hot and stuffy and his heart started pounding. Shortness of breath and dizziness overcame Walter as his fingers started to tingle. He was terrified and thought he was having a heart attack. Emergency personnel rushed onto the plane. Later, at the hospital, the doctor told Walter he had not had heart attack and they could find nothing wrong. After this episode, Walter was panic-free for a of couple years until at a job interview at a prestigious company, when he became aware of his heart beating rapidly. Suddenly, his heart began pounding, he became lightheaded, and the room started to spin while he gasped for air. Since then, Walter has had several other panic attacks and is now preoccupied about having another attack and lives in fear of when the next one will occur. He is worried that these symptoms mean that his heart is weak and that he will die of a heart attack. Once athletic and fit, Walter now avoids exercising so that his heart will not beat too fast, setting off another panic attack that will then lead to a heart attack.
Clearly, the array of interoceptive stimuli in this example is quite salient and pronounced. However, experiencing a panic attack (as initially experienced by Walter on the airplane) does not necessarily mean that one will develop panic disorder. Approximately 23% of the general population has had a panic attack, whereas the prevalence of panic disorder is 3–4%.57,58 What is notable from our perspective, though, is that interoceptive conditioning appears to play an important role in the development of panic disorder (for a review, see ref (22)). For example, the interoceptive/somatic arousal (e.g., pounding heart, shortness of breath) experienced upon swerving your car to miss a herd of deer crossing the road and ending stranded in the ditch is similar to that experienced during a panic attack. This reaction is appropriate to a real threat (e.g., “fight or flight” response). In individuals that develop panic disorder, learning regarding some of the internal stimuli becomes maladaptive. From an interoceptive conditioning perspective, the “early” symptoms of panic (e.g., slight increase in heart rate as Walter experienced during his job interview) are associated with the full-blown panic attack (e.g., racing/pounding heart, shortness of breath). The maladaptive malleability of these internal stimuli is subsequently revealed when these previously innocuous early interoceptive stimuli can now evoke a full-blown panic attack in the absence of a threat. For the purposes of this mini-review, we are focusing on interoceptive cues and how learning may change their meaning. Like smoking, exteroceptive stimuli such as speaking in front of an audience or being in a small crowded space (e.g., movie theater or airplane) are clearly important.
In human laboratory studies, inhalation of a high dose of CO2-enriched air has been used to induce somatic arousal that mimics a panic attack and consequently is used as a reliable laboratory model of panic attacks.59−62 In support of an interoceptive conditioning account, in a nonclinical population, low-level somatic arousal (brief exposure to CO2-enriched air; physiologically inert) served as an internal stimulus for a longer exposure to the same concentration of CO2-enriched air; this longer exposure is a physiologically potent panicogenic internal stimulus. After repeated pairings, the presentation of the brief CO2 stimulus evoked a significant increase in reported fear and distress, as well as electrodermal response relative to controls that were exposed only to the same brief CO2 exposure, but not the longer panicogenic CO2 exposure.63 These and other findings,64−67 establish the feasibility of interoceptive conditioning in panic disorder, where mild somatic changes (i.e., the conditional stimulus) come to be associated with a larger somatic change. Interestingly, patients with panic disorder appear to be hypersensitive to the effects of CO2 at concentrations that do not induce panic in controls.68 This enhancement presumably reflects an interoceptive learning history that differs from control participants.
Researchers have utilized preclinical animal models to evaluate components of panic disorder. For example, anxiety is a key symptom and anti-anxiety medications and potential novel targets have been evaluated for efficacy in reducing anxiety-like behavior in various animal models (see ref (69) for a review). Utilization of conditioned fear models has also allowed for the investigation of pharmacological targets. These fear conditioning studies have further contributed to our understanding of the neurobiology of the fear circuitry that may have implications for understanding panic disorder.70−73 Basic research has also focused on the interoceptive panic-like somatic changes that accompany panic attacks. For example, preclinical work utilizing brain region-specific electrical stimulation or pharmacological manipulation has been able to induce panic-like somatic responses (as well as behavioral panic-like responses, e.g., escape behaviors). Accordingly, this has led to the hypothesis that dysregulation in panic-related brain circuitry/regions (i.e., implicated in modulating normal panic responses), such as the hypothalamus, amygdala, periaqueductal gray, and frontal cortex, may contribute to the generation of panic disorder (see ref (74)). Future work could examine whether maladaptive changes in these panic-related brain circuits emerge as a consequence of interoceptive conditioning, especially during differing stages of conditioning (e.g., early vs late). Together, such work may provide insight into neurobiological adaptations allowing for identification of novel molecular targets for preclinical and clinical research to pursue.
Along this line of inquiry, recall that patients with panic disorder show increased sensitivity to CO2-enriched air. These individuals also exhibit increased sensitivity to sodium lactate.75−78 Accordingly, in a rodent model designed to mimic the increased somatic response to sodium lactate, rats receive infusion of a γ-Aminobutyric acid (GABA) synthesis inhibitor (l-allylglycine; l-AG) into the dorsomedial hypothalamus for several days to disrupt inhibitory GABAergic activity (cf. ref (74)). This low dose of l-AG infusion alone does not induce panic-like responses. However, upon a sodium lactate infusion, these rats show robust panic-like responses (i.e., increased heart rate, respiratory rate) in addition to increased anxiety-like behaviors relative to controls. Using these panic-prone rats, several receptor targets including GABA, N-methyl-d-aspartate (NMDA), metabotropic glutamate 2/3 (mGlu2/3), and orexin-1 have been identified as playing a functional role in modulating the increased sensitivity to the somatic and anxiety-producing effects of sodium lactate.79−82
Presently, treatment for panic disorder includes cognitive-behavioral therapy and/or medications for the treatment of panic disorder which include anti-anxiety medications and antidepressants. Several meta-analyses have shown these therapies and medications to be effective for the reduction of panic symptoms and anxiety.83−85 The implication of interoceptive conditioning in the etiology of panic disorder would point to the importance of cue-exposure therapies that include exteroceptive and interoceptive stimuli. Indeed, some intervention strategies utilize exposure therapy and such techniques commonly incorporate repeated exposure to arousal-inducing activities (e.g., hyperventilation, running on the spot, chair spinning, breathing through a straw) as a method by which to reduce the ability of such interoceptive stimuli to induce a full-blown panic attack.86 As would be predicted from an interoceptive conditioning perspective, individuals with panic disorder tend to exhibit larger responses to such standard interoceptive stimulus exposure exercises.87
These interoceptive exposure exercises likely do not replicate the entire panic experience.86−88 That is, in the therapeutic environment, the physiologically potent panicogenic internal stimulus that typically follows the early interoceptive stimuli is either blunted or absent. Fundamental principles of learning predict that the acquired reaction to the early internal stimuli will be reduced upon repeated presentation without the reinforcer (i.e., the full-blown panic attack). This appears to be case for some individuals and has led to the suggestion that the controlled internal stimulus induced by CO2 exposure may be an important addition to exposure therapy.64 Future research further refining our understanding of the prepotent internal stimuli, as well as behavioral and biological factors that predispose individuals to develop panic disorder will be of import. The current preclinical animal models, some briefly discussed here, have provided key insights into likely behavioral, neurobiological, and neurochemical mechanisms. Further development of these animal models with better construct validity (e.g., more closely simulating interoceptive conditioning experiences) is needed. For example, could the model with the panic-prone rats79−82 be adapted such that environmental consequence reliably followed induction of the anxiety? That is, will the extent of the anxiety and its underlying neurobiological processes change depending on the nature of the consequence (i.e., appetitive vs aversive). With new models, the field will be able to better translate scientific advances to better treatment outcomes (cf. refs (89) and (90)).
In Closing
Pavlov1,2 wrote nearly 90 years ago on interoceptive conditioning and its potential contribution to neuropathologies seen in humans. Programmatic research on how experience can change the relevance or meaning of internal states and how this change contributes to adaptive and maladaptive behavior has been mixed since the seminal work of Pavlov. Notably, awareness by researchers and practitioners regarding the likely importance of learning involving internal states to some diseases and psychopathologies has increased in recent years. The time is here for research and theory to catch up with this awareness. The research that has been done indicates the potential import of interoceptive conditioning to such health issues as treatment of cancer,14 cardiovascular disease,15 chronic pain,16 schizophrenia,17 impaired cognition in aging,91 depression,4 eating disorders,18,19 obesity,3 as well as smoking/drug addiction20,21 and panic disorder22,23 discussed in this mini-review. For these, and countless other diseases and psychopathologies, much is still unknown regarding the nature of the interoceptive stimuli and how experience may change the perception and meaning of these stimuli for individuals. With continued advancement in the methodological and conceptual tools available to researchers, we will better understand the import of learning involving internal stimuli, as well as the underlying behavioral, neurochemical, and neuroanatomical adaptations. Our hope and belief is that such advancement will lead to new therapeutic approaches that will reduce the personal suffering and fiscal cost of such diseases and psychopathologies.
R.A.B. was partially supported by USPHS Grant DA034389 and J.B. was partially supported by AA019682, AA020914, and the Center for Alcohol Studies while writing this manuscript.
The authors declare no competing financial interest.
References
- Pavlov I. P. (1927) Conditioned reflexes; an investigation of the physiological activity of the cerebral cortex, Oxford University Press, Humphrey Milford, London. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlov I. (1941) Conditioned reflexes and psychiatry. In Lectures on conditioned reflexes, International Publishers, New York. [Google Scholar]
- Paulus M. P.; Tapert S. F.; Schulteis G. (2009) The role of interoception and alliesthesia in addiction. Pharmacol., Biochem. Behav. 94, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus M. P.; Stein M. B. (2010) Interoception in anxiety and depression. Brain Struct. Funct. 214, 451–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus M. P. (2007) Neural basis of reward and craving—A homeostatic point of view. Dialogues Clin. Neurosci. 9, 379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus M. P.; Stewart J. L. (2014) Interoception and drug addiction. Neuropharmacology 76(Pt B), 342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig A. D. (2002) How do you feel? Interoception: the sense of the physiological condition of the body. Nat. Rev. Neurosci 3, 655–666. [DOI] [PubMed] [Google Scholar]
- Craig A. D. (2009) How do you feel—now? The anterior insula and human awareness. Nat. Rev. Neurosci. 10, 59–70. [DOI] [PubMed] [Google Scholar]
- Deen B.; Pitskel N. B.; Pelphrey K. A. (2011) Three systems of insular functional connectivity identified with cluster analysis. Cereb. Cortex 21, 1498–1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauda F.; D’Agata F.; Sacco K.; Duca S.; Geminiani G.; Vercelli A. (2011) Functional connectivity of the insula in the resting brain. NeuroImage 55, 8–23. [DOI] [PubMed] [Google Scholar]
- Cloutman L. L.; Binney R. J.; Drakesmith M.; Parker G. J.; Lambon Ralph M. A. (2012) The variation of function across the human insula mirrors its patterns of structural connectivity: evidence from in vivo probabilistic tractography. NeuroImage 59, 3514–3521. [DOI] [PubMed] [Google Scholar]
- Bykov K. M. (1957) The cerebral cortex and the internal organs, Chemical Publishing Co., New York. [Google Scholar]
- Doty R. W. (1961) Conditioned reflexes formed and evoked by brain stimulation. In Electrical stimulation of the brain: An interdisciplinary survey of neurobehavioral integrative systems (Sheer D. E., Ed.), pp 397–412, University of Texas Press, Austin, TX. [Google Scholar]
- Meagher M. W. (2010) Developing translational animal models of cancer-related fatigue. In Cancer Symptom Science: Measurement, Mechanisms, and Management (Cleeland C., Fisch M., and Dunn A., Eds.), pp 124–141, Cambridge University Press, Cambridge. [Google Scholar]
- Koroboki E.; Zakopoulos N.; Manios E.; Rotas V.; Papadimitriou G.; Papageorgiou C. (2010) Interoceptive awareness in essential hypertension. Int. J. Psychophysiol. 78, 158–162. [DOI] [PubMed] [Google Scholar]
- De Peuter S.; Van Diest I.; Vansteenwegen D.; Van den Bergh O.; Vlaeyen J. W. (2011) Understanding fear of pain in chronic pain: Interoceptive fear conditioning as a novel approach. Eur. J. Pain 15, 889–894. [DOI] [PubMed] [Google Scholar]
- Wylie K. P.; Tregellas J. R. (2010) The role of the insula in schizophrenia. Schizophr. Res. 123, 93–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson T. L. (1993) The nature and function of interoceptive signals to feed: toward integration of physiological and learning perspectives. Psychol. Rev. 100, 640–657. [DOI] [PubMed] [Google Scholar]
- Oldershaw A.; Hambrook D.; Stahl D.; Tchanturia K.; Treasure J.; Schmidt U. (2011) The socio-emotional processing stream in anorexia nervosa. Neurosci. Biobehav. Rev. 35, 970–988. [DOI] [PubMed] [Google Scholar]
- Bevins R. A., and Murray J. E. (2011) Internal stimuli generated by abused substances: Role of Pavlovian conditioning and its implications for drug addiction. In Associative Learning and Conditioning: Human and Non-Human Applications (Schachtman T. R., and Reilly S., Eds.), pp 270–289, Oxford University Press, New York. [Google Scholar]
- Wise R. A.; Wang B.; You Z. B. (2008) Cocaine serves as a peripheral interoceptive conditioned stimulus for central glutamate and dopamine release. PLoS One 3, e2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouton M. E.; Mineka S.; Barlow D. H. (2001) A modern learning theory perspective on the etiology of panic disorder. Psychol. Rev. 108, 4–32. [DOI] [PubMed] [Google Scholar]
- Deacon B. J.; Lickel J. J.; Farrell N. R.; Kemp J. J.; Hipol L. J. (2013) Therapist perceptions and delivery of interoceptive exposure for panic disorder. J. Anxiety Disord. 27, 259–264. [DOI] [PubMed] [Google Scholar]
- Franklin T.; Wang Z.; Suh J. J.; Hazan R.; Cruz J.; Li Y.; Goldman M.; Detre J. A.; O’Brien C. P.; Childress A. R. (2011) Effects of varenicline on smoking cue-triggered neural and craving responses. Arch. Gen. Psychiatry 68, 516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose J. E. (1996) Nicotine addiction and treatment. Annu. Rev. Med. 47, 493–507. [DOI] [PubMed] [Google Scholar]
- Tiffany S. T., Warthen M. W., and Goedeker K. C. (2009) The functional significance of craving in nicotine dependence. In The motivational impact of nicotine and its role in tobacco use (Bevins R. A. and Caggiula A. R., Eds.), Nebraska Symposium on Motivation Vol. 55, pp 171–197, Springer, New York. [DOI] [PubMed] [Google Scholar]
- Bevins R. A. (2009) Altering the motivational function of nicotine through conditioning processes. In The motivational impact of nicotine and its role in tobacco use (Bevins R. A. and Caggiula A. R., Eds.), Nebraska Symposium on Motivation Vol. 55, pp 111–129, Springer, New York. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevins R. A.; Palmatier M. I. (2004) Extending the role of associative learning processes in nicotine addiction. Behav. Cognit. Neurosci. Rev. 3, 143–158. [DOI] [PubMed] [Google Scholar]
- Perkins K. A. (1999) Nicotine discrimination in men and women. Pharmacol., Biochem. Behav. 64, 295–299. [DOI] [PubMed] [Google Scholar]
- Besheer J.; Palmatier M. I.; Metschke D. M.; Bevins R. A. (2004) Nicotine as a signal for the presence or absence of sucrose reward: A Pavlovian drug appetitive conditioning preparation in rats. Psychopharmacology (Berlin, Ger.) 172, 108–117. [DOI] [PubMed] [Google Scholar]
- Pittenger S. T.; Bevins R. A. (2013) Interoceptive conditioning with a nicotine stimulus is susceptible to reinforcer devaluation. Behav. Neurosci. 127, 465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A. L.; Baril L. L. (1976) Conditioned Taste Aversions - Bibliography. Anim. Learn. Behav. 4, S1–S13. [Google Scholar]
- Struthers A. M.; Wilkinson J. L.; Dwoskin L. P.; Crooks P. A.; Bevins R. A. (2009) Mecamylamine, dihydro-beta-erythroidine, and dextromethorphan block conditioned responding evoked by the conditional stimulus effects of nicotine. Pharmacol., Biochem. Behav. 94, 319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holladay M. W.; Dart M. J.; Lynch J. K. (1997) Neuronal nicotinic acetylcholine receptors as targets for drug discovery. J. Med. Chem. 40, 4169–4194. [DOI] [PubMed] [Google Scholar]
- Reichel C. M.; Murray J. E.; Barr J. D.; Bevins R. A. (2010) Extinction with varenicline and nornicotine, but not ABT-418, weakens conditioned responding evoked by the interoceptive stimulus effects of nicotine. Neuropharmacology 58, 1237–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihalak K. B.; Carroll F. I.; Luetje C. W. (2006) Varenicline is a partial agonist at alpha4beta2 and a full agonist at alpha7 neuronal nicotinic receptors. Mol. Pharmacol. 70, 801–805. [DOI] [PubMed] [Google Scholar]
- Dwoskin L. P.; Crooks P. A. (2001) Competitive neuronal nicotinic receptor antagonists: a new direction for drug discovery. J. Pharmacol. Exp. Ther. 298, 395–402. [PubMed] [Google Scholar]
- Wishka D. G.; Walker D. P.; Yates K. M.; Reitz S. C.; Jia S.; Myers J. K.; Olson K. L.; Jacobsen E. J.; Wolfe M. L.; Groppi V. E.; Hanchar A. J.; Thornburgh B. A.; Cortes-Burgos L. A.; Wong E. H.; Staton B. A.; Raub T. J.; Higdon N. R.; Wall T. M.; Hurst R. S.; Walters R. R.; Hoffmann W. E.; Hajos M.; Franklin S.; Carey G.; Gold L. H.; Cook K. K.; Sands S. B.; Zhao S. X.; Soglia J. R.; Kalgutkar A. S.; Arneric S. P.; Rogers B. N. (2006) Discovery of N-[(3R)-1-azabicyclo[2.2.2]oct-3-yl]furo[2,3-c]pyridine-5-carboxamide, an agonist of the alpha7 nicotinic acetylcholine receptor, for the potential treatment of cognitive deficits in schizophrenia: synthesis and structure--activity relationship. J. Med. Chem. 49, 4425–4436. [DOI] [PubMed] [Google Scholar]
- Wooters T. E.; Bevins R. A.; Bardo M. T. (2009) Neuropharmacology of the interoceptive stimulus properties of nicotine. Curr. Drug Abuse Rev. 2, 243–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charntikov S.; Tracy M. E.; Zhao C.; Li M.; Bevins R. A. (2012) Conditioned response evoked by nicotine conditioned stimulus preferentially induces c-Fos expression in medial regions of caudate-putamen. Neuropsychopharmacology 37, 876–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everitt B. J.; Robbins T. W. (2005) Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat. Neurosci 8, 1481–1489. [DOI] [PubMed] [Google Scholar]
- Ashare R. L.; Falcone M.; Lerman C. (2014) Cognitive function during nicotine withdrawal: Implications for nicotine dependence treatment. Neuropharmacology 76(Pt B), 581–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markou A., and Paterson N. E.. (2009) Multiple motivational forces contribute to nicotine dependence In The motivational impact of nicotine and its role in tobacco use (Bevins R. A., and Caggiula A. R., Eds.), Nebraska Symposium on Motivation Vol. 55, pp 65–89, Springer, New York. [DOI] [PubMed] [Google Scholar]
- Robbins T. W. (2002) The 5-choice serial reaction time task: behavioural pharmacology and functional neurochemistry. Psychopharmacology (Berlin, Ger.) 163, 362–380. [DOI] [PubMed] [Google Scholar]
- Shoaib M.; Bizarro L. (2005) Deficits in a sustained attention task following nicotine withdrawal in rats. Psychopharmacology (Berlin, Ger.) 178, 211–222. [DOI] [PubMed] [Google Scholar]
- Levin E. D.; McClernon F. J.; Rezvani A. H. (2006) Nicotinic effects on cognitive function: behavioral characterization, pharmacological specification, and anatomic localization. Psychopharmacology (Berlin, Ger.) 184, 523–539. [DOI] [PubMed] [Google Scholar]
- Portugal G. S.; Gould T. J. (2007) Bupropion dose-dependently reverses nicotine withdrawal deficits in contextual fear conditioning. Pharmacol., Biochem. Behav. 88, 179–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markou A.; Chiamulera C.; Geyer M. A.; Tricklebank M.; Steckler T. (2009) Removing obstacles in neuroscience drug discovery: the future path for animal models. Neuropsychopharmacology 34, 74–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scammell T. E.; Estabrooke I. V.; McCarthy M. T.; Chemelli R. M.; Yanagisawa M.; Miller M. S.; Saper C. B. (2000) Hypothalamic arousal regions are activated during modafinil-induced wakefulness. J. Neurosci. 20, 8620–8628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballon J. S.; Feifel D. (2006) A systematic review of modafinil: Potential clinical uses and mechanisms of action. J. Clin. Psychiatry 67, 554–566. [DOI] [PubMed] [Google Scholar]
- Wisor J. P.; Eriksson K. S. (2005) Dopaminergic-adrenergic interactions in the wake promoting mechanism of modafinil. Neuroscience 132, 1027–1034. [DOI] [PubMed] [Google Scholar]
- Dopheide M. M.; Morgan R. E.; Rodvelt K. R.; Schachtman T. R.; Miller D. K. (2007) Modafinil evokes striatal [(3)H]dopamine release and alters the subjective properties of stimulants. Eur. J. Pharmacol. 568, 112–123. [DOI] [PubMed] [Google Scholar]
- Ferraro L.; Tanganelli S.; O’Connor W. T.; Antonelli T.; Rambert F.; Fuxe K. (1996) The vigilance promoting drug modafinil increases dopamine release in the rat nucleus accumbens via the involvement of a local GABAergic mechanism. Eur. J. Pharmacol. 306, 33–39. [DOI] [PubMed] [Google Scholar]
- Ferraro L.; Antonelli T.; O’Connor W. T.; Tanganelli S.; Rambert F. A.; Fuxe K. (1998) The effects of modafinil on striatal, pallidal and nigral GABA and glutamate release in the conscious rat: evidence for a preferential inhibition of striato-pallidal GABA transmission. Neurosci. Lett. 253, 135–138. [DOI] [PubMed] [Google Scholar]
- Perkins K. A.; Lerman C. (2014) An efficient early phase 2 procedure to screen medications for efficacy in smoking cessation. Psychopharmacology (Berlin, Ger.) 231, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnoll R. A.; Wileyto E. P.; Pinto A.; Leone F.; Gariti P.; Siegel S.; Perkins K. A.; Dackis C.; Heitjan D. F.; Berrettini W.; Lerman C. (2008) A placebo-controlled trial of modafinil for nicotine dependence. Drug Alcohol Depend. 98, 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C.; Chiu W. T.; Jin R.; Ruscio A. M.; Shear K.; Walters E. E. (2006) The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 63, 415–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M. M.; Bland R. C.; Canino G. J.; Faravelli C.; Greenwald S.; Hwu H. G.; Joyce P. R.; Karam E. G.; Lee C. K.; Lellouch J.; Lepine J. P.; Newman S. C.; Oakley-Browne M. A.; Rubio-Stipec M.; Wells J. E.; Wickramaratne P. J.; Wittchen H. U.; Yeh E. K. (1997) The cross-national epidemiology of panic disorder. Arch. Gen. Psychiatry 54, 305–309. [DOI] [PubMed] [Google Scholar]
- Schruers K.; Esquivel G.; van Duinen M.; Wichers M.; Kenis G.; Colasanti A.; Knuts I.; Goossens L.; Jacobs N.; van Rozendaal J.; Smeets H.; van Os J.; Griez E. (2011) Genetic moderation of CO2-induced fear by 5-HTTLPR genotype. J. Psychopharmacol. 25, 37–42. [DOI] [PubMed] [Google Scholar]
- Leibold N. K.; Viechtbauer W.; Goossens L.; De Cort K.; Griez E. J.; Myin-Germeys I.; Steinbusch H. W.; van den Hove D. L.; Schruers K. R. (2013) Carbon dioxide inhalation as a human experimental model of panic: the relationship between emotions and cardiovascular physiology. Biol. Psychol. 94, 331–340. [DOI] [PubMed] [Google Scholar]
- Forsyth J. P.; Eifert G. H. (1998) Response intensity in content-specific fear conditioning comparing 20% versus 13% CO2-enriched air as unconditioned stimuli. J. Abnorm. Psychol. 107, 291–304. [DOI] [PubMed] [Google Scholar]
- van den Bergh O.; Kempynck P. J.; van de Woestijne K. P.; Baeyens F.; Eelen P. (1995) Respiratory learning and somatic complaints: a conditioning approach using CO2-enriched air inhalation. Behav. Res. Ther. 33, 517–527. [DOI] [PubMed] [Google Scholar]
- Acheson D. T.; Forsyth J. P.; Prenoveau J. M.; Bouton M. E. (2007) Interoceptive fear conditioning as a learning model of panic disorder: an experimental evaluation using 20% CO(2)-enriched air in a non-clinical sample. Behav. Res. Ther. 45, 2280–2294. [DOI] [PubMed] [Google Scholar]
- De Cort K.; Griez E.; Buchler M.; Schruers K. (2012) The role of “interoceptive” fear conditioning in the development of panic disorder. Behav. Ther. 43, 203–215. [DOI] [PubMed] [Google Scholar]
- Stegen K.; De Bruyne K.; Rasschaert W.; Van de Woestijne K. P.; Van den Bergh O. (1999) Fear-relevant images as conditioned stimuli for somatic complaints, respiratory behavior, and reduced end-tidal pCO2. J. Abnorm. Psychol. 108, 143–152. [DOI] [PubMed] [Google Scholar]
- Forsyth J. P.; Eifert G. H.; Thompson R. N. (1996) Systemic alarms in fear conditioning 0.2. An experimental methodology using 20% carbon dioxide inhalation as an unconditioned stimulus. Behav. Ther. 27, 391–415. [Google Scholar]
- Acheson D. T.; Forsyth J. P.; Moses E. (2012) Interoceptive fear conditioning and panic disorder: the role of conditioned stimulus-unconditioned stimulus predictability. Behav. Ther. 43, 174–189. [DOI] [PubMed] [Google Scholar]
- Gorman J. M.; Papp L. A.; Coplan J. D.; Martinez J. M.; Lennon S.; Goetz R. R.; Ross D.; Klein D. F. (1994) Anxiogenic effects of CO2 and hyperventilation in patients with panic disorder. Am. J. Psychiatry 151, 547–553. [DOI] [PubMed] [Google Scholar]
- Griebel G.; Holmes A. (2013) 50 years of hurdles and hope in anxiolytic drug discovery. Nat. Rev. Drug Discovery 12, 667–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigurdsson T.; Doyere V.; Cain C. K.; LeDoux J. E. (2007) Long-term potentiation in the amygdala: a cellular mechanism of fear learning and memory. Neuropharmacology 52, 215–227. [DOI] [PubMed] [Google Scholar]
- Rosen J. B.; Donley M. P. (2006) Animal studies of amygdala function in fear and uncertainty: relevance to human research. Biol. Psychol. 73, 49–60. [DOI] [PubMed] [Google Scholar]
- Gorman J. M.; Kent J. M.; Sullivan G. M.; Coplan J. D. (2000) Neuroanatomical hypothesis of panic disorder, revised. Am. J. Psychiatry 157, 493–505. [DOI] [PubMed] [Google Scholar]
- Garakani A.; Mathew S. J.; Charney D. S. (2006) Neurobiology of anxiety disorders and implications for treatment. Mt. Sinai J. Med. 73, 941–949. [PubMed] [Google Scholar]
- Johnson P. L.; Shekhar A. (2012) An animal model of panic vulnerability with chronic disinhibition of the dorsomedial/perifornical hypothalamus. Physiol. Behav. 107, 686–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebowitz M. R.; Gorman J.; Fyer A.; Levitt M.; Levy G.; Dillon D.; Appleby I.; Anderson S.; Palij M.; Davies S. O. (1984) Biological accompaniments of lactate-induced panic. Psychopharmacol. Bull. 20, 43–44. [PubMed] [Google Scholar]
- Cowley D. S.; Dager S. R.; Roy-Byrne P. P.; Avery D. H.; Dunner D. L. (1991) Lactate vulnerability after alprazolam versus placebo treatment of panic disorder. Biol. Psychiatry 30, 49–56. [DOI] [PubMed] [Google Scholar]
- Jensen C. F.; Peskind E. R.; Keller T. W.; McFall M. E.; Raskind M. A. (1998) Comparison of sodium lactate-induced panic symptoms between panic disorder and posttraumatic stress disorder. Depression Anxiety 7, 122–125. [PubMed] [Google Scholar]
- Goetz R. R.; Klein D. F.; Gorman J. M. (1996) Symptoms essential to the experience of sodium lactate-induced panic. Neuropsychopharmacology 14, 355–366. [DOI] [PubMed] [Google Scholar]
- Johnson P. L.; Shekhar A. (2006) Panic-prone state induced in rats with GABA dysfunction in the dorsomedial hypothalamus is mediated by NMDA receptors. J. Neurosci. 26, 7093–7104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekhar A.; Keim S. R. (2000) LY354740, a potent group II metabotropic glutamate receptor agonist prevents lactate-induced panic-like response in panic-prone rats. Neuropharmacology 39, 1139–1146. [DOI] [PubMed] [Google Scholar]
- Johnson P. L.; Fitz S. D.; Engleman E. A.; Svensson K. A.; Schkeryantz J. M.; Shekhar A. (2013) Group II metabotropic glutamate receptor type 2 allosteric potentiators prevent sodium lactate-induced panic-like response in panic-vulnerable rats. J. Psychopharmacol. 27, 152–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson P. L.; Truitt W.; Fitz S. D.; Minick P. E.; Dietrich A.; Sanghani S.; Traskman-Bendz L.; Goddard A. W.; Brundin L.; Shekhar A. (2010) A key role for orexin in panic anxiety. Nat. Med. 16, 111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitte K. (2005) A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. J. Affective Disord. 88, 27–45. [DOI] [PubMed] [Google Scholar]
- Andrisano C.; Chiesa A.; Serretti A. (2013) Newer antidepressants and panic disorder: a meta-analysis. Int. Clin. Psychopharmacol. 28, 33–45. [DOI] [PubMed] [Google Scholar]
- van Balkom A. J.; Bakker A.; Spinhoven P.; Blaauw B. M.; Smeenk S.; Ruesink B. (1997) A meta-analysis of the treatment of panic disorder with or without agoraphobia: a comparison of psychopharmacological, cognitive-behavioral, and combination treatments. J. Nerv. Ment. Dis. 185, 510–516. [DOI] [PubMed] [Google Scholar]
- Schmidt N. B.; Trakowski J. (2004) Interoceptive assessment and exposure in panic disorder: A descriptive study. Cognit. Behav. Pract. 11, 81–92. [Google Scholar]
- Antony M. M.; Ledley D. R.; Liss A.; Swinson R. P. (2006) Responses to symptom induction exercises in panic disorder. Behav. Res. Ther. 44, 85–98. [DOI] [PubMed] [Google Scholar]
- Lee K.; Noda Y.; Nakano Y.; Ogawa S.; Kinoshita Y.; Funayama T.; Furukawa T. A. (2006) Interoceptive hypersensitivity and interoceptive exposure in patients with panic disorder: Specificity and effectiveness. BMC Psychiatry 6, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norberg M. M.; Krystal J. H.; Tolin D. F. (2008) A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol. Psychiatry 63, 1118–1126. [DOI] [PubMed] [Google Scholar]
- Otto M. W.; Tolin D. F.; Simon N. M.; Pearlson G. D.; Basden S.; Meunier S. A.; Hofmann S. G.; Eisenmenger K.; Krystal J. H.; Pollack M. H. (2010) Efficacy of d-cycloserine for enhancing response to cognitive-behavior therapy for panic disorder. Biol. Psychiatry 67, 365–370. [DOI] [PubMed] [Google Scholar]
- Fadel J.; Burk J. A. (2010) Orexin/hypocretin modulation of the basal forebrain cholinergic system: Role in attention. Brain Res. 1314, 112–123. [DOI] [PMC free article] [PubMed] [Google Scholar]


